Temporal Association of Reduced Serum Vitamin D with COVID-19 Infection: Two Single-Institution Case–Control Studies
et al., Nutrients, doi:10.3390/nu14132757, Jul 2022
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 135 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
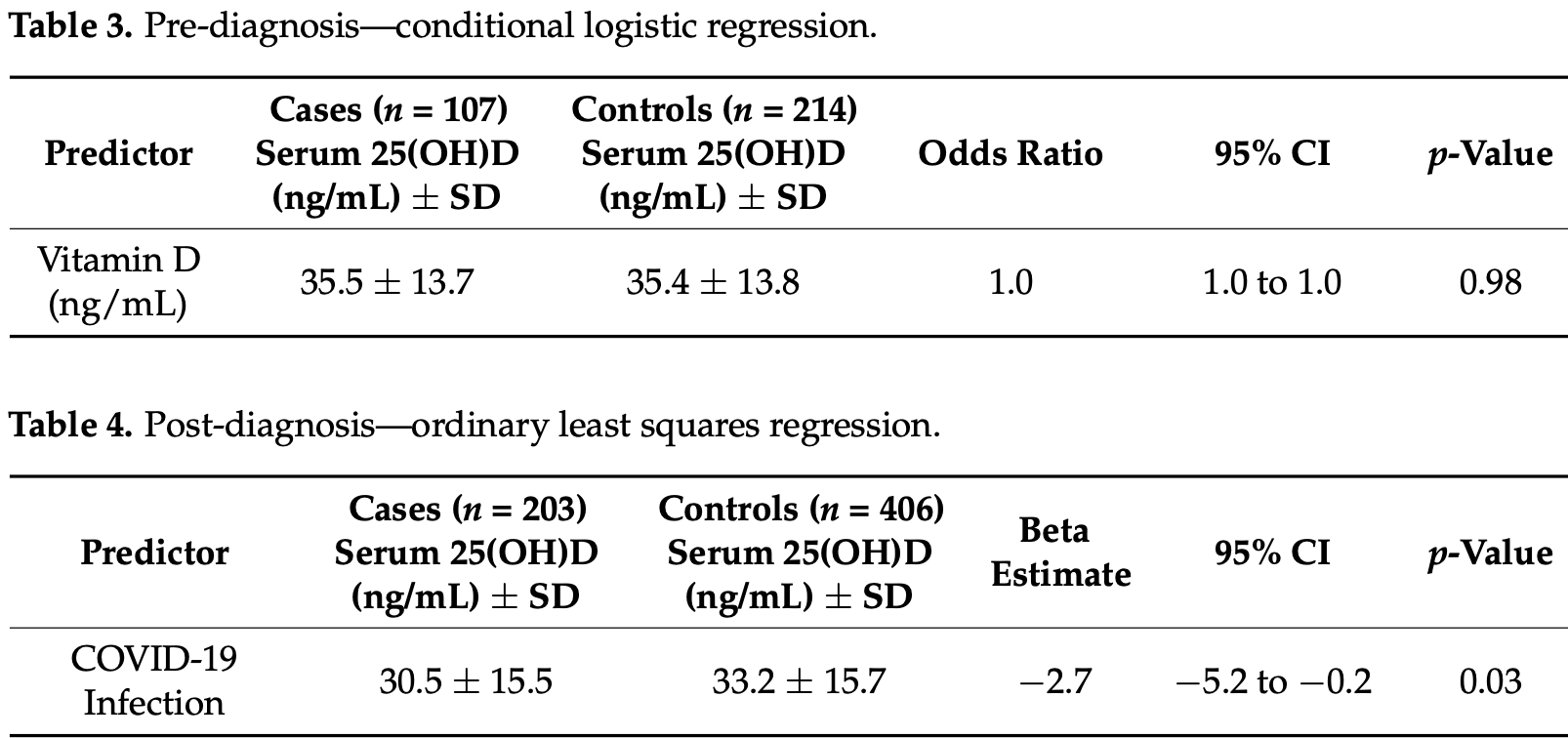
Retrospective study of 107 COVID-19 patients with vitamin D levels measured within 180 days before diagnosis, and 203 patients with levels measured after diagnosis, showing lower vitamin D levels for COVID-19 hospitalized patients compared to non-COVID-19 patients, but no significant association between vitamin D levels before infection and cases.
Authors do not analyze the risk of serious outcomes based on pre-infection levels. Intervention studies show minimal benefit for cases, but much greater benefit for serious outcomes. Results are provided only for vitamin D as a continuous variable.
Gupta et al., 2 Jul 2022, USA, peer-reviewed, 4 authors, study period 1 January, 2020 - 30 September, 2020.
Contact: bryansun@health.ucsd.edu (corresponding author), digupta@health.ucsd.edu, s1menon@health.ucsd.edu, mcriqui@health.ucsd.edu.
Temporal Association of Reduced Serum Vitamin D with COVID-19 Infection: Two Single-Institution Case–Control Studies
Nutrients, doi:10.3390/nu14132757
1) Background: Vitamin D supplementation has been proposed for the prevention and treatment of COVID-19, but it is not clear if reduced serum vitamin D predisposes individuals to COVID-19 and/or is a secondary consequence of infection. This study assessed the temporal association between serum vitamin D and COVID-19 with two single-institution case-control studies through the University of California San Diego (UCSD) Health System. (2) Methods: This study included patients who tested positive for COVID-19 from 1 January to 30 September 2020 with serum 25-hydroxy-vitamin D (25(OH)D) measured within 180 days of diagnosis. Patients were separated based on whether 25(OH)D was measured before (n = 107 cases, 214 controls) or after (n = 203 cases, 406 controls) COVID-19 diagnosis. COVID-19 infection status was the outcome variable in the pre-diagnosis study, whereas serum 25(OH)D level was the outcome variable in the post-diagnosis study. (3) Results: Serum 25(OH)D levels were not associated with the odds of subsequent COVID-19 infection (OR 1.0, 95% CI: 1.0 to 1.0, p = 0.98). However, COVID-19-positive individuals had serum 25(OH)D measurements that were 2.7 ng/mL lower than the controls (95% CI: −5.2 to −0.2, p = 0.03). (4) Conclusions: In our study population, serum 25(OH)D levels were not associated with the risk of acquiring COVID-19 infection but were reduced in subjects after COVID-19 infection. These results support the possibility that reduced serum 25(OH)D is a consequence and not a cause of COVID-19 infection.
Conflicts of Interest: The authors declare no conflict of interest.
References
Ali, Role of Vitamin D in Preventing of COVID-19 Infection, Progression and Severity, J. Infection Public Health, doi:10.1016/j.jiph.2020.06.021
Alpcan, Tursun, Kandur, Vitamin D Levels in Children with COVID-19: A Report from Turkey, Epidemiol. Infect, doi:10.1017/S0950268821001825
Annweiler, Hanotte, Grandin De L'eprevier, Sabatier, Lafaie et al., Vitamin D and Survival in COVID-19 Patients: A Quasi-Experimental Study, J. Steroid Biochem. Mol. Biol, doi:10.1016/j.jsbmb.2020.105771
Aranow, Vitamin D and the Immune System, J. Investig. Med, doi:10.2310/JIM.0b013e31821b8755
Bang, Novovic, Andersen, Fenger, Hansen et al., Variations in Serum 25-Hydroxyvitamin D during Acute Pancreatitis: An Exploratory Longitudinal Study, Endocrine Res, doi:10.3109/07435800.2011.554937
Barlow, Svoboda, Mackellar, Nash, York et al., Antiviral Activity and Increased Host Defense against Influenza Infection Elicited by the Human Cathelicidin LL-37, PLoS ONE
Bialek, Boundy, Bowen, Chow, Cohn et al., Severe Outcomes Among Patients with Coronavirus Disease 2019 (COVID-19) -United States, MMWR Morb. Mortal. Wkly. Rep, doi:10.15585/mmwr.mm6912e2
Campi, Gennari, Merlotti, Mingiano, Frosali et al., Vitamin D and COVID-19 Severity and Related Mortality: A Prospective Study in Italy, BMC Infect. Dis, doi:10.1186/s12879-021-06281-7
Castillo, Entrenas Costa, Vaquero Barrios, Alcalá Díaz, López Miranda et al., Effect of Calcifediol Treatment and Best Available Therapy versus Best Available Therapy on Intensive Care Unit Admission and Mortality among Patients Hospitalized for COVID-19: A Pilot Randomized Clinical Study, J. Steroid Biochem. Mol. Biol, doi:10.1016/j.jsbmb.2020.105751
D'avolio, Avataneo, Manca, Cusato, De Nicolò et al., 25-Hydroxyvitamin D Concentrations Are Lower in Patients with Positive PCR for SARS-CoV-2, Nutrients, doi:10.3390/nu12051359
Davoudi, Najafi, Aarabi, Tayebi, Nikaeen et al., Lack of Association between Vitamin D Insufficiency and Clinical Outcomes of Patients with COVID-19 Infection, BMC Infect. Dis, doi:10.1186/s12879-021-06168-7
Ferrari, Locatelli, No Significant Association between Vitamin D and COVID-19. A Retrospective Study from a Northern Italian Hospital, Int. J. Vitamin Nutr. Res, doi:10.1024/0300-9831/a000687
Ginde, Mansbach, Camargo, Vitamin, Respiratory Infections, and Asthma, Curr. Allergy Asthma Rep, doi:10.1007/s11882-009-0012-7
Grant, Lahore, Mcdonnell, Baggerly, French et al., Evidence That Vitamin D Supplementation Could Reduce Risk of Influenza and COVID-19 Infections and Deaths, Nutrients, doi:10.3390/nu12040988
Hastie, Mackay, Ho, Celis-Morales, Katikireddi et al., Vitamin D Concentrations and COVID-19 Infection in UK Biobank, Diabet. Metab. Syndr. Clin. Res. Rev, doi:10.1016/j.dsx.2020.04.050
Haugen, Chandyo, Ulak, Mathisen, Basnet et al., 25-Hydroxy-Vitamin D Concentration Is Not Affected by Severe or Non-Severe Pneumonia, or Inflammation, in Young Children, Nutrients, doi:10.3390/nu9010052
Hicks, Kammerling, The Relationship between a Severity of Illness Indicator and Mortality and Length-of-Stay, Health Trends
Hughes, Norton, Vitamin, Respiratory Health, Clin. Exp. Immunol, doi:10.1111/j.1365-2249.2009.04001.x
Ilie, Stefanescu, Smith, The Role of Vitamin D in the Prevention of Coronavirus Disease 2019 Infection and Mortality, Aging Clin. Exp. Res, doi:10.1007/s40520-020-01570-8
Jolliffe, Stefanidis, Wang, Kermani, Dimitrov et al., Vitamin D Metabolism Is Dysregulated in Asthma and Chronic Obstructive Pulmonary Disease, Am. J. Respir. Crit. Care Med, doi:10.1164/rccm.201909-1867OC
Jordan, Adab, Cheng, Covid-19: Risk Factors for Severe Disease and Death, BMJ, doi:10.1136/bmj.m1198
Kasahara, Singh, Noymer, Vitamin D (25OHD) Serum Seasonality in the United States, PLoS ONE, doi:10.1371/journal.pone.0065785
Kimlin, Geographic Location and Vitamin D Synthesis, Mol. Aspects Med, doi:10.1016/j.mam.2008.08.005
Klingberg, Oleröd, Konar, Petzold, Hammarsten, Seasonal Variations in Serum 25-Hydroxy Vitamin D Levels in a Swedish Cohort, Endocrine, doi:10.1007/s12020-015-0548-3
Kruit, Zanen, The Association between Vitamin D and C-Reactive Protein Levels in Patients with Inflammatory and Non-Inflammatory Diseases, Clin. Biochem, doi:10.1016/j.clinbiochem.2016.01.002
Lai, Lucas, Banks, Ponsonby, Ausimmune Investigator Group Variability in Vitamin D Assays Impairs Clinical Assessment of Vitamin D Status: Variability in Vitamin D Assays, Intern. Med. J, doi:10.1111/j.1445-5994.2011.02471.x
Lau, Powell, Adonecchi, Danos, Dinardo et al., Pilot Phase Results of a Prospective, Randomized Controlled Trial of Narrowband Ultraviolet B Phototherapy in Hospitalized COVID-19 Patients, Exp. Dermatol, doi:10.1111/exd.14617
Macaya, Espejo Paeres, Valls, Fernández-Ortiz, González Del Castillo et al., Interaction between Age and Vitamin D Deficiency in Severe COVID-19 Infection, Nutr. Hosp
Maghbooli, Sahraian, Ebrahimi, Pazoki, Kafan et al., Vitamin D Sufficiency, a Serum 25-Hydroxyvitamin D at Least 30 Ng/ML Reduced Risk for Adverse Clinical Outcomes in Patients with COVID-19 Infection, PLoS ONE, doi:10.1371/journal.pone.0239799
Martineau, Forouhi, Vitamin D for COVID-19: A Case to Answer?, Lancet Diabet. Endocrinol
Meltzer, Best, Zhang, Vokes, Arora et al., Association of Vitamin D Status and Other Clinical Characteristics With COVID-19 Test Results, JAMA Netw. Open, doi:10.1001/jamanetworkopen.2020.19722
Meng, Hovey, Wactawski-Wende, Andrews, Lamonte et al., Intraindividual Variation in Plasma 25-Hydroxyvitamin D Measures 5 Years Apart among Postmenopausal Women, Cancer Epidemiol. Biomark. Prev, doi:10.1158/1055-9965.EPI-12-0026
Merzon, Tworowski, Gorohovski, Vinker, Golan Cohen et al., Low Plasma 25(OH) Vitamin D Level Is Associated with Increased Risk of COVID-19 Infection: An Israeli Population-based Study, FEBS J, doi:10.1111/febs.15495
Murai, Fernandes, Sales, Pinto, Goessler et al., Effect of a Single High Dose of Vitamin D3 on Hospital Length of Stay in Patients With Moderate to Severe COVID-19: A Randomized Clinical Trial, JAMA, doi:10.1001/jama.2020.26848
Newens, Filteau, Tomkins, Plasma 25-Hydroxyvitamin D Does Not Vary over the Course of a Malarial Infection, Transact. Royal Soc. Trop. Med. Hygiene, doi:10.1016/j.trstmh.2005.06.022
Panagiotou, Tee, Ihsan, Athar, Marchitelli et al., Low Serum 25-hydroxyvitamin D (25[OH]D) Levels in Patients Hospitalized with COVID-19 Are Associated with Greater Disease Severity, Clin. Endocrinol, doi:10.1111/cen.14276
Quraishi, Camargo, Vitamin D in Acute Stress and Critical Illness, Curr. Opin. Clin. Nutr. Metab. Care
Radujkovic, Hippchen, Tiwari-Heckler, Dreher, Boxberger et al., Vitamin D Deficiency and Outcome of COVID-19 Patients, Nutrients, doi:10.3390/nu12092757
Rhodes, Dunstan, Laird, Subramanian, Kenny, COVID-19 Mortality Increases with Northerly Latitude after Adjustment for Age Suggesting a Link with Ultraviolet and Vitamin D, BMJ Nutr. Prev. Health, doi:10.1136/bmjnph-2020-000110
Rubin, Sorting Out Whether Vitamin D Deficiency Raises COVID-19 Risk, JAMA, doi:10.1001/jama.2020.24127
Silva, Furlanetto, Does Serum 25-Hydroxyvitamin D Decrease during Acute-Phase Response? A Systematic Review, Nutr. Res, doi:10.1016/j.nutres.2014.12.008
Sinha, Matthay, Calfee, Is a "Cytokine Storm" Relevant to COVID-19?, JAMA Intern. Med, doi:10.1001/jamainternmed.2020.3313
Smolders, Van Den Ouweland, Geven, Pickkers, Kox, Letter to the Editor: Vitamin D Deficiency in COVID-19: Mixing up Cause and Consequence, Metabolism, doi:10.1016/j.metabol.2020.154434
Waldron, Ashby, Cornes, Bechervaise, Razavi et al., A Negative Acute Phase Reactant, J. Clin. Pathol, doi:10.1136/jclinpath-2012-201301
Wang, Liu, Wang, Li, Lan et al., Allergen Specific Immunotherapy Enhanced Defense against Bacteria via TGF-β1-Induced CYP27B1 in Asthma, Oncotarget, doi:10.18632/oncotarget.19826
Wei, Christakos, Mechanisms Underlying the Regulation of Innate and Adaptive Immunity by Vitamin D, Nutrients, doi:10.3390/nu7105392
Ye, Tang, Liao, Shaw, Deng et al., Does Serum Vitamin D Level Affect COVID-19 Infection and Its Severity?-A Case-Control Study, J. Am. Coll. Nutr, doi:10.1080/07315724.2020.1826005
DOI record:
{
"DOI": "10.3390/nu14132757",
"ISSN": [
"2072-6643"
],
"URL": "http://dx.doi.org/10.3390/nu14132757",
"abstract": "<jats:p>(1) Background: Vitamin D supplementation has been proposed for the prevention and treatment of COVID-19, but it is not clear if reduced serum vitamin D predisposes individuals to COVID-19 and/or is a secondary consequence of infection. This study assessed the temporal association between serum vitamin D and COVID-19 with two single-institution case–control studies through the University of California San Diego (UCSD) Health System. (2) Methods: This study included patients who tested positive for COVID-19 from 1 January to 30 September 2020 with serum 25-hydroxy-vitamin D (25(OH)D) measured within 180 days of diagnosis. Patients were separated based on whether 25(OH)D was measured before (n = 107 cases, 214 controls) or after (n = 203 cases, 406 controls) COVID-19 diagnosis. COVID-19 infection status was the outcome variable in the pre-diagnosis study, whereas serum 25(OH)D level was the outcome variable in the post-diagnosis study. (3) Results: Serum 25(OH)D levels were not associated with the odds of subsequent COVID-19 infection (OR 1.0, 95% CI: 1.0 to 1.0, p = 0.98). However, COVID-19-positive individuals had serum 25(OH)D measurements that were 2.7 ng/mL lower than the controls (95% CI: −5.2 to −0.2, p = 0.03). (4) Conclusions: In our study population, serum 25(OH)D levels were not associated with the risk of acquiring COVID-19 infection but were reduced in subjects after COVID-19 infection. These results support the possibility that reduced serum 25(OH)D is a consequence and not a cause of COVID-19 infection.</jats:p>",
"alternative-id": [
"nu14132757"
],
"author": [
{
"affiliation": [],
"family": "Gupta",
"given": "Diviya",
"sequence": "first"
},
{
"affiliation": [],
"family": "Menon",
"given": "Sahit",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Criqui",
"given": "Michael H.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Sun",
"given": "Bryan K.",
"sequence": "additional"
}
],
"container-title": "Nutrients",
"container-title-short": "Nutrients",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2022,
7,
5
]
],
"date-time": "2022-07-05T00:59:18Z",
"timestamp": 1656982758000
},
"deposited": {
"date-parts": [
[
2022,
7,
5
]
],
"date-time": "2022-07-05T01:29:28Z",
"timestamp": 1656984568000
},
"funder": [
{
"award": [
"N/A"
],
"name": "University of California San Diego Office of Research Affairs"
}
],
"indexed": {
"date-parts": [
[
2022,
7,
5
]
],
"date-time": "2022-07-05T02:11:03Z",
"timestamp": 1656987063606
},
"is-referenced-by-count": 0,
"issue": "13",
"issued": {
"date-parts": [
[
2022,
7,
2
]
]
},
"journal-issue": {
"issue": "13",
"published-online": {
"date-parts": [
[
2022,
7
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
7,
2
]
],
"date-time": "2022-07-02T00:00:00Z",
"timestamp": 1656720000000
}
}
],
"link": [
{
"URL": "https://www.mdpi.com/2072-6643/14/13/2757/pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1968",
"original-title": [],
"page": "2757",
"prefix": "10.3390",
"published": {
"date-parts": [
[
2022,
7,
2
]
]
},
"published-online": {
"date-parts": [
[
2022,
7,
2
]
]
},
"publisher": "MDPI AG",
"reference": [
{
"DOI": "10.3390/nu7105392",
"doi-asserted-by": "publisher",
"key": "ref1"
},
{
"DOI": "10.1007/s11882-009-0012-7",
"doi-asserted-by": "publisher",
"key": "ref2"
},
{
"DOI": "10.1371/journal.pone.0025333",
"doi-asserted-by": "publisher",
"key": "ref3"
},
{
"DOI": "10.2310/JIM.0b013e31821b8755",
"doi-asserted-by": "publisher",
"key": "ref4"
},
{
"DOI": "10.1001/jamainternmed.2020.3313",
"doi-asserted-by": "publisher",
"key": "ref5"
},
{
"DOI": "10.3390/nu12040988",
"doi-asserted-by": "publisher",
"key": "ref6"
},
{
"DOI": "10.1016/j.mam.2008.08.005",
"doi-asserted-by": "publisher",
"key": "ref7"
},
{
"DOI": "10.1001/jamanetworkopen.2020.19722",
"doi-asserted-by": "publisher",
"key": "ref8"
},
{
"DOI": "10.1111/febs.15495",
"doi-asserted-by": "publisher",
"key": "ref9"
},
{
"DOI": "10.1016/j.dsx.2020.04.050",
"doi-asserted-by": "publisher",
"key": "ref10"
},
{
"DOI": "10.1024/0300-9831/a000687",
"doi-asserted-by": "publisher",
"key": "ref11"
},
{
"DOI": "10.3390/nu12092757",
"doi-asserted-by": "publisher",
"key": "ref12"
},
{
"DOI": "10.1371/journal.pone.0239799",
"doi-asserted-by": "publisher",
"key": "ref13"
},
{
"DOI": "10.20960/nh.03193",
"doi-asserted-by": "publisher",
"key": "ref14"
},
{
"DOI": "10.1080/07315724.2020.1826005",
"doi-asserted-by": "publisher",
"key": "ref15"
},
{
"DOI": "10.1111/cen.14276",
"doi-asserted-by": "publisher",
"key": "ref16"
},
{
"DOI": "10.1016/j.jsbmb.2020.105751",
"doi-asserted-by": "publisher",
"key": "ref17"
},
{
"DOI": "10.1016/j.jsbmb.2020.105771",
"doi-asserted-by": "publisher",
"key": "ref18"
},
{
"DOI": "10.1016/S2213-8587(20)30268-0",
"doi-asserted-by": "publisher",
"key": "ref19"
},
{
"DOI": "10.1016/j.jiph.2020.06.021",
"doi-asserted-by": "publisher",
"key": "ref20"
},
{
"DOI": "10.1007/s40520-020-01570-8",
"doi-asserted-by": "publisher",
"key": "ref21"
},
{
"DOI": "10.1136/bmjnph-2020-000110",
"doi-asserted-by": "publisher",
"key": "ref22"
},
{
"DOI": "10.1371/journal.pone.0065785",
"doi-asserted-by": "publisher",
"key": "ref23"
},
{
"DOI": "10.1158/1055-9965.EPI-12-0026",
"doi-asserted-by": "publisher",
"key": "ref24"
},
{
"DOI": "10.1007/s12020-015-0548-3",
"doi-asserted-by": "publisher",
"key": "ref25"
},
{
"DOI": "10.1186/s12879-021-06281-7",
"doi-asserted-by": "publisher",
"key": "ref26"
},
{
"DOI": "10.1186/s12879-021-06168-7",
"doi-asserted-by": "publisher",
"key": "ref27"
},
{
"DOI": "10.3390/nu12051359",
"doi-asserted-by": "publisher",
"key": "ref28"
},
{
"DOI": "10.1097/MCO.0b013e328358fc2b",
"doi-asserted-by": "publisher",
"key": "ref29"
},
{
"DOI": "10.15585/mmwr.mm6912e2",
"doi-asserted-by": "publisher",
"key": "ref30"
},
{
"article-title": "The Relationship between a Severity of Illness Indicator and Mortality and Length-of-Stay",
"author": "Hicks",
"first-page": "65",
"journal-title": "Health Trends",
"key": "ref31",
"volume": "25",
"year": "1993"
},
{
"DOI": "10.1136/bmj.m1198",
"doi-asserted-by": "publisher",
"key": "ref32"
},
{
"DOI": "10.1001/jama.2020.24127",
"doi-asserted-by": "publisher",
"key": "ref33"
},
{
"DOI": "10.1017/S0950268821001825",
"doi-asserted-by": "publisher",
"key": "ref34"
},
{
"DOI": "10.3390/nu9010052",
"doi-asserted-by": "publisher",
"key": "ref35"
},
{
"DOI": "10.1016/j.trstmh.2005.06.022",
"doi-asserted-by": "publisher",
"key": "ref36"
},
{
"DOI": "10.3109/07435800.2011.554937",
"doi-asserted-by": "publisher",
"key": "ref37"
},
{
"DOI": "10.1016/j.clinbiochem.2016.01.002",
"doi-asserted-by": "publisher",
"key": "ref38"
},
{
"DOI": "10.1016/j.nutres.2014.12.008",
"doi-asserted-by": "publisher",
"key": "ref39"
},
{
"DOI": "10.1016/j.metabol.2020.154434",
"doi-asserted-by": "publisher",
"key": "ref40"
},
{
"DOI": "10.1111/j.1365-2249.2009.04001.x",
"doi-asserted-by": "publisher",
"key": "ref41"
},
{
"DOI": "10.1136/jclinpath-2012-201301",
"doi-asserted-by": "publisher",
"key": "ref42"
},
{
"DOI": "10.18632/oncotarget.19826",
"doi-asserted-by": "publisher",
"key": "ref43"
},
{
"DOI": "10.1164/rccm.201909-1867OC",
"doi-asserted-by": "publisher",
"key": "ref44"
},
{
"DOI": "10.1111/j.1445-5994.2011.02471.x",
"doi-asserted-by": "publisher",
"key": "ref45"
},
{
"DOI": "10.1111/exd.14617",
"doi-asserted-by": "publisher",
"key": "ref46"
},
{
"DOI": "10.1001/jama.2020.26848",
"doi-asserted-by": "publisher",
"key": "ref47"
}
],
"reference-count": 47,
"references-count": 47,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.mdpi.com/2072-6643/14/13/2757"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Food Science",
"Nutrition and Dietetics"
],
"subtitle": [],
"title": "Temporal Association of Reduced Serum Vitamin D with COVID-19 Infection: Two Single-Institution Case–Control Studies",
"type": "journal-article",
"volume": "14"
}
