Kidney Transplant Recipients and Omicron: Outcomes, effect of vaccines and the efficacy and safety of novel treatments
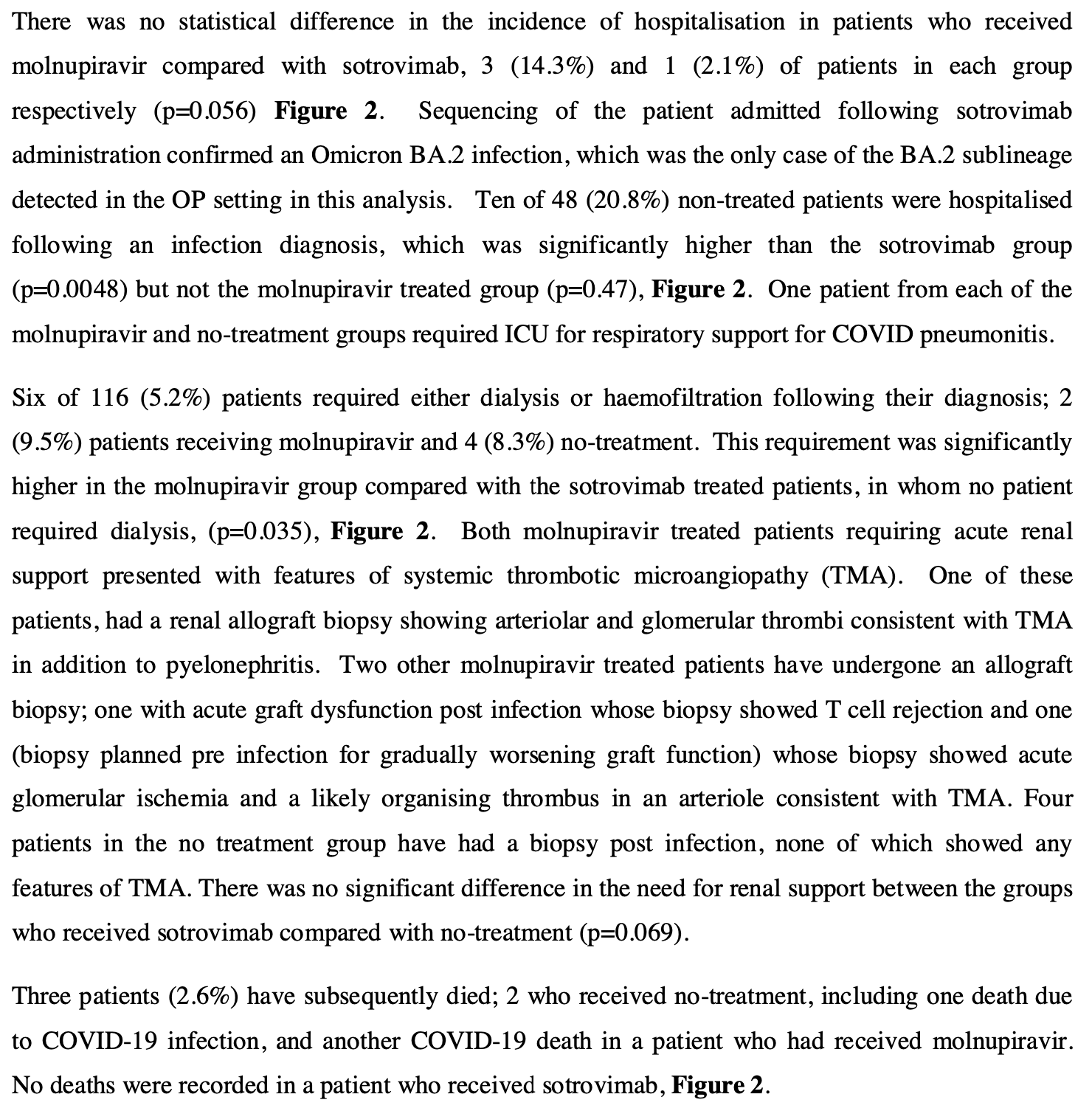
et al., medRxiv, doi:10.1101/2022.05.03.22274524, May 2022
Sotrovimab for COVID-19
45th treatment shown to reduce risk in
August 2022, now with p = 0.00048 from 29 studies, recognized in 42 countries.
Efficacy is variant dependent.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 116 kidney transplant recipients diagnosed with COVID-19 in the community during the Omicron era in the UK, showing lower hospitalization with sotrovimab, but no significant difference with molnupiravir. Two molnupiravir-treated patients requiring dialysis had features of thrombotic microangiopathy, raising potential safety concerns.
Efficacy is variant dependent. In Vitro studies predict lower efficacy for BA.11-3, BA.4, BA.54, XBB.1.9.3, XBB.1.5.24, XBB.2.9, CH.1.15, and no efficacy for BA.26, XBB, XBB.1.5, ХВВ.1.9.17, XBB.1.16, BQ.1.1.45, and CL.15. US EUA has been revoked.
Standard of Care (SOC) for COVID-19 in the study country,
the United Kingdom, is very poor with very low average efficacy for approved treatments8.
The United Kingdom focused on expensive high-profit treatments, approving only one low-cost early treatment, which required a prescription and had limited adoption. The high-cost prescription treatment strategy reduces the probability of early treatment due to access and cost barriers, and eliminates complementary and synergistic benefits seen with many low-cost treatments.
Study covers molnupiravir and sotrovimab.
|
risk of death, 66.4% lower, RR 0.34, p = 1.00, treatment 0 of 47 (0.0%), control 1 of 48 (2.1%), NNT 48, relative risk is not 0 because of continuity correction due to zero events (with reciprocal of the contrasting arm), COVID-19.
|
|
risk of death, 79.8% lower, RR 0.20, p = 0.49, treatment 0 of 47 (0.0%), control 2 of 48 (4.2%), NNT 24, relative risk is not 0 because of continuity correction due to zero events (with reciprocal of the contrasting arm), all cause.
|
|
risk of ICU admission, 66.4% lower, RR 0.34, p = 1.00, treatment 0 of 47 (0.0%), control 1 of 48 (2.1%), NNT 48, relative risk is not 0 because of continuity correction due to zero events (with reciprocal of the contrasting arm).
|
|
risk of hospitalization, 89.8% lower, RR 0.10, p = 0.008, treatment 1 of 47 (2.1%), control 10 of 48 (20.8%), NNT 5.3.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
1.
Liu et al., Striking Antibody Evasion Manifested by the Omicron Variant of SARS-CoV-2, bioRxiv, doi:10.1101/2021.12.14.472719.
2.
Sheward et al., Variable loss of antibody potency against SARS-CoV-2 B.1.1.529 (Omicron), bioRxiv, doi:10.1101/2021.12.19.473354.
3.
VanBlargan et al., An infectious SARS-CoV-2 B.1.1.529 Omicron virus escapes neutralization by several therapeutic monoclonal antibodies, bioRxiv, doi:10.1101/2021.12.15.472828.
4.
Haars et al., Prevalence of SARS-CoV-2 Omicron Sublineages and Spike Protein Mutations Conferring Resistance against Monoclonal Antibodies in a Swedish Cohort during 2022–2023, Microorganisms, doi:10.3390/microorganisms11102417.
5.
Pochtovyi et al., In Vitro Efficacy of Antivirals and Monoclonal Antibodies against SARS-CoV-2 Omicron Lineages XBB.1.9.1, XBB.1.9.3, XBB.1.5, XBB.1.16, XBB.2.4, BQ.1.1.45, CH.1.1, and CL.1, Vaccines, doi:10.3390/vaccines11101533.
6.
Zhou et al., SARS-CoV-2 Omicron BA.2 Variant Evades Neutralization by Therapeutic Monoclonal Antibodies, bioRxiv, doi:10.1101/2022.02.15.480166.
Gleeson et al., 3 May 2022, prospective, United Kingdom, preprint, 14 authors, study period 21 December, 2021 - 10 February, 2022.
Contact: m.willicombe08@imperial.ac.uk.
Kidney Transplant Recipients and Omicron: Outcomes, effect of vaccines and the efficacy and safety of novel treatments
doi:10.1101/2022.05.03.22274524
We aimed to describe the outcomes of Omicron infection in kidney transplant recipients (KTR), compare the efficacy of the community therapeutic interventions and report the safety profile of molnupiravir. From 142 KTRs diagnosed with COVID-19 infection after Omicron had become the dominant variant in the UK, 116 (78.9%) cases were diagnosed in the community; 47 receiving sotrovimab, 21 molnupiravir and 48 no treatment. 10 (20.8%) non-treated patients were hospitalised following infection, which was significantly higher than the sotrovimab group (2.1%), p=0.0048, but not the molnupiravir treated group (14.3%), p=0.47. The only admission following sotrovimab occurred in a patient infected with BA.2. One patient from the molnupiravir and no-treatment groups required ICU support, and both subsequently died, with one other death in the no-treatment group. No patient receiving sotrovimab died. 6/116 (5.2%) patients required dialysis following their diagnosis; 2 (9.5%) patients receiving molnupiravir and 4 (8.3%) no-treatment. This requirement was significantly higher in the molnupiravir group compared with the sotrovimab treated patients, in whom no patient required dialysis, p=0.035. Both molnupiravir treated patients requiring dialysis had features of systemic thrombotic microangiopathy. Post-vaccination serostatus was available in 110 patients. Seropositive patients were less likely to require hospital admission compared with seronegative patients, 6 (7.0%) and 6 (25.0%) respectively, p=0.023. Seropositive patients were also less likely to require dialysis therapy, p=0.016. In conclusion, sotrovimab treatment in the community was associated with superior patient and transplant outcomes; it's clinical efficacy against the BA.2 variant requires a rapid review. The treatment benefit of molnupiravir was not evident, and wider safety reporting in transplant patients is needed.
risk group with poor infection outcomes, immunosuppressed people often with significant comorbidities, have been excluded from policy informing studies from the start of the pandemic. Relying on extrapolating data from these studies to inform management of transplant recipients, may and has led to suboptimal outcomes.
References
Benotmane, Pre-exposure prophylaxis with Evusheld™ elicits limited neutralizing activity against the omicron variant in kidney transplant patients, medRxiv
Bernal, Molnupiravir for Oral Treatment of Covid-19 in Nonhospitalized Patients, N Engl J Med
Broecker, Clinical-pathological correlations in post-transplant thrombotic microangiopathy, Histopathology
Callaghan, Real-world Effectiveness of the Pfizer-BioNTech BNT162b2 and Oxford-AstraZeneca ChAdOx1-S Vaccines Against SARS-CoV-2 in Solid Organ and Islet Transplant Recipients, Transplantation
Chavarot, Early treatment with sotrovimab monoclonal antibody in kidney transplant recipients with Omicron infection
Extance, Covid-19: What is the evidence for the antiviral molnupiravir?, BMJ
Gupta, Early Treatment for Covid-19 with SARS-CoV-2 Neutralizing Antibody Sotrovimab, N Engl J Med
Iketani, Antibody evasion properties of SARS-CoV-2 Omicron sublineages, Nature
Kemp, SARS-CoV-2 evolution during treatment of chronic infection, Nature
Prendecki, Immunological responses to SARS-CoV-2 vaccines in kidney transplant recipients, Lancet
Villanego, Trends in COVID-19 Outcomes in Kidney Transplant Recipients During the Period of Omicron Variant Predominance, Transplantation
Willicombe, Scanlon, Miranda, Loud, Lightstone, Should we be clinically assessing antibody responses to covid vaccines in immunocompromised people?, BMJ
DOI record:
{
"DOI": "10.1101/2022.05.03.22274524",
"URL": "http://dx.doi.org/10.1101/2022.05.03.22274524",
"abstract": "<jats:title>Abstract</jats:title><jats:p>We aimed to describe the outcomes of Omicron infection in kidney transplant recipients (KTR), compare the efficacy of the community therapeutic interventions and report the safety profile of molnupiravir.</jats:p><jats:p>From 142 KTRs diagnosed with COVID-19 infection after Omicron had become the dominant variant in the UK, 116 (78.9%) cases were diagnosed in the community; 47 receiving sotrovimab, 21 molnupiravir and 48 no treatment. 10 (20.8%) non-treated patients were hospitalised following infection, which was significantly higher than the sotrovimab group (2.1%), p=0.0048, but not the molnupiravir treated group (14.3%), p=0.47. The only admission following sotrovimab occurred in a patient infected with BA.2. One patient from the molnupiravir and no-treatment groups required ICU support, and both subsequently died, with one other death in the no-treatment group. No patient receiving sotrovimab died. 6/116 (5.2%) patients required dialysis following their diagnosis; 2 (9.5%) patients receiving molnupiravir and 4 (8.3%) no-treatment. This requirement was significantly higher in the molnupiravir group compared with the sotrovimab treated patients, in whom no patient required dialysis, p=0.035. Both molnupiravir treated patients requiring dialysis had features of systemic thrombotic microangiopathy.</jats:p><jats:p>Post-vaccination serostatus was available in 110 patients. Seropositive patients were less likely to require hospital admission compared with seronegative patients, 6 (7.0%) and 6 (25.0%) respectively, p=0.023. Seropositive patients were also less likely to require dialysis therapy, p=0.016.</jats:p><jats:p>In conclusion, sotrovimab treatment in the community was associated with superior patient and transplant outcomes; it’s clinical efficacy against the BA.2 variant requires a rapid review. The treatment benefit of molnupiravir was not evident, and wider safety reporting in transplant patients is needed.</jats:p>",
"accepted": {
"date-parts": [
[
2022,
5,
3
]
]
},
"author": [
{
"ORCID": "http://orcid.org/0000-0001-5163-161X",
"affiliation": [],
"authenticated-orcid": false,
"family": "Gleeson",
"given": "Sarah",
"sequence": "first"
},
{
"affiliation": [],
"family": "Martin",
"given": "Paul",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Thomson",
"given": "Tina",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Thind",
"given": "Amarpreet",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Prendecki",
"given": "Maria",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Spensley",
"given": "Katrina J.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Clarke",
"given": "Candice L.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Roufosse",
"given": "Candice",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Pickard",
"given": "Graham",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Thomas",
"given": "David",
"sequence": "additional"
},
{
"affiliation": [],
"family": "McAdoo",
"given": "Stephen P.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Lightstone",
"given": "Liz",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Kelleher",
"given": "Peter",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Willicombe",
"given": "Michelle",
"sequence": "additional"
}
],
"container-title": [],
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2022,
5,
4
]
],
"date-time": "2022-05-04T00:00:13Z",
"timestamp": 1651622413000
},
"deposited": {
"date-parts": [
[
2022,
5,
5
]
],
"date-time": "2022-05-05T09:30:26Z",
"timestamp": 1651743026000
},
"group-title": "Nephrology",
"indexed": {
"date-parts": [
[
2024,
8,
23
]
],
"date-time": "2024-08-23T21:50:00Z",
"timestamp": 1724449800106
},
"institution": [
{
"name": "medRxiv"
}
],
"is-referenced-by-count": 11,
"issued": {
"date-parts": [
[
2022,
5,
3
]
]
},
"link": [
{
"URL": "https://syndication.highwire.org/content/doi/10.1101/2022.05.03.22274524",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "246",
"original-title": [],
"posted": {
"date-parts": [
[
2022,
5,
3
]
]
},
"prefix": "10.1101",
"published": {
"date-parts": [
[
2022,
5,
3
]
]
},
"publisher": "Cold Spring Harbor Laboratory",
"reference": [
{
"DOI": "10.1016/j.kint.2022.04.003",
"doi-asserted-by": "crossref",
"key": "2022050502301158000_2022.05.03.22274524v1.1",
"unstructured": "Chavarot, N. , et al. Early treatment with sotrovimab monoclonal antibody in kidney transplant recipients with Omicron infection. Kidney international (2022)."
},
{
"DOI": "10.1097/TP.0000000000004126",
"doi-asserted-by": "publisher",
"key": "2022050502301158000_2022.05.03.22274524v1.2"
},
{
"DOI": "10.1016/s0140-6736(21)02096-1",
"doi-asserted-by": "publisher",
"key": "2022050502301158000_2022.05.03.22274524v1.3"
},
{
"DOI": "10.1097/TP.0000000000004059",
"article-title": "Real-world Effectiveness of the Pfizer-BioNTech BNT162b2 and Oxford-AstraZeneca ChAdOx1-S Vaccines Against SARS-CoV-2 in Solid Organ and Islet Transplant Recipients",
"doi-asserted-by": "crossref",
"first-page": "436",
"journal-title": "Transplantation",
"key": "2022050502301158000_2022.05.03.22274524v1.4",
"volume": "106",
"year": "2022"
},
{
"key": "2022050502301158000_2022.05.03.22274524v1.5",
"unstructured": "Antivirals or neutralising monoclonal antibodies (nMABs) for non-hospitalised patients with COVID-19."
},
{
"DOI": "10.1056/NEJMoa2107934",
"article-title": "Early Treatment for Covid-19 with SARS-CoV-2 Neutralizing Antibody Sotrovimab",
"doi-asserted-by": "crossref",
"first-page": "1941",
"journal-title": "N Engl J Med",
"key": "2022050502301158000_2022.05.03.22274524v1.6",
"volume": "385",
"year": "2021"
},
{
"DOI": "10.1056/NEJMoa2116044",
"article-title": "Molnupiravir for Oral Treatment of Covid-19 in Nonhospitalized Patients",
"doi-asserted-by": "crossref",
"first-page": "509",
"journal-title": "N Engl J Med",
"key": "2022050502301158000_2022.05.03.22274524v1.7",
"volume": "386",
"year": "2022"
},
{
"key": "2022050502301158000_2022.05.03.22274524v1.8",
"unstructured": "Lageviro Summary of Product Characteristics."
},
{
"DOI": "10.1136/bmj.o926",
"doi-asserted-by": "publisher",
"key": "2022050502301158000_2022.05.03.22274524v1.9"
},
{
"DOI": "10.1111/his.13855",
"article-title": "Clinical-pathological correlations in post-transplant thrombotic microangiopathy",
"doi-asserted-by": "crossref",
"first-page": "88",
"journal-title": "Histopathology",
"key": "2022050502301158000_2022.05.03.22274524v1.10",
"volume": "75",
"year": "2019"
},
{
"DOI": "10.1038/s41586-021-03291-y",
"article-title": "SARS-CoV-2 evolution during treatment of chronic infection",
"doi-asserted-by": "crossref",
"first-page": "277",
"journal-title": "Nature",
"key": "2022050502301158000_2022.05.03.22274524v1.11",
"volume": "592",
"year": "2021"
},
{
"DOI": "10.1038/s41586-022-04594-4",
"article-title": "Antibody evasion properties of SARS-CoV-2 Omicron sublineages",
"doi-asserted-by": "crossref",
"first-page": "553",
"journal-title": "Nature",
"key": "2022050502301158000_2022.05.03.22274524v1.12",
"volume": "604",
"year": "2022"
},
{
"DOI": "10.1101/2022.03.21.22272669",
"doi-asserted-by": "crossref",
"key": "2022050502301158000_2022.05.03.22274524v1.13",
"unstructured": "Benotmane, I. , et al. Pre-exposure prophylaxis with Evusheld™ elicits limited neutralizing activity against the omicron variant in kidney transplant patients. medRxiv, 2022.2003.2021.22272669 (2022)."
},
{
"DOI": "10.1136/bmj.o966",
"doi-asserted-by": "publisher",
"key": "2022050502301158000_2022.05.03.22274524v1.14"
}
],
"reference-count": 14,
"references-count": 14,
"relation": {},
"resource": {
"primary": {
"URL": "http://medrxiv.org/lookup/doi/10.1101/2022.05.03.22274524"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"subtype": "preprint",
"title": "Kidney Transplant Recipients and Omicron: Outcomes, effect of vaccines and the efficacy and safety of novel treatments",
"type": "posted-content"
}
gleeson
