Early Outpatient Treatment of COVID-19: A Retrospective Analysis of 392 Cases in Italy
et al., Journal of Clinical Medicine, doi:10.3390/jcm11206138, Oct 2022
Retrospective 392 outpatients in Italy showing 0.2% mortality with early treatment, compared with >3% in Italy at the time. Treatment varied for individual patients and included HCQ, vitamin D, vitamin C, vitamin A, zinc, quercetin, bromhexine, aspirin, and azithromycin.
Bromhexine efficacy may vary depending on the degree of TMPRSS-dependent fusion for different variants1,2.
Cosentino et al., 18 Oct 2022, retrospective, Italy, peer-reviewed, mean age 48.5, 12 authors, study period 1 November, 2020 - 31 March, 2021.
Contact: marco.cosentino@uninsubria.it (corresponding author), info@ippocrateorg.org.
Early Outpatient Treatment of COVID-19: A Retrospective Analysis of 392 Cases in Italy
Journal of Clinical Medicine, doi:10.3390/jcm11206138
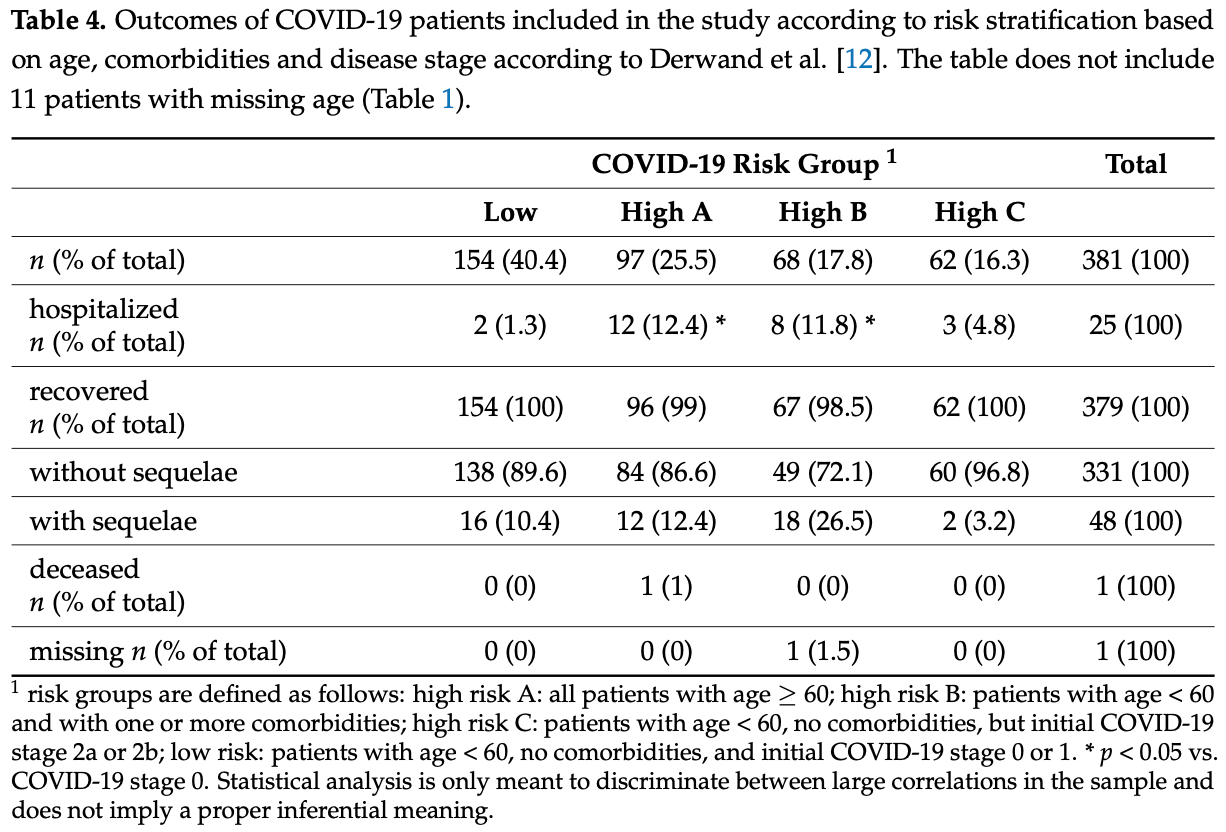
COVID-19 was declared a pandemic in March 2020. The knowledge of COVID-19 pathophysiology soon provided a strong rationale for the early use of both anti-inflammatory and antithrombotic drugs; however, its evidence was slowly and partially incorporated into institutional guidelines. The unmet needs of COVID-19 outpatients were taken care of by networks of physicians and researchers. We analyse the characteristics, management and outcomes in COVID-19 outpatients who were taken care of by physicians within the IppocrateOrg Association. In this observational retrospective study, volunteering doctors provided data on 392 COVID-19 patients. The mean age of patients was 48.5 years (range: 0.5-97), and patients were taken care of in COVID-19 stage 0 (15.6%), stage 1 (50.0%), stage 2a (28.8%) and stage 2b (5.6%). Many patients were overweight (26%) or obese (11.5%), with chronic comorbidities (34.9%), mainly cardiovascular (23%) and metabolic (13.3%). The most frequently prescribed drugs included: vitamins and supplements (98.7%), aspirin (66.1%), antibiotics (62%), glucocorticoids (41.8%), hydroxychloroquine (29.6%), enoxaparin (28.6%), colchicine (8.9%), oxygen therapy (6.9%), and ivermectin (2.8%). Hospitalization occurred in 5.8% of cases, mainly in stage 2b (27.3%). A total of 390 patients (99.6%) recovered; one patient was lost at follow up, and one patient died after hospitalization. This is the first real-world study describing the behaviours of physicians caring for COVID-19 outpatients, and the outcomes of COVID-19 early treatment. The lethality in this cohort was 0.2%, while overall, and over the same period, the COVID-19 lethality in Italy was over 3%. The drug use described in this study appears effective and safe. The present evidence should be carefully considered by physicians and political decision makers.
Supplementary Materials: The following supporting information can be downloaded at: https: //www.mdpi.com/article/10.3390/jcm11206138/s1, Table S1 : Vitamins and supplements recommended in COVID-19 phase 0 (asymptomatic with positive swab) . Table S2 . Drugs recommended in COVID-19 phase 1 (symptomatic without signs of lung disease) [62] [63] [64] [65] [66] [67] [68] [69] [70] [71] [72] [73] [74] [75] . Table S3 . Drugs recommended in COVID-19 phase 2a (symptomatic with lung disease) [76] [77] [78] [79] . Supplementary Table S4 . Drugs recommended in COVID-19 phase 2b (symptomatic with lung disease and desaturation) [76, 77, 80] . Supplementary Material: Questionnaire for Physicians, Supplementary Data: Raw Data. Author Contributions: Concept and design: M.C., V.V. and M.R. Data acquisition: B.A., M.A.B., F.B., A.D., C.S.F.P. and A.P. Data analysis and interpretation: V.V., M.C., S.M. and F.M. Manuscript drafting: M.C. Critical manuscript revision for important intellectual content: all authors. Statistical analysis: M.C. and S.M. Administrative, technical or material support: V.V. Collected data was provided by participating physicians to the IppocrateOrg Association and was routinely collected during their professional activity. Each physician is responsible for the integrity of data s/he provided. M.C., V.V., S.M. and F.M. had full access to anonymized data in the study and take responsibility for the integrity of data records and accuracy of data analysis. All..
References
Adhikari, Marasini, Rayamajhee, Bhattarai, Lamichhane et al., Potential Roles of Medicinal Plants for the Treatment of Viral Diseases Focusing on COVID-19: A Review, Phytother. Res, doi:10.1002/ptr.6893
Aigner, Pietrantonio, Bessa De Sousa, Michael, Schuster et al., The Leukotriene Receptor Antagonist Montelukast as a Potential COVID-19 Therapeutic, Front. Mol. Biosci
Alexaki, Henneicke, The Role of Glucocorticoids in the Management of COVID-19, Horm. Metab. Res
Alliance, I-MASK+-Prevention & Early Outpatient Treatment Protocol for COVID-19, Version
Bae, Kim, Mini-Review on the Roles of Vitamin C, Vitamin D, and Selenium in the Immune System against COVID-19, Molecules, doi:10.3390/molecules25225346
Bellavite, Donzelli, Hesperidin and SARS-CoV-2: New Light on the Healthy Function of Citrus Fruits, Antioxidants, doi:10.3390/antiox9080742
Biancatelli, Berrill, Catravas, Marik, Quercetin, Vitamin C: An Experimental, Synergistic Therapy for the Prevention and Treatment of SARS-CoV-2 Related Disease (COVID-19), Front. Immunol, doi:10.3389/fimmu.2020.01451
Bianconi, Violi, Fallarino, Pignatelli, Sahebkar et al., Is Acetylsalicylic Acid a Safe and Potentially Useful Choice for Adult Patients with COVID-19?, Drugs, doi:10.1007/s40265-020-01365-1
Brendler, Al-Harrasi, Bauer, Gafner, Hardy et al., Botanical Drugs and Supplements Affecting the Immune Response in the Time of COVID-19: Implications for Research and Clinical Practice, Phytother. Res, doi:10.1002/ptr.7008
Cacciapuoti, Cacciapuoti, Could Low Doses Acetylsalicylic Acid Prevent Thrombotic Complications in COVID-19 Patients?, Clin. Appl. Thromb. Hemost, doi:10.1177/10760296211014592
Carrouel, Gonçalves, Conte, Campus, Fisher et al., Antiviral Activity of Reagents in Mouth Rinses against SARS-CoV-2, J. Dent. Res, doi:10.1177/0022034520967933
Carsana, Sonzogni, Nasr, Rossi, Pellegrinelli et al., Pulmonary Post-Mortem Findings in a Series of COVID-19 Cases from Northern Italy: A Two-Centre Descriptive Study, Lancet Infect. Dis
Chang, Ng, Sun, Lactoferrin as Potential Preventative and Adjunct Treatment for COVID-19, Int. J. Antimicrob. Agents, doi:10.1016/j.ijantimicag.2020.106118
Clemency, Varughese, Gonzalez-Rojas, Morse, Phipatanakul et al., Efficacy of Inhaled Ciclesonide for Outpatient Treatment of Adolescents and Adults With Symptomatic COVID-19: A Randomized Clinical Trial, JAMA Intern. Med
Connors, Brooks, Sciurba, Krishnan, Bledsoe et al., Effect of Antithrombotic Therapy on Clinical Outcomes in Outpatients With Clinically Stable Symptomatic COVID-19: The ACTIV-4B Randomized Clinical Trial, JAMA, doi:10.1001/jama.2021.17272
Cordon-Cardo, Pujadas, Wajnberg, Sebra, Patel et al., COVID-19: Staging of a New Disease, Cancer Cell
Depfenhart, De Villiers, Lemperle, Meyer, Di Somma, Potential New Treatment Strategies for COVID-19: Is There a Role for Bromhexine as Add-on Therapy?, Intern. Emerg. Med, doi:10.1007/s11739-020-02383-3
Derosa, Maffioli, D'angelo, Di Pierro, A Role for Quercetin in Coronavirus Disease 2019 (COVID-19), Phytother. Res, doi:10.1002/ptr.6887
Derwand, Scholz, Zelenko, COVID-19 outpatients: Early risk-stratified treatment with zinc plus low-dose hydroxychloroquine and azithromycin: A retrospective case series study, Int. J. Antimicrob. Agents, doi:10.1016/j.ijantimicag.2020.106214
Drago, Gozzo, Li, Stella, Cosmi, Use of Enoxaparin to Counteract COVID-19 Infection and Reduce Thromboembolic Venous Complications: A Review of the Current Evidence, Front. Pharmacol, doi:10.3389/fphar.2020.579886
Echeverría-Esnal, Martin-Ontiyuelo, Navarrete-Rouco, De-Antonio Cuscó, Ferrández et al., Azithromycin in the Treatment of COVID-19: A Review, Expert Rev. Anti. Infect. Ther, doi:10.1080/14787210.2020.1813024
Ezer, Belga, Daneman, Chan, Smith et al., Inhaled and intranasal ciclesonide for the treatment of covid-19 in adult outpatients: CONTAIN phase II randomised controlled trial, BMJ
Fabiani, Onder, Boros, Spuri, Minelli et al., Il case fatality rate dell'infezione SARS-CoV-2 a livello regionale e attraverso le differenti fasi dell'epidemia in Italia. Versione del 20 gennaio 2021, Ist. Super. Sanità
Fazio, Bellavite, Zanolin, Mccullough, Pandolfi et al., Retrospective Study of Outcomes and Hospitalization Rates of Patients in Italy with a Confirmed Diagnosis of Early COVID-19 and Treated at Home within 3 Days or after 3 Days of Symptom Onset with Prescribed and Non-Prescribed Treatments Between November 2020 and, Med. Sci. Monit
Feld, Kandel, Biondi, Kozak, Zahoor et al., Peginterferon lambda for the treatment of outpatients with COVID-19: A phase 2, placebo-controlled randomised trial, Lancet Respir. Med
Filardo, Di Pietro, Mastromarino, Sessa, Therapeutic Potential of Resveratrol against Emerging Respiratory Viral Infections, Pharmacol. Ther, doi:10.1016/j.pharmthera.2020.107613
For, Real-Time Analysis of All 315 Studies
Frohman, Outpatient COVID-19 Treatment to Prevent Severe Disease
Grant, Lahore, Mcdonnell, Baggerly, French et al., Evidence That Vitamin D Supplementation Could Reduce Risk of Influenza and COVID-19 Infections and Deaths, Nutrients, doi:10.3390/nu12040988
Gupta, Gonzalez-Rojas, Juarez, Crespo Casal, Moya et al., Early Treatment for COVID-19 with SARS-CoV-2 Neutralizing Antibody Sotrovimab, N. Engl. J. Med, doi:10.1056/NEJMoa2107934
Guzman-Esquivel, Galvan-Salazar, Guzman-Solorzano, Cuevas-Velazquez, Guzman-Solorzano et al., Efficacy of the Use of Mefenamic Acid Combined with Standard Medical Care vs. Standard Medical Care Alone for the Treatment of COVID-19: A Randomized Double-Blind Placebo-Controlled Trial, J. Mol. Med
Hinks, Cureton, Knight, Wang, Cane et al., Azithromycin versus standard care in patients with mild-to-moderate COVID-19 (ATOMIC2): An open-label, randomised trial, Lancet Respir. Med
Holford, Carr, Jovic, Ali, Whitaker et al., Vitamin C-An Adjunctive Therapy for Respiratory Infection, Sepsis and COVID-19, Nutrients, doi:10.3390/nu12123760
Kiani, Dhuli, Anpilogov, Bressan, Dautaj et al., Natural Compounds as Inhibitors of SARS-CoV-2 Endocytosis: A Promising Approach against COVID-19, Acta Biomed
Korley, Durkalski-Mauldin, Yeatts, Schulman, Davenport et al., Early Convalescent Plasma for High-Risk Outpatients with Covid-19, N. Engl. J. Med
Kory, Meduri, Varon, Iglesias, Marik, Review of the Emerging Evidence Demonstrating the Efficacy of Ivermectin in the Prophylaxis and Treatment of COVID-19, Am. J. Ther, doi:10.1097/MJT.0000000000001377
Marik, Kory, Ivermectin, A Reanalysis of the Data, Am. J. Ther, doi:10.1097/MJT.0000000000001443
Mccullough, Alexander, Armstrong, Arvinte, Bain et al., Multifaceted highly targeted sequential multidrug treatment of early ambulatory high-risk SARS-CoV-2 infection (COVID-19), Rev. Cardiovasc. Med
Mccullough, Kelly, Ruocco, Lerma, Tumlin et al., Pathophysiological Basis and Rationale for Early Outpatient Treatment of SARS-CoV-2 (COVID-19) Infection, Am. J. Med
Midha, Kumar, Kumar, Madan, Mega Doses of Retinol: A Possible Immunomodulation in Covid-19 Illness in Resource-Limited Settings, Rev. Med. Virol, doi:10.1002/rmv.2204
Million, Lagier, Tissot-Dupont, Ravaux, Dhiver et al., Early combination therapy with hydroxychloroquine and azithromycin reduces mortality in 10,429 COVID-19 outpatients, Rev. Cardiovasc. Med
Million, Roussel, Gautret, Raoult, Effect of Hydroxychloroquine and Azithromycin on SARS-CoV-2 Clearance in COVID-19 Patients, a Meta-Analysis, Int. J. Antimicrob. Agents, doi:10.1016/j.ijantimicag.2020.106240
Nina, Dash, Hydroxychloroquine as Prophylaxis or Treatment for COVID-19: What Does the Evidence Say?, Indian J. Public Health, doi:10.4103/ijph.IJPH_496_20
Ochoa, Raffetto, Hernández, Zavala, Gutiérrez et al., Sulodexide in the Treatment of Patients with Early Stages of COVID-19: A Randomized Controlled Trial, Thromb. Haemost, doi:10.1055/a-1414-5216
Oldenburg, Pinsky, Brogdon, Chen, Ruder et al., Effect of Oral Azithromycin vs Placebo on COVID-19 Symptoms in Outpatients with SARS-CoV-2 Infection: A Randomized Clinical Trial, JAMA
Ramakrishnan, Nicolau, Langford, Mahdi, Jeffers et al., Inhaled budesonide in the treatment of early COVID-19 (STOIC): A phase 2, open-label, randomised controlled trial, Lancet Respir. Med
Rango, Guarire Il COVID-19 a Casa: Manuale per Terapia Domiciliare Personalizzata, Independently published
Reis, Moreira Silva, Medeiros Silva, Thabane, Singh et al., Effect of Early Treatment With Hydroxychloroquine or Lopinavir and Ritonavir on Risk of Hospitalization Among Patients With COVID-19: The TOGETHER Randomized Clinical Trial, JAMA Netw. Open
Remuzzi, Remuzzi, COVID-19 and Italy: What Next?, Lancet
Reyes, Hu, Teperman, Wampler Muskardin, Tardif et al., Anti-Inflammatory Therapy for COVID-19 Infection: The Case for Colchicine, Ann. Rheum. Dis, doi:10.1136/annrheumdis-2020-219174
Rodrigues, Freitas-Santos, Levi, Senerchia, Lopes et al., Hydroxychloroquine plus azithromycin early treatment of mild COVID-19 in an outpatient setting: A randomized, double-blinded, placebo-controlled clinical trial evaluating viral clearance, Int. J. Antimicrob. Agents
Roozbeh, Saeedi, Alizadeh-Navaei, Hedayatizadeh-Omran, Merat et al., Sofosbuvir and daclatasvir for the treatment of COVID-19 outpatients: A double-blind, randomized controlled trial, J. Antimicrob. Chemother
Schwartz, Boesen, Cerchiaro, Doram, Edwards et al., Assessing the efficacy and safety of hydroxychloroquine as outpatient treatment of COVID-19: A randomized controlled trial, CMAJ Open
Shi, Puyo, N-Acetylcysteine to Combat COVID-19: An Evidence Review, Ther. Clin. Risk Manag
Siddiqi, Mehra, COVID-19 illness in native and immunosuppressed states: A clinical-therapeutic staging proposal, J. Heart Lung Transpl
Sinha, Balayla, Hydroxychloroquine and COVID-19, Postgrad. Med. J, doi:10.1136/postgradmedj-2020-137785
Skalny, Rink, Ajsuvakova, Aschner, Gritsenko et al., Zinc and Respiratory Tract Infections: Perspectives for COVID-19 (Review), Int. J. Mol. Med
Susen, Tacquard, Godon, Mansour, Garrigue et al., Prevention of Thrombotic Risk in Hospitalized Patients with COVID-19 and Hemostasis Monitoring, Crit. Care
Suter, Consolaro, Pedroni, Moroni, Pastò et al., A simple, home-therapy algorithm to prevent hospitalisation for COVID-19 patients: A retrospective observational matched-cohort study, eClinicalMedicine
Tardif, Bouabdallaoui, L'allier, Gaudet, Shah et al., Colchicine for community-treated patients with COVID-19 (COLCORONA): A phase 3, randomised, double-blinded, adaptive, placebo-controlled, multicentre trial, Lancet Respir. Med, doi:10.1016/S2213-2600(21)00222-8
Thomas, Patel, Bittel, Wolski, Wang et al., Effect of High-Dose Zinc and Ascorbic Acid Supplementation vs Usual Care on Symptom Length and Reduction Among Ambulatory Patients With SARS-CoV-2 Infection: The COVID A to Z Randomized Clinical Trial, JAMA Netw. Open
Trasino, A Role for Retinoids in the Treatment of COVID-19?, Clin. Exp. Pharmacol. Physiol, doi:10.1111/1440-1681.13354
Turk, Turk, Malkan, Haznedaroglu, Three Critical Clinicobiological Phases of the Human SARS-Associated Coronavirus Infections, Eur. Rev. Med. Pharm. Sci
Wang, Wang, Wang, Luo, Wan et al., Lactoferrin for the Treatment of COVID-19 (Review), Exp. Ther. Med, doi:10.3892/etm.2020.9402
Wessels, Rolles, Rink, The Potential Impact of Zinc Supplementation on COVID-19 Pathogenesis, Front. Immunol, doi:10.3389/fimmu.2020.01712
Xu, Baylink, Chen, Reeves, Xiao et al., The Importance of Vitamin d Metabolism as a Potential Prophylactic, Immunoregulatory and Neuroprotective Treatment for COVID-19, J. Transl. Med, doi:10.1186/s12967-020-02488-5
Yates, Newman, Oshry, Glassman, Leone et al., Doxycycline Treatment of High-Risk COVID-19-Positive Patients with Comorbid Pulmonary Disease, Ther. Adv. Respir. Dis, doi:10.1177/1753466620951053
Zhou, Yu, Du, Fan, Liu et al., Clinical Course and Risk Factors for Mortality of Adult Inpatients with COVID-19 in Wuhan, China: A Retrospective Cohort Study, Lancet
DOI record:
{
"DOI": "10.3390/jcm11206138",
"ISSN": [
"2077-0383"
],
"URL": "http://dx.doi.org/10.3390/jcm11206138",
"abstract": "<jats:p>COVID-19 was declared a pandemic in March 2020. The knowledge of COVID-19 pathophysiology soon provided a strong rationale for the early use of both anti-inflammatory and antithrombotic drugs; however, its evidence was slowly and partially incorporated into institutional guidelines. The unmet needs of COVID-19 outpatients were taken care of by networks of physicians and researchers. We analyse the characteristics, management and outcomes in COVID-19 outpatients who were taken care of by physicians within the IppocrateOrg Association. In this observational retrospective study, volunteering doctors provided data on 392 COVID-19 patients. The mean age of patients was 48.5 years (range: 0.5–97), and patients were taken care of in COVID-19 stage 0 (15.6%), stage 1 (50.0%), stage 2a (28.8%) and stage 2b (5.6%). Many patients were overweight (26%) or obese (11.5%), with chronic comorbidities (34.9%), mainly cardiovascular (23%) and metabolic (13.3%). The most frequently prescribed drugs included: vitamins and supplements (98.7%), aspirin (66.1%), antibiotics (62%), glucocorticoids (41.8%), hydroxychloroquine (29.6%), enoxaparin (28.6%), colchicine (8.9%), oxygen therapy (6.9%), and ivermectin (2.8%). Hospitalization occurred in 5.8% of cases, mainly in stage 2b (27.3%). A total of 390 patients (99.6%) recovered; one patient was lost at follow up, and one patient died after hospitalization. This is the first real-world study describing the behaviours of physicians caring for COVID-19 outpatients, and the outcomes of COVID-19 early treatment. The lethality in this cohort was 0.2%, while overall, and over the same period, the COVID-19 lethality in Italy was over 3%. The drug use described in this study appears effective and safe. The present evidence should be carefully considered by physicians and political decision makers.</jats:p>",
"alternative-id": [
"jcm11206138"
],
"author": [
{
"ORCID": "http://orcid.org/0000-0002-6978-7775",
"affiliation": [],
"authenticated-orcid": false,
"family": "Cosentino",
"given": "Marco",
"sequence": "first"
},
{
"affiliation": [],
"family": "Vernocchi",
"given": "Veronica",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-2519-9138",
"affiliation": [],
"authenticated-orcid": false,
"family": "Martini",
"given": "Stefano",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Marino",
"given": "Franca",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Allasino",
"given": "Barbara",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Bàlzola",
"given": "Maria Antonietta",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Burigana",
"given": "Fabio",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Dallari",
"given": "Alberto",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Pagano",
"given": "Carlo Servo Florio",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Palma",
"given": "Antonio",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Rango",
"given": "Mauro",
"sequence": "additional"
},
{
"affiliation": [],
"name": "on behalf of IppocrateOrg Association Working Group for the Early Outpatient Treatment of COVID-19",
"sequence": "additional"
}
],
"container-title": "Journal of Clinical Medicine",
"container-title-short": "JCM",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2022,
10,
19
]
],
"date-time": "2022-10-19T04:58:51Z",
"timestamp": 1666155531000
},
"deposited": {
"date-parts": [
[
2022,
10,
19
]
],
"date-time": "2022-10-19T05:08:39Z",
"timestamp": 1666156119000
},
"indexed": {
"date-parts": [
[
2022,
12,
9
]
],
"date-time": "2022-12-09T02:09:49Z",
"timestamp": 1670551789401
},
"is-referenced-by-count": 1,
"issue": "20",
"issued": {
"date-parts": [
[
2022,
10,
18
]
]
},
"journal-issue": {
"issue": "20",
"published-online": {
"date-parts": [
[
2022,
10
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
10,
18
]
],
"date-time": "2022-10-18T00:00:00Z",
"timestamp": 1666051200000
}
}
],
"link": [
{
"URL": "https://www.mdpi.com/2077-0383/11/20/6138/pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1968",
"original-title": [],
"page": "6138",
"prefix": "10.3390",
"published": {
"date-parts": [
[
2022,
10,
18
]
]
},
"published-online": {
"date-parts": [
[
2022,
10,
18
]
]
},
"publisher": "MDPI AG",
"reference": [
{
"DOI": "10.1016/S0140-6736(20)30566-3",
"doi-asserted-by": "publisher",
"key": "ref1"
},
{
"key": "ref2",
"unstructured": "World Health Organization WHO Announces COVID-19 Outbreak a Pandemic\nhttps://www.euro.who.int/en/health-topics/health-emergencies/coronavirus-covid-19/news/news/2020/3/who-announces-covid-19-outbreak-a-pandemic"
},
{
"DOI": "10.1016/S0140-6736(20)30627-9",
"article-title": "COVID-19 and Italy: What Next?",
"author": "Remuzzi",
"doi-asserted-by": "crossref",
"first-page": "1225",
"journal-title": "Lancet",
"key": "ref3",
"volume": "395",
"year": "2020"
},
{
"article-title": "Ministero Della Salute CIRCOLARE Del 08/04/2020 Indicazioni Emergenziali Connesse Ad Epidemia COVID-19 Riguardanti Il Settore Funebre, Cimiteriale e Di Cremazione",
"key": "ref4"
},
{
"DOI": "10.1016/S1473-3099(20)30434-5",
"article-title": "Pulmonary Post-Mortem Findings in a Series of COVID-19 Cases from Northern Italy: A Two-Centre Descriptive Study",
"author": "Carsana",
"doi-asserted-by": "crossref",
"first-page": "1135",
"journal-title": "Lancet Infect. Dis.",
"key": "ref5",
"volume": "20",
"year": "2020"
},
{
"article-title": "Gestione Domiciliare Dei Pazienti Con Infezione Da SARS-CoV2 Aggiornata al 26 Aprile 2021",
"author": "Ministero della Salute CIRCOLARE Del 26/04/2021",
"key": "ref6"
},
{
"article-title": "AIFA Idrossiclorochina Nella Terapia dei Pazienti Adulti con COVID-19—Update del 22 Luglio 2020",
"key": "ref7"
},
{
"DOI": "10.1016/j.healun.2020.03.012",
"article-title": "COVID-19 illness in native and immunosuppressed states: A clinical–therapeutic staging proposal",
"author": "Siddiqi",
"doi-asserted-by": "crossref",
"first-page": "405",
"journal-title": "J. Heart Lung Transpl.",
"key": "ref8",
"volume": "39",
"year": "2020"
},
{
"article-title": "Three Critical Clinicobiological Phases of the Human SARS-Associated Coronavirus Infections",
"author": "Turk",
"first-page": "8606",
"journal-title": "Eur. Rev. Med. Pharm. Sci.",
"key": "ref9",
"volume": "24",
"year": "2020"
},
{
"DOI": "10.1016/j.ccell.2020.10.006",
"article-title": "COVID-19: Staging of a New Disease",
"author": "Cordon-Cardo",
"doi-asserted-by": "crossref",
"first-page": "594",
"journal-title": "Cancer Cell",
"key": "ref10",
"volume": "38",
"year": "2020"
},
{
"author": "Rango",
"key": "ref11",
"series-title": "Guarire Il COVID-19 a Casa: Manuale per Terapia Domiciliare Personalizzata",
"year": "2021"
},
{
"DOI": "10.1016/j.ijantimicag.2020.106214",
"doi-asserted-by": "publisher",
"key": "ref12"
},
{
"DOI": "10.31083/j.rcm.2020.04.264",
"article-title": "Multifaceted highly targeted sequential multidrug treatment of early ambulatory high-risk SARS-CoV-2 infection (COVID-19)",
"author": "McCullough",
"doi-asserted-by": "crossref",
"first-page": "517",
"journal-title": "Rev. Cardiovasc. Med.",
"key": "ref13",
"volume": "21",
"year": "2020"
},
{
"DOI": "10.9778/cmajo.20210069",
"article-title": "Assessing the efficacy and safety of hydroxychloroquine as outpatient treatment of COVID-19: A randomized controlled trial",
"author": "Schwartz",
"doi-asserted-by": "crossref",
"first-page": "E693",
"journal-title": "CMAJ Open",
"key": "ref14",
"volume": "9",
"year": "2021"
},
{
"DOI": "10.1001/jamanetworkopen.2021.6468",
"article-title": "Effect of Early Treatment With Hydroxychloroquine or Lopinavir and Ritonavir on Risk of Hospitalization Among Patients With COVID-19: The TOGETHER Randomized Clinical Trial",
"author": "Reis",
"doi-asserted-by": "crossref",
"first-page": "e216468",
"journal-title": "JAMA Netw. Open",
"key": "ref15",
"volume": "4",
"year": "2021"
},
{
"DOI": "10.1016/S2213-2600(21)00222-8",
"doi-asserted-by": "publisher",
"key": "ref16"
},
{
"DOI": "10.1001/jama.2021.11517",
"article-title": "Effect of Oral Azithromycin vs Placebo on COVID-19 Symptoms in Outpatients with SARS-CoV-2 Infection: A Randomized Clinical Trial",
"author": "Oldenburg",
"doi-asserted-by": "crossref",
"first-page": "490",
"journal-title": "JAMA",
"key": "ref17",
"volume": "326",
"year": "2021"
},
{
"DOI": "10.1016/S2213-2600(21)00263-0",
"article-title": "Azithromycin versus standard care in patients with mild-to-moderate COVID-19 (ATOMIC2): An open-label, randomised trial",
"author": "Hinks",
"doi-asserted-by": "crossref",
"first-page": "1130",
"journal-title": "Lancet Respir. Med.",
"key": "ref18",
"volume": "9",
"year": "2021"
},
{
"article-title": "Efficacy of the Use of Mefenamic Acid Combined with Standard Medical Care vs. Standard Medical Care Alone for the Treatment of COVID-19: A Randomized Double-Blind Placebo-Controlled Trial",
"author": "Guzman-Esquivel",
"first-page": "1",
"journal-title": "J. Mol. Med.",
"key": "ref19",
"volume": "49",
"year": "2022"
},
{
"DOI": "10.1001/jamainternmed.2021.6759",
"article-title": "Efficacy of Inhaled Ciclesonide for Outpatient Treatment of Adolescents and Adults With Symptomatic COVID-19: A Randomized Clinical Trial",
"author": "Clemency",
"doi-asserted-by": "crossref",
"first-page": "42",
"journal-title": "JAMA Intern. Med.",
"key": "ref20",
"volume": "182",
"year": "2022"
},
{
"DOI": "10.1136/bmj-2021-068060",
"article-title": "Inhaled and intranasal ciclesonide for the treatment of covid-19 in adult outpatients: CONTAIN phase II randomised controlled trial",
"author": "Ezer",
"doi-asserted-by": "crossref",
"first-page": "e068060",
"journal-title": "BMJ",
"key": "ref21",
"volume": "375",
"year": "2021"
},
{
"DOI": "10.1016/S2213-2600(21)00160-0",
"article-title": "Inhaled budesonide in the treatment of early COVID-19 (STOIC): A phase 2, open-label, randomised controlled trial",
"author": "Ramakrishnan",
"doi-asserted-by": "crossref",
"first-page": "763",
"journal-title": "Lancet Respir. Med.",
"key": "ref22",
"volume": "9",
"year": "2021"
},
{
"DOI": "10.1093/jac/dkaa501",
"article-title": "Sofosbuvir and daclatasvir for the treatment of COVID-19 outpatients: A double-blind, randomized controlled trial",
"author": "Roozbeh",
"doi-asserted-by": "crossref",
"first-page": "753",
"journal-title": "J. Antimicrob. Chemother.",
"key": "ref23",
"volume": "76",
"year": "2020"
},
{
"DOI": "10.1001/jama.2021.17272",
"doi-asserted-by": "publisher",
"key": "ref24"
},
{
"DOI": "10.1056/NEJMoa2103784",
"doi-asserted-by": "publisher",
"key": "ref25"
},
{
"DOI": "10.1056/NEJMoa2107934",
"doi-asserted-by": "publisher",
"key": "ref26"
},
{
"DOI": "10.1016/S2213-2600(20)30566-X",
"article-title": "Peginterferon lambda for the treatment of outpatients with COVID-19: A phase 2, placebo-controlled randomised trial",
"author": "Feld",
"doi-asserted-by": "crossref",
"first-page": "498",
"journal-title": "Lancet Respir. Med.",
"key": "ref27",
"volume": "9",
"year": "2021"
},
{
"DOI": "10.1055/a-1414-5216",
"doi-asserted-by": "publisher",
"key": "ref28"
},
{
"DOI": "10.1001/jamanetworkopen.2021.0369",
"article-title": "Effect of High-Dose Zinc and Ascorbic Acid Supplementation vs Usual Care on Symptom Length and Reduction Among Ambulatory Patients With SARS-CoV-2 Infection: The COVID A to Z Randomized Clinical Trial",
"author": "Thomas",
"doi-asserted-by": "crossref",
"first-page": "e210369",
"journal-title": "JAMA Netw. Open",
"key": "ref29",
"volume": "4",
"year": "2021"
},
{
"DOI": "10.1016/j.ijantimicag.2021.106428",
"article-title": "Hydroxychloroquine plus azithromycin early treatment of mild COVID-19 in an outpatient setting: A randomized, double-blinded, placebo-controlled clinical trial evaluating viral clearance",
"author": "Rodrigues",
"doi-asserted-by": "crossref",
"first-page": "106428",
"journal-title": "Int. J. Antimicrob. Agents",
"key": "ref30",
"volume": "58",
"year": "2021"
},
{
"DOI": "10.12659/MSM.935379",
"article-title": "Retrospective Study of Outcomes and Hospitalization Rates of Patients in Italy with a Confirmed Diagnosis of Early COVID-19 and Treated at Home within 3 Days or after 3 Days of Symptom Onset with Prescribed and Non-Prescribed Treatments Between November 2020 and August 2021",
"author": "Fazio",
"doi-asserted-by": "crossref",
"first-page": "e935379",
"journal-title": "Med. Sci. Monit.",
"key": "ref31",
"volume": "28",
"year": "2021"
},
{
"DOI": "10.1016/j.eclinm.2021.100941",
"article-title": "A simple, home-therapy algorithm to prevent hospitalisation for COVID-19 patients: A retrospective observational matched-cohort study",
"author": "Suter",
"doi-asserted-by": "crossref",
"first-page": "100941",
"journal-title": "eClinicalMedicine",
"key": "ref32",
"volume": "37",
"year": "2021"
},
{
"DOI": "10.1016/j.amjmed.2020.07.003",
"article-title": "Pathophysiological Basis and Rationale for Early Outpatient Treatment of SARS-CoV-2 (COVID-19) Infection",
"author": "McCullough",
"doi-asserted-by": "crossref",
"first-page": "16",
"journal-title": "Am. J. Med.",
"key": "ref33",
"volume": "134",
"year": "2021"
},
{
"article-title": "I-MASK+—Prevention & Early Outpatient Treatment Protocol for COVID-19",
"author": "Alliance",
"first-page": "1",
"journal-title": "Version",
"key": "ref34",
"volume": "19",
"year": "2022"
},
{
"key": "ref35",
"unstructured": "Outpatient COVID-19 Treatment to Prevent Severe Disease\nhttps://thefrohmanfoundation.org/research/covid-19-treatment/outpatient-covid-19-treatment-to-prevent-severe-disease/"
},
{
"article-title": "Il case fatality rate dell’infezione SARS-CoV-2 a livello regionale e attraverso le differenti fasi dell’epidemia in Italia. Versione del 20 gennaio 2021",
"author": "Fabiani",
"first-page": "15",
"journal-title": "Ist. Super. Sanità",
"key": "ref36",
"volume": "51",
"year": "2021"
},
{
"key": "ref37",
"unstructured": "Aggiornamento Nazionale: 28 Aprile 2021\nhttps://www.epicentro.iss.it/coronavirus/bollettino/Bollettino-sorveglianza-integrata-COVID-19_28-aprile-2021.pdf"
},
{
"DOI": "10.31083/j.rcm2203116",
"article-title": "Early combination therapy with hydroxychloroquine and azithromycin reduces mortality in 10,429 COVID-19 outpatients",
"author": "Million",
"doi-asserted-by": "crossref",
"first-page": "1063",
"journal-title": "Rev. Cardiovasc. Med.",
"key": "ref38",
"volume": "22",
"year": "2021"
},
{
"DOI": "10.3390/molecules25225346",
"doi-asserted-by": "publisher",
"key": "ref39"
},
{
"DOI": "10.3390/nu12040988",
"doi-asserted-by": "publisher",
"key": "ref40"
},
{
"DOI": "10.1186/s12967-020-02488-5",
"doi-asserted-by": "publisher",
"key": "ref41"
},
{
"key": "ref42",
"unstructured": "Vitamin D for COVID-19: Real-Time Analysis of All 315 Studies\nhttps://c19vitamind.com/"
},
{
"DOI": "10.3390/nu12123760",
"doi-asserted-by": "publisher",
"key": "ref43"
},
{
"DOI": "10.3389/fimmu.2020.01451",
"doi-asserted-by": "publisher",
"key": "ref44"
},
{
"key": "ref45",
"unstructured": "Vitamin C for COVID-19: Real-Time Analysis of All 86 Studies\nhttps://c19early.com/"
},
{
"DOI": "10.3389/fimmu.2020.01712",
"doi-asserted-by": "publisher",
"key": "ref46"
},
{
"DOI": "10.3892/ijmm.2020.4575",
"doi-asserted-by": "publisher",
"key": "ref47"
},
{
"key": "ref48",
"unstructured": "Zinc for COVID-19: Real-Time Analysis of All 90 Studies\nhttps://c19zinc.com/"
},
{
"DOI": "10.3390/antiox9080742",
"doi-asserted-by": "publisher",
"key": "ref49"
},
{
"DOI": "10.1002/ptr.6893",
"doi-asserted-by": "publisher",
"key": "ref50"
},
{
"DOI": "10.1002/ptr.6887",
"doi-asserted-by": "publisher",
"key": "ref51"
},
{
"key": "ref52",
"unstructured": "Quercetin for COVID-19: Real-Time Analysis of All 22 Studies\nhttps://c19quercetin.com/"
},
{
"DOI": "10.3892/etm.2020.9402",
"doi-asserted-by": "publisher",
"key": "ref53"
},
{
"DOI": "10.1016/j.ijantimicag.2020.106118",
"doi-asserted-by": "publisher",
"key": "ref54"
},
{
"DOI": "10.1007/s11739-020-02383-3",
"doi-asserted-by": "publisher",
"key": "ref55"
},
{
"DOI": "10.1002/ptr.7008",
"doi-asserted-by": "publisher",
"key": "ref56"
},
{
"DOI": "10.23750/abm.v91i13-S.10520",
"doi-asserted-by": "publisher",
"key": "ref57"
},
{
"DOI": "10.1177/0022034520967933",
"doi-asserted-by": "publisher",
"key": "ref58"
},
{
"DOI": "10.1111/1440-1681.13354",
"doi-asserted-by": "publisher",
"key": "ref59"
},
{
"DOI": "10.1002/rmv.2204",
"doi-asserted-by": "publisher",
"key": "ref60"
},
{
"DOI": "10.1016/j.pharmthera.2020.107613",
"doi-asserted-by": "publisher",
"key": "ref61"
},
{
"DOI": "10.1007/s40265-020-01365-1",
"doi-asserted-by": "publisher",
"key": "ref62"
},
{
"DOI": "10.1177/10760296211014592",
"doi-asserted-by": "publisher",
"key": "ref63"
},
{
"key": "ref64",
"unstructured": "Aspirin for COVID-19: Real-Time Analysis of All 61 Studies\nhttps://c19aspirin.com/"
},
{
"DOI": "10.1097/MJT.0000000000001377",
"doi-asserted-by": "publisher",
"key": "ref65"
},
{
"DOI": "10.1097/MJT.0000000000001443",
"doi-asserted-by": "publisher",
"key": "ref66"
},
{
"key": "ref67",
"unstructured": "Ivermectin for COVID-19: Real-Time Analysis of All 185 Studies\nhttps://c19ivermectin.com/"
},
{
"DOI": "10.1016/j.ijantimicag.2020.106240",
"doi-asserted-by": "publisher",
"key": "ref68"
},
{
"DOI": "10.4103/ijph.IJPH_496_20",
"doi-asserted-by": "publisher",
"key": "ref69"
},
{
"DOI": "10.1136/postgradmedj-2020-137785",
"doi-asserted-by": "publisher",
"key": "ref70"
},
{
"key": "ref71",
"unstructured": "HCQ for COVID-19: Real-Time Analysis of All 444 Studies\nhttps://c19hcq.com/"
},
{
"DOI": "10.1080/14787210.2020.1813024",
"doi-asserted-by": "publisher",
"key": "ref72"
},
{
"DOI": "10.1177/1753466620951053",
"doi-asserted-by": "publisher",
"key": "ref73"
},
{
"DOI": "10.1136/annrheumdis-2020-219174",
"doi-asserted-by": "publisher",
"key": "ref74"
},
{
"key": "ref75",
"unstructured": "Colchicine for COVID-19: Real-Time Analysis of All 39 Studies\nhttps://c19colchicine.com/"
},
{
"DOI": "10.3389/fphar.2020.579886",
"doi-asserted-by": "publisher",
"key": "ref76"
},
{
"DOI": "10.1186/s13054-020-03000-7",
"doi-asserted-by": "publisher",
"key": "ref77"
},
{
"DOI": "10.2147/TCRM.S273700",
"doi-asserted-by": "publisher",
"key": "ref78"
},
{
"DOI": "10.3389/fmolb.2020.610132",
"doi-asserted-by": "publisher",
"key": "ref79"
},
{
"DOI": "10.1055/a-1300-2550",
"doi-asserted-by": "publisher",
"key": "ref80"
}
],
"reference-count": 80,
"references-count": 80,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.mdpi.com/2077-0383/11/20/6138"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"General Medicine"
],
"subtitle": [],
"title": "Early Outpatient Treatment of COVID-19: A Retrospective Analysis of 392 Cases in Italy",
"type": "journal-article",
"volume": "11"
}
cosentino