Safety and efficacy of probiotic supplements as adjunctive therapies in patients with COVID-19: A systematic review and meta-analysis
et al., PLOS ONE, doi:10.1371/journal.pone.0278356, PROSPERO CRD42022328256, Mar 2023
Probiotics for COVID-19
20th treatment shown to reduce risk in
March 2021, now with p = 0.00000044 from 29 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
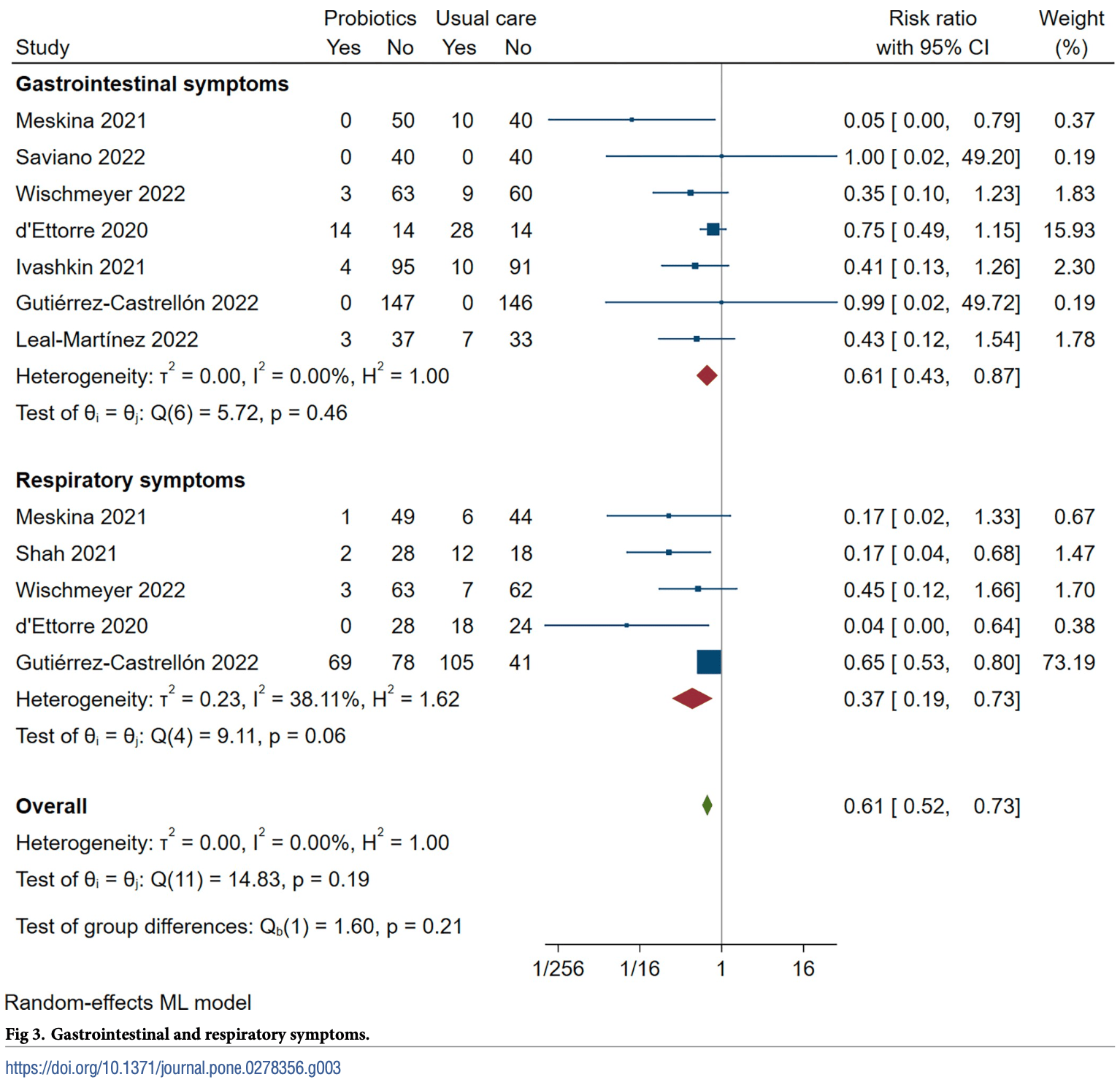
Systematic review and meta-analysis of 8 RCTs with 1,027 patients showing that early probiotic supplements in COVID-19 patients reduced risk of a composite clinical endpoint of escalation or mortality (ow certainty), diarrhea, and cough/dyspnea respiratory symptoms, and are associated with reduced adverse events.
Probiotic efficacy depends on the specific strains used. Specific microbes may decrease or increase COVID-19 risk1.
Currently there are 29 probiotics for COVID-19 studies, showing 59% lower mortality [35‑74%], 38% lower ventilation [-87‑79%], 21% lower ICU admission [-20‑48%], 13% lower hospitalization [5‑21%], and 36% fewer cases [7‑55%].
1.
Li et al., Large-scale genetic correlation studies explore the causal relationship and potential mechanism between gut microbiota and COVID-19-associated risks, BMC Microbiology, doi:10.1186/s12866-024-03423-0.
Zhu et al., 31 Mar 2023, peer-reviewed, 5 authors, trial PROSPERO CRD42022328256.
Contact: julie.zhu@nshealth.ca.
Safety and efficacy of probiotic supplements as adjunctive therapies in patients with COVID-19: A systematic review and meta-analysis
PLOS ONE, doi:10.1371/journal.pone.0278356
Background and aims Oral probiotic supplementation may be a beneficial adjunctive therapy for patients with symptomatic COVID-19. However, its safety and efficacy are unclear. We aimed to investigate how probiotic supplementation impacts COVID-19 symptom trajectory and patient outcomes by conducting a systematic review and meta-analysis of randomized controlled trials (RCTs).
Methods RCTs randomizing patients with COVID-19 to probiotics were searched in PubMed Central, Embase, CINAHL, and Cochrane Library from inception to July 31, 2022. We performed a random-effects pairwise meta-analysis for all outcomes using the restricted maximum likelihood (REML) estimator. We used the GRADE approach to assess the certainty of the evidence.
References
Allen, Wareham, Wang, Bradley, Hutchings et al., Lactobacilli and bifidobacteria in the prevention of antibiotic-associated diarrhoea and Clostridium difficile diarrhoea in older inpatients (PLACIDE): a randomised, double-blind, placebo-controlled, multicentre trial, Lancet, doi:10.1016/S0140-6736%2813%2961218-0
Alpiza-Rodriguez, Lesker, Gronow, Gilbert, Raemy et al., Prevotella copri in individuals at risk for rheumatoid arthritis, Ann Rheum Dis, doi:10.1136/annrheumdis-2018-214514
Anderson, 'donoghue, Dechen, Mechanic, Stevens, Uptake of Outpatient Monoclonal Antibody Treatments for COVID-19 in the United States: a Cross-Sectional Analysis, J. Gen. Intern. Med, doi:10.1007/s11606-021-07109-5
Bulanda, Wypych, Bypassing the Gut-Lung Axis via Microbial Metabolites: Implications for Chronic Respiratory Diseases, Front Microbiol, doi:10.3389/fmicb.2022.857418
Cheema, Shahid, Ayyan, Mustafa, Zahid et al., Probiotics for the Prevention of Ventilator-Associated Pneumonia: An Updated Systematic Review and Meta-Analysis of Randomised Controlled Trials, Nutrients, doi:10.3390/nu14081600
Cheung, Hung, Chan, Lung, Tso et al., Gastrointestinal Manifestations of SARS-CoV-2 Infection and Virus Load in Fecal Samples From a Hong Kong Cohort: Systematic Review and Meta-analysis, Gastroenterology, doi:10.1053/j.gastro.2020.03.065
De Sire, De Sire, Curci, Castiglione, Wahli, Role of Dietary Supplements and Probiotics in Modulating Microbiota and Bone Health: The Gut-Bone Axis, Cells, doi:10.3390/cells11040743
Ettorre, Ceccarelli, Marazzato, Campagna, Pinacchio et al., Challenges in the Management of SARS-CoV2 Infection: The Role of Oral Bacteriotherapy as Complementary Therapeutic Strategy to Avoid the Progression of COVID-19, Front Med, doi:10.3389/fmed.2020.00389
Ferna ´ndez-Ferreiro, Formigo-Couceiro, Veiga-Gutierrez, Maldonado-Lobo ´n, Hermida-Cao et al., Effects of Loigolactobacillus coryniformis K8 CECT 5711 on the Immune Response of Elderly Subjects to COVID-19 Vaccination: A Randomized Controlled Trial, Nutrients, doi:10.3390/nu14010228
Goldenberg, Mertz, Johnston, Probiotics to prevent clostridium difficile infection in patients receiving antibiotics, J. Am. Med. Assoc, doi:10.1001/jama.2018.9064
Grandy, Medina, Soria, Tera ´n Cg, Araya, Probiotics in the treatment of acute rotavirus diarrhoea. A randomized, double-blind, controlled trial using two different probiotic preparations in Bolivian children, BMC Infect Dis, doi:10.1186/1471-2334-10-253
Guo, Goldenberg, Humphrey, Dib, Johnston, Probiotics for the prevention of pediatric antibiotic-associated diarrhea, Cochrane Database Syst. Rev, doi:10.1002/14651858.CD004827.pub5
Gutie ´rrez-Castrello ´n, Gandara-Martı, Abreu, Nieto-Rufino, Lo ´pez-Orduña et al., Probiotic improves symptomatic and viral clearance in Covid19 outpatients: a randomized, quadruple-blinded, placebo-controlled trial, Gut Microbes, doi:10.1080/19490976.2021.2018899
Hao, Dong, Wu, Probiotics for preventing acute upper respiratory tract infections, Cochrane Database Syst. Rev, doi:10.1002/14651858.CD006895.pub3
Hempel, Newberry, Maher, Wang, Miles et al., Probiotics for the prevention and treatment of antibiotic-associated diarrhea: a systematic review and meta-analysis, J. Am. Med. Assoc, doi:10.1001/jama.2012.3507
Islam, Albarracin, Tomokiyo, Valdez, Sacur et al., Immunobiotic Lactobacilli Improve Resistance of Respiratory Epithelial Cells to SARS-CoV-2 Infection, Pathogens, doi:10.3390/pathogens10091197
Isolauri, Su ¨tas, Kankaanpa ¨a ¨p, Arvilommi, Salminen, Probiotics: effects on immunity, Am J Clin Nutr, doi:10.1093/ajcn/73.2.444s
Ivashkin, Fomin, Moiseev, Brovko, Maslennikov et al., Efficacy of a Probiotic Consisting of Lacticaseibacillus rhamnosus PDV 1705, Bifidobacterium bifidum PDV 0903, Bifidobacterium longum subsp. Infantis PDV 1911, and Bifidobacterium longum subsp. longum PDV 2301 in the Treatment of Hospitalized Patients with COVID-19: a Randomized Controlled Trial, Probiotics Antimicrob Proteins, doi:10.1007/s12602-021-09858-5
Kunath, Hickl, Queiro ´s P, Martin-Gallausiaux, Lebrun, Halder, Alterations of oral microbiota and impact on the gut microbiome in type 1 diabetes mellitus revealed by integrated multiomic analyses, Microbiome [Internet, doi:10.1186/s40168-022-01435-4
Kurian, Unnikrishnan, Miraj, Bagchi, Banerjee et al., Probiotics in Prevention and Treatment of COVID-19: Current Perspective and Future Prospects, Arch Med Res, doi:10.1016/j.arcmed.2021.03.002
Leal-Martı ´nez, Abarca-Bernal, Garcı ´a-Pe ´rez, Gonza ´lez-Tolosa, ´zares et al., Effect of a Nutritional Support System to Increase Survival and Reduce Mortality in Patients with COVID-19 in Stage III and Comorbidities: A Blinded Randomized Controlled Clinical Trial, Int. J. Environ. Res. Public Health, doi:10.3390/ijerph19031172
Meskina, Tselipanova, Khadisova, Galkina, Stashko, Efficiency of application of sorbed probiotics in complex therapy of pneumonia caused by SARS-CoV-2. Part 1. Heating clinical displays period, Ter Arkh, doi:10.26442/00403660.2021.04.200835
Mirashrafi, Moravejolahkami, Zehi, Kermani, Nm Haratian, The efficacy of probiotics on virus titres and antibody production in virus diseases: A systematic review on recent evidence for COVID-19 treatment, Clin Nutri ESPEN, doi:10.1016/j.clnesp.2021.10.016
Morrow, Kollef, Casale, Probiotic prophylaxis of ventilator-associated pneumonia: a blinded, randomized, controlled trial, Am J Respir Crit Care Med, doi:10.1164/rccm.200912-1853OC
Page, Mckenzie, Bossuyt, Boutron, Hoffmann et al., The PRISMA 2020 statement: an updated guideline for reporting systematic reviews, BMJ, doi:10.1136/bmj.n71
Peng, Zhang, Yao, Kwok, Zhang, Probiotics as Adjunctive Treatment for Patients Contracted COVID-19: Current Understanding and Future Needs, Front Nutri, doi:10.3389/fnut.2021.669808
Redd, Zhou, Hathorn, Mccarty, Bazarbashi et al., Prevalence and Characteristics of Gastrointestinal Symptoms in Patients With Severe Acute Respiratory Syndrome Coronavirus 2 Infection in the United States: A Multicenter Cohort Study, Gastroenterology, doi:10.1053/j.gastro.2020.04.045
Salaris, Scarpa, Elli, Bertolini, Guglielmetti et al., Lacticaseibacillus paracasei DG enhances the lactoferrin anti-SARS-CoV-2 response in Caco-2 cells, Gut Microbes, doi:10.1080/19490976.2021.1961970
Sartor, Wu, Roles for Intestinal Bacteria, Viruses, and Fungi in Pathogenesis of Inflammatory Bowel Diseases and Therapeutic Approaches, Gastroenterology, doi:10.1053/j.gastro.2016.10.012
Saviano, Potenza, Siciliano, Petruzziello, Tarli et al., COVID-19 Pneumonia and Gut Inflammation: The Role of a Mix of Three Probiotic Strains in Reducing Inflammatory Markers and Need for Oxygen Support, J. Clin. Med, doi:10.3390/jcm11133758
Schandelmaier, Briel, Varadhan, Schmid, Devasenapathy et al., Development of the Instrument to assess the Credibility of Effect Modification Analyses (ICEMAN) in randomized controlled trials and meta-analyses, CMAJ, doi:10.1503/cmaj.200077
Shah, Parent, Vispute, Potential of the Combination of a Systemic Enzyme Complex and Probiotics administration to Combat COVID-19: A Randomized Open Label Prospective Analysis, Adv Clin Toxicol, doi:10.23880/act-16000205
Sharif, Greer, Skorupski, Hao, Johnstone et al., Probiotics in Critical Illness: A Systematic Review and Meta-Analysis of Randomized Controlled Trials, Crit Care Med, doi:10.1097/CCM.0000000000005580
Vacheron, Lepape, Savey, Machut, Timsit et al., Attributable Mortality of Ventilator-associated Pneumonia Among Patients with COVID-19, Am J Respir Crit Care Med, doi:10.1164/rccm.202202-0357OC
Wei, Wang, Niu, Ye, Peng et al., Diarrhea Is Associated With Prolonged Symptoms and Viral Carriage in Corona Virus Disease 2019, Clin Gastroenterol Hepatol, doi:10.1016/j.cgh.2020.04.030
Wischmeyer, Tang, Ren, Bohannon, Ramirez et al., Daily Lactobacillus Probiotic versus Placebo in COVID-19-Exposed Household Contacts (PROTECT-EHC): A Randomized Clinical Trial, doi:10.1101/2022.01.04.21268275v1
Yeoh, Zuo, Lui, Zhang, Liu et al., Gut microbiota composition reflects disease severity and dysfunctional immune responses in patients with COVID-19, Gut, doi:10.1136/gutjnl-2020-323020
Zeng, Wang, Zhang, Qi, Wang et al., Effect of probiotics on the incidence of ventilator-associated pneumonia in critically ill patients: a randomized controlled multicenter trial, Intensive Care Med, doi:10.1007/s00134-016-4303-x
Zhang, Han, Li, Chen, Xie et al., Probiotics use is associated with improved clinical outcomes among hospitalized patients with COVID-19, Therap Adv Gastroenterol, doi:10.1177/17562848211035670
DOI record:
{
"DOI": "10.1371/journal.pone.0278356",
"ISSN": [
"1932-6203"
],
"URL": "http://dx.doi.org/10.1371/journal.pone.0278356",
"abstract": "<jats:sec id=\"sec001\">\n<jats:title>Background and aims</jats:title>\n<jats:p>Oral probiotic supplementation may be a beneficial adjunctive therapy for patients with symptomatic COVID-19. However, its safety and efficacy are unclear. We aimed to investigate how probiotic supplementation impacts COVID-19 symptom trajectory and patient outcomes by conducting a systematic review and meta-analysis of randomized controlled trials (RCTs).</jats:p>\n</jats:sec>\n<jats:sec id=\"sec002\">\n<jats:title>Methods</jats:title>\n<jats:p>RCTs randomizing patients with COVID-19 to probiotics were searched in PubMed Central, Embase, CINAHL, and Cochrane Library from inception to July 31, 2022. We performed a random-effects pairwise meta-analysis for all outcomes using the restricted maximum likelihood (REML) estimator. We used the GRADE approach to assess the certainty of the evidence.</jats:p>\n</jats:sec>\n<jats:sec id=\"sec003\">\n<jats:title>Results</jats:title>\n<jats:p>A total of 1027 participants from eight RCT studies were included in the meta-analysis. Probiotic supplements probably reduce the incidence of diarrhea (RR 0.61 [0.43 to 0.87]; moderate certainty) and probably reduce cough or dyspnea compared to placebo/standard care (RR 0.37 [0.19 to 0.73]; moderate certainty). Probiotic supplements may improve composite endpoint measured by clinical escalation or mortality compared to placebo (RR 0.41 [0.18 to 0.93]; low certainty evidence); however, they may not significantly reduce the need for clinical escalation (RR 0.57 [0.31 to 1.07]; low certainty evidence) or mortality (RR 0.50 [0.20 to 1.29]; low certainty evidence). In addition, the probiotic supplement is associated with reduced adverse events (RR 0.62 [0.46 to 0.83]; moderate certainty).</jats:p>\n</jats:sec>\n<jats:sec id=\"sec004\">\n<jats:title>Conclusion</jats:title>\n<jats:p>Early probiotic supplement is a safe and effective adjunctive therapy that reduces the risk of symptoms and health care burden related to COVID-19 across all severity types.</jats:p>\n</jats:sec>",
"author": [
{
"ORCID": "http://orcid.org/0000-0001-6057-8275",
"affiliation": [],
"authenticated-orcid": true,
"family": "Zhu",
"given": "Julie",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0003-3015-0723",
"affiliation": [],
"authenticated-orcid": true,
"family": "Pitre",
"given": "Tyler",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ching",
"given": "Carmen",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Zeraatkar",
"given": "Dena",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Gruchy",
"given": "Steven",
"sequence": "additional"
}
],
"container-title": "PLOS ONE",
"container-title-short": "PLoS ONE",
"content-domain": {
"crossmark-restriction": false,
"domain": [
"www.plosone.org"
]
},
"created": {
"date-parts": [
[
2023,
3,
31
]
],
"date-time": "2023-03-31T17:55:47Z",
"timestamp": 1680285347000
},
"deposited": {
"date-parts": [
[
2023,
3,
31
]
],
"date-time": "2023-03-31T17:56:19Z",
"timestamp": 1680285379000
},
"editor": [
{
"affiliation": [],
"family": "de Sire",
"given": "Alessandro",
"sequence": "first"
}
],
"indexed": {
"date-parts": [
[
2024,
1,
5
]
],
"date-time": "2024-01-05T06:02:47Z",
"timestamp": 1704434567639
},
"is-referenced-by-count": 2,
"issue": "3",
"issued": {
"date-parts": [
[
2023,
3,
31
]
]
},
"journal-issue": {
"issue": "3",
"published-online": {
"date-parts": [
[
2023,
3,
31
]
]
}
},
"language": "en",
"license": [
{
"URL": "http://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
3,
31
]
],
"date-time": "2023-03-31T00:00:00Z",
"timestamp": 1680220800000
}
}
],
"link": [
{
"URL": "https://dx.plos.org/10.1371/journal.pone.0278356",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "340",
"original-title": [],
"page": "e0278356",
"prefix": "10.1371",
"published": {
"date-parts": [
[
2023,
3,
31
]
]
},
"published-online": {
"date-parts": [
[
2023,
3,
31
]
]
},
"publisher": "Public Library of Science (PLoS)",
"reference": [
{
"author": "World Health Organization",
"journal-title": "Coronavirus disease (COVID-19) pandemic",
"key": "pone.0278356.ref001",
"year": "2022"
},
{
"author": "Centers For Disease Control and Prevention",
"key": "pone.0278356.ref002",
"volume-title": "Estimated COVID-19 Burden [Internet].",
"year": "2022"
},
{
"author": "Centers For Disease Control and Prevention",
"key": "pone.0278356.ref003",
"volume-title": "COVID-19 Symptoms [Internet]",
"year": "2022"
},
{
"article-title": "COVID-19 and GI Symptoms [Internet].",
"author": "Gastrointestinal Society",
"journal-title": "Gastrointestinal Society",
"key": "pone.0278356.ref004",
"year": "2022"
},
{
"DOI": "10.1053/j.gastro.2020.03.065",
"article-title": "Gastrointestinal Manifestations of SARS-CoV-2 Infection and Virus Load in Fecal Samples From a Hong Kong Cohort: Systematic Review and Meta-analysis",
"author": "KS Cheung",
"doi-asserted-by": "crossref",
"first-page": "81",
"issue": "1",
"journal-title": "Gastroenterology",
"key": "pone.0278356.ref005",
"volume": "159",
"year": "2020"
},
{
"DOI": "10.1093/ajcn/73.2.444s",
"article-title": "Probiotics: effects on immunity",
"author": "E Isolauri",
"doi-asserted-by": "crossref",
"first-page": "444S",
"issue": "2 Suppl",
"journal-title": "Am J Clin Nutr",
"key": "pone.0278356.ref006",
"volume": "73",
"year": "2001"
},
{
"DOI": "10.1136/annrheumdis-2018-214514",
"article-title": "Prevotella copri in individuals at risk for rheumatoid arthritis",
"author": "D Alpiza-Rodriguez",
"doi-asserted-by": "crossref",
"first-page": "590",
"issue": "5",
"journal-title": "Ann Rheum Dis",
"key": "pone.0278356.ref007",
"volume": "78",
"year": "2019"
},
{
"DOI": "10.3390/cells11040743",
"article-title": "Role of Dietary Supplements and Probiotics in Modulating Microbiota and Bone Health: The Gut-Bone Axis.",
"author": "A de Sire",
"doi-asserted-by": "crossref",
"first-page": "743",
"issue": "4",
"journal-title": "Cells [Internet].",
"key": "pone.0278356.ref008",
"volume": "11",
"year": "2022"
},
{
"DOI": "10.1186/s40168-022-01435-4",
"article-title": "Alterations of oral microbiota and impact on the gut microbiome in type 1 diabetes mellitus revealed by integrated multi-omic analyses.",
"author": "BJ Kunath",
"doi-asserted-by": "crossref",
"first-page": "243",
"issue": "1",
"journal-title": "Microbiome [Internet].",
"key": "pone.0278356.ref009",
"volume": "10",
"year": "2022"
},
{
"DOI": "10.1053/j.gastro.2016.10.012",
"article-title": "Roles for Intestinal Bacteria, Viruses, and Fungi in Pathogenesis of Inflammatory Bowel Diseases and Therapeutic Approaches",
"author": "RB Sartor",
"doi-asserted-by": "crossref",
"first-page": "327",
"issue": "2",
"journal-title": "Gastroenterology [Internet].",
"key": "pone.0278356.ref010",
"volume": "152",
"year": "2017"
},
{
"article-title": "Bypassing the Gut-Lung Axis via Microbial Metabolites: Implications for Chronic Respiratory Diseases. Front Microbiol",
"author": "E Bulanda",
"first-page": "857418",
"journal-title": "Internet]",
"key": "pone.0278356.ref011",
"volume": "13",
"year": "2022"
},
{
"article-title": "Probiotics for preventing acute upper respiratory tract infections",
"author": "Q Hao",
"first-page": "CD006895",
"issue": "2",
"journal-title": "Cochrane Database Syst. Rev. [Internet].",
"key": "pone.0278356.ref012",
"year": "2015"
},
{
"DOI": "10.1164/rccm.200912-1853OC",
"article-title": "Probiotic prophylaxis of ventilator-associated pneumonia: a blinded, randomized, controlled trial",
"author": "LE Morrow",
"doi-asserted-by": "crossref",
"first-page": "1058",
"issue": "8",
"journal-title": "Am J Respir Crit Care Med",
"key": "pone.0278356.ref013",
"volume": "182",
"year": "2010"
},
{
"DOI": "10.1007/s00134-016-4303-x",
"article-title": "Effect of probiotics on the incidence of ventilator-associated pneumonia in critically ill patients: a randomized controlled multicenter trial.",
"author": "J Zeng",
"doi-asserted-by": "crossref",
"first-page": "1018",
"issue": "6",
"journal-title": "Intensive Care Med.Jun",
"key": "pone.0278356.ref014",
"volume": "42",
"year": "2016"
},
{
"DOI": "10.1097/CCM.0000000000005580",
"article-title": "Probiotics in Critical Illness: A Systematic Review and Meta-Analysis of Randomized Controlled Trials.",
"author": "S Sharif",
"doi-asserted-by": "crossref",
"first-page": "1175",
"issue": "8",
"journal-title": "Crit Care Med.",
"key": "pone.0278356.ref015",
"volume": "50",
"year": "2022"
},
{
"DOI": "10.1001/jama.2012.3507",
"article-title": "Probiotics for the prevention and treatment of antibiotic-associated diarrhea: a systematic review and meta-analysis",
"author": "S Hempel",
"doi-asserted-by": "crossref",
"first-page": "1959",
"issue": "18",
"journal-title": "J. Am. Med. Assoc",
"key": "pone.0278356.ref016",
"volume": "307",
"year": "2012"
},
{
"DOI": "10.1016/S0140-6736(13)61218-0",
"article-title": "Lactobacilli and bifidobacteria in the prevention of antibiotic-associated diarrhoea and Clostridium difficile diarrhoea in older inpatients (PLACIDE): a randomised, double-blind, placebo-controlled, multicentre trial.",
"author": "SJ Allen",
"doi-asserted-by": "crossref",
"first-page": "1249",
"issue": "9900",
"journal-title": "Lancet",
"key": "pone.0278356.ref017",
"volume": "382",
"year": "2013"
},
{
"article-title": "Probiotics for the prevention of pediatric antibiotic-associated diarrhea",
"author": "Q Guo",
"first-page": "CD004827",
"issue": "4",
"journal-title": "Cochrane Database Syst. Rev",
"key": "pone.0278356.ref018",
"volume": "4",
"year": "2019"
},
{
"DOI": "10.1001/jama.2018.9064",
"article-title": "Probiotics to prevent clostridium difficile infection in patients receiving antibiotics",
"author": "JZ Goldenberg",
"doi-asserted-by": "crossref",
"first-page": "499",
"issue": "5",
"journal-title": "J. Am. Med. Assoc",
"key": "pone.0278356.ref019",
"volume": "320",
"year": "2018"
},
{
"DOI": "10.1080/19490976.2021.1961970",
"article-title": "Lacticaseibacillus paracasei DG enhances the lactoferrin anti-SARS-CoV-2 response in Caco-2 cells",
"author": "C Salaris",
"doi-asserted-by": "crossref",
"first-page": "1961970",
"issue": "1",
"journal-title": "Gut Microbes",
"key": "pone.0278356.ref020",
"volume": "13",
"year": "2021"
},
{
"DOI": "10.3390/pathogens10091197",
"article-title": "Immunobiotic Lactobacilli Improve Resistance of Respiratory Epithelial Cells to SARS-CoV-2 Infection.",
"author": "MA Islam",
"doi-asserted-by": "crossref",
"first-page": "1197",
"issue": "9",
"journal-title": "Pathogens.",
"key": "pone.0278356.ref021",
"volume": "10",
"year": "2021"
},
{
"DOI": "10.1177/17562848211035670",
"article-title": "Probiotics use is associated with improved clinical outcomes among hospitalized patients with COVID-19.",
"author": "L Zhang",
"doi-asserted-by": "crossref",
"first-page": "17562848211035670",
"journal-title": "Therap Adv Gastroenterol.",
"key": "pone.0278356.ref022",
"volume": "14",
"year": "2021"
},
{
"DOI": "10.1136/bmj.n71",
"article-title": "The PRISMA 2020 statement: an updated guideline for reporting systematic reviews.",
"author": "MJ Page",
"doi-asserted-by": "crossref",
"first-page": "n71",
"journal-title": "BMJ",
"key": "pone.0278356.ref023",
"volume": "372",
"year": "2021"
},
{
"DOI": "10.1016/S1473-3099(20)30483-7",
"article-title": "WHO Working Group on the Clinical Characterisation and Management of COVID-19 infection. A minimal common outcome measure set for COVID-19 clinical research",
"doi-asserted-by": "crossref",
"first-page": "e192",
"issue": "8",
"journal-title": "Lancet Infect Dis",
"key": "pone.0278356.ref024",
"volume": "20",
"year": "2020"
},
{
"DOI": "10.1503/cmaj.200077",
"article-title": "Development of the Instrument to assess the Credibility of Effect Modification Analyses (ICEMAN) in randomized controlled trials and meta-analyses.",
"author": "S Schandelmaier",
"doi-asserted-by": "crossref",
"first-page": "E901",
"issue": "32",
"journal-title": "CMAJ.",
"key": "pone.0278356.ref025",
"volume": "192",
"year": "2020"
},
{
"DOI": "10.1080/19490976.2021.2018899",
"article-title": "Probiotic improves symptomatic and viral clearance in Covid19 outpatients: a randomized, quadruple-blinded, placebo-controlled trial",
"author": "P Gutiérrez-Castrellón",
"doi-asserted-by": "crossref",
"first-page": "2018899",
"issue": "1",
"journal-title": "Gut Microbes",
"key": "pone.0278356.ref026",
"volume": "14",
"year": "2022"
},
{
"DOI": "10.3389/fmed.2020.00389",
"article-title": "Challenges in the Management of SARS-CoV2 Infection: The Role of Oral Bacteriotherapy as Complementary Therapeutic Strategy to Avoid the Progression of COVID-19.",
"author": "G d’Ettorre",
"doi-asserted-by": "crossref",
"first-page": "389",
"journal-title": "Front Med (Lausanne).",
"key": "pone.0278356.ref027",
"volume": "7",
"year": "2020"
},
{
"DOI": "10.3390/ijerph19031172",
"article-title": "Effect of a Nutritional Support System to Increase Survival and Reduce Mortality in Patients with COVID-19 in Stage III and Comorbidities: A Blinded Randomized Controlled Clinical Trial",
"author": "F Leal-Martínez",
"doi-asserted-by": "crossref",
"first-page": "1172",
"issue": "3",
"journal-title": "Int. J. Environ. Res. Public Health",
"key": "pone.0278356.ref028",
"volume": "19",
"year": "2022"
},
{
"DOI": "10.3390/jcm11133758",
"article-title": "COVID-19 Pneumonia and Gut Inflammation: The Role of a Mix of Three Probiotic Strains in Reducing Inflammatory Markers and Need for Oxygen Support",
"author": "A Saviano",
"doi-asserted-by": "crossref",
"first-page": "3758",
"issue": "13",
"journal-title": "J. Clin. Med",
"key": "pone.0278356.ref029",
"volume": "11",
"year": "2022"
},
{
"article-title": "Daily Lactobacillus Probiotic versus Placebo in COVID-19-Exposed Household Contacts (PROTECT-EHC): A Randomized Clinical Trial.",
"author": "PE Wischmeyer",
"journal-title": "medRxiv [Internet].",
"key": "pone.0278356.ref030",
"year": "2022"
},
{
"article-title": "Efficacy of a Probiotic Consisting of Lacticaseibacillus rhamnosus PDV 1705, Bifidobacterium bifidum PDV 0903, Bifidobacterium longum subsp. Infantis PDV 1911, and Bifidobacterium longum subsp. longum PDV 2301 in the Treatment of Hospitalized Patients with COVID-19: a Randomized Controlled Trial.",
"author": "V Ivashkin",
"first-page": "1",
"journal-title": "Probiotics Antimicrob Proteins",
"key": "pone.0278356.ref031",
"year": "2021"
},
{
"article-title": "Efficiency of application of sorbed probiotics in complex therapy of pneumonia caused by SARS-CoV-2. Part 1. Heating clinical displays period [Article originally in Russian].",
"author": "ER Meskina",
"first-page": "456",
"issue": "4",
"journal-title": "Ter Arkh.",
"key": "pone.0278356.ref032",
"volume": "93",
"year": "2021"
},
{
"DOI": "10.23880/act-16000205",
"article-title": "Potential of the Combination of a Systemic Enzyme Complex and Probiotics administration to Combat COVID-19: A Randomized Open Label Prospective Analysis.",
"author": "N Shah",
"doi-asserted-by": "crossref",
"first-page": "000205",
"issue": "1",
"journal-title": "Adv Clin Toxicol.",
"key": "pone.0278356.ref033",
"volume": "6",
"year": "2021"
},
{
"DOI": "10.3390/nu14010228",
"article-title": "Effects of Loigolactobacillus coryniformis K8 CECT 5711 on the Immune Response of Elderly Subjects to COVID-19 Vaccination: A Randomized Controlled Trial",
"author": "A Fernández-Ferreiro",
"doi-asserted-by": "crossref",
"first-page": "228",
"issue": "1",
"journal-title": "Nutrients",
"key": "pone.0278356.ref034",
"volume": "14",
"year": "2022"
},
{
"author": "Centers For Disease Control and Prevention",
"key": "pone.0278356.ref035",
"volume-title": "COVID-19 Treatments and Medications [Internet]",
"year": "2022"
},
{
"DOI": "10.1007/s11606-021-07109-5",
"article-title": "Uptake of Outpatient Monoclonal Antibody Treatments for COVID-19 in the United States: a Cross-Sectional Analysis",
"author": "Anderson TS",
"doi-asserted-by": "crossref",
"first-page": "3922",
"journal-title": "J. Gen. Intern. Med",
"key": "pone.0278356.ref036",
"volume": "36",
"year": "2021"
},
{
"author": "National Institute of Health",
"key": "pone.0278356.ref037",
"volume-title": "COVID-19 Treatment Guidelines [Internet]",
"year": "2022"
},
{
"DOI": "10.3389/fnut.2021.669808",
"article-title": "Probiotics as Adjunctive Treatment for Patients Contracted COVID-19: Current Understanding and Future Needs.",
"author": "J Peng",
"doi-asserted-by": "crossref",
"first-page": "669808",
"journal-title": "Front Nutri.",
"key": "pone.0278356.ref038",
"volume": "8",
"year": "2021"
},
{
"DOI": "10.1016/j.clnesp.2021.10.016",
"article-title": "The efficacy of probiotics on virus titres and antibody production in virus diseases: A systematic review on recent evidence for COVID-19 treatment.",
"author": "S Mirashrafi",
"doi-asserted-by": "crossref",
"first-page": "1",
"journal-title": "Clin Nutri ESPEN.",
"key": "pone.0278356.ref039",
"volume": "46",
"year": "2021"
},
{
"DOI": "10.3390/nu14081600",
"article-title": "Probiotics for the Prevention of Ventilator-Associated Pneumonia: An Updated Systematic Review and Meta-Analysis of Randomised Controlled Trials.",
"author": "HA Cheema",
"doi-asserted-by": "crossref",
"first-page": "1600",
"issue": "8",
"journal-title": "Nutrients.",
"key": "pone.0278356.ref040",
"volume": "14",
"year": "2022"
},
{
"DOI": "10.1164/rccm.202202-0357OC",
"article-title": "Attributable Mortality of Ventilator-associated Pneumonia Among Patients with COVID-19",
"author": "CH Vacheron",
"doi-asserted-by": "crossref",
"first-page": "161",
"issue": "2",
"journal-title": "Am J Respir Crit Care Med",
"key": "pone.0278356.ref041",
"volume": "206",
"year": "2022"
},
{
"DOI": "10.1053/j.gastro.2020.04.045",
"article-title": "Prevalence and Characteristics of Gastrointestinal Symptoms in Patients With Severe Acute Respiratory Syndrome Coronavirus 2 Infection in the United States: A Multicenter Cohort Study",
"author": "WD Redd",
"doi-asserted-by": "crossref",
"first-page": "765",
"issue": "2",
"journal-title": "Gastroenterology",
"key": "pone.0278356.ref042",
"volume": "159",
"year": "2020"
},
{
"DOI": "10.1016/j.cgh.2020.04.030",
"article-title": "Diarrhea Is Associated With Prolonged Symptoms and Viral Carriage in Corona Virus Disease 2019.",
"author": "XS Wei",
"doi-asserted-by": "crossref",
"first-page": "1753",
"issue": "8",
"journal-title": "Clin Gastroenterol Hepatol",
"key": "pone.0278356.ref043",
"volume": "18",
"year": "2020"
},
{
"DOI": "10.1136/gutjnl-2020-323020",
"article-title": "Gut microbiota composition reflects disease severity and dysfunctional immune responses in patients with COVID-19",
"author": "YK Yeoh",
"doi-asserted-by": "crossref",
"first-page": "698",
"issue": "4",
"journal-title": "Gut",
"key": "pone.0278356.ref044",
"volume": "70",
"year": "2021"
},
{
"DOI": "10.1186/1471-2334-10-253",
"article-title": "Probiotics in the treatment of acute rotavirus diarrhoea. A randomized, double-blind, controlled trial using two different probiotic preparations in Bolivian children.",
"author": "G Grandy",
"doi-asserted-by": "crossref",
"first-page": "253",
"journal-title": "BMC Infect Dis.",
"key": "pone.0278356.ref045",
"volume": "10",
"year": "2010"
},
{
"DOI": "10.1016/j.arcmed.2021.03.002",
"article-title": "Probiotics in Prevention and Treatment of COVID-19: Current Perspective and Future Prospects",
"author": "SJ Kurian",
"doi-asserted-by": "crossref",
"first-page": "582",
"issue": "6",
"journal-title": "Arch Med Res",
"key": "pone.0278356.ref046",
"volume": "52",
"year": "2021"
}
],
"reference-count": 46,
"references-count": 46,
"relation": {},
"resource": {
"primary": {
"URL": "https://dx.plos.org/10.1371/journal.pone.0278356"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Multidisciplinary"
],
"subtitle": [],
"title": "Safety and efficacy of probiotic supplements as adjunctive therapies in patients with COVID-19: A systematic review and meta-analysis",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1371/journal.pone.corrections_policy",
"volume": "18"
}
