Probiotics improve symptoms of patients with COVID-19 through gut-lung axis: a systematic review and meta-analysis
et al., Frontiers in Nutrition, doi:10.3389/fnut.2023.1179432, PROSPERO CRD42023398309, May 2023
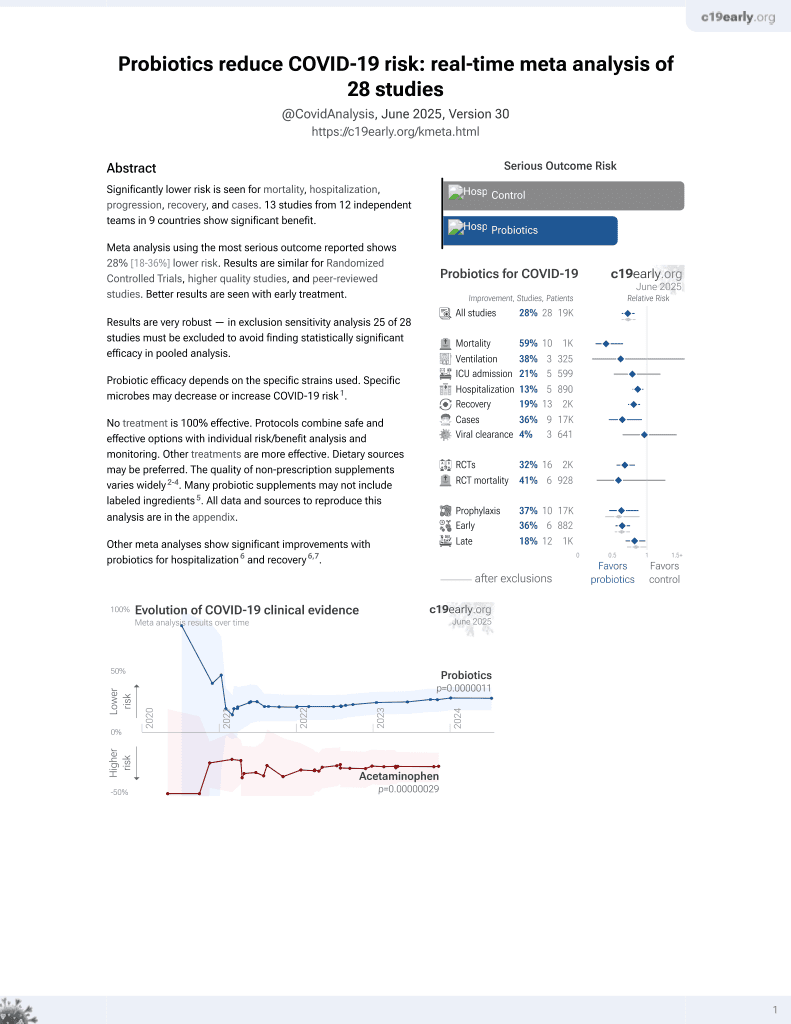
Probiotics for COVID-19
20th treatment shown to reduce risk in
March 2021, now with p = 0.00000044 from 29 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Systematic review and meta-analysis of 10 studies (8 RCTs and 2 retrospective studies) with 1,198 COVID-19 patients showing improved overall symptoms, reduced diarrhea duration, lower C-reactive protein levels, and shorter hospital stays with various probiotic interventions compared to placebo or standard care. Authors suggest probiotics may alleviate gastrointestinal and respiratory symptoms in COVID-19 through modulation of the gut-lung axis.
Probiotic efficacy depends on the specific strains used. Specific microbes may decrease or increase COVID-19 risk1.
Currently there are 29 probiotics for COVID-19 studies, showing 59% lower mortality [35‑74%], 38% lower ventilation [-87‑79%], 21% lower ICU admission [-20‑48%], 13% lower hospitalization [5‑21%], and 36% fewer cases [7‑55%].
1.
Li et al., Large-scale genetic correlation studies explore the causal relationship and potential mechanism between gut microbiota and COVID-19-associated risks, BMC Microbiology, doi:10.1186/s12866-024-03423-0.
Tian et al., 22 May 2023, peer-reviewed, 7 authors, trial PROSPERO CRD42023398309.
Contact: pant414@163.com.
Probiotics improve symptoms of patients with COVID-through gut-lung axis: a systematic review and meta-analysis
Background: Multi system symptoms such as gastrointestinal tract and respiratory tract exist in coronavirus disease (COVID-) patients. There is a lack of reliable evidence to prove that probiotics are e ective in improving these symptoms. In this study, we aimed to evaluate the e cacy of probiotics in metaanalysis. Methods: We systematically searched PubMed, Embase, Web of Science, and Cochrane Library up to February , . Randomized controlled trials or high quality retrospective studies comparing the e cacy of probiotics as supplementation with non-probiotics in improving symptoms for patients with COVID-were included. This meta-analysis assessed endpoints using Review Manager . .
Result: Ten citations comprising patients with COVID-were included. The results showed that probiotics could increase the number of people with overall symptom improvement (RR = . , % CI [ . , . ], P = . ) and shorten the duration (days) of overall symptoms (MD = -. , % CI [-. , -. ], P = . ). For the duration (days) of specific symptoms, probiotics could improve diarrhea (MD = -. , % CI [-. , -. ], P < . ), cough (MD = -. , % CI [-. , . ], P = . ) and shortness of breath (MD = -. , % CI [-. , -. ], P = . ). Probiotics had no obvious e ect on fever, headache and weakness. For inflammation, probiotics could e ectively reduce C-reactive Protein (CRP) serum level (mg/L) (MD = -. , % CI [-. , -. ], P < . ). Regarding hospital stay (days), probiotics group was shorter than non-probiotics group (MD = -. , % CI [-. , -. ], P = . ).
Conclusion: To some extent probiotics could improve the overall symptoms, inflammatory reaction and shorten hospital stay of patients with COVID-. Probiotics may improve gastrointestinal symptoms (such as improving intestinal flora and reducing the duration of diarrhea) and further improve respiratory symptoms through the gut-lung axis.
Author contributions Data curation and writing-review and editing: YT, HR, XW, and GF. Formal analysis: XW and RL. Funding acquisition: XW and TP. Investigation: YT and RL. Methodology: YT and HR. Project administration: YT, XW, and TP. Software: YT and XZ. Supervision and visualization: GF. Writing-original draft: YT, XW, and XZ. All authors contributed to the article and approved the submitted version.
Conflict of interest The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note All claims expressed in this article are solely those of the authors and do not necessarily represent those of
Supplementary material The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnut.2023. 1179432/full#supplementary-material
References
Abbasi-Dokht, Sadrifar, Forouzandeh, Malek, Hemmati et al., Multistrain probiotics supplement alleviates asthma symptoms via increasing Treg cells population: A randomized, double-blind, placebo-controlled trial, Int Arch Allergy Immunol, doi:10.1159/000526739
Anwar, Altayb, Fa, Kamal, Kumar, Antiviral effects of probiotic metabolites on COVID-19, J Biomol Struct Dyn, doi:10.1080/07391102.2020.1775123
Argenziano, Bruce, Slater, Tiao, Baldwin et al., Characterization and clinical course of 1000 patients with coronavirus disease 2019 in New York: retrospective case series, BMJ, doi:10.1136/bmj.m1996
Bonfrate, Palo, Celano, Albert, Angelis et al., The beneficial effects of a novel formulation of Bifidobacterium longum BB536 and Lactobacillus rhamnosus HN001 with B6 vitamin on gut microbiota and intestinal permeability in IBS patients, Eur J Clin Invest, doi:10.1111/eci.13108
Bottari, Castellone, Neviani, Probiotics and Covid-19, Int J Food Sci Nutr, doi:10.1080/09637486.2020.1807475
Cipriano, Ruberti, Giacalone, Gastrointestinal infection could be new focus for coronavirus diagnosis, Cureus, doi:10.7759/cureus.7422
De Oliveira, Oliveira, Pinzan, De Salis, Cardoso, Microbiota modulation of the gut-lung axis in COVID-19, Front Immunol, doi:10.3389/fimmu.2021.635471
Dhar, Mohanty, Gut microbiota and Covid-19-possible link and implications, Virus Res, doi:10.1016/j.virusres.2020.198018
Fernandes, Rodrigues, Araújo, Formiga, Horan et al., Risk factors and survival in patients with COVID-19 in northeastern Brazil, PLoS ONE, doi:10.1101/2022.01.27.22269602
Fernández-Ferreiro, Formigo-Couceiro, Veiga-Gutierrez, Maldonado-Lobón, Hermida-Cao et al., Effects of Loigolactobacillus coryniformis K8 CECT 5711 on the immune response of elderly subjects to COVID-19 vaccination: a randomized controlled trial, Nutrients, doi:10.3390/nu14010228
Foladori, Cutrupi, Segata, Manara, Pinto et al., SARS-CoV-2 from faeces to wastewater treatment: What do we know? A review, Sci Total Environ, doi:10.1016/j.scitotenv.2020.140444
Gutiérrez-Castrellón, Gandara-Martí, Abreu, Nieto-Rufino, López-Orduña et al., Probiotic improves symptomatic and viral clearance in Covid19 outpatients: a randomized, quadruple-blinded, placebocontrolled trial, Gut Microbes, doi:10.1080/19490976.2021.2018899
Huang, Pranata, Lim, Oehadian, Alisjahbana, C-reactive protein, procalcitonin, D-dimer, and ferritin in severe coronavirus disease-2019: a metaanalysis, Ther Adv Respir Dis, doi:10.1177/1753466620937175
Ivashkin, Fomin, Moiseev, Brovko, Maslennikov et al., Efficacy of a probiotic consisting of Lacticaseibacillus rhamnosus PDV 1705, Bifidobacterium bifidum PDV 0903, Bifidobacterium longum subsp. infantis PDV 1911, and Bifidobacterium longum subsp. longum PDV 2301 in the treatment of hospitalized patients with COVID-19: a randomized controlled trial, Probiotics Antimicrob Proteins, doi:10.1007/s12602-021-09858-5
Jaeschke, Singer, Guyatt, Measurement of health status. Ascertaining the minimal clinically important difference Control, Clin Trials, doi:10.1016/0197-2456(89)90005-6
Johnston, Patrick, Thorlund, Busse, Da et al., Patient-reported outcomes in meta-analyses-part 2: methods for improving interpretability for decision-makers, Health Qual Life Outcomes, doi:10.1186/1477-7525-11-211
Karim, Muhammad, Iqbal, Qaisar, multistrain probiotic improves handgrip strength and functional capacity in patients with COPD: a randomized controlled trial, Arch Gerontol Geriatr, doi:10.1016/j.archger.2022.104721
Kokubo, Komano, Tsuji, Fujiwara, Fujii et al., The effects of plasmacytoid dendritic cell-stimulative lactic acid bacteria, Lactococcus lactis strain plasma, on exercise-induced fatigue and recovery via immunomodulatory action, Int J Sport Nutr Exerc Metab, doi:10.1123/ijsnem.2018-0377
Li, Zhou, Yan, Wan, An update on the mutual impact between SARS-CoV-2 infection and gut microbiota, Viruses, doi:10.3390/v14081774
Lu, Zhao, Li, Niu, Yang et al., Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding, Lancet, doi:10.1016/S0140-6736(20)30251-8
Luo, Wan, Liu, Tong, Optimally estimating the sample mean from the sample size, median, mid-range, and/or mid-quartile range, Stat Methods Med Res, doi:10.1177/0962280216669183
Maeda, Motooka, Kawasaki, Oki, Noda et al., Longitudinal alterations of the gut mycobiota and microbiota on COVID-19 severity, BMC Infect Dis, doi:10.1186/s12879-022-07358-7
Maev, Andreev, Sokolov, Devkota, Andreev, Efficacy of Saccharomyces boulardii CNCM I-745 probiotic drug in the prevention and treatment of diarrhea in hospitalized patients with new coronavirus infection COVID-19, Ter Arkh, doi:10.26442/00403660.2022.10.201881
Mahooti, Miri, Ghaemi, The immunomodulatory effects of probiotics on respiratory viral infections: A hint for COVID-19 treatment?, Microb Pathog, doi:10.1016/j.micpath.2020.104452
Merola, Armelao, De, Prevalence of gastrointestinal symptoms in coronavirus disease 2019: a meta-analysis, Acta Gastroenterol Belg
Meskina, Tselipanova, Khadisova, Galkina, Stashko, Efficiency of application of sorbed probiotics in complex therapy of pneumonia caused by SARS-CoV-2. Part 1 Heating clinical displays period, Ter Arkh, doi:10.26442/00403660.2021.04.200835
Moher, Liberati, Tetzlaff, Altman, Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement, Ann Intern Med, doi:10.7326/0003-4819-151-4-200908180-00135
Naghibzadeh, Salmani, Nomiri, Tavakoli, Investigating the effect of quadruple therapy with Saccharomyces boulardii or Lactobacillus reuteri strain (DSMZ 17648) supplements on eradication of Helicobacter pylori and treatments adverse effects: a double-blind placebo-controlled randomized clinical trial, BMC Gastroenterol, doi:10.1186/s12876-022-02187-z
Navarro-López, Hernández-Belmonte, Pérez, Ayo-González, Losa-Rodríguez et al., Oral intake of Kluyveromyces marxianus B0399 plus Lactobacillus rhamnosus CECT 30579 to mitigate symptoms in COVID-19 patients: a randomized open label clinical trial, Med Microecol, doi:10.1016/j.medmic.2022.100061
Neag, Vulturar, Gherman, Burlacu, Todea et al., Gastrointestinal microbiota: a predictor of COVID-19 severity?, World J Gastroenterol, doi:10.3748/wjg.v28.i45.6328
Neris, Do, De Carvalho, Tianeze, Santana et al., Benefits of probiotic use on COVID-19: A systematic review and meta-analysis, Crit Rev Food Sci Nutr, doi:10.1080/10408398.2022.2128713
Peladic, Aquila, Carrieri, Maggio, Cherubini et al., Potential roe of probiotics for inflammaging: a narrative review, Nutrients, doi:10.3390/nu13092919
Piletz, Cooper, Chidester, Erson, Melton et al., Transepithelial effect of probiotics in a novel model of gut lumen to nerve signaling, Nutrients, doi:10.3390/nu14224856
Ray, Santee, Mccauley, Panzer, Lynch, Gut Bifidobacteria enrichment following oral Lactobacillus-supplementation is associated with clinical improvements in children with cystic fibrosis, BMC Pulm Med, doi:10.1186/s12890-022-02078-9
Rozman, Rituper, Kačar, Kopač, Zidarn et al., Length of hospital stay and survival of hospitalized COVID-19 patients during the second wave of the pandemic: a single centre retrospective study from slovenia, Zdr Varst, doi:10.2478/sjph-2022-0027
Sadeghi-Haddad-Zavareh, Bayani, Shokri, Ebrahimpour, Babazadeh et al., C-reactive protein as a prognostic indicator in COVID-19 patients, Interdiscip Perspect Infect Dis, doi:10.1155/2021/5557582
Saviano, Potenza, Siciliano, Petruzziello, Tarli et al., COVID-19 pneumonia and gut inflammation: the role of a mix of three probiotic strains in reducing inflammatory markers and need for oxygen support, J Clin Med, doi:10.3390/jcm11133758
Schmulson, Dávalos, Berumen, Beware: Gastrointestinal symptoms can be a manifestation of COVID-19, Rev Gastroenterol Mex, doi:10.1016/j.rgmxen.2020.04.001
Shahbazi, Yasavoli-Sharahi, Alsadi, Ismail, Matar, Probiotics in treatment of viral respiratory infections and neuroinflammatory disorders, Molecules, doi:10.3390/molecules25214891
Singh, Bhadani, Surabhi, Sinha, Bharti et al., Significance of immune-inflammatory markers in predicting clinical outcome of COVID-19 patients Indian, J Pathol Microbiol, doi:10.4103/ijpm.ijpm_658_21
Song, Kim, Hong, Lee, Lee et al., Oral intake of Lactobacillus rhamnosus M21 enhances the survival rate of mice lethally infected with influenza virus, J Microbiol Immunol Inf, doi:10.1016/j.jmii.2014.07.011
Sundararaman, Ray, Ravindra, Halami, Role of probiotics to combat viral infections with emphasis on COVID-19, Appl Microbiol Biotechnol, doi:10.1007/s00253-020-10832-4
Synodinou, Nikolaki, Triantafyllou, Kasti, Immunomodulatory effects of probiotics on COVID-19 infection by targeting the gut-lung axis microbial cross-talk, Microorganisms, doi:10.3390/microorganisms10091764
Tan, Zhu, Du, Zhang, Yin, Effects of probiotics on serum levels of Th1/Th2 cytokine and clinical outcomes in severe traumatic brain-injured patients: a prospective randomized pilot study, Critical Care, doi:10.1186/cc10579
Vaezi, Ravanshad, Rad, Zarrinfar, Kabiri, The effect of synbiotic adjunct therapy on clinical and paraclinical outcomes in hospitalized COVID-19 patients: A randomized placebo-controlled trial, J Med Virol, doi:10.1002/jmv.28463
Vanbelle, Teller, Focant, Probiotics in animal nutrition: a review, Archiv für Tierernährung, doi:10.1080/17450399009428406
Viera-Segura, Vega-Magaña, García-Chagollán, Peña-Rodríguez, Muñoz-Sánchez, A comprehensive descriptive epidemiological and clinical analysis of SARS-CoV-2 in west-Mexico during COVID-19 pandemic 2020, Int J Environ Res Public Health, doi:10.3390/ijerph182010644
Wan, Wang, Liu, Tong, Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range, BMC Med Res Methodol, doi:10.1186/1471-2288-14-135
Wang, Wang, Lu, Qiu, Song et al., The efficacy of probiotics in patients with severe COVID-19, Ann Palliat Med, doi:10.21037/apm-21-3373
Wischmeyer, Tang, Ren, Bohannon, Ramirez Z E, Andermann, Daily lactobacillus probiotic versus placebo in COVID-19-exposed household contacts (PROTECT-EHC), Clin Trial, doi:10.1101/2022.01.04.21268275
Wu, Nasab, Arora, Athari, Study effect of probiotics and prebiotics on treatment of OVA-LPS-induced of allergic asthma inflammation and pneumonia by regulating the TLR4/NF-kB signaling pathway, J. Transl Med, doi:10.1186/s12967-022-03337-3
Xavier-Santos, Padilha, Fabiano, Vinderola, Gomes et al., Evidences and perspectives of the use of probiotics, prebiotics, synbiotics, and postbiotics as adjuvants for prevention and treatment of COVID-19: a bibliometric analysis and systematic review, Trends Food Sci Technol, doi:10.1016/j.tifs.2021.12.033
Zhang, Han, Li, Chen, Xie et al., Probiotics use is associated with improved clinical outcomes among hospitalized patients with COVID-19, Therap Adv Gastroenterol, doi:10.1177/17562848211035670
Zhao, Feng, Meng, Li, Li, Modulated gut microbiota for potential COVID-19 prevention and treatment, Front Med, doi:10.3389/fmed.2022.811176
DOI record:
{
"DOI": "10.3389/fnut.2023.1179432",
"ISSN": [
"2296-861X"
],
"URL": "http://dx.doi.org/10.3389/fnut.2023.1179432",
"abstract": "<jats:sec><jats:title>Background</jats:title><jats:p>Multi system symptoms such as gastrointestinal tract and respiratory tract exist in coronavirus disease 2019 (COVID-19) patients. There is a lack of reliable evidence to prove that probiotics are effective in improving these symptoms. In this study, we aimed to evaluate the efficacy of probiotics in meta-analysis.</jats:p></jats:sec><jats:sec><jats:title>Methods</jats:title><jats:p>We systematically searched PubMed, Embase, Web of Science, and Cochrane Library up to February 15, 2023. Randomized controlled trials or high quality retrospective studies comparing the efficacy of probiotics as supplementation with non-probiotics in improving symptoms for patients with COVID-19 were included. This meta-analysis assessed endpoints using Review Manager 5.3.</jats:p></jats:sec><jats:sec><jats:title>Result</jats:title><jats:p>Ten citations comprising 1198 patients with COVID-19 were included. The results showed that probiotics could increase the number of people with overall symptom improvement (RR = 1.62, 95% CI [1.10, 2.38], <jats:italic>P</jats:italic> = 0.01) and shorten the duration (days) of overall symptoms (MD = −1.26, 95% CI [−2.36, −0.16], <jats:italic>P</jats:italic> = 0.02). For the duration (days) of specific symptoms, probiotics could improve diarrhea (MD = −2.12, 95% CI [−2.41, −1.83], <jats:italic>P</jats:italic> &lt; 0.00001), cough (MD = −2.21, 95% CI [-4.56, 0.13], <jats:italic>P</jats:italic> = 0.06) and shortness of breath (MD = −1.37, 95% CI [-2.22, −0.53], P = 0.001). Probiotics had no obvious effect on fever, headache and weakness. For inflammation, probiotics could effectively reduce C-reactive Protein (CRP) serum level (mg/L) (MD = −4.03, 95% CI [−5.12, −2.93], <jats:italic>P</jats:italic> &lt; 0.00001). Regarding hospital stay (days), probiotics group was shorter than non-probiotics group (MD = −0.98, 95% CI [−1.95, −0.01], <jats:italic>P</jats:italic> = 0.05).</jats:p></jats:sec><jats:sec><jats:title>Conclusion</jats:title><jats:p>To some extent probiotics could improve the overall symptoms, inflammatory reaction and shorten hospital stay of patients with COVID-19. Probiotics may improve gastrointestinal symptoms (such as improving intestinal flora and reducing the duration of diarrhea) and further improve respiratory symptoms through the gut-lung axis.</jats:p></jats:sec><jats:sec><jats:title>Systematic review registration</jats:title><jats:p><jats:ext-link>https://www.crd.york.ac.uk/PROSPERO/display_record.php?RecordID=398309</jats:ext-link>, identifier: CRD42023398309.</jats:p></jats:sec>",
"alternative-id": [
"10.3389/fnut.2023.1179432"
],
"author": [
{
"affiliation": [],
"family": "Tian",
"given": "Yong",
"sequence": "first"
},
{
"affiliation": [],
"family": "Ran",
"given": "Hongmei",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Wen",
"given": "Xudong",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Fu",
"given": "Guochuan",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Zhou",
"given": "Xiaofang",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Liu",
"given": "Rui",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Pan",
"given": "Tao",
"sequence": "additional"
}
],
"container-title": "Frontiers in Nutrition",
"container-title-short": "Front. Nutr.",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"frontiersin.org"
]
},
"created": {
"date-parts": [
[
2023,
5,
22
]
],
"date-time": "2023-05-22T04:47:54Z",
"timestamp": 1684730874000
},
"deposited": {
"date-parts": [
[
2023,
5,
22
]
],
"date-time": "2023-05-22T04:47:58Z",
"timestamp": 1684730878000
},
"funder": [
{
"DOI": "10.13039/501100004829",
"award": [
"2021YJ0198"
],
"doi-asserted-by": "publisher",
"name": "Department of Science and Technology of Sichuan Province"
},
{
"DOI": "10.13039/501100008402",
"award": [
"YYZX2020036"
],
"doi-asserted-by": "publisher",
"name": "Chengdu University of Traditional Chinese Medicine"
}
],
"indexed": {
"date-parts": [
[
2024,
1,
5
]
],
"date-time": "2024-01-05T06:06:20Z",
"timestamp": 1704434780204
},
"is-referenced-by-count": 3,
"issued": {
"date-parts": [
[
2023,
5,
22
]
]
},
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
5,
22
]
],
"date-time": "2023-05-22T00:00:00Z",
"timestamp": 1684713600000
}
}
],
"link": [
{
"URL": "https://www.frontiersin.org/articles/10.3389/fnut.2023.1179432/full",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1965",
"original-title": [],
"prefix": "10.3389",
"published": {
"date-parts": [
[
2023,
5,
22
]
]
},
"published-online": {
"date-parts": [
[
2023,
5,
22
]
]
},
"publisher": "Frontiers Media SA",
"reference": [
{
"DOI": "10.1136/bmj.m1996",
"article-title": "Characterization and clinical course of 1000 patients with coronavirus disease 2019 in New York: retrospective case series",
"author": "Argenziano M",
"doi-asserted-by": "publisher",
"first-page": "m1996",
"journal-title": "BMJ.",
"key": "B1",
"volume": "369",
"year": "2020"
},
{
"DOI": "10.3390/ijerph182010644",
"article-title": "A comprehensive descriptive epidemiological and clinical analysis of SARS-CoV-2 in west-Mexico during COVID-19 pandemic 2020",
"author": "Viera-Segura",
"doi-asserted-by": "publisher",
"first-page": "20",
"journal-title": "Int J Environ Res Public Health.",
"key": "B2",
"volume": "18",
"year": "2021"
},
{
"DOI": "10.3389/fimmu.2021.635471",
"article-title": "Microbiota modulation of the gut-lung axis in COVID-19",
"author": "de Oliveira",
"doi-asserted-by": "publisher",
"first-page": "635471",
"journal-title": "Front Immunol.",
"key": "B3",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.1016/j.micpath.2020.104452",
"article-title": "Ghaemi A. The immunomodulatory effects of probiotics on respiratory viral infections: A hint for COVID-19 treatment?",
"author": "Mahooti",
"doi-asserted-by": "publisher",
"first-page": "104452",
"journal-title": "Microb Pathog.",
"key": "B4",
"volume": "148",
"year": "2020"
},
{
"DOI": "10.1080/17450399009428406",
"article-title": "Probiotics in animal nutrition: a review",
"author": "Vanbelle",
"doi-asserted-by": "publisher",
"first-page": "543",
"journal-title": "Archiv für Tierernährung.",
"key": "B5",
"volume": "40",
"year": "1990"
},
{
"DOI": "10.1186/s12876-022-02187-z",
"article-title": "Investigating the effect of quadruple therapy with Saccharomyces boulardii or Lactobacillus reuteri strain (DSMZ 17648) supplements on eradication of Helicobacter pylori and treatments adverse effects: a double-blind placebo-controlled randomized clinical trial",
"author": "Naghibzadeh",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "BMC Gastroenterol.",
"key": "B6",
"volume": "22",
"year": "2022"
},
{
"DOI": "10.1186/s12890-022-02078-9",
"article-title": "Gut Bifidobacteria enrichment following oral Lactobacillus-supplementation is associated with clinical improvements in children with cystic fibrosis",
"author": "Ray K",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "BMC Pulm Med.",
"key": "B7",
"volume": "22",
"year": "2022"
},
{
"DOI": "10.1111/eci.13108",
"article-title": "The beneficial effects of a novel formulation of Bifidobacterium longum BB536 and Lactobacillus rhamnosus HN001 with B6 vitamin on gut microbiota and intestinal permeability in IBS patients",
"author": "Bonfrate",
"doi-asserted-by": "publisher",
"first-page": "81",
"journal-title": "Eur J Clin Invest.",
"key": "B8",
"volume": "49",
"year": "2019"
},
{
"DOI": "10.3390/molecules25214891",
"article-title": "Probiotics in treatment of viral respiratory infections and neuroinflammatory disorders",
"author": "Shahbazi",
"doi-asserted-by": "publisher",
"first-page": "21",
"journal-title": "Molecules.",
"key": "B9",
"volume": "25",
"year": "2020"
},
{
"DOI": "10.1159/000526739",
"article-title": "Multistrain probiotics supplement alleviates asthma symptoms via increasing Treg cells population: A randomized, double-blind, placebo-controlled trial",
"author": "Abbasi-Dokht",
"doi-asserted-by": "publisher",
"first-page": "291",
"journal-title": "Int Arch Allergy Immunol.",
"key": "B10",
"volume": "184",
"year": "2023"
},
{
"DOI": "10.1186/s12967-022-03337-3",
"article-title": "Study effect of probiotics and prebiotics on treatment of OVA-LPS-induced of allergic asthma inflammation and pneumonia by regulating the TLR4/NF-kB signaling pathway",
"author": "Wu",
"doi-asserted-by": "publisher",
"first-page": "3",
"journal-title": "J. Transl Med.",
"key": "B11",
"volume": "20",
"year": "2022"
},
{
"DOI": "10.1016/j.archger.2022.104721",
"article-title": "multistrain probiotic improves handgrip strength and functional capacity in patients with COPD: a randomized controlled trial",
"author": "Karim",
"doi-asserted-by": "publisher",
"first-page": "102",
"journal-title": "Arch Gerontol Geriatr.",
"key": "B12",
"volume": "10",
"year": "2022"
},
{
"DOI": "10.1123/ijsnem.2018-0377",
"article-title": "The effects of plasmacytoid dendritic cell-stimulative lactic acid bacteria, Lactococcus lactis strain plasma, on exercise-induced fatigue and recovery via immunomodulatory action",
"author": "Kokubo",
"doi-asserted-by": "publisher",
"first-page": "354",
"journal-title": "Int J Sport Nutr Exerc Metab.",
"key": "B13",
"volume": "29",
"year": "2019"
},
{
"DOI": "10.1016/j.jmii.2014.07.011",
"article-title": "Oral intake of Lactobacillus rhamnosus M21 enhances the survival rate of mice lethally infected with influenza virus",
"author": "Song J",
"doi-asserted-by": "publisher",
"first-page": "16",
"journal-title": "J Microbiol Immunol Inf.",
"key": "B14",
"volume": "49",
"year": "2016"
},
{
"DOI": "10.1186/cc10579",
"article-title": "Effects of probiotics on serum levels of Th1/Th2 cytokine and clinical outcomes in severe traumatic brain-injured patients: a prospective randomized pilot study",
"author": "Tan",
"doi-asserted-by": "publisher",
"first-page": "6",
"journal-title": "Critical Care.",
"key": "B15",
"volume": "15",
"year": "2011"
},
{
"DOI": "10.3390/nu14224856",
"article-title": "Transepithelial effect of probiotics in a novel model of gut lumen to nerve signaling",
"author": "Piletz J",
"doi-asserted-by": "publisher",
"first-page": "22",
"journal-title": "Nutrients.",
"key": "B16",
"volume": "14",
"year": "2022"
},
{
"DOI": "10.1007/s00253-020-10832-4",
"article-title": "Role of probiotics to combat viral infections with emphasis on COVID-19",
"author": "Sundararaman",
"doi-asserted-by": "publisher",
"first-page": "8089",
"journal-title": "Appl Microbiol Biotechnol.",
"key": "B17",
"volume": "104",
"year": "2020"
},
{
"DOI": "10.3390/microorganisms10091764",
"article-title": "Immunomodulatory effects of probiotics on COVID-19 infection by targeting the gut-lung axis microbial cross-talk",
"author": "Synodinou K",
"doi-asserted-by": "publisher",
"first-page": "9",
"journal-title": "Microorganisms.",
"key": "B18",
"volume": "10",
"year": "2022"
},
{
"DOI": "10.7326/0003-4819-151-4-200908180-00135",
"article-title": "Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement",
"author": "Moher",
"doi-asserted-by": "publisher",
"first-page": "264",
"journal-title": "Ann Intern Med",
"key": "B19",
"volume": "151",
"year": "2009"
},
{
"DOI": "10.1177/0962280216669183",
"article-title": "Optimally estimating the sample mean from the sample size, median, mid-range, and/or mid-quartile range",
"author": "Luo",
"doi-asserted-by": "publisher",
"first-page": "1785",
"journal-title": "Stat Methods Med Res.",
"key": "B20",
"volume": "27",
"year": "2018"
},
{
"DOI": "10.1186/1471-2288-14-135",
"article-title": "Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range",
"author": "Wan",
"doi-asserted-by": "publisher",
"first-page": "135",
"journal-title": "BMC Med Res Methodol.",
"key": "B21",
"volume": "14",
"year": "2014"
},
{
"DOI": "10.1007/s12602-021-09858-5",
"article-title": "Efficacy of a probiotic consisting of Lacticaseibacillus rhamnosus PDV 1705, Bifidobacterium bifidum PDV 0903, Bifidobacterium longum subsp. infantis PDV 1911, and Bifidobacterium longum subsp. longum PDV 2301 in the treatment of hospitalized patients with COVID-19: a randomized controlled trial",
"author": "Ivashkin",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "Probiotics Antimicrob Proteins.",
"key": "B22",
"volume": "13",
"year": "2021"
},
{
"DOI": "10.1080/19490976.2021.2018899",
"article-title": "Probiotic improves symptomatic and viral clearance in Covid19 outpatients: a randomized, quadruple-blinded, placebo-controlled trial",
"author": "Gutiérrez-Castrellón",
"doi-asserted-by": "publisher",
"first-page": "2018899",
"journal-title": "Gut Microbes.",
"key": "B23",
"volume": "14",
"year": "2022"
},
{
"DOI": "10.21037/apm-21-3373",
"article-title": "The efficacy of probiotics in patients with severe COVID-19",
"author": "Wang",
"doi-asserted-by": "publisher",
"first-page": "12374",
"journal-title": "Ann Palliat Med.",
"key": "B24",
"volume": "10",
"year": "2021"
},
{
"DOI": "10.1177/17562848211035670",
"article-title": "Probiotics use is associated with improved clinical outcomes among hospitalized patients with COVID-19",
"author": "Zhang",
"doi-asserted-by": "publisher",
"first-page": "1088218646",
"journal-title": "Therap Adv Gastroenterol.",
"key": "B25",
"volume": "14",
"year": "2021"
},
{
"DOI": "10.1016/j.medmic.2022.100061",
"article-title": "Oral intake of Kluyveromyces marxianus B0399 plus Lactobacillus rhamnosus CECT 30579 to mitigate symptoms in COVID-19 patients: a randomized open label clinical trial",
"author": "Navarro-López",
"doi-asserted-by": "publisher",
"first-page": "100061",
"journal-title": "Med Microecol.",
"key": "B26",
"volume": "14",
"year": "2022"
},
{
"DOI": "10.1101/2022.01.04.21268275",
"article-title": "Daily lactobacillus probiotic versus placebo in COVID-19-exposed household contacts (PROTECT-EHC)",
"author": "Wischmeyer P",
"doi-asserted-by": "publisher",
"first-page": "2022",
"journal-title": "Clin Trial.",
"key": "B27",
"volume": "1",
"year": "2022"
},
{
"DOI": "10.3390/jcm11133758",
"article-title": "COVID-19 pneumonia and gut inflammation: the role of a mix of three probiotic strains in reducing inflammatory markers and need for oxygen support",
"author": "Saviano",
"doi-asserted-by": "publisher",
"first-page": "13",
"journal-title": "J Clin Med.",
"key": "B28",
"volume": "11",
"year": "2022"
},
{
"DOI": "10.26442/00403660.2021.04.200835",
"article-title": "[Efficiency of application of sorbed probiotics in complex therapy of pneumonia caused by SARS-CoV-2. Part 1 Heating clinical displays period]",
"author": "Meskina",
"doi-asserted-by": "publisher",
"first-page": "456",
"journal-title": "Ter Arkh.",
"key": "B29",
"volume": "93",
"year": "2021"
},
{
"DOI": "10.26442/00403660.2022.10.201881",
"article-title": "[Efficacy of Saccharomyces boulardii CNCM I-745 probiotic drug in the prevention and treatment of diarrhea in hospitalized patients with new coronavirus infection COVID-19]",
"author": "Maev I",
"doi-asserted-by": "publisher",
"first-page": "1163",
"journal-title": "Ter Arkh.",
"key": "B30",
"volume": "94",
"year": "2022"
},
{
"DOI": "10.1002/jmv.28463",
"article-title": "The effect of synbiotic adjunct therapy on clinical and paraclinical outcomes in hospitalized COVID-19 patients: A randomized placebo-controlled trial",
"author": "Vaezi",
"doi-asserted-by": "publisher",
"journal-title": "J Med Virol.",
"key": "B31",
"year": "2023"
},
{
"DOI": "10.1016/S0140-6736(20)30251-8",
"article-title": "Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding",
"author": "Lu",
"doi-asserted-by": "publisher",
"first-page": "565",
"journal-title": "Lancet.",
"key": "B32",
"volume": "395",
"year": "2020"
},
{
"DOI": "10.1016/j.virusres.2020.198018",
"article-title": "Gut microbiota and Covid-19- possible link and implications",
"author": "Dhar",
"doi-asserted-by": "publisher",
"first-page": "198018",
"journal-title": "Virus Res.",
"key": "B33",
"volume": "285",
"year": "2020"
},
{
"DOI": "10.1016/j.scitotenv.2020.140444",
"article-title": "SARS-CoV-2 from faeces to wastewater treatment: What do we know?",
"author": "Foladori",
"doi-asserted-by": "publisher",
"first-page": "140444",
"journal-title": "A review Sci Total Environ.",
"key": "B34",
"volume": "743",
"year": "2020"
},
{
"article-title": "Prevalence of gastrointestinal symptoms in coronavirus disease 2019: a meta-analysis",
"author": "Merola",
"first-page": "603",
"journal-title": "Acta Gastroenterol Belg.",
"key": "B35",
"volume": "83",
"year": "2020"
},
{
"DOI": "10.7759/cureus.7422",
"article-title": "Gastrointestinal infection could be new focus for coronavirus diagnosis",
"author": "Cipriano",
"doi-asserted-by": "publisher",
"first-page": "e7422",
"journal-title": "Cureus.",
"key": "B36",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1016/j.rgmxen.2020.04.001",
"article-title": "Beware: Gastrointestinal symptoms can be a manifestation of COVID-19",
"author": "Schmulson",
"doi-asserted-by": "publisher",
"first-page": "282",
"journal-title": "Rev Gastroenterol Mex.",
"key": "B37",
"volume": "85",
"year": "2020"
},
{
"DOI": "10.1080/09637486.2020.1807475",
"article-title": "Probiotics and Covid-19",
"author": "Bottari",
"doi-asserted-by": "publisher",
"first-page": "293",
"journal-title": "Int J Food Sci Nutr.",
"key": "B38",
"volume": "72",
"year": "2021"
},
{
"DOI": "10.3390/v14081774",
"article-title": "An update on the mutual impact between SARS-CoV-2 infection and gut microbiota",
"author": "Li",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "Viruses.",
"key": "B39",
"volume": "14",
"year": "2022"
},
{
"DOI": "10.1186/s12879-022-07358-7",
"article-title": "Longitudinal alterations of the gut mycobiota and microbiota on COVID-19 severity",
"author": "Maeda",
"doi-asserted-by": "publisher",
"first-page": "572",
"journal-title": "BMC Infect Dis.",
"key": "B40",
"volume": "22",
"year": "2022"
},
{
"DOI": "10.3748/wjg.v28.i45.6328",
"article-title": "Gastrointestinal microbiota: a predictor of COVID-19 severity?",
"author": "Neag",
"doi-asserted-by": "publisher",
"first-page": "6328",
"journal-title": "World J Gastroenterol.",
"key": "B41",
"volume": "28",
"year": "2022"
},
{
"DOI": "10.3389/fmed.2022.811176",
"article-title": "Modulated gut microbiota for potential COVID-19 prevention and treatment",
"author": "Zhao",
"doi-asserted-by": "publisher",
"first-page": "811176",
"journal-title": "Front Med.",
"key": "B42",
"volume": "9",
"year": "2022"
},
{
"DOI": "10.3390/nu14010228",
"article-title": "Effects of Loigolactobacillus coryniformis K8 CECT 5711 on the immune response of elderly subjects to COVID-19 vaccination: a randomized controlled trial",
"author": "Fernández-Ferreiro",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "Nutrients.",
"key": "B43",
"volume": "14",
"year": "2022"
},
{
"DOI": "10.1080/07391102.2020.1775123",
"article-title": "Antiviral effects of probiotic metabolites on COVID-19",
"author": "Anwar",
"doi-asserted-by": "publisher",
"first-page": "4175",
"journal-title": "J Biomol Struct Dyn.",
"key": "B44",
"volume": "39",
"year": "2021"
},
{
"DOI": "10.1016/j.tifs.2021.12.033",
"article-title": "Evidences and perspectives of the use of probiotics, prebiotics, synbiotics, and postbiotics as adjuvants for prevention and treatment of COVID-19: a bibliometric analysis and systematic review",
"author": "Xavier-Santos",
"doi-asserted-by": "publisher",
"first-page": "174",
"journal-title": "Trends Food Sci Technol.",
"key": "B45",
"volume": "120",
"year": "2022"
},
{
"DOI": "10.1080/10408398.2022.2128713",
"article-title": "Benefits of probiotic use on COVID-19: A systematic review and meta-analysis",
"author": "Neris",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "Crit Rev Food Sci Nutr.",
"key": "B46",
"volume": "5",
"year": "2022"
},
{
"DOI": "10.4103/ijpm.ijpm_658_21",
"article-title": "Significance of immune-inflammatory markers in predicting clinical outcome of COVID-19 patients Indian",
"author": "Singh",
"doi-asserted-by": "publisher",
"first-page": "111",
"journal-title": "J Pathol Microbiol.",
"key": "B47",
"volume": "66",
"year": "2023"
},
{
"DOI": "10.1177/1753466620937175",
"article-title": "C-reactive protein, procalcitonin, D-dimer, and ferritin in severe coronavirus disease-2019: a meta-analysis",
"author": "Huang",
"doi-asserted-by": "publisher",
"first-page": "1022295081",
"journal-title": "Ther Adv Respir Dis.",
"key": "B48",
"volume": "14",
"year": "2020"
},
{
"DOI": "10.1155/2021/5557582",
"article-title": "C-reactive protein as a prognostic indicator in COVID-19 patients",
"author": "Sadeghi-Haddad-Zavareh",
"doi-asserted-by": "publisher",
"first-page": "5557582",
"journal-title": "Interdiscip Perspect Infect Dis.",
"key": "B49",
"volume": "2021",
"year": "2021"
},
{
"DOI": "10.3390/nu13092919",
"article-title": "Potential roe of probiotics for inflammaging: a narrative review",
"author": "Peladic",
"doi-asserted-by": "publisher",
"first-page": "9",
"journal-title": "Nutrients.",
"key": "B50",
"volume": "13",
"year": "2021"
},
{
"DOI": "10.2478/sjph-2022-0027",
"article-title": "Length of hospital stay and survival of hospitalized COVID-19 patients during the second wave of the pandemic: a single centre retrospective study from slovenia",
"author": "Rozman",
"doi-asserted-by": "publisher",
"first-page": "201",
"journal-title": "Zdr Varst.",
"key": "B51",
"volume": "61",
"year": "2022"
},
{
"DOI": "10.1101/2022.01.27.22269602",
"article-title": "Risk factors and survival in patients with COVID-19 in northeastern Brazil",
"author": "Fernandes A",
"doi-asserted-by": "publisher",
"first-page": "e278213",
"journal-title": "PLoS ONE.",
"key": "B52",
"volume": "17",
"year": "2022"
},
{
"DOI": "10.1186/1477-7525-11-211",
"article-title": "Patient-reported outcomes in meta-analyses-part 2: methods for improving interpretability for decision-makers",
"author": "Johnston B",
"doi-asserted-by": "publisher",
"first-page": "211",
"journal-title": "Health Qual Life Outcomes.",
"key": "B53",
"volume": "11",
"year": "2013"
},
{
"DOI": "10.1016/0197-2456(89)90005-6",
"article-title": "Measurement of health status. Ascertaining the minimal clinically important difference Control",
"author": "Jaeschke",
"doi-asserted-by": "publisher",
"first-page": "407",
"journal-title": "Clin Trials.",
"key": "B54",
"volume": "10",
"year": "1989"
}
],
"reference-count": 54,
"references-count": 54,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.frontiersin.org/articles/10.3389/fnut.2023.1179432/full"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Nutrition and Dietetics",
"Endocrinology, Diabetes and Metabolism",
"Food Science"
],
"subtitle": [],
"title": "Probiotics improve symptoms of patients with COVID-19 through gut-lung axis: a systematic review and meta-analysis",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.3389/crossmark-policy",
"volume": "10"
}