A multicenter, real-world cohort study: effectiveness and safety of Azvudine in hospitalized COVID-19 patients with pre-existing diabetes
et al., Frontiers in Endocrinology, doi:10.3389/fendo.2025.1467303, Feb 2025
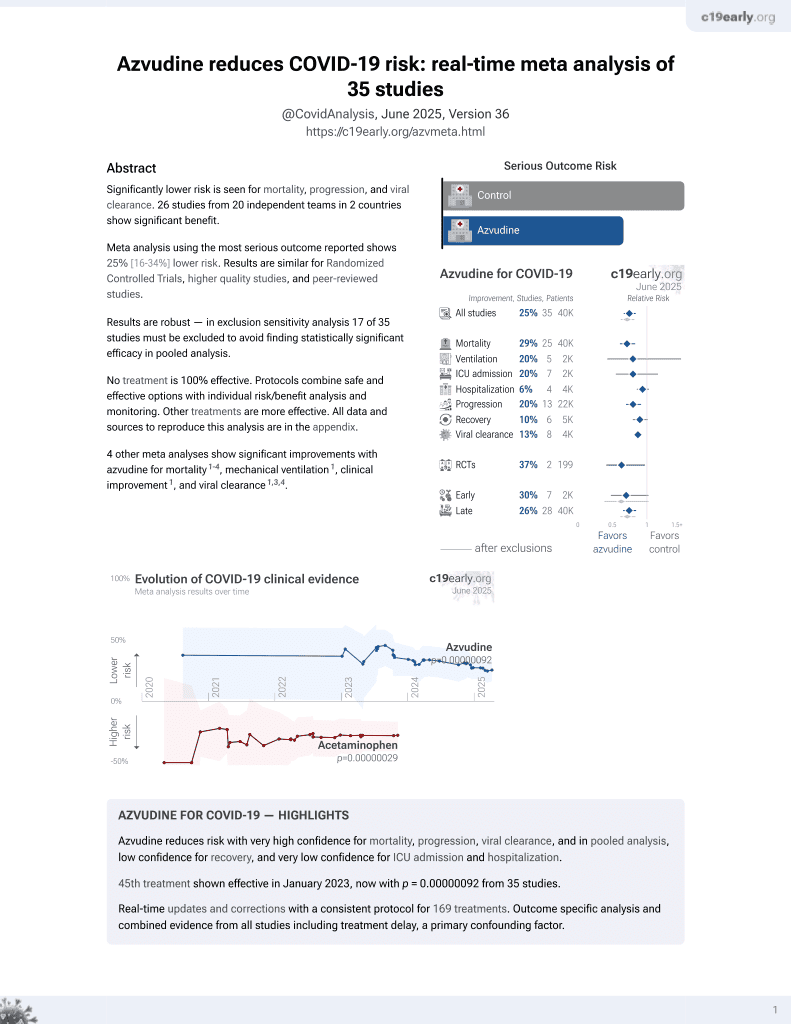
Azvudine for COVID-19
48th treatment shown to reduce risk in
January 2023, now with p = 0.000000017 from 39 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
PSM retrospective 2,834 hospitalized COVID-19 patients with pre-existing diabetes in China showing lower all-cause mortality with azvudine, but no significant difference in composite disease progression.
Standard of Care (SOC) for COVID-19 in the study country,
China, is average with moderate efficacy for approved treatments3.
|
risk of death, 26.0% lower, HR 0.74, p = 0.01, treatment 1,417, control 1,417, adjusted per study, propensity score matching, multivariable, Cox proportional hazards.
|
|
risk of progression, 9.0% lower, HR 0.91, p = 0.35, treatment 1,417, control 1,417, adjusted per study, propensity score matching, multivariable, Cox proportional hazards.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
1.
Xiong et al., Real-world data of Azvudine-induced hepatotoxicity among hospitalized COVID-19 patients in China: a retrospective case-control study, Frontiers in Pharmacology, doi:10.3389/fphar.2025.1558054.
Zhou et al., 18 Feb 2025, retrospective, China, peer-reviewed, 15 authors, study period 5 December, 2022 - 31 January, 2023.
A multicenter, real-world cohort study: effectiveness and safety of Azvudine in hospitalized COVID-19 patients with pre-existing diabetes
doi:10.3389/fendo.2025.1467303
Introduction: During the Omicron infection wave, diabetic patients are susceptible to COVID-19, which is linked to a poor prognosis. However, research on the real-world effectiveness and safety of Azvudine, a common medication for COVID-19, is insufficient in those with pre-existing diabetes. Methods: In this retrospective study, we included 32,864 hospitalized COVID-19 patients from 9 hospitals in Henan Province. Diabetic patients were screened and divided into the Azvudine group and the control group, via 1:1 propensity score matching. The primary outcome was all-cause mortality, and the secondary outcome was composite disease progression. Laboratory abnormal results were used for safety evaluation. Results: A total of 1,417 patients receiving Azvudine and 1,417 patients receiving standard treatment were ultimately included. Kaplan-Meier curves suggested that all-cause mortality (P = 0.0026) was significantly lower in the Azvudine group than in the control group, but composite disease progression did not significantly differ (P = 0.1). Cox regression models revealed Azvudine treatment could reduce 26% risk of all-cause mortality (95% CI: 0.583-0.942, P = 0.015) versus controls, and not reduce the risk of composite disease progression (HR: 0.91, 95% CI: 0.750-1.109, P = 0.355). The results of subgroup analysis and three sensitivity analyses were consistent with the previous findings. Safety analysis revealed that the incidence rates of most adverse events were similar between the two groups.
Ethics statement The study was approved by the Ethics Committee of the First Affiliated Hospital of Zhengzhou University (2023-KY-0865-001). The studies were conducted in accordance with the local legislation and institutional requirements. The ethics committee/institutional review board waived the requirement of written informed consent for participation from the participants or the participants' legal guardians/next of kin because the private information of all patients was not disclosed in this retrospective study, the Ethics Committee of the First Affiliated Hospital of Zhengzhou University approved the waiver of obtaining informed consent.
Author contributions
Conflict of interest The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fendo.2025.1467303/ full#supplementary-material
References
Arbel, Sagy, Hoshen, Battat, Lavie et al., Nirmatrelvir use and severe covid-19 outcomes during the omicron surge, N Engl J Med, doi:10.1056/NEJMoa2204919
Bernal, Da Silva, Musungaie, Kovalchuk, Gonzalez et al., Molnupiravir for oral treatment of covid-19 in nonhospitalized patients, N Engl J Med, doi:10.1056/NEJMoa2116044
Bode, Garrett, Messler, Mcfarland, Crowe et al., Glycemic characteristics and clinical outcomes of COVID-19 patients hospitalized in the United States, J Diabetes Sci Technol, doi:10.1177/1932296820924469
Brufsky, Hyperglycemia, hydroxychloroquine, and the COVID-19 pandemic, J Med Virol, doi:10.1002/jmv.25887
Caretto, Terlizzi, Pedone, Pennella, Cobelli et al., Tight and stable glucose control is associated with better prognosis in patients hospitalized for covid-19 and pneumonia, Acta Diabetol, doi:10.1007/s00592-024-02409-8
Cariou, Hadjadj, Wargny, Pichelin, Al-Salameh et al., Phenotypic characteristics and prognosis of inpatients with COVID-19 and diabetes: The CORONADO study, Diabetologia, doi:10.1007/s00125-020-05180-x
Codo, Davanzo, Monteiro, De, De Souza et al., Elevated glucose levels favor SARS-CoV-2 infection and monocyte response through a HIF-1a/glycolysis-dependent axis, Cell Metab, doi:10.1016/j.cmet.2020.07.007
De Souza, Cabral, Da Silva, Arruda, Sp De et al., randomized, double-blind, placebo-controlled clinical study: A study on the safety and clinical efficacy of AZVUDINE in moderate COVID-19 patients, Front Med, doi:10.3389/fmed.2023.1215916
Garcia-Beltran, Lam, Denis, Nitido, Garcia et al., Multiple SARS-CoV-2 variants escape neutralization by vaccine-induced humoral immunity, Cell, doi:10.1016/j.cell.2021.03.013
Gregory, Slaughter, Duffus, Smith, Lestourgeon et al., COVID-19 severity is tripled in the diabetes community: A prospective analysis of the pandemic's impact in type 1 and type 2 diabetes, Diabetes Care, doi:10.2337/dc20-2260
Gutieŕrez-Calderoń, Sarti, COVID-19 vaccination hesitancy in Mexico city among healthy adults and adults with chronic diseases: A survey of complacency, confidence, and convenience challenges in the transition to endemic control, Vaccines, doi:10.3390/vaccines10111944
Han, Du, Deng, Tang, Dong et al., Real-world effectiveness and safety of simnotrelvir/ritonavir for COVID-19: A nationwide, multicenter, prospective, observational cohort study in China, J Infect, doi:10.1016/j.jinf.2024.106339
Laurenzi, Caretto, Molinari, Bazzigaluppi, Brigatti et al., Pre-existing diabetes and COVID-associated hyperglycaemia in patients with COVID-19 pneumonia, Biology, doi:10.3390/biology10080754
Li, Shen, Yang, Fairley, Chai et al., Global diabetes prevalence in COVID-19 patients and contribution to COVID-19-related severity and mortality: A systematic review and meta-analysis, Diabetes Care, doi:10.2337/dc22-1943
Lim, Bae, Kwon, Nauck, COVID-19 and diabetes mellitus: From pathophysiology to clinical management, Nat Rev Endocrinol, doi:10.1038/s41574-020-00435-4
Michalakis, Ilias, COVID-19 and hyperglycemia/diabetes, World J Diabetes, doi:10.4239/wjd.v12.i5.642
Montefusco, Nasr, 'addio, Loretelli, Rossi et al., Acute and long-term disruption of glycometabolic control after SARS-CoV-2 infection, Nat Metab, doi:10.1038/s42255-021-00407-6
Prete, Favoino, Catacchio, Racanelli, Perosa, SARS-CoV-2 inflammatory syndrome. Clinical features and rationale for immunological treatment, Int J Mol Sci, doi:10.3390/ijms21093377
Ren, Luo, Yu, Song, Liang et al., A randomized, open-label, controlled clinical trial of azvudine tablets in the treatment of mild and common COVID-19, a pilot study, Adv Sci, doi:10.1002/advs.202001435
Seyit, Avci, Nar, Senol, Yilmaz et al., Neutrophil to lymphocyte ratio, lymphocyte to monocyte ratio and platelet to lymphocyte ratio to predict the severity of COVID-19, Am J Emerg Med, doi:10.1016/j.ajem.2020.11.058
Shi, Zhang, Jiang, Zhang, Hu et al., Clinical characteristics and risk factors for mortality of COVID-19 patients with diabetes in wuhan, China: A two-center, retrospective study, Diabetes Care, doi:10.2337/dc20-0598
Singh, Gillies, Singh, Singh, Chudasama et al., Prevalence of co-morbidities and their association with mortality in patients with COVID-19: A systematic review and meta-analysis, Diabetes Obes Metab, doi:10.1111/dom.v22.10
Sun, Dian, Shen, Zeng, Chen, Oral azvudine for hospitalised patients with COVID-19 and pre-existing conditions: A retrospective cohort study, EClinicalMedicine, doi:10.1016/j.eclinm.2023.101981
Who, WHO COVID-19 dashboard
Who, WHO recommends highly successful COVID-19 therapy and calls for wide geographical distribution and transparency from originator
Who, WHO updates its treatment guidelines to include molnupiravir
Wu, He, Huang, Guo, Li et al., Azvudine for the treatment of COVID-19 in pre-existing cardiovascular diseases: A single-center, real-world experience, Adv Sci, doi:10.1002/advs.202306050
Wu, Mcgoogan, Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: Summary of a report of 72 314 cases from the Chinese center for disease control and prevention, JAMA, doi:10.1001/jama.2020.2648
Yang, Wang, Bench-to-bedside: Innovation of small molecule anti-SARS-CoV-2 drugs in China, Eur J Med Chem, doi:10.1016/j.ejmech.2023.115503
Yu, Chang, The first Chinese oral anti-COVID-19 drug azvudine launched, Innovation, doi:10.1016/j.xinn.2022.100321
Yu, Li, Sun, Wang, Insulin treatment is associated with increased mortality in patients with COVID-19 and type 2 diabetes, Cell Metab, doi:10.1016/j.cmet.2020.11.014
Zhang, Li, Wang, Liu, Lu et al., Azvudine is a thymushoming anti-SARS-CoV-2 drug effective in treating COVID-19 patients, Signal Transduct Target Ther, doi:10.1038/s41392-021-00835-6
Zheng, Ma, Wang, Cheng, Zhou et al., Efficacy and safety of paxlovid for COVID-19:A meta-analysis, J Infect, doi:10.1016/j.jinf.2022.09.027
Zhu, Feng, Jiang, Mi, Yang et al., Correlation between white blood cell count at admission and mortality in COVID-19 patients: A retrospective study, BMC Infect Dis, doi:10.1186/s12879-021-06277-3
Zhu, She, Cheng, Qin, Zhang et al., Association of blood glucose control and outcomes in patients with COVID-19 and pre-existing type 2 diabetes, Cell Metab, doi:10.1016/j.cmet.2020.04.021
Zong, Zhou, Li, Jiang, Liu et al., Azvudine reduces the in-hospital mortality of COVID-19 patients: A retrospective cohort study, Acta Pharm Sin B, doi:10.1016/j.apsb.2023.07.007