Folic acid restricts SARS-CoV-2 invasion by methylating ACE2
et al., Frontiers in Microbiology, doi:10.3389/fmicb.2022.980903, Aug 2022
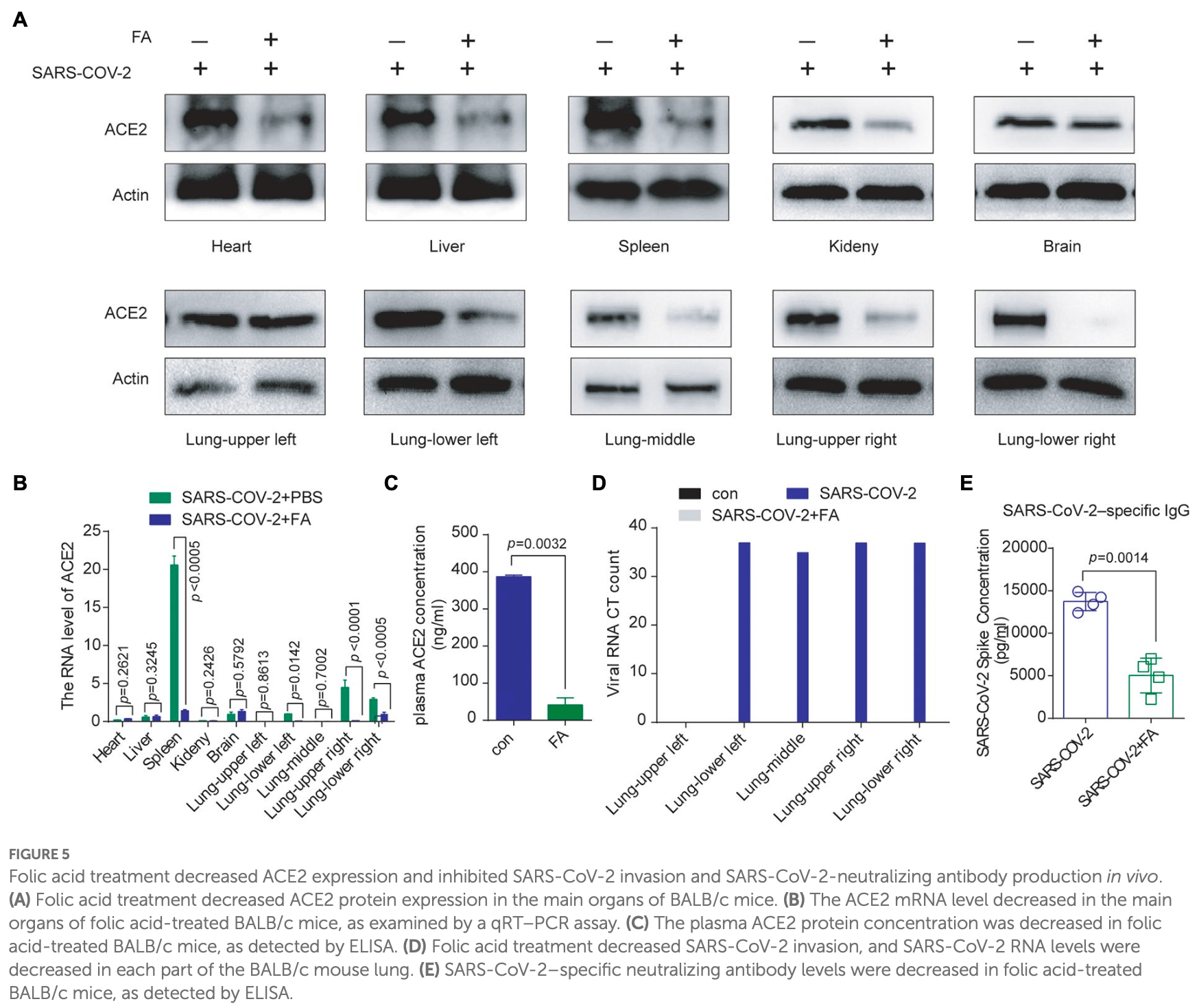
In vitro and mouse study showing that folic acid decreased ACE2 expression and inhibited SARS-CoV-2.
14 preclinical studies support the efficacy of vitamin B9 for COVID-19:
Vitamin B9 has been identified by the European Food Safety Authority (EFSA) as having sufficient evidence for a causal relationship between intake and optimal immune system function12-14.
Vitamin B9 inhibits SARS-CoV-2 in silico3-11, reduces spike protein binding ability11, binds with the spike protein receptor binding domain for alpha and omicron variants2, inhibits the SARS-CoV-2 nucleocapsid protein3, inhibits 3CLpro and PLpro in enzymatic assays2, significantly reduces infection for alpha and omicron SARS-CoV-2 pseudoviruses2, and inhibits ACE2 expression and SARS-CoV-2 infection in a mouse model11.
1.
Wu et al., Biomarkers Prediction and Immune Landscape in Covid-19 and “Brain Fog”, Elsevier BV, doi:10.2139/ssrn.4897774.
2.
Pennisi et al., An Integrated In Silico and In Vitro Approach for the Identification of Natural Products Active against SARS-CoV-2, Biomolecules, doi:10.3390/biom14010043.
3.
Chen et al., Folic acid: a potential inhibitor against SARS-CoV-2 nucleocapsid protein, Pharmaceutical Biology, doi:10.1080/13880209.2022.2063341.
4.
Eskandari, V., Repurposing the natural compounds as potential therapeutic agents for COVID-19 based on the molecular docking study of the main protease and the receptor-binding domain of spike protein, Journal of Molecular Modeling, doi:10.1007/s00894-022-05138-3.
5.
Pandya et al., Unravelling Vitamin B12 as a potential inhibitor against SARS-CoV-2: A computational approach, Informatics in Medicine Unlocked, doi:10.1016/j.imu.2022.100951.
6.
Serseg et al., Hispidin and Lepidine E: Two Natural Compounds and Folic Acid as Potential Inhibitors of 2019-novel Coronavirus Main Protease (2019-nCoVMpro), Molecular Docking and SAR Study, Current Computer-Aided Drug Design, doi:10.2174/1573409916666200422075440.
7.
Hosseini et al., Computational molecular docking and virtual screening revealed promising SARS-CoV-2 drugs, Precision Clinical Medicine, doi:10.1093/pcmedi/pbab001.
8.
Ugurel et al., Evaluation of the potency of FDA-approved drugs on wild type and mutant SARS-CoV-2 helicase (Nsp13), International Journal of Biological Macromolecules, doi:10.1016/j.ijbiomac.2020.09.138.
9.
Kumar et al., In silico virtual screening-based study of nutraceuticals predicts the therapeutic potentials of folic acid and its derivatives against COVID-19, VirusDisease, doi:10.1007/s13337-020-00643-6.
10.
Moatasim et al., Potent Antiviral Activity of Vitamin B12 against Severe Acute Respiratory Syndrome Coronavirus 2, Middle East Respiratory Syndrome Coronavirus, and Human Coronavirus 229E, Microorganisms, doi:10.3390/microorganisms11112777.
11.
Zhang et al., Folic acid restricts SARS-CoV-2 invasion by methylating ACE2, Frontiers in Microbiology, doi:10.3389/fmicb.2022.980903.
12.
Galmés et al., Suboptimal Consumption of Relevant Immune System Micronutrients Is Associated with a Worse Impact of COVID-19 in Spanish Populations, Nutrients, doi:10.3390/nu14112254.
13.
Galmés (B) et al., Current State of Evidence: Influence of Nutritional and Nutrigenetic Factors on Immunity in the COVID-19 Pandemic Framework, Nutrients, doi:10.3390/nu12092738.
14.
EFSA, Scientific Opinion on the substantiation of health claims related to folate and blood formation (ID 79), homocysteine metabolism (ID 80), energy-yielding metabolism (ID 90), function of the immune system (ID 91), function of blood vessels (ID 94, 175, 192), cell division (ID 193), and maternal tissue growth during pregnancy (ID 2882) pursuant to Article 13(1) of Regulation (EC) No 1924/2006, EFSA Journal, doi:10.2903/j.efsa.2009.1213.
Zhang et al., 17 Aug 2022, China, peer-reviewed, 7 authors.
Contact: luoxy@shsci.org.
Folic acid restricts SARS-CoV-2 invasion by methylating ACE2
Frontiers in Microbiology, doi:10.3389/fmicb.2022.980903
The current COVID-19 pandemic is motivating us to elucidate the molecular mechanism of SARS-CoV-2 invasion and find methods for decreasing its transmissibility. We found that SARS-CoV-2 could increase the protein level of ACE2 in mice. Folic acid and 5-10-methylenetetrahydrofolate reductase (MTHFR) could promote the methylation of the ACE2 promoter and inhibit ACE2 expression. Folic acid treatment decreased the binding ability of Spike protein, pseudovirus and inactivated authentic SARS-CoV-2 to host cells. Thus, folic acid treatment could decrease SARS-CoV-2 invasion and SARS-CoV-2-neutralizing antibody production in mice. These data suggest that increased intake of folic acid may inhibit ACE2 expression and reduce the transmissibility of SARS-CoV-2. Folic acid could play an important role in SARS-CoV-2 infection prevention and control.
Ethics statement The animal study was reviewed and approved by Institutional Animal Care and Use Committee of Model Animal Research Center of Shanghai Cancer Institute.
Author contributions XL: manuscript editing, review, and data analysis. YZ, YP, and BX: data collection and experiments. XC, SL, and JH: figures preparation. All authors contributed to the article and approved the submitted version.
Conflict of interest The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmicb.2022.980903/ full#supplementary-material
References
Aleksova, Ferro, Gagno, Cappelletto, Santon et al., COVID-19 and renin-angiotensin system inhibition: role of angiotensin converting enzyme 2 (ACE2) -is there any scientific evidence for controversy?, J. Intern. Med, doi:10.1111/joim.13101
Altmann, Boyton, Beale, Immunity to SARS-CoV-2 variants of concern, Science, doi:10.1126/science.abg7404
Artese, Svicher, Costa, Salpini, Di Maio et al., Current status of antivirals and druggable targets of SARS CoV-2 and other human pathogenic coronaviruses, Drug Resist. Updat, doi:10.1016/j.drup.2020.100721
Bae, Kamynina, Guetterman, Farinola, Caudill et al., Provision of folic acid for reducing arsenic toxicity in arsenic-exposed children and adults, Cochrane Database Syst. Rev, doi:10.1002/14651858.CD012649
Bavishi, Maddox, Messerli, Coronavirus disease 2019 (COVID-19) infection and renin angiotensin system blockers, JAMA Cardiol, doi:10.1001/jamacardio.2020.1282
Bueverova, The concept of folic acid in health and disease, Molecules, doi:10.3390/molecules26123731
Bushman, Kahn, Taylor, Lipsitch, Hanage, None
Callaway, Population impact of SARS-CoV-2 variants with enhanced transmissibility and/or partial immune escape, Nature, doi:10.1038/d41586-021-03672-3
Cao, Goreshnik, Coventry, Case, Miller et al., None
Chakraborty, Mallajosyula, Tato, Tan, Wang, De novo design of picomolar SARS-CoV-2 miniprotein inhibitors, Science, doi:10.1126/science.abd9909
Chmielewska, Czarnota, Bienkowska-Szewczyk, Grzyb, None
Christensen, Mikael, Leung, Levesque, Deng et al., High folic acid consumption leads to pseudo-MTHFR deficiency, altered lipid metabolism, and liver injury in mice, Am. J. Clin. Nutr, doi:10.3945/ajcn.114.086603
Chung, Thone, Kwon, COVID-19 vaccines: The status and perspectives in delivery points of view, Adv. Drug Deliv. Rev, doi:10.1016/j.addr.2020.12.011
Covid, Team, Delorme-Axford, Klionsky, Highlights in the fight against COVID-19: does autophagy play a role in SARS-CoV-2 infection, doi:10.1080/15548627.2020.1844940
Evans, Rainger, Mason, Guzik, Osto et al., Endothelial dysfunction in COVID-19: a position paper of the ESC working Group for Atherosclerosis and Vascular Biology, and the ESC Council of basic cardiovascular science, Ann. N. Y. Acad. Sci, doi:10.1111/nyas.13499
Forni, Mantovani, COVID-19 vaccines: where we stand and challenges ahead, Cell Death Differ, doi:10.1038/s41418-020-00720-9
Fousse, Schub, Merzou, Fassbender, Sester et al., Case report: cerebral sinus vein thrombosis in two patients with AstraZeneca SARS-CoV-2 vaccination, J. Neurol, doi:10.1007/s00415-021-10731-2
Gao, Bao, Mao, Wang, Xu et al., Development of an inactivated vaccine candidate for SARS-CoV-2, Science, doi:10.1126/science.abc1932
Gheblawi, Wang, Viveiros, Nguyen, Zhong et al., Angiotensin-converting enzyme 2: SARS-CoV-2 receptor and regulator of the renin-angiotensin system: celebrating the 20th anniversary of the discovery of ACE2, Circ. Res, doi:10.1161/CIRCRESAHA.120.317015
Gintoni, Adamopoulou, Yapijakis, The Impact ofACEandACE2Gene Polymorphisms in Pulmonary Diseases Including COVID-19
Grint, Wing, Houlihan, Gibbs, Evans et al., Comprehensive structural and molecular comparison of spike proteins of SARS-CoV-2, SARS-CoV and MERS-CoV, and their interactions with ACE2, Clin. Infect. Dis, doi:10.3390/cells9122638
Huang, Lin, Kuo, Chen, Lin et al., Humanized COVID-19 decoy antibody effectively blocks viral entry and prevents SARS-CoV-2 infection, EMBO Mol. Med, doi:10.1038/s41467-020-18880-0
Kadam, Sukhramani, Bishnoi, Pable, Barvkar, SARS-CoV-2, the pandemic coronavirus: molecular and structural insights, J. Basic Microbiol, doi:10.1002/jobm.202000537
Kim, Cho, Kim, Kim, Yang et al., None
Levine-Tiefenbrun, Yelin, Alapi, Katz, Herzel et al., Engineered small extracellular vesicles displaying ACE2 variants on the surface protect against SARS-CoV-2 infection
Moll, Varga, Homocysteine and MTHFR mutations, Circulation, doi:10.1161/CIRCULATIONAHA.114.013311
Narula, Yusuf, Chong, Ramasundarahettige, Rangarajan et al., Plasma ACE2 and risk of death or cardiometabolic diseases: a case-cohort analysis, Lancet, doi:10.1016/S0140-6736(20)31964-4
Nie, Pouyan, Lauster, Trimpert, Kerkhoff et al., Polysulfates Block SARS-CoV-2 uptake through electrostatic interactions*, Angew. Chem. Int. Ed. Engl, doi:10.1002/anie.202102717
Oz, Lorke, Kabbani, A comprehensive guide to the pharmacologic regulation of angiotensin converting enzyme 2 (ACE2), the SARS-CoV-2 entry receptor, Pharmacol. Ther, doi:10.1016/j.pharmthera.2020.107750
Raghubeer, Matsha, Methylenetetrahydrofolate (MTHFR), the one-carbon cycle, and cardiovascular risks, Nutrients, doi:10.3390/nu13124562
Roche, Samson, Green, Karakochuk, Martinez, Perspective: weekly iron and folic acid supplementation (WIFAS): A critical review and rationale for inclusion in the essential medicines list to accelerate anemia and neural tube defects reduction, Adv. Nutr, doi:10.1093/advances/nmaa169
Roman, Mancera-Paez, Bernal, Epigenetic factors in late-onset Alzheimer's disease: MTHFR and CTH gene polymorphisms, metabolic Transsulfuration and methylation pathways, and B vitamins, Int. J. Mol. Sci, doi:10.3390/ijms20020319
Rubin, Baden, Karim, Morrissey, Audio interview: The omicron variant of SARS-CoV-2, N. Engl. J. Med, doi:10.1056/NEJMe2118839
Santos, Sampaio, Alzamora, Motta-Santos, Alenina et al., The ACE2/angiotensin-(1-7)/MAS Axis of the reninangiotensin system: focus on angiotensin-(1-7), Physiol. Rev, doi:10.1152/physrev.00023.2016
Shulpekova, Nechaev, Kardasheva, Sedova, Kurbatova, None
Soiza, Scicluna, Thomson, Efficacy and safety of COVID-19 vaccines in older people, Age Ageing, doi:10.1093/ageing/afaa274
South, Brady, Flynn, ACE2 (angiotensin-converting enzyme 2), COVID-19, and ACE inhibitor and Ang II (angiotensin II) receptor blocker use During the pandemic: The pediatric perspective, Hypertension, doi:10.1161/HYPERTENSIONAHA.120.15291
South, Tomlinson, Edmonston, Hiremath, Sparks, Controversies of renin-angiotensin system inhibition during the COVID-19 pandemic, Nat. Rev. Nephrol, doi:10.1038/s41581-020-0279-4
Sun, Liu, Amanat, Gonzalez-Dominguez, Mccroskery et al., A Newcastle disease virus expressing a stabilized spike protein of SARS-CoV-2 induces protective immune responses, J. Am. Chem. Soc, doi:10.1021/jacs.1c08226
Tada, Fan, Chen, Kaur, Stapleford et al., None
Vaduganathan, Vardeny, Michel, Mcmurray, Pfeffer et al., Structural analysis of SARS-CoV-2 genome and predictions of the human interactome, Nucleic Acids Res, doi:10.1093/nar/gkaa864
Wang, Nair, Liu, Iketani, Luo et al., Antibody resistance of SARS-CoV-2 variants B.1.351 and, Nature, doi:10.1038/s41586-021-03398-2
Wang, Wang, Chen, Zhao, Han et al., Membrane nanoparticles Derived from ACE2-rich cells Block SARS-CoV-2 infection, ACS Nano, doi:10.1021/acsnano.0c06836
Weile, Kishore, Sun, Maaieh, Verby et al., Shifting landscapes of human MTHFR missense-variant effects, Am. J. Hum. Genet, doi:10.1016/j.ajhg.2021.05.009
Weisblum, Schmidt, Zhang, Dasilva, Poston et al., Escape from neutralizing antibodies by SARS-CoV-2 spike protein variants, elife, doi:10.7554/eLife.61312
Xiong, Redwood, Prendergast, Chen, Coronaviruses and the cardiovascular system: acute and long-term implications, Eur. Heart J, doi:10.1093/eurheartj/ehaa231
Zhang, Xiang, Huo, Zhou, Jiang et al., Molecular mechanism of interaction between SARS-CoV-2 and host cells and interventional therapy, Signal Transduct. Target. Ther, doi:10.1038/s41569-020-0360-5
Zhou, Wang, Fast-spreading SARS-CoV-2 variants: challenges to and new design strategies of COVID-19 vaccines, Signal Transduct. Target. Ther, doi:10.1038/s41392-021-00644-x
DOI record:
{
"DOI": "10.3389/fmicb.2022.980903",
"ISSN": [
"1664-302X"
],
"URL": "http://dx.doi.org/10.3389/fmicb.2022.980903",
"abstract": "<jats:p>The current COVID-19 pandemic is motivating us to elucidate the molecular mechanism of SARS-CoV-2 invasion and find methods for decreasing its transmissibility. We found that SARS-CoV-2 could increase the protein level of ACE2 in mice. Folic acid and 5-10-methylenetetrahydrofolate reductase (MTHFR) could promote the methylation of the ACE2 promoter and inhibit ACE2 expression. Folic acid treatment decreased the binding ability of Spike protein, pseudovirus and inactivated authentic SARS-CoV-2 to host cells. Thus, folic acid treatment could decrease SARS-CoV-2 invasion and SARS-CoV-2-neutralizing antibody production in mice. These data suggest that increased intake of folic acid may inhibit ACE2 expression and reduce the transmissibility of SARS-CoV-2. Folic acid could play an important role in SARS-CoV-2 infection prevention and control.</jats:p>",
"alternative-id": [
"10.3389/fmicb.2022.980903"
],
"author": [
{
"affiliation": [],
"family": "Zhang",
"given": "Yuanzhou",
"sequence": "first"
},
{
"affiliation": [],
"family": "Pang",
"given": "Yechun",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Xu",
"given": "Baiyin",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Chen",
"given": "Xingshi",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Liang",
"given": "Shunshun",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Hu",
"given": "Jingying",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Luo",
"given": "Xiaoying",
"sequence": "additional"
}
],
"container-title": "Frontiers in Microbiology",
"container-title-short": "Front. Microbiol.",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"frontiersin.org"
]
},
"created": {
"date-parts": [
[
2022,
8,
17
]
],
"date-time": "2022-08-17T07:19:35Z",
"timestamp": 1660720775000
},
"deposited": {
"date-parts": [
[
2022,
8,
17
]
],
"date-time": "2022-08-17T07:19:40Z",
"timestamp": 1660720780000
},
"funder": [
{
"DOI": "10.13039/501100012166",
"award": [
"SQ2021YFE011305"
],
"doi-asserted-by": "publisher",
"name": "National key research and development program"
},
{
"DOI": "10.13039/501100001809",
"award": [
"81572454"
],
"doi-asserted-by": "publisher",
"name": "Natural Science Foundation of China"
}
],
"indexed": {
"date-parts": [
[
2023,
3,
1
]
],
"date-time": "2023-03-01T06:27:24Z",
"timestamp": 1677652044111
},
"is-referenced-by-count": 3,
"issued": {
"date-parts": [
[
2022,
8,
17
]
]
},
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
8,
17
]
],
"date-time": "2022-08-17T00:00:00Z",
"timestamp": 1660694400000
}
}
],
"link": [
{
"URL": "https://www.frontiersin.org/articles/10.3389/fmicb.2022.980903/full",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1965",
"original-title": [],
"prefix": "10.3389",
"published": {
"date-parts": [
[
2022,
8,
17
]
]
},
"published-online": {
"date-parts": [
[
2022,
8,
17
]
]
},
"publisher": "Frontiers Media SA",
"reference": [
{
"DOI": "10.1111/joim.13101",
"article-title": "COVID-19 and renin-angiotensin system inhibition: role of angiotensin converting enzyme 2 (ACE2) - is there any scientific evidence for controversy?",
"author": "Aleksova",
"doi-asserted-by": "publisher",
"first-page": "410",
"journal-title": "J. Intern. Med.",
"key": "ref1",
"volume": "288",
"year": "2020"
},
{
"DOI": "10.1126/science.abg7404",
"article-title": "Immunity to SARS-CoV-2 variants of concern",
"author": "Altmann",
"doi-asserted-by": "publisher",
"first-page": "1103",
"journal-title": "Science",
"key": "ref2",
"volume": "371",
"year": "2021"
},
{
"DOI": "10.1016/j.drup.2020.100721",
"article-title": "Current status of antivirals and druggable targets of SARS CoV-2 and other human pathogenic coronaviruses",
"author": "Artese",
"doi-asserted-by": "publisher",
"first-page": "100721",
"journal-title": "Drug Resist. Updat.",
"key": "ref3",
"volume": "53",
"year": "2020"
},
{
"DOI": "10.1002/14651858.CD012649",
"article-title": "Provision of folic acid for reducing arsenic toxicity in arsenic-exposed children and adults",
"author": "Bae",
"doi-asserted-by": "publisher",
"first-page": "CD012649",
"journal-title": "Cochrane Database Syst. Rev.",
"key": "ref4",
"volume": "10",
"year": "2021"
},
{
"DOI": "10.1001/jamacardio.2020.1282",
"article-title": "Coronavirus disease 2019 (COVID-19) infection and renin angiotensin system blockers",
"author": "Bavishi",
"doi-asserted-by": "publisher",
"first-page": "745",
"journal-title": "JAMA Cardiol.",
"key": "ref5",
"volume": "5",
"year": "2020"
},
{
"DOI": "10.1016/j.cell.2021.11.026",
"article-title": "Population impact of SARS-CoV-2 variants with enhanced transmissibility and/or partial immune escape",
"author": "Bushman",
"doi-asserted-by": "publisher",
"first-page": "6229.e18",
"journal-title": "Cell",
"key": "ref6",
"volume": "184",
"year": "2021"
},
{
"DOI": "10.1038/d41586-021-00031-0",
"article-title": "Could new COVID variants undermine vaccines? Labs scramble to find out",
"author": "Callaway",
"doi-asserted-by": "publisher",
"first-page": "177",
"journal-title": "Nature",
"key": "ref7",
"volume": "589",
"year": ""
},
{
"DOI": "10.1038/d41586-021-03672-3",
"article-title": "Omicron likely to weaken COVID vaccine protection",
"author": "Callaway",
"doi-asserted-by": "publisher",
"first-page": "367",
"journal-title": "Nature",
"key": "ref8",
"volume": "600",
"year": ""
},
{
"DOI": "10.1126/science.abd9909",
"article-title": "De novo design of picomolar SARS-CoV-2 miniprotein inhibitors",
"author": "Cao",
"doi-asserted-by": "publisher",
"first-page": "426",
"journal-title": "Science",
"key": "ref9",
"volume": "370",
"year": "2020"
},
{
"DOI": "10.1016/j.addr.2021.01.014",
"article-title": "SARS-CoV-2 vaccines in advanced clinical trials: where do we stand?",
"author": "Chakraborty",
"doi-asserted-by": "publisher",
"first-page": "314",
"journal-title": "Adv. Drug Deliv. Rev.",
"key": "ref10",
"volume": "172",
"year": "2021"
},
{
"DOI": "10.1038/s41541-021-00404-6",
"article-title": "Immune response against SARS-CoV-2 variants: the role of neutralization assays",
"author": "Chmielewska",
"doi-asserted-by": "publisher",
"first-page": "142",
"journal-title": "NPJ Vaccines",
"key": "ref11",
"volume": "6",
"year": "2021"
},
{
"DOI": "10.3945/ajcn.114.086603",
"article-title": "High folic acid consumption leads to pseudo-MTHFR deficiency, altered lipid metabolism, and liver injury in mice",
"author": "Christensen",
"doi-asserted-by": "publisher",
"first-page": "646",
"journal-title": "Am. J. Clin. Nutr.",
"key": "ref12",
"volume": "101",
"year": "2015"
},
{
"DOI": "10.1016/j.addr.2020.12.011",
"article-title": "COVID-19 vaccines: The status and perspectives in delivery points of view",
"author": "Chung",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "Adv. Drug Deliv. Rev.",
"key": "ref13",
"volume": "170",
"year": "2021"
},
{
"DOI": "10.15585/mmwr.mm7050e1",
"article-title": "SARS-CoV-2 B.1.1.529 (omicron) variant - United States, December 1-8, 2021",
"doi-asserted-by": "crossref",
"first-page": "1731",
"journal-title": "MMWR Morb. Mortal. Wkly Rep.",
"key": "ref14",
"volume": "70",
"year": "2021"
},
{
"DOI": "10.1080/15548627.2020.1844940",
"article-title": "Highlights in the fight against COVID-19: does autophagy play a role in SARS-CoV-2 infection?",
"author": "Delorme-Axford",
"doi-asserted-by": "publisher",
"first-page": "2123",
"journal-title": "Autophagy",
"key": "ref15",
"volume": "16",
"year": "2020"
},
{
"DOI": "10.1093/cvr/cvaa230",
"article-title": "Endothelial dysfunction in COVID-19: a position paper of the ESC working Group for Atherosclerosis and Vascular Biology, and the ESC Council of basic cardiovascular science",
"author": "Evans",
"doi-asserted-by": "publisher",
"first-page": "2177",
"journal-title": "Cardiovasc. Res.",
"key": "ref16",
"volume": "116",
"year": "2020"
},
{
"DOI": "10.1111/nyas.13499",
"article-title": "Safety of folic acid",
"author": "Field",
"doi-asserted-by": "publisher",
"first-page": "59",
"journal-title": "Ann. N. Y. Acad. Sci.",
"key": "ref17",
"volume": "1414",
"year": "2018"
},
{
"DOI": "10.1038/s41418-020-00720-9",
"article-title": "COVID-19 vaccines: where we stand and challenges ahead",
"author": "Forni",
"doi-asserted-by": "publisher",
"first-page": "626",
"journal-title": "Cell Death Differ.",
"key": "ref18",
"volume": "28",
"year": "2021"
},
{
"DOI": "10.1007/s00415-021-10731-2",
"article-title": "Case report: cerebral sinus vein thrombosis in two patients with AstraZeneca SARS-CoV-2 vaccination",
"author": "Fousse",
"doi-asserted-by": "publisher",
"first-page": "583",
"journal-title": "J. Neurol.",
"key": "ref19",
"volume": "269",
"year": "2022"
},
{
"DOI": "10.1126/science.abc1932",
"article-title": "Development of an inactivated vaccine candidate for SARS-CoV-2",
"author": "Gao",
"doi-asserted-by": "publisher",
"first-page": "77",
"journal-title": "Science",
"key": "ref20",
"volume": "369",
"year": "2020"
},
{
"DOI": "10.1161/CIRCRESAHA.120.317015",
"article-title": "Angiotensin-converting enzyme 2: SARS-CoV-2 receptor and regulator of the renin-angiotensin system: celebrating the 20th anniversary of the discovery of ACE2",
"author": "Gheblawi",
"doi-asserted-by": "publisher",
"first-page": "1456",
"journal-title": "Circ. Res.",
"key": "ref21",
"volume": "126",
"year": "2020"
},
{
"DOI": "10.21873/invivo.12672",
"article-title": "The Impact ofACEandACE2Gene Polymorphisms in Pulmonary Diseases Including COVID-19",
"author": "Gintoni",
"doi-asserted-by": "publisher",
"first-page": "13",
"journal-title": "In Vivo",
"key": "ref22",
"volume": "36",
"year": "2022"
},
{
"DOI": "10.1093/cid/ciab754",
"article-title": "Severity of SARS-CoV-2 alpha variant (B.1.1.7) in England",
"author": "Grint",
"doi-asserted-by": "publisher",
"first-page": "ciab754",
"journal-title": "Clin. Infect. Dis.",
"key": "ref23",
"year": "2021"
},
{
"DOI": "10.3390/cells9122638",
"article-title": "Comprehensive structural and molecular comparison of spike proteins of SARS-CoV-2, SARS-CoV and MERS-CoV, and their interactions with ACE2",
"author": "Hatmal",
"doi-asserted-by": "publisher",
"first-page": "638",
"journal-title": "Cell",
"key": "ref24",
"volume": "9",
"year": "2020"
},
{
"DOI": "10.15252/emmm.202012828",
"article-title": "Humanized COVID-19 decoy antibody effectively blocks viral entry and prevents SARS-CoV-2 infection",
"author": "Huang",
"doi-asserted-by": "crossref",
"first-page": "e12828",
"journal-title": "EMBO Mol. Med.",
"key": "ref25",
"volume": "13",
"year": "2021"
},
{
"DOI": "10.1038/s41467-020-18880-0",
"article-title": "ACE2 mouse models: a toolbox for cardiovascular and pulmonary research",
"author": "Jia",
"doi-asserted-by": "publisher",
"first-page": "5165",
"journal-title": "Nat. Commun.",
"key": "ref26",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.1002/jobm.202000537",
"article-title": "SARS-CoV-2, the pandemic coronavirus: molecular and structural insights",
"author": "Kadam",
"doi-asserted-by": "publisher",
"first-page": "180",
"journal-title": "J. Basic Microbiol.",
"key": "ref27",
"volume": "61",
"year": "2021"
},
{
"DOI": "10.1002/jev2.12179",
"article-title": "Engineered small extracellular vesicles displaying ACE2 variants on the surface protect against SARS-CoV-2 infection",
"author": "Kim",
"doi-asserted-by": "crossref",
"first-page": "e12179",
"journal-title": "J Extracell Vesicles",
"key": "ref28",
"volume": "11",
"year": "2022"
},
{
"DOI": "10.1038/s41591-021-01575-4",
"article-title": "Viral loads of Delta-variant SARS-CoV-2 breakthrough infections after vaccination and booster with BNT162b2",
"author": "Levine-Tiefenbrun",
"doi-asserted-by": "publisher",
"first-page": "2108",
"journal-title": "Nat. Med.",
"key": "ref29",
"volume": "27",
"year": "2021"
},
{
"DOI": "10.1161/CIRCULATIONAHA.114.013311",
"article-title": "Homocysteine and MTHFR mutations",
"author": "Moll",
"doi-asserted-by": "publisher",
"first-page": "e6",
"journal-title": "Circulation",
"key": "ref30",
"volume": "132",
"year": "2015"
},
{
"DOI": "10.1016/S0140-6736(20)31964-4",
"article-title": "Plasma ACE2 and risk of death or cardiometabolic diseases: a case-cohort analysis",
"author": "Narula",
"doi-asserted-by": "publisher",
"first-page": "968",
"journal-title": "Lancet",
"key": "ref31",
"volume": "396",
"year": "2020"
},
{
"DOI": "10.1002/anie.202102717",
"article-title": "Polysulfates Block SARS-CoV-2 uptake through electrostatic interactions*",
"author": "Nie",
"doi-asserted-by": "publisher",
"first-page": "15870",
"journal-title": "Angew. Chem. Int. Ed. Engl.",
"key": "ref32",
"volume": "60",
"year": "2021"
},
{
"DOI": "10.1016/j.pharmthera.2020.107750",
"article-title": "A comprehensive guide to the pharmacologic regulation of angiotensin converting enzyme 2 (ACE2), the SARS-CoV-2 entry receptor",
"author": "Oz",
"doi-asserted-by": "publisher",
"first-page": "107750",
"journal-title": "Pharmacol. Ther.",
"key": "ref33",
"volume": "221",
"year": "2021"
},
{
"DOI": "10.3390/nu13124562",
"article-title": "Methylenetetrahydrofolate (MTHFR), the one-carbon cycle, and cardiovascular risks",
"author": "Raghubeer",
"doi-asserted-by": "publisher",
"first-page": "4562",
"journal-title": "Nutrients",
"key": "ref34",
"volume": "13",
"year": "2021"
},
{
"DOI": "10.1093/advances/nmaa169",
"article-title": "Perspective: weekly iron and folic acid supplementation (WIFAS): A critical review and rationale for inclusion in the essential medicines list to accelerate anemia and neural tube defects reduction",
"author": "Roche",
"doi-asserted-by": "publisher",
"first-page": "334",
"journal-title": "Adv. Nutr.",
"key": "ref35",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.3390/ijms20020319",
"article-title": "Epigenetic factors in late-onset Alzheimer's disease: MTHFR and CTH gene polymorphisms, metabolic Transsulfuration and methylation pathways, and B vitamins",
"author": "Roman",
"doi-asserted-by": "publisher",
"first-page": "319",
"journal-title": "Int. J. Mol. Sci.",
"key": "ref36",
"volume": "20",
"year": "2019"
},
{
"DOI": "10.1056/NEJMe2118839",
"article-title": "Audio interview: The omicron variant of SARS-CoV-2",
"author": "Rubin",
"doi-asserted-by": "publisher",
"first-page": "e96",
"journal-title": "N. Engl. J. Med.",
"key": "ref37",
"volume": "385",
"year": "2021"
},
{
"DOI": "10.1152/physrev.00023.2016",
"article-title": "The ACE2/angiotensin-(1-7)/MAS Axis of the renin-angiotensin system: focus on angiotensin-(1-7)",
"author": "Santos",
"doi-asserted-by": "publisher",
"first-page": "505",
"journal-title": "Physiol. Rev.",
"key": "ref38",
"volume": "98",
"year": "2018"
},
{
"DOI": "10.3390/molecules26123731",
"article-title": "The concept of folic acid in health and disease",
"author": "Shulpekova",
"doi-asserted-by": "publisher",
"first-page": "731",
"journal-title": "Molecules",
"key": "ref39",
"volume": "26",
"year": "2021"
},
{
"DOI": "10.1093/ageing/afaa274",
"article-title": "Efficacy and safety of COVID-19 vaccines in older people",
"author": "Soiza",
"doi-asserted-by": "publisher",
"first-page": "279",
"journal-title": "Age Ageing",
"key": "ref40",
"volume": "50",
"year": "2021"
},
{
"DOI": "10.1161/HYPERTENSIONAHA.120.15291",
"article-title": "ACE2 (angiotensin-converting enzyme 2), COVID-19, and ACE inhibitor and Ang II (angiotensin II) receptor blocker use During the pandemic: The pediatric perspective",
"author": "South",
"doi-asserted-by": "publisher",
"first-page": "16",
"journal-title": "Hypertension",
"key": "ref41",
"volume": "76",
"year": ""
},
{
"DOI": "10.1038/s41581-020-0279-4",
"article-title": "Controversies of renin-angiotensin system inhibition during the COVID-19 pandemic",
"author": "South",
"doi-asserted-by": "publisher",
"first-page": "305",
"journal-title": "Nat. Rev. Nephrol.",
"key": "ref42",
"volume": "16",
"year": ""
},
{
"DOI": "10.1038/s41467-021-26499-y",
"article-title": "A Newcastle disease virus expressing a stabilized spike protein of SARS-CoV-2 induces protective immune responses",
"author": "Sun",
"doi-asserted-by": "publisher",
"first-page": "6197",
"journal-title": "Nat. Commun.",
"key": "ref43",
"volume": "12",
"year": ""
},
{
"DOI": "10.1021/jacs.1c08226",
"article-title": "Spherical neutralizing Aptamer inhibits SARS-CoV-2 infection and suppresses mutational escape",
"author": "Sun",
"doi-asserted-by": "publisher",
"first-page": "21541",
"journal-title": "J. Am. Chem. Soc.",
"key": "ref44",
"volume": "143",
"year": ""
},
{
"DOI": "10.1016/j.celrep.2020.108528",
"article-title": "An ACE2 microbody containing a single immunoglobulin fc domain is a potent inhibitor of SARS-CoV-2",
"author": "Tada",
"doi-asserted-by": "publisher",
"first-page": "108528",
"journal-title": "Cell Rep.",
"key": "ref45",
"volume": "33",
"year": "2020"
},
{
"DOI": "10.1016/S1473-3099(21)00770-2",
"article-title": "Emerging SARS-CoV-2 variants: shooting the messenger",
"doi-asserted-by": "crossref",
"first-page": "1",
"journal-title": "Lancet Infect. Dis.",
"key": "ref46",
"volume": "22",
"year": "2022"
},
{
"DOI": "10.1056/NEJMsr2005760",
"article-title": "Renin-angiotensin-aldosterone system inhibitors in patients with Covid-19",
"author": "Vaduganathan",
"doi-asserted-by": "publisher",
"first-page": "1653",
"journal-title": "N. Engl. J. Med.",
"key": "ref47",
"volume": "382",
"year": "2020"
},
{
"DOI": "10.1093/nar/gkaa864",
"article-title": "Structural analysis of SARS-CoV-2 genome and predictions of the human interactome",
"author": "Vandelli",
"doi-asserted-by": "publisher",
"first-page": "11270",
"journal-title": "Nucleic Acids Res.",
"key": "ref48",
"volume": "48",
"year": "2020"
},
{
"DOI": "10.1038/s41586-021-03398-2",
"article-title": "Antibody resistance of SARS-CoV-2 variants B.1.351 and B.1.1.7",
"author": "Wang",
"doi-asserted-by": "publisher",
"first-page": "130",
"journal-title": "Nature",
"key": "ref49",
"volume": "593",
"year": ""
},
{
"DOI": "10.1021/acsnano.0c06836",
"article-title": "Membrane nanoparticles Derived from ACE2-rich cells Block SARS-CoV-2 infection",
"author": "Wang",
"doi-asserted-by": "publisher",
"first-page": "6340",
"journal-title": "ACS Nano",
"key": "ref50",
"volume": "15",
"year": ""
},
{
"DOI": "10.1016/j.ajhg.2021.05.009",
"article-title": "Shifting landscapes of human MTHFR missense-variant effects",
"author": "Weile",
"doi-asserted-by": "publisher",
"first-page": "1283",
"journal-title": "Am. J. Hum. Genet.",
"key": "ref51",
"volume": "108",
"year": "2021"
},
{
"DOI": "10.7554/eLife.61312",
"article-title": "Escape from neutralizing antibodies by SARS-CoV-2 spike protein variants",
"author": "Weisblum",
"doi-asserted-by": "publisher",
"first-page": "312",
"journal-title": "elife",
"key": "ref52",
"volume": "9",
"year": "2020"
},
{
"DOI": "10.1093/eurheartj/ehaa231",
"article-title": "Coronaviruses and the cardiovascular system: acute and long-term implications",
"author": "Xiong",
"doi-asserted-by": "publisher",
"first-page": "1798",
"journal-title": "Eur. Heart J.",
"key": "ref53",
"volume": "41",
"year": "2020"
},
{
"DOI": "10.1038/s41392-021-00653-w",
"article-title": "Molecular mechanism of interaction between SARS-CoV-2 and host cells and interventional therapy",
"author": "Zhang",
"doi-asserted-by": "publisher",
"first-page": "233",
"journal-title": "Signal Transduct. Target. Ther.",
"key": "ref54",
"volume": "6",
"year": "2021"
},
{
"DOI": "10.1038/s41569-020-0360-5",
"article-title": "COVID-19 and the cardiovascular system",
"author": "Zheng",
"doi-asserted-by": "publisher",
"first-page": "259",
"journal-title": "Nat. Rev. Cardiol.",
"key": "ref55",
"volume": "17",
"year": "2020"
},
{
"DOI": "10.1038/s41392-021-00644-x",
"article-title": "Fast-spreading SARS-CoV-2 variants: challenges to and new design strategies of COVID-19 vaccines",
"author": "Zhou",
"doi-asserted-by": "publisher",
"first-page": "226",
"journal-title": "Signal Transduct. Target. Ther.",
"key": "ref56",
"volume": "6",
"year": "2021"
}
],
"reference-count": 56,
"references-count": 56,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.frontiersin.org/articles/10.3389/fmicb.2022.980903/full"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Microbiology (medical)",
"Microbiology"
],
"subtitle": [],
"title": "Folic acid restricts SARS-CoV-2 invasion by methylating ACE2",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.3389/crossmark-policy",
"volume": "13"
}