Effectiveness of Curcumin on Outcomes of Hospitalized COVID-19 Patients: A Systematic Review of Clinical Trials
et al., Nutrients, doi:10.3390/nu14020256, Jan 2022
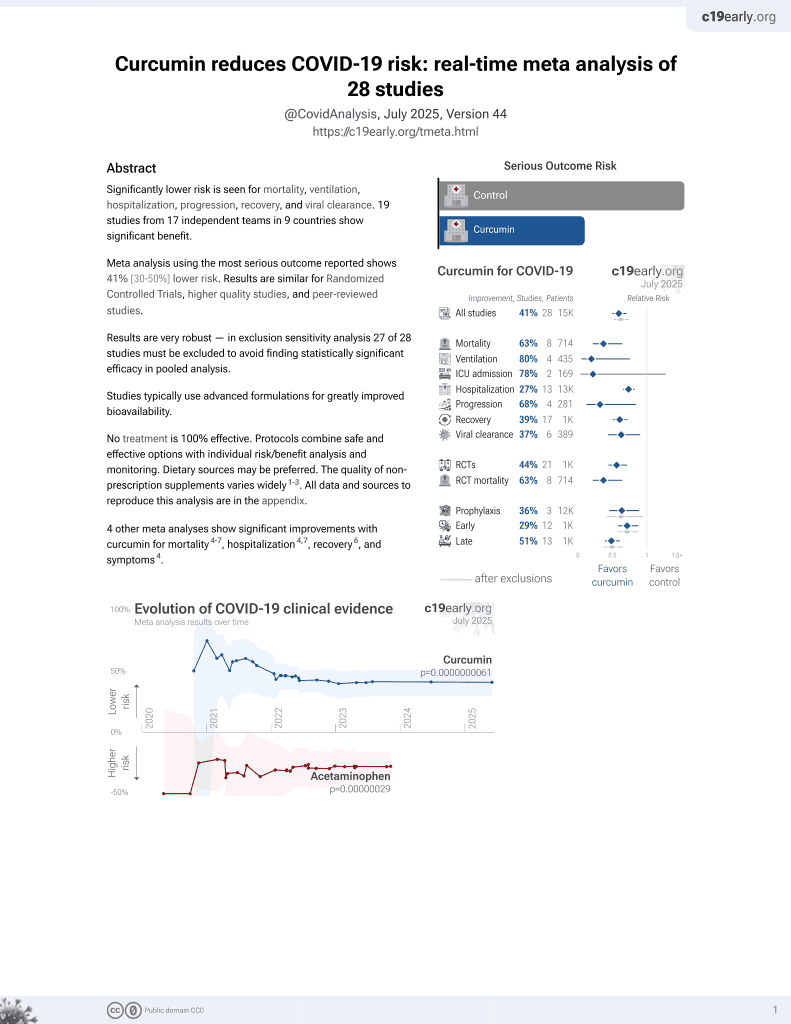
Curcumin for COVID-19
17th treatment shown to reduce risk in
February 2021, now with p = 0.0000000061 from 28 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Review of 6 COVID-19 curcumin studies showing that treatment resulted in significant improvement in symptoms, duration of hospitalization, and mortality, and a significant decrease in proinflammatory cytokines and increase in anti-inflammatory cytokines.
6 meta-analyses show significant improvements with curcumin for mortality1-6,
mechanical ventilation6,
hospitalization1,4,
recovery3,6,
progression6, and
symptoms1.
1.
Vahedian-Azimi et al., Effectiveness of Curcumin on Outcomes of Hospitalized COVID-19 Patients: A Systematic Review of Clinical Trials, Nutrients, doi:10.3390/nu14020256.
2.
Kow et al., The effect of curcumin on the risk of mortality in patients with COVID-19: A systematic review and meta-analysis of randomized trials, Phytotherapy Research, doi:10.1002/ptr.7468.
3.
Shafiee et al., Curcumin for the treatment of COVID-19 patients: A meta-analysis of randomized controlled trials, Phytotherapy Research, doi:10.1002/ptr.7724.
4.
Shojaei et al., The effectiveness of nano‐curcumin on patients with COVID‐19: A systematic review of clinical trials, Phytotherapy Research, doi:10.1002/ptr.7778.
Vahedian-Azimi et al., 7 Jan 2022, peer-reviewed, 9 authors.
Effectiveness of Curcumin on Outcomes of Hospitalized COVID-19 Patients: A Systematic Review of Clinical Trials
Nutrients, doi:10.3390/nu14020256
Despite the ongoing vaccination efforts, there is still an urgent need for safe and effective treatments to help curb the debilitating effects of COVID-19 disease. This systematic review aimed to investigate the efficacy of supplemental curcumin treatment on clinical outcomes and inflammationrelated biomarker profiles in COVID-19 patients. We searched PubMed, Scopus, Web of Science, EMBASE, ProQuest, and Ovid databases up to 30 June 2021 to find studies that assessed the effects of curcumin-related compounds in mild to severe COVID-19 patients. Six studies were identified which showed that curcumin supplementation led to a significant decrease in common symptoms, duration of hospitalization and deaths. In addition, all of these studies showed that the intervention led to amelioration of cytokine storm effects thought to be a driving force in severe COVID-19 cases. This was seen as a significant (p < 0.05) decrease in proinflammatory cytokines such as IL1β and IL6, with a concomitant significant (p < 0.05) increase in anti-inflammatory cytokines, including IL-10, IL-35 and TGF-α. Taken together, these findings suggested that curcumin exerts its beneficial effects through at least partial restoration of pro-inflammatory/anti-inflammatory balance. In conclusion, curcumin supplementation may offer an efficacious and safe option for improving COVID-19 disease outcomes. We highlight the point that future clinical studies of COVID-19 disease should employ larger cohorts of patients in different clinical settings with standardized preparations of curcuminrelated compounds.
Supplementary Materials: The following supporting information can be downloaded at: https: //www.mdpi.com/article/10.3390/nu14020256/s1, Supplementary File S1. Details of search strategy; Supplementary File S2. Methodological quality assessment for RCTs included studies using the Jadad rating scale.
References
Abd-Alkhalek, Omayma, Managements of COVID-19 by curcumin, Acta Sci. Pharm. Sci, doi:10.31080/ASPS.2020.05.0657
Aggarwal, Sundaram, Malani, Ichikawa, Curcumin: The Indian solid gold, Adv. Exp. Med. Biol
Ahmadi, Salari, Sharifi, Reihani, Rostamiani et al., Oral nano-curcumin formulation efficacy in the management of mild to moderate outpatient COVID-19: A randomized triple-blind placebo-controlled clinical trial, Food Sci. Nutr, doi:10.1002/fsn3.2226
Alidadi, Liberale, Montecucco, Majeed, Al-Rasadi et al., Protective effects of curcumin on endothelium: An updated review. Studies on Biomarkers and New Targets in Aging Research in Iran, Adv. Exp. Med. Biol
Alidadi, Sahebkar, Eslami, Vakilian, Jarahi et al., The effect of curcumin supplementation on pulse wave velocity in patients with metabolic syndrome: A randomized, double-blind, placebo-controlled trial, Adv. Exp. Med. Biol
Baeten, Van Zeebroeck, Kleinewietfeld, Hellings, Broux, Improving the efficacy of regulatory T cell therapy, Clin. Rev. Allergy Immunol, doi:10.1007/s12016-021-08866-1
Bagherniya, Darand, Askari, Guest, Sathyapalan et al., The clinical use of curcumin for the treatment of rheumatoid arthritis: A systematic review of clinical trials, Adv. Exp. Med. Biol
Bhaskar, Sinha, Banach, Mittoo, Weissert et al., Cytokine storm in COVID-19-immunopathological mechanisms, clinical considerations, and therapeutic approaches: The REPROGRAM consortium position paper, Front. Immunol, doi:10.3389/fimmu.2020.01648
Cano Glu, Şaylan, Çalışkan, COVID-19 and thrombosis: Prophylaxis and management, Tuberk. Toraks
Cicero, Sahebkar, Fogacci, Bove, Giovannini et al., Effects of phytosomal curcumin on anthropometric parameters, insulin resistance, cortisolemia and non-alcoholic fatty liver disease indices: A double-blind, placebo-controlled clinical trial, Eur. J. Nutr, doi:10.1007/s00394-019-01916-7
Cuomo, Appendino, Dern, Schneider, Mckinnon et al., Comparative absorption of a standardized curcuminoid mixture and its lecithin formulation, J. Nat. Prod, doi:10.1021/np1007262
Devreese, COVID-19-related laboratory coagulation findings, Int. J. Lab. Hematol, doi:10.1111/ijlh.13547
Dolati, Ahmadi, Rikhtegar, Babaloo, Ayromlou et al., Changes in Th17 cells function after nanocurcumin use to treat multiple sclerosis, Int. Immunopharmacol, doi:10.1016/j.intimp.2018.05.018
Dolati, Babaloo, Ayromlou, Ahmadi, Rikhtegar et al., Nanocurcumin improves regulatory T-cell frequency and function in patients with multiple sclerosis, J. Neuroimmunol, doi:10.1016/j.jneuroim.2019.01.007
Ege, Action mechanisms of curcumin in alzheimer's disease and its brain targeted delivery, Materials, doi:10.3390/ma14123332
Ferguson, Abbott, Garg, Anti-inflammatory effects of oral supplementation with curcumin: A systematic review and meta-analysis of randomized controlled trials, Nutr. Rev, doi:10.1093/nutrit/nuaa114
Gasmi, Chirumbolo, Peana, Noor, Menzel et al., The role of diet and supplementation of natural products in COVID-19 prevention, Biol. Trace Elem. Res, doi:10.1007/s12011-021-02623-3
George, Mayne, The Novel Coronavirus and Inflammation, Adv. Exp. Med. Biol
Ghandadi, Sahebkar, Curcumin: An effective inhibitor of interleukin-6, Curr. Pharm. Des, doi:10.2174/1381612822666161006151605
Ghasemi, Shafiee, Banikazemi, Pourhanifeh, Khanbabaei et al., Curcumin inhibits NF-kB and Wnt/β-catenin pathways in cervical cancer cells, Pathol.-Res. Pract, doi:10.1016/j.prp.2019.152556
Gorabi, Razi, Aslani, Abbasifard, Imani et al., Effect of curcumin on pro-inflammatory cytokines: A meta-analysis of randomized controlled trials, Cytokine, doi:10.1016/j.cyto.2021.155541
Guest, Sahebkar, Research in the middle east into the health benefits of curcumin, Adv. Exp. Med. Biol
Gupta, Patchva, Aggarwal, Therapeutic roles of curcumin: Lessons learned from clinical trials, AAPS J, doi:10.1208/s12248-012-9432-8
Haftcheshmeh, Khosrojerdi, Aliabadi, Lotfi, Mohammadi et al., Immunomodulatory effects of curcumin in rheumatoid arthritis: Evidence from molecular mechanisms to clinical outcomes, Rev. Physiol. Biochem. Pharmacol
Hatcher, Planalp, Cho, Torti, Torti, Curcumin: From ancient medicine to current clinical trials, Cell. Mol. Life Sci, doi:10.1007/s00018-008-7452-4
Hewlings, Kalman, Curcumin: A review of its effects on human health, Foods, doi:10.3390/foods6100092
Jadad, Moore, Carroll, Jenkinson, Reynolds et al., Assessing the quality of reports of randomized clinical trials: Is blinding necessary? Control, Clin. Trials, doi:10.1016/0197-2456(95)00134-4
Jantan, Rohani, Sumantri, Immunomodulatory effects and mechanisms of curcuma species and their bioactive compounds: A review, Front. Pharmacol, doi:10.3389/fphar.2021.643119
Jin, Cai, Cheng, Cheng, Deng et al., A rapid advice guideline for the diagnosis and treatment of 2019 novel coronavirus (2019-nCoV) infected pneumonia (standard version), Mil. Med. Res, doi:10.1186/s40779-020-0233-6
Kubo, Motomura, Transcriptional regulation of the anti-inflammatory cytokine IL-10 in acquired immune cells, Front. Immunol, doi:10.3389/fimmu.2012.00275
Kunnumakkara, Bordoloi, Padmavathi, Monisha, Roy et al., Curcumin, the golden nutraceutical: Multitargeting for multiple chronic diseases, Br. J. Pharmacol, doi:10.1111/bph.13621
Li, Zhang, Pei, Liu, Dai et al., Molecular mechanism of olaquindox-induced hepatotoxicity and the hepatic protective role of curcumin, Food Chem. Toxicol, doi:10.1016/j.fct.2020.111727
Melo, Milby, Caparroz, Pinto, Santos et al., Biomarkers of cytokine storm as red flags for severe and fatal COVID-19 cases: A living systematic review and meta-analysis, PLoS ONE, doi:10.1371/journal.pone.0253894
Moher, Liberati, Tetzlaff, Altman, Prisma Group, Reprint-preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement, Phys. Ther, doi:10.1093/ptj/89.9.873
Mollazadeh, Cicero, Blesso, Pirro, Majeed et al., Immune modulation by curcumin: The role of interleukin-10, Crit. Rev. Food Sci. Nutr, doi:10.1080/10408398.2017.1358139
Momtazi, Shahabipour, Khatibi, Johnston, Pirro et al., Curcumin as a MicroRNA regulator in cancer: A review, Rev. Physiol. Biochem. Pharmacol
Mortezaee, Salehi, Mirtavoos-Mahyari, Motevaseli, Najafi et al., Mechanisms of apoptosis modulation by curcumin: Implications for cancer therapy, J. Cell. Physiol, doi:10.1002/jcp.28122
Noori, Nejadghaderi, Arshi, Carson-Chahhoud, Ansarin et al., Potency of BNT162b2 and mRNA-1273 vaccine-induced neutralizing antibodies against severe acute respiratory syndrome-CoV-2 variants of concern: A systematic review of in vitro studies, Rev. Med. Virol, doi:10.1002/rmv.2277
Panahi, Karbasi, Valizadegan, Ostadzadeh, Soflaei et al., Effect of curcumin on severity of functional dyspepsia: A triple blinded clinical trial, Adv. Exp. Med. Biol
Panahi, Khalili, Sahebi, Namazi, Majeed et al., Effects of curcuminoids plus piperine on glycemic, hepatic and inflammatory biomarkers in patients with type 2 diabetes mellitus: A randomized double-blind placebo-controlled trial, Drug Res, doi:10.1055/s-0044-101752
Pawar, Mastud, Pawar, Pawar, Bhoite et al., Oral curcumin with piperine as adjuvant therapy for the treatment of COVID-19: A randomized clinical trial, Front. Pharmacol, doi:10.3389/fphar.2021.669362
Plitas, Rudensky, Regulatory T cells: Differentiation and function, Cancer Immunol. Res, doi:10.1158/2326-6066.CIR-16-0193
Proal, Vanelzakker, Long COVID or post-acute sequelae of COVID-19 (PASC): An overview of biological factors that may contribute to persistent symptoms, Front. Microbiol, doi:10.3389/fmicb.2021.698169
Pt, None, doi:10.1016/j.intimp.2020.107088
Quek, Tahir, Kumar, Hastings, Jha, Treatment of COVID-19: A review of current and prospective pharmacotherapies, Br. J. Hosp. Med, doi:10.12968/hmed.2021.0112
Rahimi, Hassanzadeh, Khanbabaei, Haftcheshmeh, Ahmadi et al., Curcumin: A dietary phytochemical for targeting the phenotype and function of dendritic cells, Curr. Med. Chem, doi:10.2174/0929867327666200515101228
Ramasamy, Subbian, Critical determinants of cytokine storm and type I interferon response in COVID-19 pathogenesis, Clin. Microbiol. Rev, doi:10.1128/CMR.00299-20
Rezaei, Mahmoudi, Mortaz, Marjani, Immune cell profiling and antibody responses in patients with COVID-19, BMC Infect. Dis, doi:10.1186/s12879-021-06278-2
Ruscica, Penson, Ferri, Sirtori, Pirro et al., Impact of nutraceuticals on markers of systemic inflammation: Potential relevance to cardiovascular diseases-A position paper from the international lipid expert panel (ILEP), Prog. Cardiovasc. Dis, doi:10.1016/j.pcad.2021.06.010
Saber-Moghaddam, Salari, Hejazi, Amini, Taherzadeh et al., Oral nano-curcumin formulation efficacy in management of mild to moderate hospitalized coronavirus disease-19 patients: An open-label non-randomized clinical trial, Phytother. Res, doi:10.1002/ptr.7004
Sahebkar, Molecular mechanisms for curcumin benefits against ischemic injury, Fertil. Steril, doi:10.1016/j.fertnstert.2010.07.1071
Santoro, Carafoli, Remdesivir: From ebola to COVID-19, Biochem. Biophys. Res. Commun, doi:10.1016/j.bbrc.2020.11.043
Tahmasebi, El-Esawi, Mahmoud, Timoshin, Valizadeh et al., Immunomodulatory effects of nanocurcumin on Th17 cell responses in mild and severe COVID-19 patients, J. Cell. Physiol, doi:10.1002/jcp.30233
Tahmasebi, Saeed, Temirgalieva, Yumashev, El-Esawi et al., Nanocurcumin improves Treg cell responses in patients with mild and severe SARS-CoV2, Life Sci, doi:10.1016/j.lfs.2021.119437
Talebi, Safarian, Jaafari, Sayedi, Abbasi et al., The effects of nano-curcumin as a nutritional strategy on clinical and inflammatory factors in children with cystic fibrosis: The study protocol for a randomized controlled trial, Trials, doi:10.1186/s13063-021-05224-6
Tan, Liu, Zhou, Deng, Li et al., Immunopathological characteristics of coronavirus disease 2019 cases in Guangzhou, China, Immunology, doi:10.1111/imm.13223
Valizadeh, Abdolmohammadi-Vahid, Danshina, Gencer, Ammari et al., Nano-curcumin therapy, a promising method in modulating inflammatory cytokines in COVID-19 patients, Int. Immunopharmacol
Valle, Kim-Schulze, Huang, Beckmann, Nirenberg et al., An inflammatory cytokine signature predicts COVID-19 severity and survival, Nat. Med
Wang, Truong, COVID-19 infection on IL-23 inhibition, Dermatol. Ther, doi:10.1111/dth.13893
Wang, Zheng, Islam, Yang, Hu et al., The role of CD4 + FoxP3 + regulatory T cells in the immunopathogenesis of COVID-19: Implications for treatment, Int. J. Biol. Sci, doi:10.7150/ijbs.59534
Yavarpour-Bali, Ghasemi-Kasman, Pirzadeh, Curcumin-loaded nanoparticles: A novel therapeutic strategy in treatment of central nervous system disorders, Int. J. Nanomed, doi:10.2147/IJN.S208332
Yazdanpanah, Hamblin, Rezaei, The immune system and COVID-19: Friend or foe?, Life Sci, doi:10.1016/j.lfs.2020.117900
Yuandani, None
Zahedipour, Hosseini, Sathyapalan, Majeed, Jamialahmadi et al., Potential effects of curcumin in the treatment of COVID-19 infection, Phytother. Res, doi:10.1002/ptr.6738
Zhang, Ai, Chen, Liu, Gong et al., Associations of immunological features with COVID-19 severity: A systematic review and meta-analysis, BMC Infect. Dis, doi:10.1186/s12879-021-06457-1
DOI record:
{
"DOI": "10.3390/nu14020256",
"ISSN": [
"2072-6643"
],
"URL": "http://dx.doi.org/10.3390/nu14020256",
"abstract": "<jats:p>Despite the ongoing vaccination efforts, there is still an urgent need for safe and effective treatments to help curb the debilitating effects of COVID-19 disease. This systematic review aimed to investigate the efficacy of supplemental curcumin treatment on clinical outcomes and inflammation-related biomarker profiles in COVID-19 patients. We searched PubMed, Scopus, Web of Science, EMBASE, ProQuest, and Ovid databases up to 30 June 2021 to find studies that assessed the effects of curcumin-related compounds in mild to severe COVID-19 patients. Six studies were identified which showed that curcumin supplementation led to a significant decrease in common symptoms, duration of hospitalization and deaths. In addition, all of these studies showed that the intervention led to amelioration of cytokine storm effects thought to be a driving force in severe COVID-19 cases. This was seen as a significant (p < 0.05) decrease in proinflammatory cytokines such as IL1β and IL6, with a concomitant significant (p < 0.05) increase in anti-inflammatory cytokines, including IL-10, IL-35 and TGF-α. Taken together, these findings suggested that curcumin exerts its beneficial effects through at least partial restoration of pro-inflammatory/anti-inflammatory balance. In conclusion, curcumin supplementation may offer an efficacious and safe option for improving COVID-19 disease outcomes. We highlight the point that future clinical studies of COVID-19 disease should employ larger cohorts of patients in different clinical settings with standardized preparations of curcumin-related compounds.</jats:p>",
"alternative-id": [
"nu14020256"
],
"author": [
{
"affiliation": [],
"family": "Vahedian-Azimi",
"given": "Amir",
"sequence": "first"
},
{
"affiliation": [],
"family": "Abbasifard",
"given": "Mitra",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Rahimi-Bashar",
"given": "Farshid",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Guest",
"given": "Paul C.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Majeed",
"given": "Muhammed",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Mohammadi",
"given": "Asadollah",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-6690-6874",
"affiliation": [],
"authenticated-orcid": false,
"family": "Banach",
"given": "Maciej",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Jamialahmadi",
"given": "Tannaz",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-8656-1444",
"affiliation": [],
"authenticated-orcid": false,
"family": "Sahebkar",
"given": "Amirhossein",
"sequence": "additional"
}
],
"container-title": [
"Nutrients"
],
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2022,
1,
10
]
],
"date-time": "2022-01-10T04:06:15Z",
"timestamp": 1641787575000
},
"deposited": {
"date-parts": [
[
2022,
1,
10
]
],
"date-time": "2022-01-10T05:05:33Z",
"timestamp": 1641791133000
},
"indexed": {
"date-parts": [
[
2022,
1,
10
]
],
"date-time": "2022-01-10T05:51:10Z",
"timestamp": 1641793870842
},
"is-referenced-by-count": 0,
"issn-type": [
{
"type": "electronic",
"value": "2072-6643"
}
],
"issue": "2",
"issued": {
"date-parts": [
[
2022,
1,
7
]
]
},
"journal-issue": {
"issue": "2",
"published-online": {
"date-parts": [
[
2022,
1
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
1,
7
]
],
"date-time": "2022-01-07T00:00:00Z",
"timestamp": 1641513600000
}
}
],
"link": [
{
"URL": "https://www.mdpi.com/2072-6643/14/2/256/pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1968",
"original-title": [],
"page": "256",
"prefix": "10.3390",
"published": {
"date-parts": [
[
2022,
1,
7
]
]
},
"published-online": {
"date-parts": [
[
2022,
1,
7
]
]
},
"publisher": "MDPI AG",
"reference": [
{
"key": "ref1",
"unstructured": "COVID-19 Dashboardhttps://coronavirus.jhu.edu/map.html"
},
{
"key": "ref2",
"unstructured": "Coronavirus (COVID-19) Vaccinationshttps://ourworldindata.org/covid-vaccinations"
},
{
"DOI": "10.1002/rmv.2277",
"doi-asserted-by": "publisher",
"key": "ref3"
},
{
"DOI": "10.3389/fmicb.2021.698169",
"doi-asserted-by": "publisher",
"key": "ref4"
},
{
"DOI": "10.1016/j.lfs.2020.117900",
"doi-asserted-by": "publisher",
"key": "ref5"
},
{
"DOI": "10.5578/tt.20219818",
"doi-asserted-by": "publisher",
"key": "ref6"
},
{
"DOI": "10.3389/fimmu.2020.01648",
"doi-asserted-by": "publisher",
"key": "ref7"
},
{
"DOI": "10.1016/j.bbrc.2020.11.043",
"doi-asserted-by": "publisher",
"key": "ref8"
},
{
"DOI": "10.12968/hmed.2021.0112",
"doi-asserted-by": "publisher",
"key": "ref9"
},
{
"DOI": "10.1111/ijlh.13547",
"doi-asserted-by": "publisher",
"key": "ref10"
},
{
"DOI": "10.1007/s12011-021-02623-3",
"doi-asserted-by": "publisher",
"key": "ref11"
},
{
"DOI": "10.3389/fphar.2021.643119",
"doi-asserted-by": "publisher",
"key": "ref12"
},
{
"DOI": "10.2174/0929867327666200515101228",
"doi-asserted-by": "publisher",
"key": "ref13"
},
{
"DOI": "10.31080/ASPS.2020.05.0657",
"doi-asserted-by": "publisher",
"key": "ref14"
},
{
"DOI": "10.1016/j.prp.2019.152556",
"doi-asserted-by": "publisher",
"key": "ref15"
},
{
"DOI": "10.1007/978-3-030-56153-6_6",
"article-title": "Protective effects of curcumin on endothelium: An updated review. Studies on Biomarkers and New Targets in Aging Research in Iran",
"author": "Alidadi",
"doi-asserted-by": "crossref",
"first-page": "103",
"journal-title": "Adv. Exp. Med. Biol.",
"key": "ref16",
"volume": "1291",
"year": "2021"
},
{
"DOI": "10.1016/j.pcad.2021.06.010",
"doi-asserted-by": "publisher",
"key": "ref17"
},
{
"DOI": "10.2174/1381612822666161006151605",
"doi-asserted-by": "publisher",
"key": "ref18"
},
{
"DOI": "10.1016/j.fertnstert.2010.07.1071",
"doi-asserted-by": "publisher",
"key": "ref19"
},
{
"DOI": "10.1055/s-0044-101752",
"doi-asserted-by": "publisher",
"key": "ref20"
},
{
"DOI": "10.1002/jcp.28122",
"doi-asserted-by": "publisher",
"key": "ref21"
},
{
"DOI": "10.1002/ptr.6738",
"doi-asserted-by": "publisher",
"key": "ref22"
},
{
"DOI": "10.1007/978-0-387-46401-5_1",
"article-title": "Curcumin: The Indian solid gold",
"author": "Aggarwal",
"doi-asserted-by": "crossref",
"first-page": "1",
"journal-title": "Adv. Exp. Med. Biol.",
"key": "ref23",
"volume": "595",
"year": "2007"
},
{
"DOI": "10.1007/s00018-008-7452-4",
"doi-asserted-by": "publisher",
"key": "ref24"
},
{
"DOI": "10.1007/978-3-030-56153-6_1",
"article-title": "Research in the middle east into the health benefits of curcumin",
"author": "Guest",
"doi-asserted-by": "crossref",
"first-page": "1",
"journal-title": "Adv. Exp. Med. Biol.",
"key": "ref25",
"volume": "1291",
"year": "2021"
},
{
"DOI": "10.3390/foods6100092",
"doi-asserted-by": "publisher",
"key": "ref26"
},
{
"DOI": "10.1007/978-3-030-64872-5_10",
"article-title": "Effect of curcumin on severity of functional dyspepsia: A triple blinded clinical trial",
"author": "Panahi",
"doi-asserted-by": "crossref",
"first-page": "119",
"journal-title": "Adv. Exp. Med. Biol.",
"key": "ref27",
"volume": "1308",
"year": "2021"
},
{
"DOI": "10.1186/s13063-021-05224-6",
"doi-asserted-by": "publisher",
"key": "ref28"
},
{
"DOI": "10.1007/s00394-019-01916-7",
"doi-asserted-by": "publisher",
"key": "ref29"
},
{
"DOI": "10.1007/978-3-030-64872-5_1",
"article-title": "The effect of curcumin supplementation on pulse wave velocity in patients with metabolic syndrome: A randomized, double-blind, placebo-controlled trial",
"author": "Alidadi",
"doi-asserted-by": "crossref",
"first-page": "1",
"journal-title": "Adv. Exp. Med. Biol.",
"key": "ref30",
"volume": "1308",
"year": "2021"
},
{
"DOI": "10.1093/ptj/89.9.873",
"doi-asserted-by": "publisher",
"key": "ref31"
},
{
"DOI": "10.1186/s40779-020-0233-6",
"doi-asserted-by": "publisher",
"key": "ref32"
},
{
"DOI": "10.1016/0197-2456(95)00134-4",
"doi-asserted-by": "publisher",
"key": "ref33"
},
{
"DOI": "10.1002/fsn3.2226",
"doi-asserted-by": "publisher",
"key": "ref34"
},
{
"DOI": "10.1002/ptr.7004",
"doi-asserted-by": "publisher",
"key": "ref35"
},
{
"DOI": "10.1016/j.intimp.2020.107088",
"doi-asserted-by": "publisher",
"key": "ref36"
},
{
"DOI": "10.1002/jcp.30233",
"doi-asserted-by": "publisher",
"key": "ref37"
},
{
"DOI": "10.1016/j.lfs.2021.119437",
"doi-asserted-by": "publisher",
"key": "ref38"
},
{
"DOI": "10.3389/fphar.2021.669362",
"doi-asserted-by": "publisher",
"key": "ref39"
},
{
"DOI": "10.7150/ijbs.59534",
"doi-asserted-by": "publisher",
"key": "ref40"
},
{
"DOI": "10.1007/s12016-021-08866-1",
"doi-asserted-by": "publisher",
"key": "ref41"
},
{
"DOI": "10.1186/s12879-021-06278-2",
"doi-asserted-by": "publisher",
"key": "ref42"
},
{
"DOI": "10.1186/s12879-021-06457-1",
"doi-asserted-by": "publisher",
"key": "ref43"
},
{
"DOI": "10.1111/imm.13223",
"doi-asserted-by": "publisher",
"key": "ref44"
},
{
"DOI": "10.1111/dth.13893",
"doi-asserted-by": "publisher",
"key": "ref45"
},
{
"DOI": "10.1038/s41591-020-1051-9",
"doi-asserted-by": "publisher",
"key": "ref46"
},
{
"DOI": "10.1007/978-3-030-59261-5_11",
"article-title": "The Novel Coronavirus and Inflammation",
"author": "George",
"doi-asserted-by": "crossref",
"first-page": "127",
"journal-title": "Adv. Exp. Med. Biol.",
"key": "ref47",
"volume": "1321",
"year": "2021"
},
{
"DOI": "10.1128/CMR.00299-20",
"doi-asserted-by": "publisher",
"key": "ref48"
},
{
"DOI": "10.1371/journal.pone.0253894",
"doi-asserted-by": "publisher",
"key": "ref49"
},
{
"DOI": "10.1016/j.intimp.2018.05.018",
"doi-asserted-by": "publisher",
"key": "ref50"
},
{
"DOI": "10.1016/j.jneuroim.2019.01.007",
"doi-asserted-by": "publisher",
"key": "ref51"
},
{
"article-title": "Immunomodulatory effects of curcumin in rheumatoid arthritis: Evidence from molecular mechanisms to clinical outcomes",
"author": "Haftcheshmeh",
"first-page": "1",
"journal-title": "Rev. Physiol. Biochem. Pharmacol.",
"key": "ref52",
"volume": "179",
"year": "2021"
},
{
"DOI": "10.1007/978-3-030-56153-6_15",
"article-title": "The clinical use of curcumin for the treatment of rheumatoid arthritis: A systematic review of clinical trials",
"author": "Bagherniya",
"doi-asserted-by": "crossref",
"first-page": "251",
"journal-title": "Adv. Exp. Med. Biol.",
"key": "ref53",
"volume": "1291",
"year": "2021"
},
{
"DOI": "10.1080/10408398.2017.1358139",
"doi-asserted-by": "publisher",
"key": "ref54"
},
{
"DOI": "10.2147/IJN.S208332",
"doi-asserted-by": "publisher",
"key": "ref55"
},
{
"DOI": "10.3390/ma14123332",
"doi-asserted-by": "publisher",
"key": "ref56"
},
{
"DOI": "10.1093/nutrit/nuaa114",
"doi-asserted-by": "publisher",
"key": "ref57"
},
{
"DOI": "10.1016/j.cyto.2021.155541",
"doi-asserted-by": "publisher",
"key": "ref58"
},
{
"DOI": "10.1007/112_2016_3",
"article-title": "Curcumin as a MicroRNA regulator in cancer: A review",
"author": "Momtazi",
"doi-asserted-by": "crossref",
"first-page": "1",
"journal-title": "Rev. Physiol. Biochem. Pharmacol.",
"key": "ref59",
"volume": "171",
"year": "2016"
},
{
"DOI": "10.1016/j.fct.2020.111727",
"doi-asserted-by": "publisher",
"key": "ref60"
},
{
"DOI": "10.3389/fimmu.2012.00275",
"doi-asserted-by": "publisher",
"key": "ref61"
},
{
"DOI": "10.1158/2326-6066.CIR-16-0193",
"doi-asserted-by": "publisher",
"key": "ref62"
},
{
"DOI": "10.1111/bph.13621",
"doi-asserted-by": "publisher",
"key": "ref63"
},
{
"DOI": "10.1021/np1007262",
"doi-asserted-by": "publisher",
"key": "ref64"
},
{
"DOI": "10.1208/s12248-012-9432-8",
"doi-asserted-by": "publisher",
"key": "ref65"
}
],
"reference-count": 65,
"references-count": 65,
"relation": {},
"score": 1,
"short-container-title": [
"Nutrients"
],
"short-title": [],
"source": "Crossref",
"subject": [
"Food Science",
"Nutrition and Dietetics"
],
"subtitle": [],
"title": [
"Effectiveness of Curcumin on Outcomes of Hospitalized COVID-19 Patients: A Systematic Review of Clinical Trials"
],
"type": "journal-article",
"volume": "14"
}