Vitamin D Status and SARS-CoV-2 Infection in a Cohort of Kidney Transplanted Patients
et al., Nutrients, doi:10.3390/nu14020317, Jan 2022
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 136 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 61 COVID+ kidney transplant patients and 122 matched controls, showing significantly lower vitamin D levels in COVID+ patients, and lower cases with vitamin D supplementation, without statistical significance.
This is the 67th of 136 COVID-19 controlled studies for vitamin D, which collectively show efficacy with p<0.0000000001.
40 studies are RCTs, which show efficacy with p=0.0000001.
|
risk of case, 33.0% lower, OR 0.67, p = 0.21, treatment 32 of 60 (53.3%) cases,
75 of 119 (63.0%) controls, NNT 11, case control OR, vitamin D supplementation for ≥3 months in the last year.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Regalia et al., 13 Jan 2022, retrospective, Italy, peer-reviewed, 10 authors, dosage varies.
Vitamin D Status and SARS-CoV-2 Infection in a Cohort of Kidney Transplanted Patients
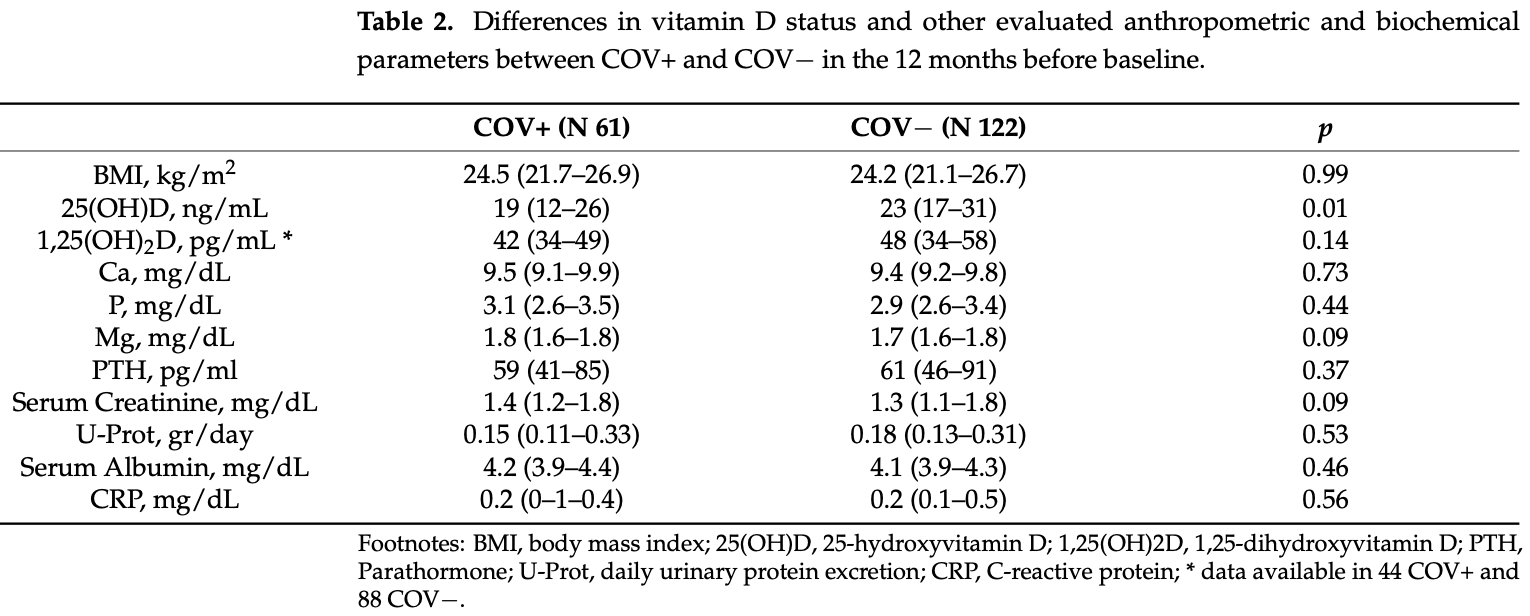
Nutrients, doi:10.3390/nu14020317
Background: Recently the protective role of 25-hydroxyvitamin D (25(OH)D) against viral infections has been hypothesized. We evaluated the association between vitamin D status and SARS-CoV-2 infection susceptibility and severity in a cohort of kidney transplanted patients (KTxp). Methods: A total of 61 KTxp with SARS-CoV-2 infection (COV+) were matched with 122 healthy KTxp controls (COV−). Main biochemical parameters at 1, 6, and 12 months before SARS-CoV-2 infection were recorded. Vitamin D status was considered as the mean of two 25(OH)D measures obtained 6 ± 2 months apart during the last year. The severity of SARS-CoV-2 infection was based on the need for hospitalization (HOSP+) and death (D+). Results: 25(OH)D levels were lower in COV+ than in controls [19(12-26) vs. 23(17-31) ng/mL, p = 0.01]. No differences among the other biochemical parameters were found. The SARS-CoV-2 infection discriminative power of 25(OH)D was evaluated by ROC-curve (AUC 0.61, 95% CI 0.5-0.7, p = 0.01). 25(OH)D was not significantly different between vs. 20(15-26) ng/mL, p = 0.19] and between D+ and D− [14(6-23) vs. 20(14-26) ng/mL, p = 0.22] and had no significant correlation with disease length. Conclusions: During the year preceding the infection, 25(OH)D levels were lower in COV+ KTxp in comparison with controls matched for demographic features and comorbidities. No significant association between vitamin D status and SARS-CoV-2 infection related outcomes was found.
Informed Consent Statement: Given the observational and retrospective nature of the study, it was not necessary to obtain informed consent from patients. In any case, all of the data were collected digitally, analyzed, and reported in the results in a totally and anonymous manner.
Conflicts of Interest: The authors declare no conflict of interest.
References
Abdrabbo, Birch, Brandt, Cicigoi, Coffey et al., Vitamin D and COVID-19: A review on the role of vitamin D in preventing and reducing the severity of COVID-19 infection, Protein Sci, doi:10.1002/pro.4190
Akalin, Azzi, Bartash, Seethamraju, Parides et al., Covid-19 and Kidney Transplantation, N. Engl. J. Med, doi:10.1056/NEJMc2011117
Alfieri, Regalia, Zanoni, Vettoretti, Cozzolino et al., The Importance of Adherence in the Treatment of Secondary Hyperparathyroidism, Blood Purif, doi:10.1159/000492918
Alfieri, Ruzhytska, Vettoretti, Caldiroli, Cozzolino et al., Native Hypovitaminosis D in CKD Patients: From Experimental Evidence to Clinical Practice, Nutrients, doi:10.3390/nu11081918
Baeke, Takiishi, Korf, Gysemans, Mathieu et al., Modulator of the immune system, Curr. Opin. Pharmacol, doi:10.1016/j.coph.2010.04.001
Bassatne, Basbous, Chakhtoura, El Zein, Rahme et al., The link between COVID-19 and Vitamin D (VIVID): A systematic review and meta-analysis, Metabolism, doi:10.1016/j.metabol.2021.154753
Benskin, A Basic Review of the Preliminary Evidence That COVID-19 Risk and Severity Is Increased in Vitamin D Deficiency, Front. Public Health, doi:10.3389/fpubh.2020.00513
Bouillon, Quesada-Gomez, Vitamin D Endocrine System and COVID-19, JBMR Plus, doi:10.1002/jbm4.10576
Boulkrane, Ilina, Melchakov, Fedotova, Drago et al., COVID-19 Disease and Vitamin D: A Mini-Review, Front. Pharmacol, doi:10.3389/fphar.2020.604579
Brenner, Vitamin D Supplementation to Prevent COVID-19 Infections and Deaths-Accumulating Evidence from Epidemiological and Intervention Studies Calls for Immediate Action, Nutrients, doi:10.3390/nu13020411
Brito, Ribeiro, Daltro, Silva, The possible benefits of vitamin D in COVID-19, Nutrition, doi:10.1016/j.nut.2021.111356
Campi, Gennari, Merlotti, Mingiano, Frosali et al., Vitamin D and COVID-19 severity and related mortality: A prospective study in Italy, BMC Infect. Dis
Campise, Alfieri, Perego, Tamborini, Cresseri et al., COVID-19 Infection in Kidney Transplant Patients: An Italian One Year Single Centre Experience, Pathogens, doi:10.3390/pathogens10080964
Castillo, Costa, Barrios, Díaz, Miranda et al., Effect of calcifediol treatment and best available therapy versus best available therapy on intensive care unit admission and mortality among patients hospitalized for COVID-19: A pilot randomized clinical study, J. Steroid Biochem. Mol. Biol, doi:10.1016/j.jsbmb.2020.105751
Crafa, Cannarella, Condorelli, Mongioì, Barbagallo et al., Influence of 25-hydroxy-cholecalciferol levels on SARS-CoV-2 infection and COVID-19 severity: A systematic review and meta-analysis, EClinicalMedicine, doi:10.1016/j.eclinm.2021.100967
D'avolio, Avataneo, Manca, Cusato, De Nicolò et al., 25-Hydroxyvitamin D Concentrations Are Lower in Patients with Positive PCR for SARS-CoV-2, Nutrients, doi:10.3390/nu12051359
De Smet, De Smet, Herroelen, Gryspeerdt, Martens, Serum 25(OH)D Level on Hospital Admission Associated with COVID-19 Stage and Mortality, Am. J. Clin. Pathol, doi:10.1093/ajcp/aqaa252
Drucker, Diabetes, obesity, metabolism, and SARS-CoV-2 infection: The end of the beginning, Cell Metab, doi:10.1016/j.cmet.2021.01.016
Flythe, Assimon, Tugman, Chang, Gupta et al., Characteristics and Outcomes of Individuals with Pre-existing Kidney Disease and COVID-19 Admitted to Intensive Care Units in the United States, Am. J. Kidney Dis, doi:10.1053/j.ajkd.2020.09.003
Greiller, Martineau, Modulation of the Immune Response to Respiratory Viruses by Vitamin D, Nutrients, doi:10.3390/nu7064240
Grove, Osokogu, Al-Khudairy, Mehrabian, Zanganeh et al., Association between vitamin D supplementation or serum vitamin D level and susceptibility to SARS-CoV-2 infection or COVID-19 including clinical course, morbidity and mortality outcomes? A systematic review, BMJ Open, doi:10.1136/bmjopen-2020-043737
Guan, Ni, Hu, Liang, Ou et al., Clinical Characteristics of Coronavirus Disease in China, N. Engl. J. Med, doi:10.1056/NEJMoa2002032
Hernández, Nan, Fernandez-Ayala, García-Unzueta, Hernández-Hernández et al., Vitamin D Status in Hospitalized Patients with SARS-CoV-2
Jean, Souberbielle, Chazot, Vitamin D in Chronic Kidney Disease and Dialysis Patients, Nutrients, doi:10.3390/nu9040328
Jimenez, González-Parra, Riera, Rincón Bello, López-Herradón et al., Mortality in Hemodialysis Patients with COVID-19, the Effect of Paricalcitol or Calcimimetics, Nutrients, doi:10.3390/nu13082559
Kaufman, Niles, Kroll, Bi, Holick, SARS-CoV-2 positivity rates associated with circulating 25-hydroxyvitamin D levels, PLoS ONE, doi:10.1371/journal.pone.0239252
Kumar, Rathi, Haq, Wimalawansa, Sharma, Putative roles of vitamin D in modulating immune response and immunopathology associated with COVID-19, Virus Res, doi:10.1016/j.virusres.2020.198235
Malaguarnera, Vitamin D3 as Potential Treatment Adjuncts for COVID-19, Nutrients, doi:10.3390/nu12113512
Mercola, Grant, Wagner, Evidence Regarding Vitamin D and Risk of COVID-19 and Its Severity, Nutrients, doi:10.3390/nu12113361
Messa, Regalia, Alfieri, Nutritional Vitamin D in Renal Transplant Patients: Speculations and Reality, Nutrients, doi:10.3390/nu9060550
Mohan, Cherian, Sharma, Exploring links between vitamin D deficiency and COVID-19, PLoS Pathog, doi:10.1371/journal.ppat.1008874
Oristrell, Oliva, Subirana, Casado, Domínguez et al., Association of Calcitriol Supplementation with Reduced COVID-19 Mortality in Patients with Chronic Kidney Disease: A Population-Based Study, Biomedicines, doi:10.3390/biomedicines9050509
Ozturk, Turgutalp, Arici, Odabas, Altiparmak et al., Mortality analysis of COVID-19 infection in chronic kidney disease, haemodialysis and renal transplant patients compared with patients without kidney disease: A nationwide analysis from Turkey, Nephrol. Dial. Transplant, doi:10.1093/ndt/gfaa271
Pecora, Persico, Argentiero, Neglia, Esposito, The Role of Micronutrients in Support of the Immune Response against Viral Infections, Nutrients, doi:10.3390/nu12103198
Quesada-Gomez, Bouillon, Is calcifediol better than cholecalciferol for vitamin D supplementation?, Osteoporos Int, doi:10.1007/s00198-018-4520-y
Radujkovic, Hippchen, Tiwari-Heckler, Dreher, Boxberger et al., Vitamin D Deficiency and Outcome of COVID-19 Patients, Nutrients, doi:10.3390/nu12092757
Raisi-Estabragh, Martineau, Curtis, Moon, Darling et al., Vitamin D and coronavirus disease 2019 (COVID-19): Rapid evidence review, Aging Clin. Exp. Res, doi:10.1007/s40520-021-01894-z
Reynolds, Adhikari, Pulgarin, Troxel, Iturrate et al., Renin-Angiotensin-Aldosterone System Inhibitors and Risk of Covid-19, N. Engl. J. Med, doi:10.1056/NEJMoa2008975
Santaolalla, Beckmann, Kibaru, Josephs, Van Hemelrijck et al., Association between Vitamin D and Novel SARS-CoV-2 Respiratory Dysfunction-A Scoping Review of Current Evidence and Its Implication for COVID-19 Pandemic, Front. Physiol, doi:10.3389/fphys.2020.564387
Stroehlein, Wallqvist, Iannizzi, Mikolajewska, Metzendorf et al., Vitamin D supplementation for the treatment of COVID-19: A living systematic review, Cochrane Database Syst. Rev
Teshome, Adane, Girma, Mekonnen, The Impact of Vitamin D Level on COVID-19 Infection: Systematic Review and Meta-Analysis, Front. Public Health, doi:10.3389/fpubh.2021.624559
Zelzer, Prüller, Curcic, Sloup, Holter et al., Vitamin D Metabolites and Clinical Outcome in Hospitalized COVID-19 Patients, Nutrients, doi:10.3390/nu13072129
DOI record:
{
"DOI": "10.3390/nu14020317",
"ISSN": [
"2072-6643"
],
"URL": "http://dx.doi.org/10.3390/nu14020317",
"abstract": "<jats:p>Background: Recently the protective role of 25-hydroxyvitamin D (25(OH)D) against viral infections has been hypothesized. We evaluated the association between vitamin D status and SARS-CoV-2 infection susceptibility and severity in a cohort of kidney transplanted patients (KTxp). Methods: A total of 61 KTxp with SARS-CoV-2 infection (COV+) were matched with 122 healthy KTxp controls (COV−). Main biochemical parameters at 1, 6, and 12 months before SARS-CoV-2 infection were recorded. Vitamin D status was considered as the mean of two 25(OH)D measures obtained 6 ± 2 months apart during the last year. The severity of SARS-CoV-2 infection was based on the need for hospitalization (HOSP+) and death (D+). Results: 25(OH)D levels were lower in COV+ than in controls [19(12–26) vs. 23(17–31) ng/mL, p = 0.01]. No differences among the other biochemical parameters were found. The SARS-CoV-2 infection discriminative power of 25(OH)D was evaluated by ROC-curve (AUC 0.61, 95% CI 0.5–0.7, p = 0.01). 25(OH)D was not significantly different between HOSP+ and HOSP− [17(8–25) vs. 20(15–26) ng/mL, p = 0.19] and between D+ and D− [14(6–23) vs. 20(14–26) ng/mL, p = 0.22] and had no significant correlation with disease length. Conclusions: During the year preceding the infection, 25(OH)D levels were lower in COV+ KTxp in comparison with controls matched for demographic features and comorbidities. No significant association between vitamin D status and SARS-CoV-2 infection related outcomes was found.</jats:p>",
"alternative-id": [
"nu14020317"
],
"author": [
{
"affiliation": [],
"family": "Regalia",
"given": "Anna",
"sequence": "first"
},
{
"affiliation": [],
"family": "Benedetti",
"given": "Matteo",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Malvica",
"given": "Silvia",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-3860-5219",
"affiliation": [],
"authenticated-orcid": false,
"family": "Alfieri",
"given": "Carlo",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Campise",
"given": "Mariarosaria",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Cresseri",
"given": "Donata",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Gandolfo",
"given": "Maria Teresa",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Tripodi",
"given": "Federica",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Castellano",
"given": "Giuseppe",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Messa",
"given": "Piergiorgio",
"sequence": "additional"
}
],
"container-title": [
"Nutrients"
],
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2022,
1,
14
]
],
"date-time": "2022-01-14T08:14:03Z",
"timestamp": 1642148043000
},
"deposited": {
"date-parts": [
[
2022,
1,
18
]
],
"date-time": "2022-01-18T02:33:49Z",
"timestamp": 1642473229000
},
"indexed": {
"date-parts": [
[
2022,
1,
18
]
],
"date-time": "2022-01-18T06:00:41Z",
"timestamp": 1642485641245
},
"is-referenced-by-count": 0,
"issn-type": [
{
"type": "electronic",
"value": "2072-6643"
}
],
"issue": "2",
"issued": {
"date-parts": [
[
2022,
1,
13
]
]
},
"journal-issue": {
"issue": "2",
"published-online": {
"date-parts": [
[
2022,
1
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
1,
13
]
],
"date-time": "2022-01-13T00:00:00Z",
"timestamp": 1642032000000
}
}
],
"link": [
{
"URL": "https://www.mdpi.com/2072-6643/14/2/317/pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1968",
"original-title": [],
"page": "317",
"prefix": "10.3390",
"published": {
"date-parts": [
[
2022,
1,
13
]
]
},
"published-online": {
"date-parts": [
[
2022,
1,
13
]
]
},
"publisher": "MDPI AG",
"reference": [
{
"DOI": "10.1056/NEJMoa2002032",
"doi-asserted-by": "publisher",
"key": "ref1"
},
{
"DOI": "10.1016/j.coph.2010.04.001",
"doi-asserted-by": "publisher",
"key": "ref2"
},
{
"DOI": "10.3390/nu7064240",
"doi-asserted-by": "publisher",
"key": "ref3"
},
{
"DOI": "10.1002/pro.4190",
"doi-asserted-by": "publisher",
"key": "ref4"
},
{
"DOI": "10.3390/nu11081918",
"doi-asserted-by": "publisher",
"key": "ref5"
},
{
"DOI": "10.3390/nu9060550",
"doi-asserted-by": "publisher",
"key": "ref6"
},
{
"DOI": "10.3390/pathogens10080964",
"doi-asserted-by": "publisher",
"key": "ref7"
},
{
"DOI": "10.1056/NEJMc2011117",
"doi-asserted-by": "publisher",
"key": "ref8"
},
{
"key": "ref9"
},
{
"DOI": "10.3390/nu12103198",
"doi-asserted-by": "publisher",
"key": "ref10"
},
{
"DOI": "10.1371/journal.ppat.1008874",
"doi-asserted-by": "publisher",
"key": "ref11"
},
{
"DOI": "10.1016/j.nut.2021.111356",
"doi-asserted-by": "publisher",
"key": "ref12"
},
{
"DOI": "10.3390/nu13020411",
"doi-asserted-by": "publisher",
"key": "ref13"
},
{
"DOI": "10.3389/fphar.2020.604579",
"doi-asserted-by": "publisher",
"key": "ref14"
},
{
"DOI": "10.3390/nu12113512",
"doi-asserted-by": "publisher",
"key": "ref15"
},
{
"DOI": "10.1016/j.virusres.2020.198235",
"doi-asserted-by": "publisher",
"key": "ref16"
},
{
"DOI": "10.3390/nu12051359",
"doi-asserted-by": "publisher",
"key": "ref17"
},
{
"DOI": "10.1371/journal.pone.0239252",
"doi-asserted-by": "publisher",
"key": "ref18"
},
{
"DOI": "10.3389/fpubh.2021.624559",
"doi-asserted-by": "publisher",
"key": "ref19"
},
{
"DOI": "10.3389/fphys.2020.564387",
"doi-asserted-by": "publisher",
"key": "ref20"
},
{
"DOI": "10.1016/j.metabol.2021.154753",
"doi-asserted-by": "publisher",
"key": "ref21"
},
{
"DOI": "10.1007/s40520-021-01894-z",
"doi-asserted-by": "publisher",
"key": "ref22"
},
{
"DOI": "10.1016/j.eclinm.2021.100967",
"doi-asserted-by": "publisher",
"key": "ref23"
},
{
"DOI": "10.1136/bmjopen-2020-043737",
"doi-asserted-by": "publisher",
"key": "ref24"
},
{
"DOI": "10.3390/nu12113361",
"doi-asserted-by": "publisher",
"key": "ref25"
},
{
"DOI": "10.3389/fpubh.2020.00513",
"doi-asserted-by": "publisher",
"key": "ref26"
},
{
"DOI": "10.1186/s12879-021-06281-7",
"doi-asserted-by": "publisher",
"key": "ref27"
},
{
"DOI": "10.3390/nu12092757",
"doi-asserted-by": "publisher",
"key": "ref28"
},
{
"DOI": "10.1093/ajcp/aqaa252",
"doi-asserted-by": "publisher",
"key": "ref29"
},
{
"DOI": "10.1016/j.jsbmb.2020.105751",
"doi-asserted-by": "publisher",
"key": "ref30"
},
{
"article-title": "Vitamin D supplementation for the treatment of COVID-19: A living systematic review",
"author": "Stroehlein",
"first-page": "CD015043",
"journal-title": "Cochrane Database Syst. Rev.",
"key": "ref31",
"volume": "2021",
"year": "2021"
},
{
"DOI": "10.1002/jbm4.10576",
"doi-asserted-by": "publisher",
"key": "ref32"
},
{
"DOI": "10.3390/nu9040328",
"doi-asserted-by": "publisher",
"key": "ref33"
},
{
"DOI": "10.1053/j.ajkd.2020.09.003",
"doi-asserted-by": "publisher",
"key": "ref34"
},
{
"DOI": "10.1093/ndt/gfaa271",
"doi-asserted-by": "publisher",
"key": "ref35"
},
{
"DOI": "10.3390/biomedicines9050509",
"doi-asserted-by": "publisher",
"key": "ref36"
},
{
"DOI": "10.3390/nu13082559",
"doi-asserted-by": "publisher",
"key": "ref37"
},
{
"DOI": "10.1016/j.cmet.2021.01.016",
"doi-asserted-by": "publisher",
"key": "ref38"
},
{
"DOI": "10.1056/NEJMoa2008975",
"doi-asserted-by": "publisher",
"key": "ref39"
},
{
"DOI": "10.1159/000492918",
"doi-asserted-by": "publisher",
"key": "ref40"
},
{
"DOI": "10.1007/s00198-018-4520-y",
"doi-asserted-by": "publisher",
"key": "ref41"
},
{
"DOI": "10.3390/nu13072129",
"doi-asserted-by": "publisher",
"key": "ref42"
},
{
"DOI": "10.1210/clinem/dgaa733",
"doi-asserted-by": "publisher",
"key": "ref43"
}
],
"reference-count": 43,
"references-count": 43,
"relation": {},
"score": 1,
"short-container-title": [
"Nutrients"
],
"short-title": [],
"source": "Crossref",
"subject": [
"Food Science",
"Nutrition and Dietetics"
],
"subtitle": [],
"title": [
"Vitamin D Status and SARS-CoV-2 Infection in a Cohort of Kidney Transplanted Patients"
],
"type": "journal-article",
"volume": "14"
}
