Mortality in Hemodialysis Patients with COVID-19, the Effect of Paricalcitol or Calcimimetics
et al., Nutrients, doi:10.3390/nu13082559, Jul 2021
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 136 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
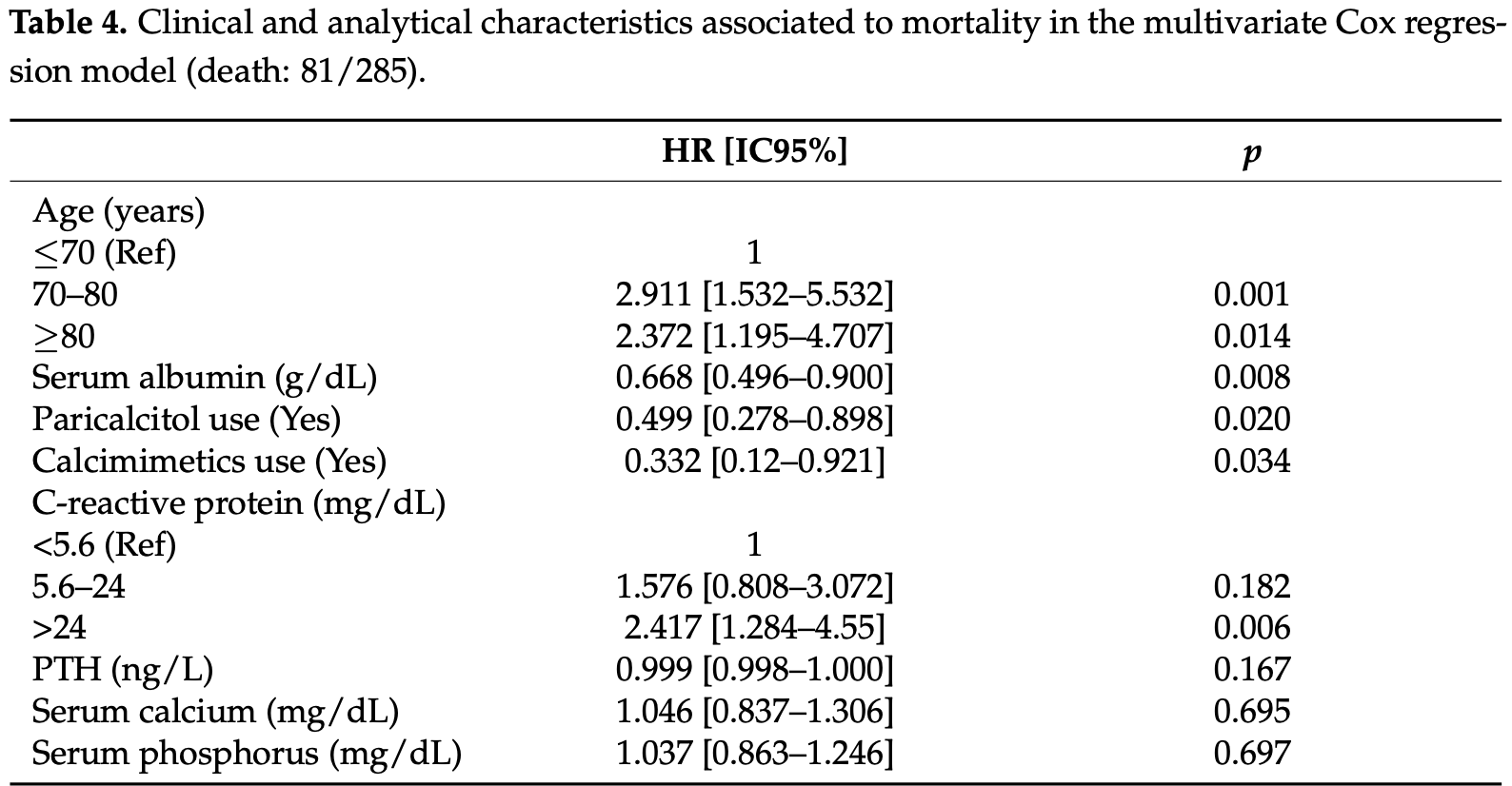
Retrospective 288 hemodialysis patients in Spain, 137 with existing vitamin D treatments (94 with paricalcitol), showing lower mortality with treatment. There was no significant difference in outcomes based on serum levels, however authors do not separate patients that received vitamin D treatment.
This is the 44th of 136 COVID-19 controlled studies for vitamin D, which collectively show efficacy with p<0.0000000001.
40 studies are RCTs, which show efficacy with p=0.0000001.
|
risk of death, 50.1% lower, HR 0.50, p = 0.02, treatment 16 of 94 (17.0%), control 65 of 191 (34.0%), NNT 5.9, adjusted per study, paricalcitol treatment, multivariate Cox regression.
|
|
risk of death, 50.7% lower, HR 0.49, p = 0.003, all vitamin D derivatives, univariate.
|
|
risk of death, 7.7% higher, OR 1.08, p = 0.81, high D levels 50, low D levels 110, >30 vs. <20ng/ml, RR approximated with OR, outcome based on serum levels, excluded in exclusion analyses:
many patients received vitamin D treatment.
|
|
risk of mechanical ventilation, 47.5% lower, OR 0.53, p = 0.56, high D levels 50, low D levels 110, >30 vs. <20ng/ml, RR approximated with OR, outcome based on serum levels, excluded in exclusion analyses:
many patients received vitamin D treatment.
|
|
risk of ICU admission, 12.2% lower, OR 0.88, p = 0.87, high D levels 50, low D levels 110, >30 vs. <20ng/ml, RR approximated with OR, outcome based on serum levels, excluded in exclusion analyses:
many patients received vitamin D treatment.
|
|
risk of hospitalization, 0.8% lower, OR 0.99, p = 0.98, high D levels 50, low D levels 110, >30 vs. <20ng/ml, RR approximated with OR, outcome based on serum levels, excluded in exclusion analyses:
many patients received vitamin D treatment.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Jimenez et al., 26 Jul 2021, retrospective, Spain, peer-reviewed, 21 authors, study period 12 March, 2020 - 21 May, 2020, dosage paricalcitol 0.9μg weekly.
Mortality in Hemodialysis Patients with COVID-19, the Effect of Paricalcitol or Calcimimetics
Nutrients, doi:10.3390/nu13082559
Background. In COVID-19 patients, low serum vitamin D (VD) levels have been associated with severe acute respiratory failure and poor prognosis. In regular hemodialysis (HD) patients, there is VD deficiency and markedly reduced calcitriol levels, which may predispose them to worse outcomes of COVID-19 infection. Some hemodialysis patients receive treatment with drugs for secondary hyperparathyroidism, which have well known pleiotropic effects beyond mineral metabolism. The aim of this study was to evaluate the impact of VD status and the administration of active vitamin D medications, used to treat secondary hyperparathyroidism, on survival in a cohort of COVID-19 positive HD patients. Methods. A cross-sectional retrospective observational study was conducted from 12 March to 21 May 2020 in 288 HD patients with positive PCR for SARS-CoV2. Patients were from 52 different centers in Spain. Results. The percent of HD patients with COVID-19 was 6.1% (288 out of 4743). Mortality rate was 28.4% (81/285). Three patients were lost to follow-up. Serum 25(OH)D (calcidiol) level was 17. 1 [10.6-27.5] ng/mL and was not significantly associated to mortality (OR 0.99 (0.97-1.01), p = 0.4). Patients receiving active vitamin D medications (16/94 (17%) vs. 65/191(34%), p = 0.003), including calcimimetics (4/49 (8.2%) vs. 77/236 (32.6%), p = 0.001), paricalcitol or calcimimetics (19/117 (16.2%) vs. 62/168 (36.9%); p < 0.001), and also those on both paricalcitol and calcimimetics, to treat secondary hyperparathyroidism (SHPTH) (1/26 (3.8%) vs. 80/259 (30.9%), p < 0.001) showed a lower mortality rate than patients receiving no treatment with either drug. Multivariate Cox regression analysis confirmed this increased survival. Conclusions.
References
Alfieri, Regalia, Zanoni, Vettoretti, Cozzolino et al., The Importance of Adherence in the Treatment of Secondary Hyperparathyroidism, Blood Purif, doi:10.1159/000492918
Ali, Role of vitamin D in preventing of COVID-19 infection, progression and severity, J. Infect. Public Health
Arcidiacono, Yang, Fernandez, Dusso, The induction of C/EBPβ contributes to vitamin D inhibition of ADAM17 expression and parathyroid hyperplasia in kidney disease, Nephrol. Dial. Transplant, doi:10.1093/ndt/gfu311
Arenas, Crespo, Pérez-Sáez, Collado, Redondo-Pachón et al., Clinical Profiles in Renal Patients with COVID-19, J. Clin. Med, doi:10.3390/jcm9082665
Atchison, Ortiz-Capisano, Beierwaltes, Acute activation of the calcium-sensing receptor inhibits plasma renin activity in vivo, Am. J. Physiol. Regul. Integr. Comp. Physiol, doi:10.1152/ajpregu.00238.2010
Autier, Mullie, Macacu, Dragomir, Boniol et al., Effect of vitamin D supplementation on non-skeletal disorders: A systematic review of meta-analyses and randomised trials, Lancet Diabetes Endocrinol, doi:10.1016/S2213-8587(17)30357-1
Carpagnano, Di Lecce, Quaranta, Zito, Buonamico et al., Vitamin D deficiency as a predictor of poor prognosis in patients with acute respiratory failure due to COVID-19, J. Endocrinol. Investig, doi:10.1007/s40618-020-01370-x
Castillo, Costa, Barrios, Díaz, Miranda et al., Effect of calcifediol treatment and best available therapy versus best available therapy on intensive care unit admission and mortality among patients hospitalized for COVID-19: A pilot randomized clinical study, J. Steroid Biochem. Mol. Biol, doi:10.1016/j.jsbmb.2020.105751
Chertow, Plone, Dillon, Burke, Slatopolsky, Hyperparathyroidism and dialysis vintage, Clin. Nephrol
Cucinotta, Vanelli, WHO Declares COVID-19 a Pandemic, Acta Biomed
Cui, Xu, Li, Qiao, Han et al., Vitamin D receptor activation regulates microglia polarization and oxidative stress in spontaneously hypertensive rats and angiotensin II-exposed microglial cells: Role of renin-angiotensin system, Redox Biol, doi:10.1016/j.redox.2019.101295
Dancer, Parekh, Lax, D'souza, Zheng et al., Vitamin D deficiency contributes directly to the acute respiratory distress syndrome (ARDS), Thorax, doi:10.1136/thoraxjnl-2014-206680
Dijkman, Jebbink, Deijs, Milewska, Pyrc et al., Replication-dependent downregulation of cellular angiotensin-converting enzyme 2 protein expression by human coronavirus NL63, J. Gen. Virol, doi:10.1099/vir.0.043919-0
Gassen, Niemeyer, Muth, Corman, Martinelli et al., SKP2 attenuates autophagy through Beclin1-ubiquitination and its inhibition reduces MERS-Coronavirus infection, Nat. Commun, doi:10.1038/s41467-019-13659-4
Goicoechea, Cámara, Macías, De Morales, Rojas et al., COVID-19: Clinical course and outcomes of 36 hemodialysis patients in Spain, Kidney Int, doi:10.1016/j.kint.2020.04.031
Grant, Lahore, Mcdonnell, Baggerly, French et al., Evidence that Vitamin D Supplementation Could Reduce Risk of Influenza and COVID-19 Infections and Deaths, Nutrients, doi:10.3390/nu12040988
Guerrero, De Oca, Aguilera-Tejero, Zafra, Rodriguez et al., The effect of vitamin D derivatives on vascular calcification associated with inflammation, Nephrol. Dial. Transplant, doi:10.1093/ndt/gfr555
Han, Li, Yang, King, Xiao et al., Counter-regulatory paracrine actions of FGF-23 and 1,25(OH)2D in macrophages, FEBS Lett, doi:10.1002/1873-3468.12040
Hastie, Mackay, Ho, Celis-Morales, Katikireddi et al., Vitamin D concentrations and COVID-19 infection in UK Biobank, Diabetes Metab. Syndr
Holick, Binkley, Bischoff-Ferrari, Gordon, Hanley et al., Evaluation, treatment, and prevention of vitamin D deficiency: An Endocrine Society clinical practice guideline, J. Clin. Endocrinol. Metab, doi:10.1210/jc.2011-0385
Huang, Wang, Li, Ren, Zhao et al., Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China, Lancet, doi:10.1016/S0140-6736(20)30183-5
Ilie, Stefanescu, Smith, The role of vitamin D in the prevention of coronavirus disease 2019 infection and mortality, Aging Clin. Exp. Res, doi:10.1007/s40520-020-01570-8
Isakova, Wahl, Vargas, Gutiérrez, Scialla et al., Fibroblast growth factor 23 is elevated before parathyroid hormone and phosphate in chronic kidney disease, Kidney Int, doi:10.1038/ki.2011.47
Jean, Souberbielle, Chazot, Vitamin D in Chronic Kidney Disease and Dialysis Patients, Nutrients, doi:10.3390/nu9040328
Jolliffe, Stefanidis, Wang, Kermani, Dimitrov et al., Vitamin D Metabolism Is Dysregulated in Asthma and Chronic Obstructive Pulmonary Disease, Am. J. Respir. Crit. Care Med, doi:10.1164/rccm.201909-1867OC
Leifheit-Nestler, Grabner, Hermann, Richter, Schmitz et al., Vitamin D treatment attenuates cardiac FGF23/FGFR4 signaling and hypertrophy in uremic rats, Nephrol. Dial. Transplant, doi:10.1093/ndt/gfw454
Martineau, Jolliffe, Hooper, Greenberg, Aloia et al., Vitamin D supplementation to prevent acute respiratory tract infections: Systematic review and meta-analysis of individual participant data, BMJ, doi:10.1136/bmj.i6583
Mcgonagle, Sharif, O'regan, Bridgewood, The Role of Cytokines including Interleukin-6 in COVID-19 induced Pneumonia and Macrophage Activation Syndrome-Like Disease, Autoimmun. Rev, doi:10.1016/j.autrev.2020.102537
Mehta, Mcauley, Brown, Sanchez, Tattersall et al., COVID-19: Consider cytokine storm syndromes and immunosuppression, Lancet, doi:10.1016/S0140-6736(20)30628-0
Meltzer, Best, Zhang, Vokes, Arora et al., Association of Vitamin D Levels, Race/Ethnicity, and Clinical Characteristics With COVID-19 Test Results, JAMA Netw. Open, doi:10.1001/jamanetworkopen.2021.4117
Merzon, Tworowski, Gorohovski, Vinker, Cohen et al., Low plasma 25(OH) vitamin D level is associated with increased risk of COVID-19 infection: An Israeli population-based study, FEBS J, doi:10.1111/febs.15495
Moe, Chertow, Parfrey, Kubo, Block et al., Fibroblast Growth Factor-23, and Cardiovascular Disease in Hemodialysis: The Evaluation of Cinacalcet HCl Therapy to Lower Cardiovascular Events (EVOLVE) Trial, Circulation, doi:10.1161/CIRCULATIONAHA.114.013876
Ostroverkhova, Hu, Tarasov, Melnikova, Porozov et al., Calcium-Sensing Receptor and Regulation of WNK Kinases in the Kidney, Cells, doi:10.3390/cells9071644
Palau, Riera, Soler, ADAM17 inhibition may exert a protective effect on COVID-19, Nephrol. Dial. Transplant, doi:10.1093/ndt/gfaa093
Panizo, Carrillo-López, Naves-Díaz, Solache-Berrocal, Martínez-Arias et al., Regulation of miR-29b and miR-30c by vitamin D receptor activators contributes to attenuate uraemia-induced cardiac fibrosis, Nephrol. Dial. Transplant, doi:10.1093/ndt/gfx060
Patel, Clarke, Wang, Fan, Parajuli et al., Angiotensin II induced proteolytic cleavage of myocardial ACE2 is mediated by TACE/ADAM-17: A positive feedback mechanism in the RAS, J. Mol. Cell. Cardiol, doi:10.1016/j.yjmcc.2013.11.017
Peiris, Guan, Yuen, Severe acute respiratory syndrome, Nat. Med, doi:10.1038/nm1143
Pilz, Zittermann, Trummer, Theiler-Schwetz, Lerchbaum et al., Vitamin D testing and treatment: A narrative review of current evidence, Endocr. Connect, doi:10.1530/EC-18-0432
Riera, Anguiano, Clotet, Ho, Rebull et al., Paricalcitol modulates ACE2 shedding and renal ADAM17 in NOD mice beyond proteinuria, Am. J. Physiol. Renal Physiol, doi:10.1152/ajprenal.00082.2015
Rincón, Moreso, López-Herradón, Fernández-Robres, Cidraque et al., The keys to control a COVID-19 outbreak in a haemodialysis unit, Clin. Kidney J, doi:10.1093/ckj/sfaa119
Rodriguez-Morales, Cardona-Ospina, Gutiérrez-Ocampo, Villamizar-Peña, Holguin-Rivera et al., Clinical, laboratory and imaging features of COVID-19: A systematic review and meta-analysis, Travel Med. Infect. Dis, doi:10.1016/j.tmaid.2020.101623
Rossaint, Oehmichen, Van Aken, Reuter, Pavenstädt et al., FGF23 signaling impairs neutrophil recruitment and host defense during CKD, J. Clin. Investig, doi:10.1172/JCI83470
Sodhi, Wohlford-Lenane, Yamaguchi, Prindle, Fulton et al., Attenuation of pulmonary ACE2 activity impairs inactivation of des-Arg9 bradykinin/BKB1R axis and facilitates LPS-induced neutrophil infiltration, Am. J. Physiol. Lung Cell. Mol. Physiol, doi:10.1152/ajplung.00498.2016
Sánchez-Álvarez, Pérez Fontán, Jiménez Martín, Pelícano, Reina et al., SARS-CoV-2 infection in patients on renal replacement therapy. Report of the COVID-19 Registry of the Spanish Society of Nephrology (SEN), Nefrologia, doi:10.1016/j.nefro.2020.04.002
Teng, Wolf, Lowrie, Ofsthun, Lazarus et al., Survival of Patients Undergoing Hemodialysis with Paricalcitol or Calcitriol Therapy, N. Engl. J. Med, doi:10.1056/NEJMoa022536
Torregrosa, Bover, Andía, Lorenzo, De Francisco et al., Recomendaciones de la Sociedad Española de Nefrología para el manejo de las alteraciones del metabolismo óseo-mineral en los pacientes con enfermedad renal crónica (S.E.N.-MM), Nefrologia
Wolf, Shah, Gutierrez, Ankers, Monroy et al., Vitamin D levels and early mortality among incident hemodialysis patients, Kidney Int, doi:10.1038/sj.ki.5002451
Wu, Leung, Leung, Nowcasting and forecasting the potential domestic and international spread of the 2019-nCoV outbreak originating in Wuhan, China: A modelling study, Lancet, doi:10.1016/S0140-6736(20)30260-9
Xu, Yang, Chen, Luo, Zhang et al., Vitamin D alleviates lipopolysaccharide-induced acute lung injury via regulation of the renin-angiotensin system, Mol. Med. Rep, doi:10.3892/mmr.2017.7546
Zhang, Darssan, Pascoe, Johnson, Pi et al., Vitamin D status and mortality risk among patients on dialysis: A systematic review and meta-analysis of observational studies, Nephrol. Dial. Transplant, doi:10.1093/ndt/gfy016
Zhang, Penninger, Li, Zhong, Slutsky, Angiotensin-converting enzyme 2 (ACE2) as a SARS-CoV-2 receptor: Molecular mechanisms and potential therapeutic target, Intensive Care Med, doi:10.1007/s00134-020-05985-9
Zheng, Peng, Xu, Zhao, Liu et al., Risk factors of critical & mortal COVID-19 cases: A systematic literature review and meta-analysis, J. Infect, doi:10.1016/j.jinf.2020.04.021
Zhou, Yu, Du, Fan, Liu et al., Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study, Lancet
DOI record:
{
"DOI": "10.3390/nu13082559",
"ISSN": [
"2072-6643"
],
"URL": "http://dx.doi.org/10.3390/nu13082559",
"abstract": "<jats:p>Background. In COVID-19 patients, low serum vitamin D (VD) levels have been associated with severe acute respiratory failure and poor prognosis. In regular hemodialysis (HD) patients, there is VD deficiency and markedly reduced calcitriol levels, which may predispose them to worse outcomes of COVID-19 infection. Some hemodialysis patients receive treatment with drugs for secondary hyperparathyroidism, which have well known pleiotropic effects beyond mineral metabolism. The aim of this study was to evaluate the impact of VD status and the administration of active vitamin D medications, used to treat secondary hyperparathyroidism, on survival in a cohort of COVID-19 positive HD patients. Methods. A cross-sectional retrospective observational study was conducted from 12 March to 21 May 2020 in 288 HD patients with positive PCR for SARS-CoV2. Patients were from 52 different centers in Spain. Results. The percent of HD patients with COVID-19 was 6.1% (288 out of 4743). Mortality rate was 28.4% (81/285). Three patients were lost to follow-up. Serum 25(OH)D (calcidiol) level was 17.1 [10.6–27.5] ng/mL and was not significantly associated to mortality (OR 0.99 (0.97–1.01), p = 0.4). Patients receiving active vitamin D medications (16/94 (17%) vs. 65/191(34%), p = 0.003), including calcimimetics (4/49 (8.2%) vs. 77/236 (32.6%), p = 0.001), paricalcitol or calcimimetics (19/117 (16.2%) vs. 62/168 (36.9%); p < 0.001), and also those on both paricalcitol and calcimimetics, to treat secondary hyperparathyroidism (SHPTH) (1/26 (3.8%) vs. 80/259 (30.9%), p < 0.001) showed a lower mortality rate than patients receiving no treatment with either drug. Multivariate Cox regression analysis confirmed this increased survival. Conclusions. Our findings suggest that the use of paricalcitol, calcimimetics or the combination of both, seem to be associated with the improvement of survival in HD patients with COVID-19. No correlation was found between serum VD levels and prognosis or outcomes in HD patients with COVID-19. Prospective studies and clinical trials are needed to support these findings.</jats:p>",
"alternative-id": [
"nu13082559"
],
"author": [
{
"affiliation": [],
"family": "Arenas Jimenez",
"given": "María Dolores",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0002-0701-3969",
"affiliation": [],
"authenticated-orcid": false,
"family": "González-Parra",
"given": "Emilio",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-4362-7965",
"affiliation": [],
"authenticated-orcid": false,
"family": "Riera",
"given": "Marta",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Rincón Bello",
"given": "Abraham",
"sequence": "additional"
},
{
"affiliation": [],
"family": "López-Herradón",
"given": "Ana",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Cao",
"given": "Higini",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Hurtado",
"given": "Sara",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Collado",
"given": "Silvia",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ribera",
"given": "Laura",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Barbosa",
"given": "Francesc",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Dapena",
"given": "Fabiola",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Torregrosa",
"given": "Vicent",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-4559-9083",
"affiliation": [],
"authenticated-orcid": false,
"family": "Broseta",
"given": "José-Jesús",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Soto Montañez",
"given": "Carlos",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-5015-7474",
"affiliation": [],
"authenticated-orcid": false,
"family": "Navarro-González",
"given": "Juan F.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ramos",
"given": "Rosa",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Bover",
"given": "Jordi",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Nogués-Solan",
"given": "Xavier",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-1852-2259",
"affiliation": [],
"authenticated-orcid": false,
"family": "Crespo",
"given": "Marta",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Dusso",
"given": "Adriana S.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Pascual",
"given": "Julio",
"sequence": "additional"
}
],
"container-title": "Nutrients",
"container-title-short": "Nutrients",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2021,
7,
27
]
],
"date-time": "2021-07-27T02:22:46Z",
"timestamp": 1627352566000
},
"deposited": {
"date-parts": [
[
2021,
7,
27
]
],
"date-time": "2021-07-27T17:01:55Z",
"timestamp": 1627405315000
},
"indexed": {
"date-parts": [
[
2024,
3,
20
]
],
"date-time": "2024-03-20T05:59:12Z",
"timestamp": 1710914352189
},
"is-referenced-by-count": 10,
"issue": "8",
"issued": {
"date-parts": [
[
2021,
7,
26
]
]
},
"journal-issue": {
"issue": "8",
"published-online": {
"date-parts": [
[
2021,
8
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
7,
26
]
],
"date-time": "2021-07-26T00:00:00Z",
"timestamp": 1627257600000
}
}
],
"link": [
{
"URL": "https://www.mdpi.com/2072-6643/13/8/2559/pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1968",
"original-title": [],
"page": "2559",
"prefix": "10.3390",
"published": {
"date-parts": [
[
2021,
7,
26
]
]
},
"published-online": {
"date-parts": [
[
2021,
7,
26
]
]
},
"publisher": "MDPI AG",
"reference": [
{
"DOI": "10.1016/S0140-6736(20)30260-9",
"doi-asserted-by": "publisher",
"key": "ref1"
},
{
"article-title": "WHO Declares COVID-19 a Pandemic",
"author": "Cucinotta",
"first-page": "157",
"journal-title": "Acta Biomed.",
"key": "ref2",
"volume": "91",
"year": "2020"
},
{
"DOI": "10.1016/S0140-6736(20)30183-5",
"doi-asserted-by": "publisher",
"key": "ref3"
},
{
"DOI": "10.1038/nm1143",
"doi-asserted-by": "publisher",
"key": "ref4"
},
{
"DOI": "10.1016/S0140-6736(20)30566-3",
"doi-asserted-by": "publisher",
"key": "ref5"
},
{
"DOI": "10.1016/j.autrev.2020.102537",
"doi-asserted-by": "publisher",
"key": "ref6"
},
{
"DOI": "10.1016/j.jinf.2020.04.021",
"doi-asserted-by": "publisher",
"key": "ref7"
},
{
"DOI": "10.3390/jcm9082665",
"doi-asserted-by": "publisher",
"key": "ref8"
},
{
"DOI": "10.1016/j.kint.2020.04.031",
"doi-asserted-by": "publisher",
"key": "ref9"
},
{
"DOI": "10.1093/ckj/sfaa119",
"doi-asserted-by": "publisher",
"key": "ref10"
},
{
"DOI": "10.1007/s40618-020-01370-x",
"doi-asserted-by": "publisher",
"key": "ref11"
},
{
"DOI": "10.1136/thoraxjnl-2014-206680",
"doi-asserted-by": "publisher",
"key": "ref12"
},
{
"DOI": "10.1136/bmj.i6583",
"doi-asserted-by": "publisher",
"key": "ref13"
},
{
"DOI": "10.1164/rccm.201909-1867OC",
"doi-asserted-by": "publisher",
"key": "ref14"
},
{
"DOI": "10.1530/EC-18-0432",
"doi-asserted-by": "publisher",
"key": "ref15"
},
{
"DOI": "10.1007/s00134-020-05985-9",
"doi-asserted-by": "publisher",
"key": "ref16"
},
{
"DOI": "10.1016/j.kisu.2017.04.001",
"doi-asserted-by": "publisher",
"key": "ref17"
},
{
"article-title": "Recomendaciones de la Sociedad Española de Nefrología para el manejo de las alteraciones del metabolismo óseo-mineral en los pacientes con enfermedad renal crónica (S.E.N.-MM)",
"author": "Torregrosa",
"first-page": "3",
"journal-title": "Nefrologia",
"key": "ref18",
"volume": "31",
"year": "2011"
},
{
"DOI": "10.1210/jc.2011-0385",
"doi-asserted-by": "publisher",
"key": "ref19"
},
{
"DOI": "10.3390/nu9040328",
"doi-asserted-by": "publisher",
"key": "ref20"
},
{
"DOI": "10.1016/j.nefro.2020.04.002",
"doi-asserted-by": "publisher",
"key": "ref21"
},
{
"DOI": "10.1016/j.tmaid.2020.101623",
"doi-asserted-by": "publisher",
"key": "ref22"
},
{
"article-title": "Hyperparathyroidism and dialysis vintage",
"author": "Chertow",
"first-page": "295",
"journal-title": "Clin. Nephrol.",
"key": "ref23",
"volume": "54",
"year": "2000"
},
{
"DOI": "10.1159/000492918",
"doi-asserted-by": "publisher",
"key": "ref24"
},
{
"DOI": "10.1093/ndt/gfy016",
"doi-asserted-by": "publisher",
"key": "ref25"
},
{
"DOI": "10.1016/S2213-8587(17)30357-1",
"doi-asserted-by": "publisher",
"key": "ref26"
},
{
"DOI": "10.3390/nu12040988",
"doi-asserted-by": "publisher",
"key": "ref27"
},
{
"DOI": "10.1007/s40520-020-01570-8",
"doi-asserted-by": "publisher",
"key": "ref28"
},
{
"DOI": "10.1016/j.jiph.2020.06.021",
"doi-asserted-by": "publisher",
"key": "ref29"
},
{
"DOI": "10.1016/j.dsx.2020.04.050",
"doi-asserted-by": "publisher",
"key": "ref30"
},
{
"DOI": "10.1111/febs.15495",
"doi-asserted-by": "publisher",
"key": "ref31"
},
{
"DOI": "10.1001/jamanetworkopen.2021.4117",
"doi-asserted-by": "publisher",
"key": "ref32"
},
{
"DOI": "10.1093/ndt/gfr555",
"doi-asserted-by": "publisher",
"key": "ref33"
},
{
"DOI": "10.1152/ajprenal.00082.2015",
"doi-asserted-by": "publisher",
"key": "ref34"
},
{
"DOI": "10.1093/ndt/gfw454",
"doi-asserted-by": "publisher",
"key": "ref35"
},
{
"DOI": "10.1093/ndt/gfx060",
"doi-asserted-by": "publisher",
"key": "ref36"
},
{
"DOI": "10.1016/j.jsbmb.2020.105751",
"doi-asserted-by": "publisher",
"key": "ref37"
},
{
"DOI": "10.1038/s41467-019-13659-4",
"doi-asserted-by": "publisher",
"key": "ref38"
},
{
"DOI": "10.3892/mmr.2017.7546",
"doi-asserted-by": "publisher",
"key": "ref39"
},
{
"DOI": "10.1016/j.redox.2019.101295",
"doi-asserted-by": "publisher",
"key": "ref40"
},
{
"DOI": "10.1099/vir.0.043919-0",
"doi-asserted-by": "publisher",
"key": "ref41"
},
{
"DOI": "10.1152/ajplung.00498.2016",
"doi-asserted-by": "publisher",
"key": "ref42"
},
{
"DOI": "10.1016/j.yjmcc.2013.11.017",
"doi-asserted-by": "publisher",
"key": "ref43"
},
{
"DOI": "10.1038/sj.ki.5002451",
"doi-asserted-by": "publisher",
"key": "ref44"
},
{
"DOI": "10.1056/NEJMoa022536",
"doi-asserted-by": "publisher",
"key": "ref45"
},
{
"DOI": "10.1093/ndt/gfu311",
"doi-asserted-by": "publisher",
"key": "ref46"
},
{
"DOI": "10.1093/ndt/gfaa093",
"doi-asserted-by": "publisher",
"key": "ref47"
},
{
"DOI": "10.3390/cells9071644",
"doi-asserted-by": "publisher",
"key": "ref48"
},
{
"DOI": "10.1152/ajpregu.00238.2010",
"doi-asserted-by": "publisher",
"key": "ref49"
},
{
"DOI": "10.1161/CIRCULATIONAHA.114.013876",
"doi-asserted-by": "publisher",
"key": "ref50"
},
{
"DOI": "10.1038/ki.2011.47",
"doi-asserted-by": "publisher",
"key": "ref51"
},
{
"DOI": "10.1002/1873-3468.12040",
"doi-asserted-by": "publisher",
"key": "ref52"
},
{
"DOI": "10.1016/S0140-6736(20)30628-0",
"doi-asserted-by": "publisher",
"key": "ref53"
},
{
"DOI": "10.1172/JCI83470",
"doi-asserted-by": "publisher",
"key": "ref54"
}
],
"reference-count": 54,
"references-count": 54,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.mdpi.com/2072-6643/13/8/2559"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Food Science",
"Nutrition and Dietetics"
],
"subtitle": [],
"title": "Mortality in Hemodialysis Patients with COVID-19, the Effect of Paricalcitol or Calcimimetics",
"type": "journal-article",
"volume": "13"
}
