Effects of Different Anticoagulation Doses on Moderate-to-Severe COVID-19 Pneumonia With Hypoxemia
et al., Cureus, doi:10.7759/cureus.43389, Aug 2023
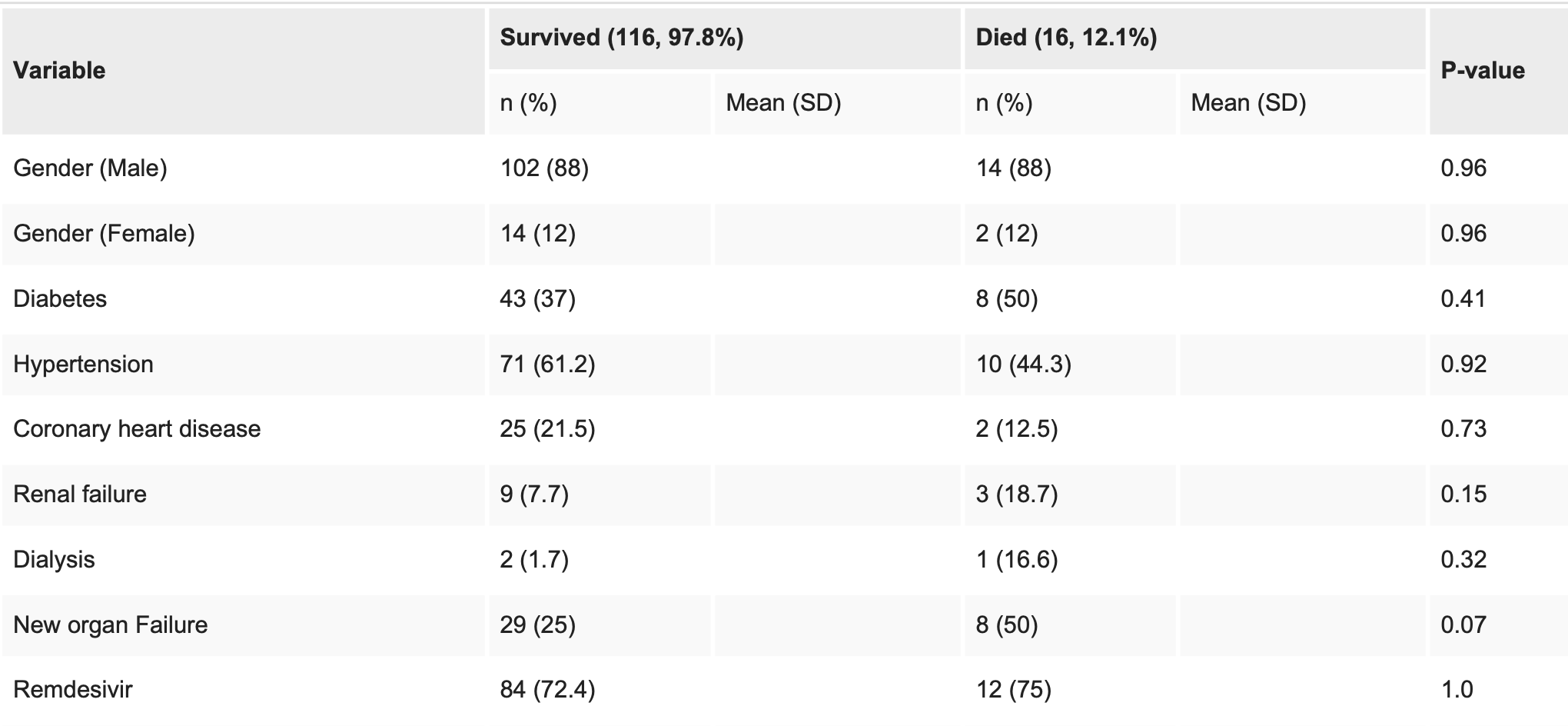
Retrospective 132 hospitalized COVID-19 patients in the USA, showing no significant difference in mortality with remdesivir in unadjusted results.
Gérard, Zhou, Wu, Kamo, Choi, Kim show increased risk of acute kidney injury, Leo, Briciu, Muntean, Petrov show increased risk of liver injury, and Negru, Cheng, Mohammed, Kwok show increased risk of cardiac disorders with remdesivir.
Standard of Care (SOC) for COVID-19 in the study country,
the USA, is very poor with very low average efficacy for approved treatments15.
Only expensive, high-profit treatments were approved for early treatment. Low-cost treatments were excluded, reducing the probability of early treatment due to access and cost barriers, and eliminating complementary and synergistic benefits seen with many low-cost treatments.
This study is excluded in the after exclusion results of meta-analysis:
unadjusted results with no group details.
|
risk of death, 12.5% higher, RR 1.12, p = 1.00, treatment 12 of 96 (12.5%), control 4 of 36 (11.1%).
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
1.
Gérard et al., Remdesivir and Acute Renal Failure: A Potential Safety Signal From Disproportionality Analysis of the WHO Safety Database, Clinical Pharmacology & Therapeutics, doi:10.1002/cpt.2145.
2.
Zhou et al., Acute Kidney Injury and Drugs Prescribed for COVID-19 in Diabetes Patients: A Real-World Disproportionality Analysis, Frontiers in Pharmacology, doi:10.3389/fphar.2022.833679.
3.
Wu et al., Acute Kidney Injury Associated With Remdesivir: A Comprehensive Pharmacovigilance Analysis of COVID-19 Reports in FAERS, Frontiers in Pharmacology, doi:10.3389/fphar.2022.692828.
4.
Kamo et al., Association of Antiviral Drugs for the Treatment of COVID-19 With Acute Renal Failure, In Vivo, doi:10.21873/invivo.13637.
5.
Choi et al., Comparative effectiveness of combination therapy with nirmatrelvir–ritonavir and remdesivir versus monotherapy with remdesivir or nirmatrelvir–ritonavir in patients hospitalised with COVID-19: a target trial emulation study, The Lancet Infectious Diseases, doi:10.1016/S1473-3099(24)00353-0.
6.
Kim et al., Investigating the Safety Profile of Fast‐Track COVID‐19 Drugs Using the FDA Adverse Event Reporting System Database: A Comparative Observational Study, Pharmacoepidemiology and Drug Safety, doi:10.1002/pds.70043.
7.
Leo et al., Hepatocellular liver injury in hospitalized patients affected by COVID-19: Presence of different risk factors at different time points, Digestive and Liver Disease, doi:10.1016/j.dld.2021.12.014.
8.
Briciu et al., Evolving Clinical Manifestations and Outcomes in COVID-19 Patients: A Comparative Analysis of SARS-CoV-2 Variant Waves in a Romanian Hospital Setting, Pathogens, doi:10.3390/pathogens12121453.
9.
Muntean et al., Effects of COVID-19 on the Liver and Mortality in Patients with SARS-CoV-2 Pneumonia Caused by Delta and Non-Delta Variants: An Analysis in a Single Centre, Pharmaceuticals, doi:10.3390/ph17010003.
10.
Petrov et al., The Effect of Potentially Hepatotoxic Medicinal Products on Alanine Transaminase Levels in COVID-19 Patients: A Case–Control Study, Safety and Risk of Pharmacotherapy, doi:10.30895/2312-7821-2025-458.
11.
Negru et al., Comparative Pharmacovigilance Analysis of Approved and Repurposed Antivirals for COVID-19: Insights from EudraVigilance Data, Biomedicines, doi:10.3390/biomedicines13061387.
12.
Cheng et al., Cardiovascular Safety of COVID-19 Treatments: A Disproportionality Analysis of Adverse Event Reports from the WHO VigiBase, Infectious Diseases and Therapy, doi:10.1007/s40121-025-01225-z.
13.
Mohammed et al., Bradycardia associated with remdesivir treatment in coronavirus disease 2019 patients: A propensity score-matched analysis, Medicine, doi:10.1097/MD.0000000000044501.
Nadeem et al., 12 Aug 2023, retrospective, USA, peer-reviewed, mean age 59.0, 6 authors, study period 1 March, 2020 - 28 February, 2022.
Contact: aminnadeem@yahoo.com.
Effects of Different Anticoagulation Doses on Moderate-to-Severe COVID-19 Pneumonia With Hypoxemia
Cureus, doi:10.7759/cureus.43389
Background COVID-19 is a prothrombotic disease that can cause thromboembolism and microthrombi, which could lead to multiorgan failure and death. Since COVID-19 is a relatively new disease, there are guidelines for anticoagulation dosing for COVID-19 patients without consensus on the dosing. We studied the effects of different doses of anticoagulation in hospitalized patients with COVID-19 pneumonia and hypoxemia on any differences in need for high-flow oxygen, mechanical ventilation, and mortality. We also analyzed the patient population who benefited most from anticoagulation.
Methodology We performed a retrospective chart review of all patients who were admitted with the diagnosis of COVID-19 infection with positive polymerase chain reaction, pneumonia (confirmed either by chest X-ray or CT chest), and hypoxemia (oxygen saturation of <94%, while on room air). These patients were studied for outcomes (the need for high-flow oxygen, the requirement for mechanical ventilation, and overall mortality) for different doses of anticoagulation (prophylactic, escalated, and therapeutic).
Results The sample consists of 132 subjects, predominantly males (116, 87%), with a mean age of 59 years and a standard deviation of 15. About one-third of the participants had diabetes, and more than 50% had hypertension. Additionally, 27 (20.3%) had a history of heart disease, and 70 (53%) of the subjects were admitted to the intensive care unit (ICU) at some point during the study. Among those admitted to the ICU, about 11 (8%) subjects required mechanical ventilation and 16 (12%) passed away during the study. Those who died had higher use of high-flow oxygen, noninvasive mechanical ventilation, and invasive mechanical ventilation and had a longer stay on mechanical ventilation. There was no significant difference in mortality or need for mechanical ventilation for any strategy of anticoagulation.
Conclusions Different doses of anticoagulation did not show any statistically significant relationship between the need for mechanical ventilation and mortality. More patients on high-flow oxygen had received escalated doses of anticoagulation as compared to those who were not on high-flow oxygen. Anticoagulation levels did not have any statistically significant effect on overall survival of patients.
Additional Information Disclosures Human subjects: Consent was obtained or waived by all participants in this study. Edward Hines Jr. Veterans Administration (VA) Hospital, Hines, IL, USA issued approval 21-015. The Institutional Review Board (IRB) committee at Edward Hines Jr. Veterans Administration (VA) Hospital, Hines, IL, USA, approved this study (approval number 21-015). Animal subjects: All authors have confirmed that this study did not involve animal subjects or tissue. Conflicts of interest: In compliance with the ICMJE uniform disclosure form, all authors declare the following: Payment/services info: All authors have declared that no financial support was received from any organization for the submitted work. Financial relationships: All authors have declared that they have no financial relationships at present or within the previous three years with any organizations that might have an interest in the submitted work. Other relationships: All authors have declared that there are no other relationships or activities that could appear to have influenced the submitted work.
References
Al-Samkari, Gupta, Leaf, Thrombosis, bleeding, and the observational effect of early therapeutic anticoagulation on survival in critically ill patients with COVID-19, Ann Intern Med, doi:10.7326/M20-6739?utm_medium=email&utm_source=transaction
Chen, Pan, Anatomical and pathological observation and analysis of SARS and COVID-19: microthrombosis is the main cause of death, Biol Proced Online, doi:10.1186/s12575-021-00142-y?utm_medium=email&utm_source=transaction
Covid-19, Coronavirus Disease 2019 (COVID-19) Treatment Guidelines, National Institutes of Health
Cuker, Tseng, Nieuwlaat, of Hematology living guidelines on the use of anticoagulation for thromboprophylaxis in patients with COVID-19: January 2022 update on the use of therapeutic-intensity anticoagulation in acutely ill patients, Blood Adv, doi:10.1182/bloodadvances.2022007561?utm_medium=email&utm_source=transaction
Giorgetti, Orazietti, Busardò, Pirani, Giorgetti, Died with or died of? Development and testing of a SARS CoV-2 significance score to assess the role of COVID-19 in the deaths of affected patients, Diagnostics (Basel), doi:10.3390/diagnostics11020190?utm_medium=email&utm_source=transaction
Henry, Vikse, Benoit, Favaloro, Lippi, Hyperinflammation and derangement of reninangiotensin-aldosterone system in COVID-19: a novel hypothesis for clinically suspected hypercoagulopathy and microvascular immunothrombosis, Clin Chim Acta, doi:10.1016/j.cca.2020.04.027?utm_medium=email&utm_source=transaction
Jhaveri, Meir, Chang, Thrombotic microangiopathy in a patient with COVID-19, Kidney Int, doi:10.1016/j.kint.2020.05.025?utm_medium=email&utm_source=transaction
Jose, Manuel, COVID-19 cytokine storm: the interplay between inflammation and coagulation, Lancet Respir Med, doi:10.1016/S2213-2600(20)30216-2?utm_medium=email&utm_source=transaction
Machhi, Herskovitz, Senan, The natural history, pathobiology, and clinical manifestations of SARS-CoV-2 infections, J Neuroimmune Pharmacol, doi:10.1007/s11481-020-09944-5?utm_medium=email&utm_source=transaction
Meizlish, Goshua, Liu, Intermediate-dose anticoagulation, aspirin, and in-hospital mortality in COVID-19: a propensity score-matched analysis, Am J Hematol, doi:10.1002/ajh.26102?utm_medium=email&utm_source=transaction
Nile, Nile, Qiu, Li, Jia et al., COVID-19: pathogenesis, cytokine storm and therapeutic potential of interferons, Cytokine Growth Factor Rev, doi:10.1016/j.cytogfr.2020.05.002?utm_medium=email&utm_source=transaction
Paranjpe, Fuster, Association of treatment dose anticoagulation with in-hospital survival among hospitalized patients with COVID-19, J Am Coll Cardiol, doi:10.1016/j.jacc.2020.05.001?utm_medium=email&utm_source=transaction
Pei, Yamana, Kandula, Kandula, Galanti et al., Burden and characteristics of COVID-19 in the United States during 2020, Nature, doi:10.1038/s41586-021-03914-4?utm_medium=email&utm_source=transaction
Rapkiewicz, Mai, Carsons, Megakaryocytes and platelet-fibrin thrombi characterize multiorgan thrombosis at autopsy in COVID-19: a case series, EClinicalMedicine, doi:10.1016/j.eclinm.2020.100434?utm_medium=email&utm_source=transaction
Sadeghipour, Talasaz, Rashidi, Effect of intermediate-dose vs standard-dose prophylactic anticoagulation on thrombotic events, extracorporeal membrane oxygenation treatment, or mortality among patients with COVID-19 admitted to the intensive care unit: the INSPIRATION randomized clinical trial, JAMA, doi:10.1001/jama.2021.4152?utm_medium=email&utm_source=transaction
Santoriello, Khairallah, Bomback, Postmortem kidney pathology findings in patients with COVID-19, J Am Soc Nephrol, doi:10.1681/ASN.2020050744?utm_medium=email&utm_source=transaction
Song, Fitzgerald, COVID-19, microangiopathy, hemostatic activation, and complement, J Clin Invest, doi:10.1172/JCI140183?utm_medium=email&utm_source=transaction
Tacquard, Mansour, Godon, Impact of high-dose prophylactic anticoagulation in critically ill patients with COVID-19 pneumonia, Chest, doi:10.1016/j.chest.2021.01.017?utm_medium=email&utm_source=transaction
Tang, Bai, Chen, Gong, Li et al., Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy, J Thromb Haemost, doi:10.1111/jth.14817?utm_medium=email&utm_source=transaction
Woolf, Chapman, Lee, COVID-19 as the leading cause of death in the United States, JAMA, doi:10.1001/jama.2020.24865?utm_medium=email&utm_source=transaction
Zhang, Liu, Wang, SARS-CoV-2 binds platelet ACE2 to enhance thrombosis in COVID-19, J Hematol Oncol, doi:10.1186/s13045-020-00954-7?utm_medium=email&utm_source=transaction
DOI record:
{
"DOI": "10.7759/cureus.43389",
"ISSN": [
"2168-8184"
],
"URL": "http://dx.doi.org/10.7759/cureus.43389",
"author": [
{
"affiliation": [],
"family": "Nadeem",
"given": "Amin Ur Rehman",
"sequence": "first"
},
{
"affiliation": [],
"family": "Naqvi",
"given": "Syed M",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Chandy",
"given": "Kurian G",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Nagineni",
"given": "Venkata V",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Nadeem",
"given": "Rashid",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Desai",
"given": "Shreya",
"sequence": "additional"
}
],
"container-title": "Cureus",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2023,
8,
12
]
],
"date-time": "2023-08-12T22:24:40Z",
"timestamp": 1691879080000
},
"deposited": {
"date-parts": [
[
2023,
8,
12
]
],
"date-time": "2023-08-12T22:24:45Z",
"timestamp": 1691879085000
},
"indexed": {
"date-parts": [
[
2023,
8,
12
]
],
"date-time": "2023-08-12T22:40:36Z",
"timestamp": 1691880036295
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2023,
8,
12
]
]
},
"language": "en",
"link": [
{
"URL": "https://www.cureus.com/articles/165816-effects-of-different-anticoagulation-doses-on-moderate-to-severe-covid-19-pneumonia-with-hypoxemia",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "297",
"original-title": [],
"prefix": "10.7759",
"published": {
"date-parts": [
[
2023,
8,
12
]
]
},
"published-print": {
"date-parts": [
[
2023,
8,
12
]
]
},
"publisher": "Springer Science and Business Media LLC",
"reference": [
{
"key": "ref1",
"unstructured": "WHO Coronavirus (COVID-19) Dashboard. (2023). Accessed. August 2, 2023: https://covid19.who.int/."
},
{
"DOI": "10.1038/s41586-021-03914-4",
"article-title": "Burden and characteristics of COVID-19 in the United States during 2020",
"author": "Pei S",
"doi-asserted-by": "publisher",
"journal-title": "Nature",
"key": "ref2",
"unstructured": "Pei S, Yamana TK, Kandula S, Kandula S, Galanti M, Shaman J. Burden and characteristics of COVID-19 in the United States during 2020. Nature. 2021, 598:338-41. 10.1038/s41586-021-03914-4",
"volume": "598",
"year": "2021"
},
{
"DOI": "10.1001/jama.2020.24865",
"article-title": "COVID-19 as the leading cause of death in the United States",
"author": "Woolf SH",
"doi-asserted-by": "publisher",
"journal-title": "JAMA",
"key": "ref3",
"unstructured": "Woolf SH, Chapman DA, Lee JH. COVID-19 as the leading cause of death in the United States. JAMA. 2021, 325:123-4. 10.1001/jama.2020.24865",
"volume": "325",
"year": "2021"
},
{
"DOI": "10.1007/s11481-020-09944-5",
"article-title": "The natural history, pathobiology, and clinical manifestations of SARS-CoV-2 infections",
"author": "Machhi J",
"doi-asserted-by": "publisher",
"journal-title": "J Neuroimmune Pharmacol",
"key": "ref4",
"unstructured": "Machhi J, Herskovitz J, Senan AM, et al.. The natural history, pathobiology, and clinical manifestations of SARS-CoV-2 infections. J Neuroimmune Pharmacol. 2020, 15:359-86. 10.1007/s11481-020-09944-5",
"volume": "15",
"year": "2020"
},
{
"DOI": "10.3390/diagnostics11020190",
"article-title": "Died with or died of? Development and testing of a SARS CoV-2 significance score to assess the role of COVID-19 in the deaths of affected patients",
"author": "Giorgetti A",
"doi-asserted-by": "publisher",
"journal-title": "Diagnostics (Basel)",
"key": "ref5",
"unstructured": "Giorgetti A, Orazietti V, Busardò FP, Pirani F, Giorgetti R. Died with or died of? Development and testing of a SARS CoV-2 significance score to assess the role of COVID-19 in the deaths of affected patients. Diagnostics (Basel). 2021, 11:10.3390/diagnostics11020190",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.1186/s12575-021-00142-y",
"article-title": "Anatomical and pathological observation and analysis of SARS and COVID-19: microthrombosis is the main cause of death",
"author": "Chen W",
"doi-asserted-by": "publisher",
"journal-title": "Biol Proced Online",
"key": "ref6",
"unstructured": "Chen W, Pan JY.. Anatomical and pathological observation and analysis of SARS and COVID-19: microthrombosis is the main cause of death. Biol Proced Online. 2021, 23:4. 10.1186/s12575-021-00142-y",
"volume": "23",
"year": "2021"
},
{
"DOI": "10.1186/s13045-020-00954-7",
"article-title": "SARS-CoV-2 binds platelet ACE2 to enhance thrombosis in COVID-19",
"author": "Zhang S",
"doi-asserted-by": "publisher",
"journal-title": "J Hematol Oncol",
"key": "ref7",
"unstructured": "Zhang S, Liu Y, Wang X, et al.. SARS-CoV-2 binds platelet ACE2 to enhance thrombosis in COVID-19. J Hematol Oncol. 2020, 13:120. 10.1186/s13045-020-00954-7",
"volume": "13",
"year": "2020"
},
{
"DOI": "10.1016/j.cca.2020.04.027",
"article-title": "Hyperinflammation and derangement of renin-angiotensin-aldosterone system in COVID-19: a novel hypothesis for clinically suspected hypercoagulopathy and microvascular immunothrombosis",
"author": "Henry BM",
"doi-asserted-by": "publisher",
"journal-title": "Clin Chim Acta",
"key": "ref8",
"unstructured": "Henry BM, Vikse J, Benoit S, Favaloro EJ, Lippi G. . Hyperinflammation and derangement of renin-angiotensin-aldosterone system in COVID-19: a novel hypothesis for clinically suspected hypercoagulopathy and microvascular immunothrombosis. Clin Chim Acta. 2020, 507:167-73. 10.1016/j.cca.2020.04.027",
"volume": "507",
"year": "2020"
},
{
"DOI": "10.1016/S2213-2600(20)30216-2",
"article-title": "COVID-19 cytokine storm: the interplay between inflammation and coagulation",
"author": "Jose RJ",
"doi-asserted-by": "publisher",
"journal-title": "Lancet Respir Med",
"key": "ref9",
"unstructured": "Jose RJ, Manuel A.. COVID-19 cytokine storm: the interplay between inflammation and coagulation. Lancet Respir Med. 2020, 8:e46-7. 10.1016/S2213-2600(20)30216-2",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1016/j.cytogfr.2020.05.002",
"article-title": "COVID-19: pathogenesis, cytokine storm and therapeutic potential of interferons",
"author": "Nile SH",
"doi-asserted-by": "publisher",
"journal-title": "Cytokine Growth Factor Rev",
"key": "ref10",
"unstructured": "Nile SH, Nile A, Qiu J, Li L, Jia X, Kai G. COVID-19: pathogenesis, cytokine storm and therapeutic potential of interferons. Cytokine Growth Factor Rev. 2020, 53:66-70. 10.1016/j.cytogfr.2020.05.002",
"volume": "53",
"year": "2020"
},
{
"DOI": "10.1111/jth.14817",
"article-title": "Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy",
"author": "Tang N",
"doi-asserted-by": "publisher",
"journal-title": "J Thromb Haemost",
"key": "ref11",
"unstructured": "Tang N, Bai H, Chen X, Gong J, Li D, Sun Z. Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy. J Thromb Haemost. 2020, 18:1094-9. 10.1111/jth.14817",
"volume": "18",
"year": "2020"
},
{
"DOI": "10.1016/j.jacc.2020.05.001",
"article-title": "Association of treatment dose anticoagulation with in-hospital survival among hospitalized patients with COVID-19",
"author": "Paranjpe I",
"doi-asserted-by": "publisher",
"journal-title": "J Am Coll Cardiol",
"key": "ref12",
"unstructured": "Paranjpe I, Fuster V, Lala A, et al.. Association of treatment dose anticoagulation with in-hospital survival among hospitalized patients with COVID-19. J Am Coll Cardiol. 2020, 76:122-4. 10.1016/j.jacc.2020.05.001",
"volume": "76",
"year": "2020"
},
{
"DOI": "10.1016/j.chest.2021.01.017",
"article-title": "Impact of high-dose prophylactic anticoagulation in critically ill patients with COVID-19 pneumonia",
"author": "Tacquard C",
"doi-asserted-by": "publisher",
"journal-title": "Chest",
"key": "ref13",
"unstructured": "Tacquard C, Mansour A, Godon A, et al.. Impact of high-dose prophylactic anticoagulation in critically ill patients with COVID-19 pneumonia. Chest. 2021, 159:2417-27. 10.1016/j.chest.2021.01.017",
"volume": "159",
"year": "2021"
},
{
"DOI": "10.7326/M20-6739",
"article-title": "Thrombosis, bleeding, and the observational effect of early therapeutic anticoagulation on survival in critically ill patients with COVID-19",
"author": "Al-Samkari H",
"doi-asserted-by": "publisher",
"journal-title": "Ann Intern Med",
"key": "ref14",
"unstructured": "Al-Samkari H, Gupta S, Leaf RK, et al.. Thrombosis, bleeding, and the observational effect of early therapeutic anticoagulation on survival in critically ill patients with COVID-19. Ann Intern Med. 2021, 174:622-32. 10.7326/M20-6739",
"volume": "174",
"year": "2021"
},
{
"DOI": "10.1001/jama.2021.4152",
"article-title": "Effect of intermediate-dose vs standard-dose prophylactic anticoagulation on thrombotic events, extracorporeal membrane oxygenation treatment, or mortality among patients with COVID-19 admitted to the intensive care unit: the INSPIRATION randomized clinical trial",
"author": "Sadeghipour P",
"doi-asserted-by": "publisher",
"journal-title": "JAMA",
"key": "ref15",
"unstructured": "Sadeghipour P, Talasaz AH, Rashidi F, et al.. Effect of intermediate-dose vs standard-dose prophylactic anticoagulation on thrombotic events, extracorporeal membrane oxygenation treatment, or mortality among patients with COVID-19 admitted to the intensive care unit: the INSPIRATION randomized clinical trial. JAMA. 2021, 325:1620-30. 10.1001/jama.2021.4152",
"volume": "325",
"year": "2021"
},
{
"DOI": "10.1002/ajh.26102",
"article-title": "Intermediate-dose anticoagulation, aspirin, and in-hospital mortality in COVID-19: a propensity score-matched analysis",
"author": "Meizlish ML",
"doi-asserted-by": "publisher",
"journal-title": "Am J Hematol",
"key": "ref16",
"unstructured": "Meizlish ML, Goshua G, Liu Y, et al.. Intermediate-dose anticoagulation, aspirin, and in-hospital mortality in COVID-19: a propensity score-matched analysis. Am J Hematol. 2021, 96:471-9. 10.1002/ajh.26102",
"volume": "96",
"year": "2021"
},
{
"DOI": "10.1172/JCI140183",
"article-title": "COVID-19, microangiopathy, hemostatic activation, and complement",
"author": "Song WC",
"doi-asserted-by": "publisher",
"journal-title": "J Clin Invest",
"key": "ref17",
"unstructured": "Song WC, FitzGerald GA. COVID-19, microangiopathy, hemostatic activation, and complement. J Clin Invest. 2020, 130:3950-3. 10.1172/JCI140183",
"volume": "130",
"year": "2020"
},
{
"DOI": "10.1016/j.kint.2020.05.025",
"article-title": "Thrombotic microangiopathy in a patient with COVID-19",
"author": "Jhaveri KD",
"doi-asserted-by": "publisher",
"journal-title": "Kidney Int",
"key": "ref18",
"unstructured": "Jhaveri KD, Meir LR, Flores Chang BS, et al.. Thrombotic microangiopathy in a patient with COVID-19. Kidney Int. 2020, 98:509-12. 10.1016/j.kint.2020.05.025",
"volume": "98",
"year": "2020"
},
{
"DOI": "10.1681/ASN.2020050744",
"article-title": "Postmortem kidney pathology findings in patients with COVID-19",
"author": "Santoriello D",
"doi-asserted-by": "publisher",
"journal-title": "J Am Soc Nephrol",
"key": "ref19",
"unstructured": "Santoriello D, Khairallah P, Bomback AS, et al.. Postmortem kidney pathology findings in patients with COVID-19. J Am Soc Nephrol. 2020, 31:2158-67. 10.1681/ASN.2020050744",
"volume": "31",
"year": "2020"
},
{
"DOI": "10.1016/j.eclinm.2020.100434",
"article-title": "Megakaryocytes and platelet-fibrin thrombi characterize multi-organ thrombosis at autopsy in COVID-19: a case series",
"author": "Rapkiewicz AV",
"doi-asserted-by": "publisher",
"journal-title": "EClinicalMedicine",
"key": "ref20",
"unstructured": "Rapkiewicz AV, Mai X, Carsons SE, et al.. Megakaryocytes and platelet-fibrin thrombi characterize multi-organ thrombosis at autopsy in COVID-19: a case series. EClinicalMedicine. 2020, 24:100434. 10.1016/j.eclinm.2020.100434",
"volume": "24",
"year": "2020"
},
{
"key": "ref21",
"unstructured": "COVID-19 Treatment Guidelines Panel. Coronavirus Disease 2019 (COVID-19) Treatment Guidelines. National Institutes of Health. (2023). Accessed. July 23, 2023: https://www.covid19treatmentguidelines.nih.gov/."
},
{
"DOI": "10.1182/bloodadvances.2022007561",
"article-title": "American Society of Hematology living guidelines on the use of anticoagulation for thromboprophylaxis in patients with COVID-19: January 2022 update on the use of therapeutic-intensity anticoagulation in acutely ill patients",
"author": "Cuker A",
"doi-asserted-by": "publisher",
"journal-title": "Blood Adv",
"key": "ref22",
"unstructured": "Cuker A, Tseng EK, Nieuwlaat R, et al.. American Society of Hematology living guidelines on the use of anticoagulation for thromboprophylaxis in patients with COVID-19: January 2022 update on the use of therapeutic-intensity anticoagulation in acutely ill patients. Blood Adv. 2022, 6:4915-23. 10.1182/bloodadvances.2022007561",
"volume": "6",
"year": "2022"
}
],
"reference-count": 22,
"references-count": 22,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.cureus.com/articles/165816-effects-of-different-anticoagulation-doses-on-moderate-to-severe-covid-19-pneumonia-with-hypoxemia"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Aerospace Engineering"
],
"subtitle": [],
"title": "Effects of Different Anticoagulation Doses on Moderate-to-Severe COVID-19 Pneumonia With Hypoxemia",
"type": "journal-article"
}