Prepandemic Physical Activity and Risk of COVID-19 Diagnosis and Hospitalization in Older Adults
et al., JAMA Network Open, doi:10.1001/jamanetworkopen.2023.55808, Feb 2024
Exercise for COVID-19
9th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 68 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Prospective study of 61,557 adults aged 45+ years showing reduced risk of COVID-19 diagnosis and hospitalization for those meeting physical activity guidelines of ≥7.5 MET-hours/week before the pandemic compared to inactive individuals.
Standard of Care (SOC) for COVID-19 in the study country,
the USA, is very poor with very low average efficacy for approved treatments1.
Only expensive, high-profit treatments were approved for early treatment. Low-cost treatments were excluded, reducing the probability of early treatment due to access and cost barriers, and eliminating complementary and synergistic benefits seen with many low-cost treatments.
|
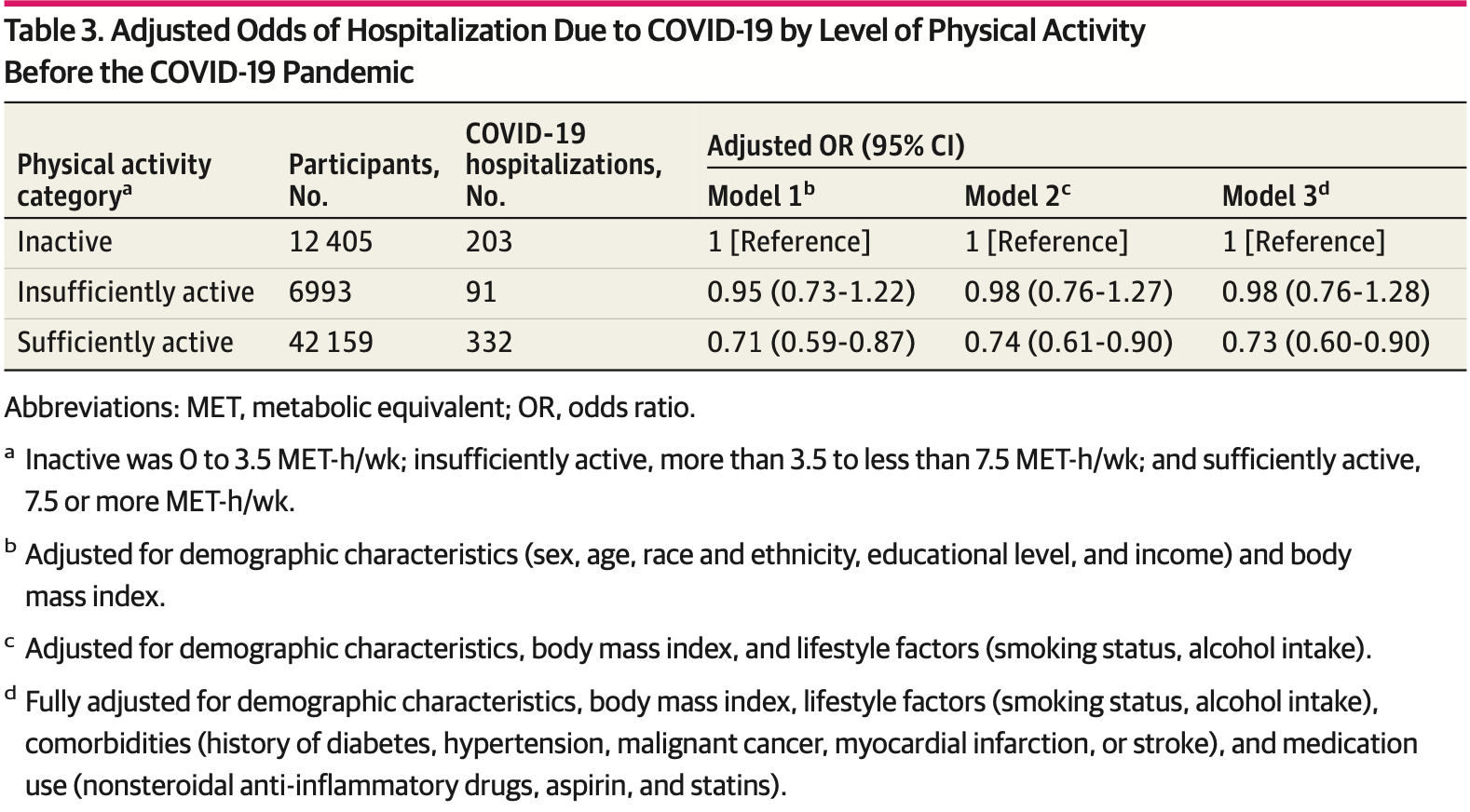
risk of hospitalization, 26.7% lower, RR 0.73, p = 0.002, high activity levels 332 of 42,159 (0.8%), low activity levels 203 of 12,405 (1.6%), adjusted per study, odds ratio converted to relative risk, sufficiently active vs. inactive, multivariable, model 3.
|
|
risk of case, 9.1% lower, RR 0.91, p = 0.004, high activity levels 3,898 of 42,159 (9.2%), low activity levels 1,293 of 12,405 (10.4%), NNT 85, adjusted per study, odds ratio converted to relative risk, sufficiently active vs. inactive, multivariable, model 3.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Muñoz-Vergara et al., 13 Feb 2024, prospective, USA, peer-reviewed, 7 authors.
Prepandemic Physical Activity and Risk of COVID-19 Diagnosis and Hospitalization in Older Adults
doi:10.1001/jamanetworkopen.2023.55808
IMPORTANCE Higher prepandemic physical activity (PA) levels have been associated with lower risk and severity of COVID-19. OBJECTIVE To investigate the association between self-reported prepandemic PA levels and the risk and severity of COVID-19 in older US adults. DESIGN, SETTING, AND PARTICIPANTS This cohort study combined cohorts from 3 ongoing prospective randomized clinical trials of US adults aged 45 years or older who provided prepandemic self-reports of baseline leisure-time PA and risk factors for COVID-19 outcomes using the most recent questionnaire completed as of December 31, 2019, as the baseline PA assessment. In multiple surveys from May 2020 through May 2022, participants indicated whether they had at least 1 positive COVID-19 test result or were diagnosed with or hospitalized for COVID-19. EXPOSURE Prepandemic PA, categorized into 3 groups by metabolic equivalent hours per week: inactive (0-3.5), insufficiently active (>3.5 to <7.5), and sufficiently active (Ն7.5).
MAIN OUTCOME AND MEASURES Primary outcomes were risk of COVID-19 and hospitalization for COVID-19. Multivariable logistic regression was used to estimate odd ratios (ORs) and 95% CIs for the association of COVID-19 diagnosis and/or hospitalization with each of the 2 upper PA categories vs the lowest PA category.
RESULTS The pooled cohort included 61 557 participants (mean [SD] age, 75.7 [6.4] years; 70.7% female), 20.2% of whom were inactive; 11.4%, insufficiently active; and 68.5%, sufficiently active. A total of 5890 confirmed incident cases of COVID-19 were reported through May 2022, including 626 hospitalizations. After controlling for demographics, body mass index, lifestyle factors, comorbidities, and medications used, compared with inactive individuals, those insufficiently active had no significant reduction in infection (OR, 0.96; 95% CI, 0.86-1.06) or hospitalization (OR, 0.98; 95% CI, 0.76-1.28), whereas those sufficiently active had a significant reduction in infection (OR, 0.90; 95% CI, 0.84-0.97) and hospitalization (OR, 0.73; 95% CI, 0.60-0.90). In subgroup analyses, the association between PA and SARS-CoV-2 infection differed by sex, with only sufficiently active women having decreased odds (OR, 0.87; 95% CI, 0.79-0.95; P = .04 for interaction).
CONCLUSIONS AND RELEVANCE In this cohort study of adults aged 45 years or older, those who adhered to PA guidelines before the pandemic had lower odds of developing or being hospitalized for COVID-19. Thus, higher prepandemic PA levels may be associated with reduced odds of SARS-CoV-2 infection and hospitalization for COVID-19.
Author Contributions: Drs Kim and Sesso had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Drs Muñoz-Vergara and Wayne contributed equally to this work. Concept and design: Wayne, Manson, Sesso.
Acquisition, analysis, or interpretation of data: All authors. Drafting of the manuscript: Muñoz-Vergara, Wayne, Sesso.
Critical review of the manuscript for important intellectual content: All authors. Statistical analysis: Muñoz-Vergara, Kim. Obtained funding: Wayne, Lee, Sesso. Administrative, technical, or material support: Muñoz-Vergara, Lee, Manson, Sesso. Supervision: Wayne, Manson, Sesso. Role of the Funder/Sponsor: The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Conflict of Interest Data Sharing Statement: See Supplement 2. Additional Contributions: We thank the COSMOS, VITAL, and WHS study participants and research staff for their tremendous dedication and commitment.
References
Ahmadi, Huang, Inan-Eroglu, Hamer, Stamatakis, Lifestyle risk factors and infectious disease mortality, including COVID-19, among middle aged and older adults: evidence from a community-based cohort study in the United Kingdom, Brain Behav Immun, doi:10.1016/j.bbi.2021.04.022
Bergman, Ballin, Nordström, Nordström, Risk factors for COVID-19 diagnosis, hospitalization, and subsequent all-cause mortality in Sweden: a nationwide study, Eur J Epidemiol, doi:10.1007/s10654-021-00732-w
Bird, Karageorghis, Hamer, Relationships among behavioural regulations, physical activity, and mental health pre-and during COVID-19 UK lockdown, Psychol Sport Exerc, doi:10.1016/j.psychsport.2021.101945
Blanchflower, Bryson, COVID and mental health in America, PLoS One, doi:10.1371/journal.pone.0269855
Brandenburg, Lesser, Thomson, Giles, Does higher self-reported cardiorespiratory fitness reduce the odds of hospitalization from COVID-19?, J Phys Act Health, doi:10.1123/jpah.2020-0817
Braveman, Gottlieb, The social determinants of health: it's time to consider the causes of the causes, Public Health Rep, doi:10.1177/00333549141291S206
Bull, Ss, Biddle, World Health Organization 2020 guidelines on physical activity and sedentary behaviour, Br J Sports Med, doi:10.1136/bjsports-2020-102955
Bwire, Coronavirus: why men are more vulnerable to COVID-19 than women? SN, Compr Clin Med, doi:10.1007/s42399-020-00341-w
Chastin, Abaraogu, Bourgois, Effects of regular physical activity on the immune system, vaccination and risk of community-acquired infectious disease in the general population: systematic review and meta-analysis, Sports Med, doi:10.1007/s40279-021-01466-1
Cho, Lee, Sy, Physical activity and the risk of COVID-19 infection and mortality: a nationwide population-based case-control study, J Clin Med, doi:10.3390/jcm10071539
Curb, Mctiernan, Heckbert, Outcomes ascertainment and adjudication methods in the Women's Health Initiative, Ann Epidemiol, doi:10.1016/S1047-2797(03)00048-6
Cuschieri, The STROBE guidelines, Saudi J Anaesth, doi:10.4103/sja.SJA_543_18
De Souza, Motta-Santos, Soares, Association of physical activity levels and the prevalence of COVID-19-associated hospitalization, J Sci Med Sport, doi:10.1016/j.jsams.2021.05.011
Drummond, Campos, Drummond, Acute and chronic effects of physical exercise on IgA and IgG levels and susceptibility to upper respiratory tract infections: a systematic review and meta-analysis, Pflugers Arch, doi:10.1007/s00424-022-02760-1
Ekblom-Bak, Väisänen, Ekblom, Cardiorespiratory fitness and lifestyle on severe COVID-19 risk in 279 455 adults: a case control study, Int J Behav Nutr Phys Act, doi:10.1186/s12966-021-01198-5
Epel, The geroscience agenda: toxic stress, hormetic stress, and the rate of aging, Ageing Res Rev, doi:10.1016/j.arr.2020.101167
Ezzatvar, Ramírez-Vélez, Izquierdo, Garcia-Hermoso, Physical activity and risk of infection, severity and mortality of COVID-19: a systematic review and non-linear dose-response meta-analysis of data from 1 853 610 adults, Br J Sports Med, doi:10.1136/bjsports-2022-105733
Francescomarino, Sciartilli, Valerio, Baldassarre, Gallina, The effect of physical exercise on endothelial function, Sports Med, doi:10.2165/11317750-000000000-00000
Gay, Salinas, Buchner, Meeting physical activity guidelines is associated with lower allostatic load and inflammation in Mexican Americans, J Immigr Minor Health, doi:10.1007/s10903-013-9950-1
Gleeson, Bishop, Stensel, Lindley, Mastana et al., The anti-inflammatory effects of exercise: mechanisms and implications for the prevention and treatment of disease, Nat Rev Immunol, doi:10.1038/nri3041
Groeneveld, Ballering, Van Boven, Akkermans, Hartman et al., Sex differences in incidence of respiratory symptoms and management by general practitioners, Fam Pract, doi:10.1093/fampra/cmaa040
Hamer, Kivimäki, Gale, Batty, Lifestyle risk factors, inflammatory mechanisms, and COVID-19 hospitalization: a community-based cohort study of 387 109 adults in UK, Brain Behav Immun, doi:10.1016/j.bbi.2020.05.059
Hasson, Sallis, Coleman, Kaushal, Nocera et al., COVID-19: implications for physical activity, health disparities, and health equity, Am J Lifestyle Med, doi:10.1177/15598276211029222
Havers, Pham, Taylor, COVID-19-associated hospitalizations among vaccinated and unvaccinated adults 18 years or older in 13 US states, January 2021 to April 2022, JAMA Intern Med, doi:https://jama.jamanetwork.com/article.aspx?doi=10.1001/jamainternmed.2022.4299&utm_campaign=articlePDF%26utm_medium=articlePDFlink%26utm_source=articlePDF%26utm_content=jamanetworkopen.2023.55808
Havervall, Marking, Svensson, Anti-spike mucosal IgA protection against SARS-CoV-2 Omicron infection, N Engl J Med, doi:10.1056/NEJMc2209651
Hoshi, Liu, Luttmann-Gibson, Association of physical activity with bioactive lipids and cardiovascular events, Circ Res, doi:10.1161/CIRCRESAHA.122.320952
Jurado-Fasoli, Di, Sanchez-Delgado, Acute and long-term exercise differently modulate plasma levels of oxylipins, endocannabinoids, and their analogues in young sedentary adults: a sub-study and secondary analyses from the ACTIBATE randomized controlled-trial, EBioMedicine, doi:10.1016/j.ebiom.2022.104313
Klöting, Ristow, Blüher, Effects of exercise on ACE2, Obesity, doi:10.1002/oby.23041
Kunutsor, Seidu, Laukkanen, Physical activity reduces the risk of pneumonia: systematic review and meta-analysis of 10 prospective studies involving 1 044 492 participants, Geroscience, doi:10.1007/s11357-021-00491-2
Lee, Cook, Manson, Buring, Randomised beta-carotene supplementation and incidence of cancer and cardiovascular disease in women: is the association modified by baseline plasma level?, Br J Cancer, doi:10.1038/sj.bjc.6600147
Lee, Lee, Moon, Physical activity and the risk of SARS-CoV-2 infection, severe COVID-19 illness and COVID-19 related mortality in South Korea: a nationwide cohort study, Br J Sports Med, doi:10.1136/bjsports-2021-104203
Li, Huang, Zou, Epidemiology of COVID-19: a systematic review and meta-analysis of clinical characteristics, risk factors, and outcomes, J Med Virol, doi:10.1002/jmv.26424
Mandolesi, Polverino, Montuori, Effects of physical exercise on cognitive functioning and wellbeing: biological and psychological benefits, Front Psychol, doi:10.3389/fpsyg.2018.00509
Manson, Bassuk, Lee, The Vitamin D and Omega-3 Trial (VITAL): rationale and design of a large randomized controlled trial of vitamin D and marine omega-3 fatty acid supplements for the primary prevention of cancer and cardiovascular disease, Contemp Clin Trials, doi:10.1016/j.cct.2011.09.009
Manson, Cook, Lee, Vitamin D supplements and prevention of cancer and cardiovascular disease, N Engl J Med, doi:10.1056/NEJMoa1809944
Mansournia, Etminan, Danaei, Kaufman, Collins, Handling time varying confounding in observational research, BMJ, doi:10.1136/bmj.j4587
Muñoz-Vergara, Burton, Bain, Understanding the dynamics of inflammatory mediators in response to mind-body movement therapies (MBMTs): a systematic review and meta-analysis of studies in healthy subjects, Brain Behav Immun Integr, doi:10.1016/j.bbii.2023.100006
Nieman, Wentz, The compelling link between physical activity and the body's defense system, J Sport Health Sci, doi:10.1016/j.jshs.2018.09.009
Petersen, Pedersen, The anti-inflammatory effect of exercise, J Appl Physiol, doi:10.1152/japplphysiol.00164.2004
Phillips, Fahimi, Immune and neuroprotective effects of physical activity on the brain in depression, Front Neurosci, doi:10.3389/fnins.2018.00498
Rexrode, Lee, Cook, Hennekens, Buring, Baseline characteristics of participants in the Women's Health Study, J Womens Health Gend Based Med, doi:10.1089/152460900318911
Ridker, Buring, Cook, Rifai, C-reactive protein, the metabolic syndrome, and risk of incident cardiovascular events: an 8-year follow-up of 14 719 initially healthy American women, Circulation, doi:10.1161/01.CIR.0000055014.62083.05
Rist, Sesso, Johnson, Design and baseline characteristics of participants in the Cocoa Supplement and Multivitamin Outcomes Study (COSMOS), Contemp Clin Trials, doi:10.1016/j.cct.2022.106728
Rossi, Cena, Binala, Alessi, Scotti et al., Evaluation of the risk of SARS-CoV-2 infection and hospitalization in vaccinated and previously infected subjects based on real world data, Sci Rep, doi:10.1038/s41598-023-28129-7
Rowlands, Dempsey, Gillies, Association between accelerometer-assessed physical activity and severity of COVID-19 in UK Biobank, Mayo Clin Proc Innov Qual Outcomes, doi:10.1016/j.mayocpiqo.2021.08.011
Saint-Maurice, Graubard, Troiano, Estimated number of deaths prevented through increased physical activity among US adults, JAMA Intern Med, doi:https://jama.jamanetwork.com/article.aspx?doi=10.1001/jamainternmed.2021.7755&utm_campaign=articlePDF%26utm_medium=articlePDFlink%26utm_source=articlePDF%26utm_content=jamanetworkopen.2023.55808
Sallis, Young, Tartof, Physical inactivity is associated with a higher risk for severe COVID-19 outcomes: a study in 48 440 adult patients, Br J Sports Med, doi:10.1136/bjsports-2021-104080
Sesso, Manson, Aragaki, Effect of cocoa flavanol supplementation for the prevention of cardiovascular disease events: the Cocoa Supplement and Multivitamin Outcomes Study (COSMOS) randomized clinical trial, Am J Clin Nutr, doi:10.1093/ajcn/nqac055
Wang, Li, Yue, Adherence to healthy lifestyle prior to infection and risk of post-COVID-19 condition, JAMA Intern Med, doi:https://jama.jamanetwork.com/article.aspx?doi=10.1001/jamainternmed.2022.6555&utm_campaign=articlePDF%26utm_medium=articlePDFlink%26utm_source=articlePDF%26utm_content=jamanetworkopen.2023.55808
Wilke, Mohr, Tenforde, A pandemic within the pandemic? physical activity levels substantially decreased in countries affected by COVID-19, Int J Environ Res Public Health, doi:10.3390/ijerph18052235
Xu, Ilyas, Weng, Endothelial dysfunction in COVID-19: an overview of evidence, biomarkers, mechanisms and potential therapies, Acta Pharmacol Sin, doi:10.1038/s41401-022-00998-0
Young, Sallis, Baecker, Associations of physical inactivity and COVID-19 outcomes among subgroups, Am J Prev Med, doi:10.1016/j.amepre.2022.10.007
Zhang, Li, Sun, Physical activity and COVID-19: an observational and Mendelian randomisation study, J Glob Health, doi:10.7189/jogh.10.020514
Zhao, Veeranki, Magnussen, Xi, Recommended physical activity and all cause and cause specific mortality in US adults: prospective cohort study, BMJ, doi:10.1136/bmj.m2031
DOI record:
{
"DOI": "10.1001/jamanetworkopen.2023.55808",
"ISSN": [
"2574-3805"
],
"URL": "http://dx.doi.org/10.1001/jamanetworkopen.2023.55808",
"abstract": "<jats:sec id=\"ab-zoi231639-4\"><jats:title>Importance</jats:title><jats:p>Higher prepandemic physical activity (PA) levels have been associated with lower risk and severity of COVID-19.</jats:p></jats:sec><jats:sec id=\"ab-zoi231639-5\"><jats:title>Objective</jats:title><jats:p>To investigate the association between self-reported prepandemic PA levels and the risk and severity of COVID-19 in older US adults.</jats:p></jats:sec><jats:sec id=\"ab-zoi231639-6\"><jats:title>Design, Setting, and Participants</jats:title><jats:p>This cohort study combined cohorts from 3 ongoing prospective randomized clinical trials of US adults aged 45 years or older who provided prepandemic self-reports of baseline leisure-time PA and risk factors for COVID-19 outcomes using the most recent questionnaire completed as of December 31, 2019, as the baseline PA assessment. In multiple surveys from May 2020 through May 2022, participants indicated whether they had at least 1 positive COVID-19 test result or were diagnosed with or hospitalized for COVID-19.</jats:p></jats:sec><jats:sec id=\"ab-zoi231639-7\"><jats:title>Exposure</jats:title><jats:p>Prepandemic PA, categorized into 3 groups by metabolic equivalent hours per week: inactive (0-3.5), insufficiently active (&amp;gt;3.5 to &amp;lt;7.5), and sufficiently active (≥7.5).</jats:p></jats:sec><jats:sec id=\"ab-zoi231639-8\"><jats:title>Main Outcome and Measures</jats:title><jats:p>Primary outcomes were risk of COVID-19 and hospitalization for COVID-19. Multivariable logistic regression was used to estimate odd ratios (ORs) and 95% CIs for the association of COVID-19 diagnosis and/or hospitalization with each of the 2 upper PA categories vs the lowest PA category.</jats:p></jats:sec><jats:sec id=\"ab-zoi231639-9\"><jats:title>Results</jats:title><jats:p>The pooled cohort included 61 557 participants (mean [SD] age, 75.7 [6.4] years; 70.7% female), 20.2% of whom were inactive; 11.4%, insufficiently active; and 68.5%, sufficiently active. A total of 5890 confirmed incident cases of COVID-19 were reported through May 2022, including 626 hospitalizations. After controlling for demographics, body mass index, lifestyle factors, comorbidities, and medications used, compared with inactive individuals, those insufficiently active had no significant reduction in infection (OR, 0.96; 95% CI, 0.86-1.06) or hospitalization (OR, 0.98; 95% CI, 0.76-1.28), whereas those sufficiently active had a significant reduction in infection (OR, 0.90; 95% CI, 0.84-0.97) and hospitalization (OR, 0.73; 95% CI, 0.60-0.90). In subgroup analyses, the association between PA and SARS-CoV-2 infection differed by sex, with only sufficiently active women having decreased odds (OR, 0.87; 95% CI, 0.79-0.95; <jats:italic>P</jats:italic> = .04 for interaction).</jats:p></jats:sec><jats:sec id=\"ab-zoi231639-10\"><jats:title>Conclusions and Relevance</jats:title><jats:p>In this cohort study of adults aged 45 years or older, those who adhered to PA guidelines before the pandemic had lower odds of developing or being hospitalized for COVID-19. Thus, higher prepandemic PA levels may be associated with reduced odds of SARS-CoV-2 infection and hospitalization for COVID-19.</jats:p></jats:sec>",
"author": [
{
"affiliation": [
{
"name": "Osher Center for Integrative Medicine, Brigham and Women’s Hospital, Harvard Medical School, Boston, Massachusetts"
},
{
"name": "Division of Preventive Medicine, Brigham and Women’s Hospital, Harvard Medical School, Boston, Massachusetts"
}
],
"family": "Muñoz-Vergara",
"given": "Dennis",
"sequence": "first"
},
{
"affiliation": [
{
"name": "Osher Center for Integrative Medicine, Brigham and Women’s Hospital, Harvard Medical School, Boston, Massachusetts"
},
{
"name": "Division of Preventive Medicine, Brigham and Women’s Hospital, Harvard Medical School, Boston, Massachusetts"
}
],
"family": "Wayne",
"given": "Peter M.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Division of Preventive Medicine, Brigham and Women’s Hospital, Harvard Medical School, Boston, Massachusetts"
}
],
"family": "Kim",
"given": "Eunjung",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Division of Preventive Medicine, Brigham and Women’s Hospital, Harvard Medical School, Boston, Massachusetts"
},
{
"name": "Department of Epidemiology, Harvard T.H. Chan School of Public Health, Boston, Massachusetts"
}
],
"family": "Lee",
"given": "I-Min",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Division of Preventive Medicine, Brigham and Women’s Hospital, Harvard Medical School, Boston, Massachusetts"
},
{
"name": "Department of Epidemiology, Harvard T.H. Chan School of Public Health, Boston, Massachusetts"
}
],
"family": "Buring",
"given": "Julie E.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Division of Preventive Medicine, Brigham and Women’s Hospital, Harvard Medical School, Boston, Massachusetts"
},
{
"name": "Department of Epidemiology, Harvard T.H. Chan School of Public Health, Boston, Massachusetts"
}
],
"family": "Manson",
"given": "JoAnn E.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Osher Center for Integrative Medicine, Brigham and Women’s Hospital, Harvard Medical School, Boston, Massachusetts"
},
{
"name": "Division of Preventive Medicine, Brigham and Women’s Hospital, Harvard Medical School, Boston, Massachusetts"
},
{
"name": "Department of Epidemiology, Harvard T.H. Chan School of Public Health, Boston, Massachusetts"
}
],
"family": "Sesso",
"given": "Howard D.",
"sequence": "additional"
}
],
"container-title": "JAMA Network Open",
"container-title-short": "JAMA Netw Open",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2024,
2,
13
]
],
"date-time": "2024-02-13T16:32:05Z",
"timestamp": 1707841925000
},
"deposited": {
"date-parts": [
[
2024,
2,
13
]
],
"date-time": "2024-02-13T16:32:09Z",
"timestamp": 1707841929000
},
"indexed": {
"date-parts": [
[
2024,
2,
14
]
],
"date-time": "2024-02-14T01:17:33Z",
"timestamp": 1707873453546
},
"is-referenced-by-count": 0,
"issue": "2",
"issued": {
"date-parts": [
[
2024,
2,
13
]
]
},
"journal-issue": {
"issue": "2",
"published-print": {
"date-parts": [
[
2024,
2,
5
]
]
}
},
"language": "en",
"link": [
{
"URL": "https://jamanetwork.com/journals/jamanetworkopen/articlepdf/2814993/muozvergara_2024_oi_231639_1707154576.18525.pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "10",
"original-title": [],
"page": "e2355808",
"prefix": "10.1001",
"published": {
"date-parts": [
[
2024,
2,
13
]
]
},
"published-online": {
"date-parts": [
[
2024,
2,
13
]
]
},
"publisher": "American Medical Association (AMA)",
"reference": [
{
"DOI": "10.1001/jamainternmed.2021.7755",
"article-title": "Estimated number of deaths prevented through increased physical activity among US adults.",
"author": "Saint-Maurice",
"doi-asserted-by": "publisher",
"first-page": "349",
"issue": "3",
"journal-title": "JAMA Intern Med",
"key": "zoi231639r1",
"volume": "182",
"year": "2022"
},
{
"DOI": "10.1136/bmj.m2031",
"article-title": "Recommended physical activity and all cause and cause specific mortality in US adults: prospective cohort study.",
"author": "Zhao",
"doi-asserted-by": "publisher",
"first-page": "m2031",
"journal-title": "BMJ",
"key": "zoi231639r2",
"volume": "370",
"year": "2020"
},
{
"DOI": "10.1161/CIRCRESAHA.122.320952",
"article-title": "Association of physical activity with bioactive lipids and cardiovascular events.",
"author": "Hoshi",
"doi-asserted-by": "publisher",
"first-page": "e84",
"issue": "4",
"journal-title": "Circ Res",
"key": "zoi231639r3",
"volume": "131",
"year": "2022"
},
{
"DOI": "10.1136/bjsports-2020-102955",
"article-title": "World Health Organization 2020 guidelines on physical activity and sedentary behaviour.",
"author": "Bull",
"doi-asserted-by": "publisher",
"first-page": "1451",
"issue": "24",
"journal-title": "Br J Sports Med",
"key": "zoi231639r4",
"volume": "54",
"year": "2020"
},
{
"DOI": "10.1016/j.arr.2020.101167",
"article-title": "The geroscience agenda: toxic stress, hormetic stress, and the rate of aging.",
"author": "Epel",
"doi-asserted-by": "publisher",
"journal-title": "Ageing Res Rev",
"key": "zoi231639r7",
"volume": "63",
"year": "2020"
},
{
"DOI": "10.1016/j.jshs.2018.09.009",
"article-title": "The compelling link between physical activity and the body’s defense system.",
"author": "Nieman",
"doi-asserted-by": "publisher",
"first-page": "201",
"issue": "3",
"journal-title": "J Sport Health Sci",
"key": "zoi231639r8",
"volume": "8",
"year": "2019"
},
{
"DOI": "10.1007/s10903-013-9950-1",
"article-title": "Meeting physical activity guidelines is associated with lower allostatic load and inflammation in Mexican Americans.",
"author": "Gay",
"doi-asserted-by": "publisher",
"first-page": "574",
"issue": "2",
"journal-title": "J Immigr Minor Health",
"key": "zoi231639r9",
"volume": "17",
"year": "2015"
},
{
"DOI": "10.1007/s40279-021-01466-1",
"article-title": "Effects of regular physical activity on the immune system, vaccination and risk of community-acquired infectious disease in the general population: systematic review and meta-analysis.",
"author": "Chastin",
"doi-asserted-by": "publisher",
"first-page": "1673",
"issue": "8",
"journal-title": "Sports Med",
"key": "zoi231639r10",
"volume": "51",
"year": "2021"
},
{
"DOI": "10.1038/nri3041",
"article-title": "The anti-inflammatory effects of exercise: mechanisms and implications for the prevention and treatment of disease.",
"author": "Gleeson",
"doi-asserted-by": "publisher",
"first-page": "607",
"issue": "9",
"journal-title": "Nat Rev Immunol",
"key": "zoi231639r11",
"volume": "11",
"year": "2011"
},
{
"DOI": "10.1136/bjsports-2022-105733",
"article-title": "Physical activity and risk of infection, severity and mortality of COVID-19: a systematic review and non-linear dose-response meta-analysis of data from 1 853 610 adults.",
"author": "Ezzatvar",
"doi-asserted-by": "publisher",
"journal-title": "Br J Sports Med",
"key": "zoi231639r13",
"year": "2022"
},
{
"DOI": "10.1136/bjsports-2021-104080",
"article-title": "Physical inactivity is associated with a higher risk for severe COVID-19 outcomes: a study in 48 440 adult patients.",
"author": "Sallis",
"doi-asserted-by": "publisher",
"first-page": "1099",
"issue": "19",
"journal-title": "Br J Sports Med",
"key": "zoi231639r15",
"volume": "55",
"year": "2021"
},
{
"DOI": "10.1001/jamainternmed.2022.6555",
"article-title": "Adherence to healthy lifestyle prior to infection and risk of post-COVID-19 condition.",
"author": "Wang",
"doi-asserted-by": "publisher",
"first-page": "232",
"issue": "3",
"journal-title": "JAMA Intern Med",
"key": "zoi231639r16",
"volume": "183",
"year": "2023"
},
{
"DOI": "10.7189/jogh.10.020514",
"article-title": "Physical activity and COVID-19: an observational and Mendelian randomisation study.",
"author": "Zhang",
"doi-asserted-by": "publisher",
"issue": "2",
"journal-title": "J Glob Health",
"key": "zoi231639r17",
"volume": "10",
"year": "2020"
},
{
"DOI": "10.1016/j.jsams.2021.05.011",
"article-title": "Association of physical activity levels and the prevalence of COVID-19-associated hospitalization.",
"author": "de Souza",
"doi-asserted-by": "publisher",
"first-page": "913",
"issue": "9",
"journal-title": "J Sci Med Sport",
"key": "zoi231639r18",
"volume": "24",
"year": "2021"
},
{
"DOI": "10.1016/j.cct.2022.106728",
"article-title": "Design and baseline characteristics of participants in the Cocoa Supplement and Multivitamin Outcomes Study (COSMOS).",
"author": "Rist",
"doi-asserted-by": "publisher",
"journal-title": "Contemp Clin Trials",
"key": "zoi231639r19",
"volume": "116",
"year": "2022"
},
{
"DOI": "10.1093/ajcn/nqac055",
"article-title": "Effect of cocoa flavanol supplementation for the prevention of cardiovascular disease events: the Cocoa Supplement and Multivitamin Outcomes Study (COSMOS) randomized clinical trial.",
"author": "Sesso",
"doi-asserted-by": "publisher",
"first-page": "1490",
"issue": "6",
"journal-title": "Am J Clin Nutr",
"key": "zoi231639r20",
"volume": "115",
"year": "2022"
},
{
"DOI": "10.1056/NEJMoa1809944",
"article-title": "Vitamin D supplements and prevention of cancer and cardiovascular disease.",
"author": "Manson",
"doi-asserted-by": "publisher",
"first-page": "33",
"issue": "1",
"journal-title": "N Engl J Med",
"key": "zoi231639r21",
"volume": "380",
"year": "2019"
},
{
"DOI": "10.1089/152460900318911",
"article-title": "Baseline characteristics of participants in the Women’s Health Study.",
"author": "Rexrode",
"doi-asserted-by": "publisher",
"first-page": "19",
"issue": "1",
"journal-title": "J Womens Health Gend Based Med",
"key": "zoi231639r22",
"volume": "9",
"year": "2000"
},
{
"DOI": "10.1038/sj.bjc.6600147",
"article-title": "Randomised beta-carotene supplementation and incidence of cancer and cardiovascular disease in women: is the association modified by baseline plasma level?",
"author": "Lee",
"doi-asserted-by": "publisher",
"first-page": "698",
"issue": "5",
"journal-title": "Br J Cancer",
"key": "zoi231639r23",
"volume": "86",
"year": "2002"
},
{
"DOI": "10.1161/01.CIR.0000055014.62083.05",
"article-title": "C-reactive protein, the metabolic syndrome, and risk of incident cardiovascular events: an 8-year follow-up of 14 719 initially healthy American women.",
"author": "Ridker",
"doi-asserted-by": "publisher",
"first-page": "391",
"issue": "3",
"journal-title": "Circulation",
"key": "zoi231639r24",
"volume": "107",
"year": "2003"
},
{
"DOI": "10.4103/sja.SJA_543_18",
"article-title": "The STROBE guidelines.",
"author": "Cuschieri",
"doi-asserted-by": "publisher",
"first-page": "S31",
"journal-title": "Saudi J Anaesth",
"key": "zoi231639r25",
"volume": "13",
"year": "2019"
},
{
"DOI": "10.1016/S1047-2797(03)00048-6",
"article-title": "Outcomes ascertainment and adjudication methods in the Women’s Health Initiative.",
"author": "Curb",
"doi-asserted-by": "publisher",
"first-page": "S122",
"issue": "9",
"journal-title": "Ann Epidemiol",
"key": "zoi231639r26",
"volume": "13",
"year": "2003"
},
{
"DOI": "10.1177/00333549141291S206",
"article-title": "The social determinants of health: it’s time to consider the causes of the causes.",
"author": "Braveman",
"doi-asserted-by": "publisher",
"first-page": "19",
"issue": "Suppl 2",
"journal-title": "Public Health Rep",
"key": "zoi231639r27",
"volume": "129",
"year": "2014"
},
{
"DOI": "10.1007/s11357-021-00491-2",
"article-title": "Physical activity reduces the risk of pneumonia: systematic review and meta-analysis of 10 prospective studies involving 1?044?492 participants.",
"author": "Kunutsor",
"doi-asserted-by": "publisher",
"first-page": "519",
"issue": "1",
"journal-title": "Geroscience",
"key": "zoi231639r28",
"volume": "44",
"year": "2022"
},
{
"DOI": "10.1016/j.amepre.2022.10.007",
"article-title": "Associations of physical inactivity and COVID-19 outcomes among subgroups.",
"author": "Young",
"doi-asserted-by": "publisher",
"first-page": "492",
"issue": "4",
"journal-title": "Am J Prev Med",
"key": "zoi231639r29",
"volume": "64",
"year": "2023"
},
{
"DOI": "10.3390/jcm10071539",
"article-title": "Physical activity and the risk of COVID-19 infection and mortality: a nationwide population-based case-control study.",
"author": "Cho",
"doi-asserted-by": "publisher",
"first-page": "1539",
"issue": "7",
"journal-title": "J Clin Med",
"key": "zoi231639r30",
"volume": "10",
"year": "2021"
},
{
"DOI": "10.1016/j.bbi.2021.04.022",
"article-title": "Lifestyle risk factors and infectious disease mortality, including COVID-19, among middle aged and older adults: evidence from a community-based cohort study in the United Kingdom.",
"author": "Ahmadi",
"doi-asserted-by": "publisher",
"first-page": "18",
"journal-title": "Brain Behav Immun",
"key": "zoi231639r31",
"volume": "96",
"year": "2021"
},
{
"DOI": "10.1016/j.mayocpiqo.2021.08.011",
"article-title": "Association between accelerometer-assessed physical activity and severity of COVID-19 in UK Biobank.",
"author": "Rowlands",
"doi-asserted-by": "publisher",
"first-page": "997",
"issue": "6",
"journal-title": "Mayo Clin Proc Innov Qual Outcomes",
"key": "zoi231639r32",
"volume": "5",
"year": "2021"
},
{
"DOI": "10.1136/bjsports-2021-104203",
"article-title": "Physical activity and the risk of SARS-CoV-2 infection, severe COVID-19 illness and COVID-19 related mortality in South Korea: a nationwide cohort study.",
"author": "Lee",
"doi-asserted-by": "publisher",
"first-page": "901",
"issue": "16",
"journal-title": "Br J Sports Med",
"key": "zoi231639r33",
"volume": "56",
"year": "2022"
},
{
"DOI": "10.1016/j.bbi.2020.05.059",
"article-title": "Lifestyle risk factors, inflammatory mechanisms, and COVID-19 hospitalization: a community-based cohort study of 387?109 adults in UK.",
"author": "Hamer",
"doi-asserted-by": "publisher",
"first-page": "184",
"journal-title": "Brain Behav Immun",
"key": "zoi231639r34",
"volume": "87",
"year": "2020"
},
{
"DOI": "10.1123/jpah.2020-0817",
"article-title": "Does higher self-reported cardiorespiratory fitness reduce the odds of hospitalization from COVID-19?",
"author": "Brandenburg",
"doi-asserted-by": "publisher",
"first-page": "782",
"issue": "7",
"journal-title": "J Phys Act Health",
"key": "zoi231639r35",
"volume": "18",
"year": "2021"
},
{
"DOI": "10.1093/fampra/cmaa040",
"article-title": "Sex differences in incidence of respiratory symptoms and management by general practitioners.",
"author": "Groeneveld",
"doi-asserted-by": "publisher",
"first-page": "631",
"issue": "5",
"journal-title": "Fam Pract",
"key": "zoi231639r36",
"volume": "37",
"year": "2020"
},
{
"DOI": "10.1007/s42399-020-00341-w",
"article-title": "Coronavirus: why men are more vulnerable to COVID-19 than women?",
"author": "Bwire",
"doi-asserted-by": "publisher",
"first-page": "874",
"issue": "7",
"journal-title": "SN Compr Clin Med",
"key": "zoi231639r37",
"volume": "2",
"year": "2020"
},
{
"DOI": "10.1186/s12966-021-01198-5",
"article-title": "Cardiorespiratory fitness and lifestyle on severe COVID-19 risk in 279?455 adults: a case control study.",
"author": "Ekblom-Bak",
"doi-asserted-by": "publisher",
"first-page": "135",
"issue": "1",
"journal-title": "Int J Behav Nutr Phys Act",
"key": "zoi231639r38",
"volume": "18",
"year": "2021"
},
{
"DOI": "10.1007/s10654-021-00732-w",
"article-title": "Risk factors for COVID-19 diagnosis, hospitalization, and subsequent all-cause mortality in Sweden: a nationwide study.",
"author": "Bergman",
"doi-asserted-by": "publisher",
"first-page": "287",
"issue": "3",
"journal-title": "Eur J Epidemiol",
"key": "zoi231639r39",
"volume": "36",
"year": "2021"
},
{
"DOI": "10.1002/jmv.v93.3",
"article-title": "Epidemiology of COVID-19: a systematic review and meta-analysis of clinical characteristics, risk factors, and outcomes.",
"author": "Li",
"doi-asserted-by": "publisher",
"first-page": "1449",
"issue": "3",
"journal-title": "J Med Virol",
"key": "zoi231639r40",
"volume": "93",
"year": "2021"
},
{
"DOI": "10.1016/j.psychsport.2021.101945",
"article-title": "Relationships among behavioural regulations, physical activity, and mental health pre- and during COVID-19 UK lockdown.",
"author": "Bird",
"doi-asserted-by": "publisher",
"journal-title": "Psychol Sport Exerc",
"key": "zoi231639r41",
"volume": "55",
"year": "2021"
},
{
"DOI": "10.1001/jamainternmed.2022.4299",
"article-title": "COVID-19-associated hospitalizations among vaccinated and unvaccinated adults 18 years or older in 13 US states, January 2021 to April 2022.",
"author": "Havers",
"doi-asserted-by": "publisher",
"first-page": "1071",
"issue": "10",
"journal-title": "JAMA Intern Med",
"key": "zoi231639r42",
"volume": "182",
"year": "2022"
},
{
"DOI": "10.1038/s41598-023-28129-7",
"article-title": "Evaluation of the risk of SARS-CoV-2 infection and hospitalization in vaccinated and previously infected subjects based on real world data.",
"author": "Rossi",
"doi-asserted-by": "publisher",
"first-page": "2018",
"issue": "1",
"journal-title": "Sci Rep",
"key": "zoi231639r43",
"volume": "13",
"year": "2023"
},
{
"DOI": "10.1038/s41401-022-00998-0",
"article-title": "Endothelial dysfunction in COVID-19: an overview of evidence, biomarkers, mechanisms and potential therapies.",
"author": "Xu",
"doi-asserted-by": "publisher",
"first-page": "695",
"issue": "4",
"journal-title": "Acta Pharmacol Sin",
"key": "zoi231639r44",
"volume": "44",
"year": "2023"
},
{
"DOI": "10.2165/11317750-000000000-00000",
"article-title": "The effect of physical exercise on endothelial function.",
"author": "Di Francescomarino",
"doi-asserted-by": "publisher",
"first-page": "797",
"issue": "10",
"journal-title": "Sports Med",
"key": "zoi231639r45",
"volume": "39",
"year": "2009"
},
{
"DOI": "10.3389/fnins.2018.00498",
"article-title": "Immune and neuroprotective effects of physical activity on the brain in depression.",
"author": "Phillips",
"doi-asserted-by": "publisher",
"first-page": "498",
"journal-title": "Front Neurosci",
"key": "zoi231639r46",
"volume": "12",
"year": "2018"
},
{
"DOI": "10.3389/fpsyg.2018.00509",
"article-title": "Effects of physical exercise on cognitive functioning and wellbeing: biological and psychological benefits.",
"author": "Mandolesi",
"doi-asserted-by": "publisher",
"first-page": "509",
"journal-title": "Front Psychol",
"key": "zoi231639r47",
"volume": "9",
"year": "2018"
},
{
"DOI": "10.1016/j.ebiom.2022.104313",
"article-title": "Acute and long-term exercise differently modulate plasma levels of oxylipins, endocannabinoids, and their analogues in young sedentary adults: a sub-study and secondary analyses from the ACTIBATE randomized controlled-trial.",
"author": "Jurado-Fasoli",
"doi-asserted-by": "publisher",
"journal-title": "EBioMedicine",
"key": "zoi231639r48",
"volume": "85",
"year": "2022"
},
{
"DOI": "10.1056/NEJMc2209651",
"article-title": "Anti-spike mucosal IgA protection against SARS-CoV-2 Omicron infection.",
"author": "Havervall",
"doi-asserted-by": "publisher",
"first-page": "1333",
"issue": "14",
"journal-title": "N Engl J Med",
"key": "zoi231639r49",
"volume": "387",
"year": "2022"
},
{
"DOI": "10.1007/s00424-022-02760-1",
"article-title": "Acute and chronic effects of physical exercise on IgA and IgG levels and susceptibility to upper respiratory tract infections: a systematic review and meta-analysis.",
"author": "Drummond",
"doi-asserted-by": "publisher",
"first-page": "1221",
"issue": "12",
"journal-title": "Pflugers Arch",
"key": "zoi231639r50",
"volume": "474",
"year": "2022"
},
{
"DOI": "10.1016/j.cct.2011.09.009",
"article-title": "The Vitamin D and Omega-3 Trial (VITAL): rationale and design of a large randomized controlled trial of vitamin D and marine omega-3 fatty acid supplements for the primary prevention of cancer and cardiovascular disease.",
"author": "Manson",
"doi-asserted-by": "publisher",
"first-page": "159",
"issue": "1",
"journal-title": "Contemp Clin Trials",
"key": "zoi231639r51",
"volume": "33",
"year": "2012"
},
{
"DOI": "10.1177/15598276211029222",
"article-title": "COVID-19: implications for physical activity, health disparities, and health equity.",
"author": "Hasson",
"doi-asserted-by": "publisher",
"first-page": "420",
"issue": "4",
"journal-title": "Am J Lifestyle Med",
"key": "zoi231639r52",
"volume": "16",
"year": "2021"
},
{
"DOI": "10.1371/journal.pone.0269855",
"article-title": "COVID and mental health in America.",
"author": "Blanchflower",
"doi-asserted-by": "publisher",
"issue": "7",
"journal-title": "PLoS One",
"key": "zoi231639r53",
"volume": "17",
"year": "2022"
},
{
"DOI": "10.3390/ijerph18052235",
"article-title": "A pandemic within the pandemic? physical activity levels substantially decreased in countries affected by COVID-19.",
"author": "Wilke",
"doi-asserted-by": "publisher",
"first-page": "2235",
"issue": "5",
"journal-title": "Int J Environ Res Public Health",
"key": "zoi231639r54",
"volume": "18",
"year": "2021"
},
{
"DOI": "10.1136/bmj.j4587",
"article-title": "Handling time varying confounding in observational research.",
"author": "Mansournia",
"doi-asserted-by": "publisher",
"first-page": "j4587",
"journal-title": "BMJ",
"key": "zoi231639r55",
"volume": "359",
"year": "2017"
},
{
"DOI": "10.1002/oby.v28.12",
"article-title": "Effects of exercise on ACE2.",
"author": "Klöting",
"doi-asserted-by": "publisher",
"first-page": "2266",
"issue": "12",
"journal-title": "Obesity (Silver Spring)",
"key": "zoi231639r56",
"volume": "28",
"year": "2020"
},
{
"key": "zoi231639r5",
"volume-title": "WHO Guidelines on Physical Activity and Sedentary Behaviour",
"year": "2020"
},
{
"key": "zoi231639r6",
"year": "2018"
},
{
"author": "Petersen",
"key": "zoi231639r12",
"year": "2005"
},
{
"author": "Muñoz-Vergara",
"first-page": "2",
"key": "zoi231639r14",
"year": "2023"
}
],
"reference-count": 56,
"references-count": 56,
"relation": {},
"resource": {
"primary": {
"URL": "https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2814993"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"General Medicine"
],
"subtitle": [],
"title": "Prepandemic Physical Activity and Risk of COVID-19 Diagnosis and Hospitalization in Older Adults",
"type": "journal-article",
"volume": "7"
}
