Associations of Physical Inactivity and COVID-19 Outcomes Among Subgroups
et al., American Journal of Preventive Medicine, doi:10.1016/j.amepre.2022.10.007, Dec 2022
Exercise for COVID-19
9th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 68 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
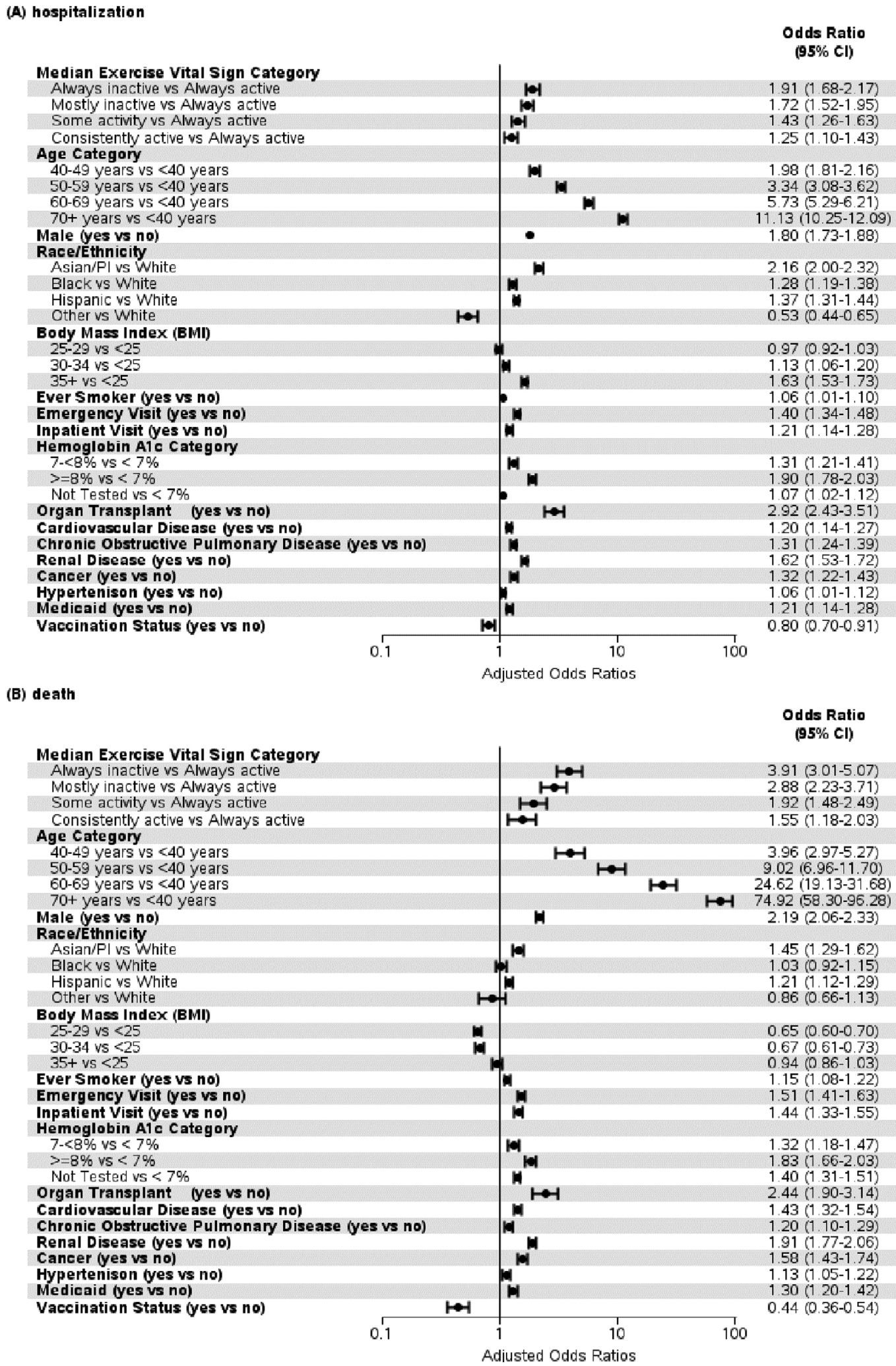
Retrospective 194,191 COVID-19 patients in the USA, showing lower risk of hospitalization and mortality with physical activity, with a dose response relationship.
Standard of Care (SOC) for COVID-19 in the study country,
the USA, is very poor with very low average efficacy for approved treatments1.
Only expensive, high-profit treatments were approved for early treatment. Low-cost treatments were excluded, reducing the probability of early treatment due to access and cost barriers, and eliminating complementary and synergistic benefits seen with many low-cost treatments.
|
risk of death, 74.4% lower, OR 0.26, p < 0.001, high activity levels 11,279, low activity levels 29,099, inverted to make OR<1 favor high activity levels, always active vs. always inactive, RR approximated with OR.
|
|
risk of death, 65.3% lower, OR 0.35, p < 0.001, high activity levels 11,279, low activity levels 83,452, inverted to make OR<1 favor high activity levels, always active vs. mostly inactive, RR approximated with OR.
|
|
risk of death, 47.9% lower, OR 0.52, p < 0.001, high activity levels 11,279, low activity levels 42,490, inverted to make OR<1 favor high activity levels, always active vs. some activity, RR approximated with OR.
|
|
risk of death, 35.5% lower, OR 0.65, p = 0.002, high activity levels 11,279, low activity levels 27,871, inverted to make OR<1 favor high activity levels, always active vs. consistently active, RR approximated with OR.
|
|
risk of hospitalization, 47.6% lower, OR 0.52, p < 0.001, high activity levels 11,279, low activity levels 29,099, inverted to make OR<1 favor high activity levels, always active vs. always inactive, RR approximated with OR.
|
|
risk of hospitalization, 41.9% lower, OR 0.58, p < 0.001, high activity levels 11,279, low activity levels 83,452, inverted to make OR<1 favor high activity levels, always active vs. mostly inactive, RR approximated with OR.
|
|
risk of hospitalization, 30.1% lower, OR 0.70, p < 0.001, high activity levels 11,279, low activity levels 42,490, inverted to make OR<1 favor high activity levels, always active vs. some activity, RR approximated with OR.
|
|
risk of hospitalization, 20.0% lower, OR 0.80, p < 0.001, high activity levels 11,279, low activity levels 27,871, inverted to make OR<1 favor high activity levels, always active vs. consistently active, RR approximated with OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Young et al., 14 Dec 2022, retrospective, USA, peer-reviewed, 7 authors, study period 1 January, 2020 - 31 May, 2021.
Contact: young@kp.org.
Associations of Physical Inactivity and COVID-19 Outcomes Among Subgroups
American Journal of Preventive Medicine, doi:10.1016/j.amepre.2022.10.007
Introduction: Physical activity before COVID-19 infection is associated with less severe outcomes. The study determined whether a dose-response association was observed and whether the associations were consistent across demographic subgroups and chronic conditions. Methods: A retrospective cohort study of Kaiser Permanente Southern California adult patients who had a positive COVID-19 diagnosis between January 1, 2020 and May 31, 2021 was created. The exposure was the median of at least 3 physical activity self-reports before diagnosis. Patients were categorized as follows: always inactive, all assessments at 10 minutes/week or less; mostly inactive, median of 0−60 minutes per week; some activity, median of 60−150 minutes per week; consistently active, median>150 minutes per week; and always active, all assessments>150 minutes per week. Outcomes were hospitalization, deterioration event, or death 90 days after a COVID-19 diagnosis. Data were analyzed in 2022. Results: Of 194,191 adults with COVID-19 infection, 6.3% were hospitalized, 3.1% experienced a deterioration event, and 2.8% died within 90 days. Dose-response effects were strong; for example, patients in the some activity category had higher odds of hospitalization (OR=1.43; 95% CI=1.26, 1.63), deterioration (OR=1.83; 95% CI=1.49, 2.25), and death (OR=1.92; 95% CI=1.48, 2.49) than those in the always active category. Results were generally consistent across sex, race and ethnicity, age, and BMI categories and for patients with cardiovascular disease or hypertension. Conclusions: There were protective associations of physical activity for adverse COVID-19 outcomes across demographic and clinical characteristics. Public health leaders should add physical activity to pandemic control strategies.
ACKNOWLEDGMENTS The authors thank the patients of Kaiser Permanente for helping to improve care through the use of information collected through our electronic health record systems. This study was supported in part by funding from the Kaiser Permanente Community Health Funds. No financial disclosures were reported by the authors of this paper.
CREDIT AUTHOR STATEMENT
SUPPLEMENTAL MATERIAL Supplemental materials associated with this article can be found in the online version at https://doi.org/10.1016/j. amepre.2022.10.007.
References
Ahmad, Cisewski, Miniño, Anderson, Provisional mortality data -United States, 2020, MMWR Morb Mortal Wkly Rep, doi:10.15585/mmwr.mm7014e1
Charlson, Pompei, Ales, Mackenzie, A new method of classifying prognostic comorbidity in longitudinal studies: development and validation, J Chronic Dis, doi:10.1016/0021-9681(87)90171-8
Chastin, Abaraogu, Bourgois, Effects of regular physical activity on the immune system, vaccination and risk of community-acquired infectious disease in the general population: systematic review and meta-analysis, Sports Med, doi:10.1007/s40279-021-01466-1
Coleman, Ngor, Reynolds, Initial validation of an exercise "vital sign" in electronic medical records, Med Sci Sports Exerc, doi:10.1249/MSS.0b013e3182630ec1
Emanuel, Osterholm, Gounder, A national strategy for the "new normal" of life with COVID, JAMA, doi:10.1001/jama.2021.24282
Evs, Exercise Vital Sign; min, minute. a Chi-square p-value
Ezzatvar, Ramírez, Elez, Izquierdo, Garcia-Hermoso, Physical activity and risk of infection, severity and mortality of COVID-19: a systematic review and non-linear dose-response meta-analysis of data from 1 853 610 adults, Br J Sports Med, doi:10.1136/bjsports-2022-105733
Hasson, Sallis, Coleman, Kaushal, Nocera et al., COVID-19: Implications for physical activity, health disparities, and health equity, Am J Lifestyle Med, doi:10.1177/15598276211029222
Hill, Whitfield, Morford, Brief summary of findings on the association between physical inactivity and severe COVID-19 outcomes
Johnson, Amin, Ali, COVID-19 incidence and death rates among unvaccinated and fully vaccinated adults with and without booster doses during periods of delta and omicron variant emergence -25 U.S. Jurisdictions, MMWR Morb Mortal Wkly Rep, doi:10.15585/mmwr.mm7104e2
Joseph, Keller, Adams, Ainsworth, Validity of two brief physical activity questionnaires with accelerometers among African-American women, Prim Health Care Res Dev, doi:10.1017/S1463423615000390
Koebnick, Langer-Gould, Gould, Sociodemographic characteristics of members of a large, integrated health care system: comparison with U.S. Census Bureau data, Perm J, doi:10.7812/TPP/12-031
Kuntz, Young, Saelens, Validity of the exercise vital sign tool to assess physical activity, Am J Prev Med, doi:10.1016/j.amepre.2021.01.012
Laddu, Lavie, Phillips, Arena, Physical activity for immunity protection: inoculating populations with healthy living medicine in preparation for the next pandemic, Prog Cardiovasc Dis, doi:10.1016/j.pcad.2020.04.006
Mackey, Ayers, Kondo, Racial and ethnic disparities in COVID-19-related infections, hospitalizations, and deaths: a systematic review, Ann Intern Med, doi:10.7326/M20-6306
Magesh, John, Li, Disparities in COVID-19 outcomes by race, ethnicity, and socioeconomic status: a systematic-review and meta-analysis, JAMA Netw Open, doi:10.1001/jamanetworkopen.2021.34147
Nau, Bruxvoort, Navarro, COVID-19 inequities across multiple racial and ethnic groups: results from an integrated health care organization, Ann Intern Med, doi:10.7326/M20-8283
Piercy, Troiano, Ballard, The physical activity guidelines for Americans, JAMA, doi:10.1001/jama.2018.14854
Powell, King, Buchner, The scientific foundation for the physical activity guidelines for Americans, J Phys Act Health, doi:10.1123/jpah.2018-0618
Rossen, Ahmad, Anderson, Disparities in excess mortality associated with COVID-19 -United States, 2020, MMWR Morb Mortal Wkly Rep, doi:10.15585/mmwr.mm7033a2
Sallis, Young, Tartof, Physical inactivity is associated with a higher risk for severe COVID-19 outcomes: a study in 48 440 adult patients, Br J Sports Med, doi:10.1136/bjsports-2021-104080
Sharp, Huang, Broder, Identifying patients with symptoms suspicious for COVID-19 at elevated risk of adverse events: the COVAS score, Am J Emerg Med, doi:10.1016/j.ajem.2020.10.068
Simpson, Katsanis, The immunological case for staying active during the COVID-19 pandemic, Brain Behav Immun, doi:10.1016/j.bbi.2020.04.041
Steenkamp, Saggers, Bandini, Small steps, strong shield: directly measured, moderate physical activity in 65 361 adults is associated with significant protective effects from severe COVID-19 outcomes, Br J Sports Med, doi:10.1136/bjsports-2021-105159
Tartof, Qian, Hong, Obesity and mortality among patients diagnosed with COVID-19: results from an integrated health care organization, Ann Intern Med, doi:10.7326/M20-3742
Williams, Sternthal, Understanding racial-ethnic disparities in health: sociological contributions, J Health Soc Behav, doi:10.1177/0022146510383838
Williamson, Walker, Bhaskaran, Factors associated with COVID-19-related death using OpenSAFELY, Nature, doi:10.1038/s41586-020-2521-4
Young, Coleman, Ngor, Reynolds, Sidell et al., Associations between physical activity and cardiometabolic risk factors assessed in a Southern California health care system, 2010 −2012, Prev Chronic Dis, doi:10.5888/pcd11.140196
Zheng, Qiu, Xia, Effect of aerobic exercise on inflammatory markers in healthy middle-aged and older adults: a systematic review and meta-analysis of randomized controlled trials, Front Aging Neurosci, doi:10.3389/fnagi.2019.00098
DOI record:
{
"DOI": "10.1016/j.amepre.2022.10.007",
"ISSN": [
"0749-3797"
],
"URL": "http://dx.doi.org/10.1016/j.amepre.2022.10.007",
"alternative-id": [
"S0749379722005268"
],
"assertion": [
{
"label": "This article is maintained by",
"name": "publisher",
"value": "Elsevier"
},
{
"label": "Article Title",
"name": "articletitle",
"value": "Associations of Physical Inactivity and COVID-19 Outcomes Among Subgroups"
},
{
"label": "Journal Title",
"name": "journaltitle",
"value": "American Journal of Preventive Medicine"
},
{
"label": "CrossRef DOI link to publisher maintained version",
"name": "articlelink",
"value": "https://doi.org/10.1016/j.amepre.2022.10.007"
},
{
"label": "Content Type",
"name": "content_type",
"value": "article"
},
{
"label": "Copyright",
"name": "copyright",
"value": "© 2022 American Journal of Preventive Medicine. Published by Elsevier Inc."
}
],
"author": [
{
"affiliation": [],
"family": "Young",
"given": "Deborah Rohm",
"sequence": "first"
},
{
"affiliation": [],
"family": "Sallis",
"given": "James F.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Baecker",
"given": "Aileen",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Cohen",
"given": "Deborah A.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Nau",
"given": "Claudia L.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Smith",
"given": "Gary N.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Sallis",
"given": "Robert E.",
"sequence": "additional"
}
],
"container-title": "American Journal of Preventive Medicine",
"container-title-short": "American Journal of Preventive Medicine",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"clinicalkey.fr",
"clinicalkey.jp",
"ajpm-online.net",
"clinicalkey.es",
"clinicalkey.com.au",
"clinicalkey.com",
"elsevier.com",
"sciencedirect.com"
]
},
"created": {
"date-parts": [
[
2022,
12,
15
]
],
"date-time": "2022-12-15T07:02:59Z",
"timestamp": 1671087779000
},
"deposited": {
"date-parts": [
[
2022,
12,
15
]
],
"date-time": "2022-12-15T07:03:39Z",
"timestamp": 1671087819000
},
"indexed": {
"date-parts": [
[
2022,
12,
16
]
],
"date-time": "2022-12-16T06:48:28Z",
"timestamp": 1671173308927
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2022,
12
]
]
},
"language": "en",
"license": [
{
"URL": "https://www.elsevier.com/tdm/userlicense/1.0/",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
12,
1
]
],
"date-time": "2022-12-01T00:00:00Z",
"timestamp": 1669852800000
}
},
{
"URL": "http://creativecommons.org/licenses/by-nc-nd/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
11,
18
]
],
"date-time": "2022-11-18T00:00:00Z",
"timestamp": 1668729600000
}
}
],
"link": [
{
"URL": "https://api.elsevier.com/content/article/PII:S0749379722005268?httpAccept=text/xml",
"content-type": "text/xml",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://api.elsevier.com/content/article/PII:S0749379722005268?httpAccept=text/plain",
"content-type": "text/plain",
"content-version": "vor",
"intended-application": "text-mining"
}
],
"member": "78",
"original-title": [],
"prefix": "10.1016",
"published": {
"date-parts": [
[
2022,
12
]
]
},
"published-print": {
"date-parts": [
[
2022,
12
]
]
},
"publisher": "Elsevier BV",
"reference": [
{
"key": "10.1016/j.amepre.2022.10.007_bib0001",
"unstructured": "Coronavirus disease (COVID-19) pandemic. World Health Organization.https://www.who.int/emergencies/diseases/novel-coronavirus-2019?adgroupsurvey={adgroupsurvey}&gclid=EAIaIQobChMIp7r9staI-gIVqxXUAR27qQwdEAAYAiAAEgKSJfD_BwE. Updated November 29, 2022. Accessed November 29, 2022."
},
{
"DOI": "10.1001/jama.2021.24282",
"article-title": "A national strategy for the “new normal” of life with COVID",
"author": "Emanuel",
"doi-asserted-by": "crossref",
"first-page": "211",
"issue": "3",
"journal-title": "JAMA",
"key": "10.1016/j.amepre.2022.10.007_bib0002",
"volume": "327",
"year": "2022"
},
{
"key": "10.1016/j.amepre.2022.10.007_bib0003",
"unstructured": "Centers for Disease Control and Prevention. COVID-19 after vaccination: possible breakthrough infection.https://www.cdc.gov/coronavirus/2019-ncov/vaccines/effectiveness/why-measure-effectiveness/breakthrough-cases.html. Updated June 23, 2022. Accessed November 29, 2022."
},
{
"DOI": "10.15585/mmwr.mm7104e2",
"article-title": "COVID-19 incidence and death rates among unvaccinated and fully vaccinated adults with and without booster doses during periods of delta and omicron variant emergence - 25 U.S. Jurisdictions, April 4–December 25, 2021",
"author": "Johnson",
"doi-asserted-by": "crossref",
"first-page": "132",
"issue": "4",
"journal-title": "MMWR Morb Mortal Wkly Rep",
"key": "10.1016/j.amepre.2022.10.007_bib0004",
"volume": "71",
"year": "2022"
},
{
"key": "10.1016/j.amepre.2022.10.007_bib0005",
"unstructured": "Hill AL, Whitfield G, Morford M, et al. Brief summary of findings on the association between physical inactivity and severe COVID-19 outcomes. https://www.cdc.gov/coronavirus/2019-ncov/downloads/clinical-care/E-Physical-Inactivity-Review.pdf. Accessed April 12, 2022."
},
{
"DOI": "10.1136/bjsports-2022-105733",
"article-title": "Physical activity and risk of infection, severity and mortality of COVID-19: a systematic review and non-linear dose-response meta-analysis of data from 1 853 610 adults",
"author": "Ezzatvar",
"doi-asserted-by": "crossref",
"journal-title": "Br J Sports Med",
"key": "10.1016/j.amepre.2022.10.007_bib0006",
"year": "2022"
},
{
"DOI": "10.1001/jama.2018.14854",
"article-title": "The physical activity guidelines for Americans",
"author": "Piercy",
"doi-asserted-by": "crossref",
"first-page": "2020",
"issue": "19",
"journal-title": "JAMA",
"key": "10.1016/j.amepre.2022.10.007_bib0007",
"volume": "320",
"year": "2018"
},
{
"DOI": "10.1136/bjsports-2021-104080",
"article-title": "Physical inactivity is associated with a higher risk for severe COVID-19 outcomes: a study in 48 440 adult patients",
"author": "Sallis",
"doi-asserted-by": "crossref",
"first-page": "1099",
"issue": "19",
"journal-title": "Br J Sports Med",
"key": "10.1016/j.amepre.2022.10.007_bib0008",
"volume": "55",
"year": "2021"
},
{
"DOI": "10.1123/jpah.2018-0618",
"article-title": "The scientific foundation for the physical activity guidelines for Americans",
"author": "Powell",
"doi-asserted-by": "crossref",
"first-page": "1",
"issue": "1",
"journal-title": "J Phys Act Health",
"key": "10.1016/j.amepre.2022.10.007_bib0009",
"volume": "16",
"year": "2018"
},
{
"DOI": "10.1007/s40279-021-01466-1",
"article-title": "Effects of regular physical activity on the immune system, vaccination and risk of community-acquired infectious disease in the general population: systematic review and meta-analysis",
"author": "Chastin",
"doi-asserted-by": "crossref",
"first-page": "1673",
"issue": "8",
"journal-title": "Sports Med",
"key": "10.1016/j.amepre.2022.10.007_bib0010",
"volume": "51",
"year": "2021"
},
{
"DOI": "10.1016/j.pcad.2020.04.006",
"article-title": "Physical activity for immunity protection: inoculating populations with healthy living medicine in preparation for the next pandemic",
"author": "Laddu",
"doi-asserted-by": "crossref",
"first-page": "102",
"journal-title": "Prog Cardiovasc Dis",
"key": "10.1016/j.amepre.2022.10.007_bib0011",
"volume": "64",
"year": "2021"
},
{
"DOI": "10.1016/j.bbi.2020.04.041",
"article-title": "The immunological case for staying active during the COVID-19 pandemic",
"author": "Simpson",
"doi-asserted-by": "crossref",
"first-page": "6",
"journal-title": "Brain Behav Immun",
"key": "10.1016/j.amepre.2022.10.007_bib0012",
"volume": "87",
"year": "2020"
},
{
"DOI": "10.3389/fnagi.2019.00098",
"article-title": "Effect of aerobic exercise on inflammatory markers in healthy middle-aged and older adults: a systematic review and meta-analysis of randomized controlled trials",
"author": "Zheng",
"doi-asserted-by": "crossref",
"first-page": "98",
"journal-title": "Front Aging Neurosci",
"key": "10.1016/j.amepre.2022.10.007_bib0013",
"volume": "11",
"year": "2019"
},
{
"DOI": "10.15585/mmwr.mm7033a2",
"article-title": "Disparities in excess mortality associated with COVID-19 - United States, 2020",
"author": "Rossen",
"doi-asserted-by": "crossref",
"first-page": "1114",
"issue": "33",
"journal-title": "MMWR Morb Mortal Wkly Rep",
"key": "10.1016/j.amepre.2022.10.007_bib0014",
"volume": "70",
"year": "2021"
},
{
"DOI": "10.15585/mmwr.mm7014e1",
"article-title": "Provisional mortality data - United States, 2020",
"author": "Ahmad",
"doi-asserted-by": "crossref",
"first-page": "519",
"issue": "14",
"journal-title": "MMWR Morb Mortal Wkly Rep",
"key": "10.1016/j.amepre.2022.10.007_bib0015",
"volume": "70",
"year": "2021"
},
{
"DOI": "10.7326/M20-6306",
"article-title": "Racial and ethnic disparities in COVID-19-related infections, hospitalizations, and deaths: a systematic review",
"author": "Mackey",
"doi-asserted-by": "crossref",
"first-page": "362",
"issue": "3",
"journal-title": "Ann Intern Med",
"key": "10.1016/j.amepre.2022.10.007_bib0016",
"volume": "174",
"year": "2021"
},
{
"DOI": "10.1001/jamanetworkopen.2021.34147",
"article-title": "Disparities in COVID-19 outcomes by race, ethnicity, and socioeconomic status: a systematic-review and meta-analysis",
"author": "Magesh",
"doi-asserted-by": "crossref",
"issue": "11",
"journal-title": "JAMA Netw Open",
"key": "10.1016/j.amepre.2022.10.007_bib0017",
"volume": "4",
"year": "2021"
},
{
"DOI": "10.1177/15598276211029222",
"article-title": "COVID-19: Implications for physical activity, health disparities, and health equity",
"author": "Hasson",
"doi-asserted-by": "crossref",
"first-page": "420",
"issue": "4",
"journal-title": "Am J Lifestyle Med",
"key": "10.1016/j.amepre.2022.10.007_bib0018",
"volume": "16",
"year": "2022"
},
{
"DOI": "10.7812/TPP/12-031",
"article-title": "Sociodemographic characteristics of members of a large, integrated health care system: comparison with U.S. Census Bureau data",
"author": "Koebnick",
"doi-asserted-by": "crossref",
"first-page": "37",
"issue": "3",
"journal-title": "Perm J",
"key": "10.1016/j.amepre.2022.10.007_bib0019",
"volume": "16",
"year": "2012"
},
{
"DOI": "10.1249/MSS.0b013e3182630ec1",
"article-title": "Initial validation of an exercise “vital sign” in electronic medical records",
"author": "Coleman",
"doi-asserted-by": "crossref",
"first-page": "2071",
"issue": "11",
"journal-title": "Med Sci Sports Exerc",
"key": "10.1016/j.amepre.2022.10.007_bib0020",
"volume": "44",
"year": "2012"
},
{
"DOI": "10.5888/pcd11.140196",
"article-title": "Associations between physical activity and cardiometabolic risk factors assessed in a Southern California health care system, 2010–2012",
"author": "Young",
"doi-asserted-by": "crossref",
"first-page": "E219",
"journal-title": "Prev Chronic Dis",
"key": "10.1016/j.amepre.2022.10.007_bib0021",
"volume": "11",
"year": "2014"
},
{
"DOI": "10.1016/j.amepre.2021.01.012",
"article-title": "Validity of the exercise vital sign tool to assess physical activity",
"author": "Kuntz",
"doi-asserted-by": "crossref",
"first-page": "866",
"issue": "6",
"journal-title": "Am J Prev Med",
"key": "10.1016/j.amepre.2022.10.007_bib0022",
"volume": "60",
"year": "2021"
},
{
"DOI": "10.1017/S1463423615000390",
"doi-asserted-by": "crossref",
"key": "10.1016/j.amepre.2022.10.007_bib0023",
"unstructured": "Joseph RP, Keller C, Adams MA, Ainsworth BE. Validity of two brief physical activity questionnaires with accelerometers among African-American women. Prim Health Care Res Dev. 2016;17(3):265–276. https://doi.org/10.1017/S1463423615000390."
},
{
"key": "10.1016/j.amepre.2022.10.007_bib0024",
"unstructured": "People with certain medical conditions. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html. Updated November 22, 2022. Accessed November 29, 2022."
},
{
"DOI": "10.1016/0021-9681(87)90171-8",
"article-title": "A new method of classifying prognostic comorbidity in longitudinal studies: development and validation",
"author": "Charlson",
"doi-asserted-by": "crossref",
"first-page": "373",
"issue": "5",
"journal-title": "J Chronic Dis",
"key": "10.1016/j.amepre.2022.10.007_bib0025",
"volume": "40",
"year": "1987"
},
{
"DOI": "10.1177/0022146510383838",
"article-title": "Understanding racial-ethnic disparities in health: sociological contributions",
"author": "Williams",
"doi-asserted-by": "crossref",
"first-page": "S15",
"issue": "suppl",
"journal-title": "J Health Soc Behav",
"key": "10.1016/j.amepre.2022.10.007_bib0026",
"volume": "51",
"year": "2010"
},
{
"DOI": "10.1038/s41586-020-2521-4",
"article-title": "Factors associated with COVID-19-related death using OpenSAFELY",
"author": "Williamson",
"doi-asserted-by": "crossref",
"first-page": "430",
"issue": "7821",
"journal-title": "Nature",
"key": "10.1016/j.amepre.2022.10.007_bib0027",
"volume": "584",
"year": "2020"
},
{
"DOI": "10.1136/bjsports-2021-105159",
"article-title": "Small steps, strong shield: directly measured, moderate physical activity in 65 361 adults is associated with significant protective effects from severe COVID-19 outcomes",
"author": "Steenkamp",
"doi-asserted-by": "crossref",
"first-page": "568",
"issue": "10",
"journal-title": "Br J Sports Med",
"key": "10.1016/j.amepre.2022.10.007_bib0028",
"volume": "56",
"year": "2022"
},
{
"DOI": "10.7326/M20-8283",
"article-title": "COVID-19 inequities across multiple racial and ethnic groups: results from an integrated health care organization",
"author": "Nau",
"doi-asserted-by": "crossref",
"first-page": "1183",
"issue": "8",
"journal-title": "Ann Intern Med",
"key": "10.1016/j.amepre.2022.10.007_bib0029",
"volume": "174",
"year": "2021"
},
{
"DOI": "10.1016/j.ajem.2020.10.068",
"article-title": "Identifying patients with symptoms suspicious for COVID-19 at elevated risk of adverse events: the COVAS score",
"author": "Sharp",
"doi-asserted-by": "crossref",
"first-page": "489",
"journal-title": "Am J Emerg Med",
"key": "10.1016/j.amepre.2022.10.007_bib0030",
"volume": "46",
"year": "2021"
},
{
"DOI": "10.7326/M20-3742",
"article-title": "Obesity and mortality among patients diagnosed with COVID-19: results from an integrated health care organization",
"author": "Tartof",
"doi-asserted-by": "crossref",
"first-page": "773",
"issue": "10",
"journal-title": "Ann Intern Med",
"key": "10.1016/j.amepre.2022.10.007_bib0031",
"volume": "173",
"year": "2020"
}
],
"reference-count": 31,
"references-count": 31,
"relation": {},
"resource": {
"primary": {
"URL": "https://linkinghub.elsevier.com/retrieve/pii/S0749379722005268"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Public Health, Environmental and Occupational Health",
"Epidemiology"
],
"subtitle": [],
"title": "Associations of Physical Inactivity and COVID-19 Outcomes Among Subgroups",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1016/elsevier_cm_policy"
}
