3219 hospitalised patients with COVID-19 in Southeast Michigan: a retrospective case cohort study
et al., BMJ Open, doi:10.1136/bmjopen-2020-042042, Apr 2021
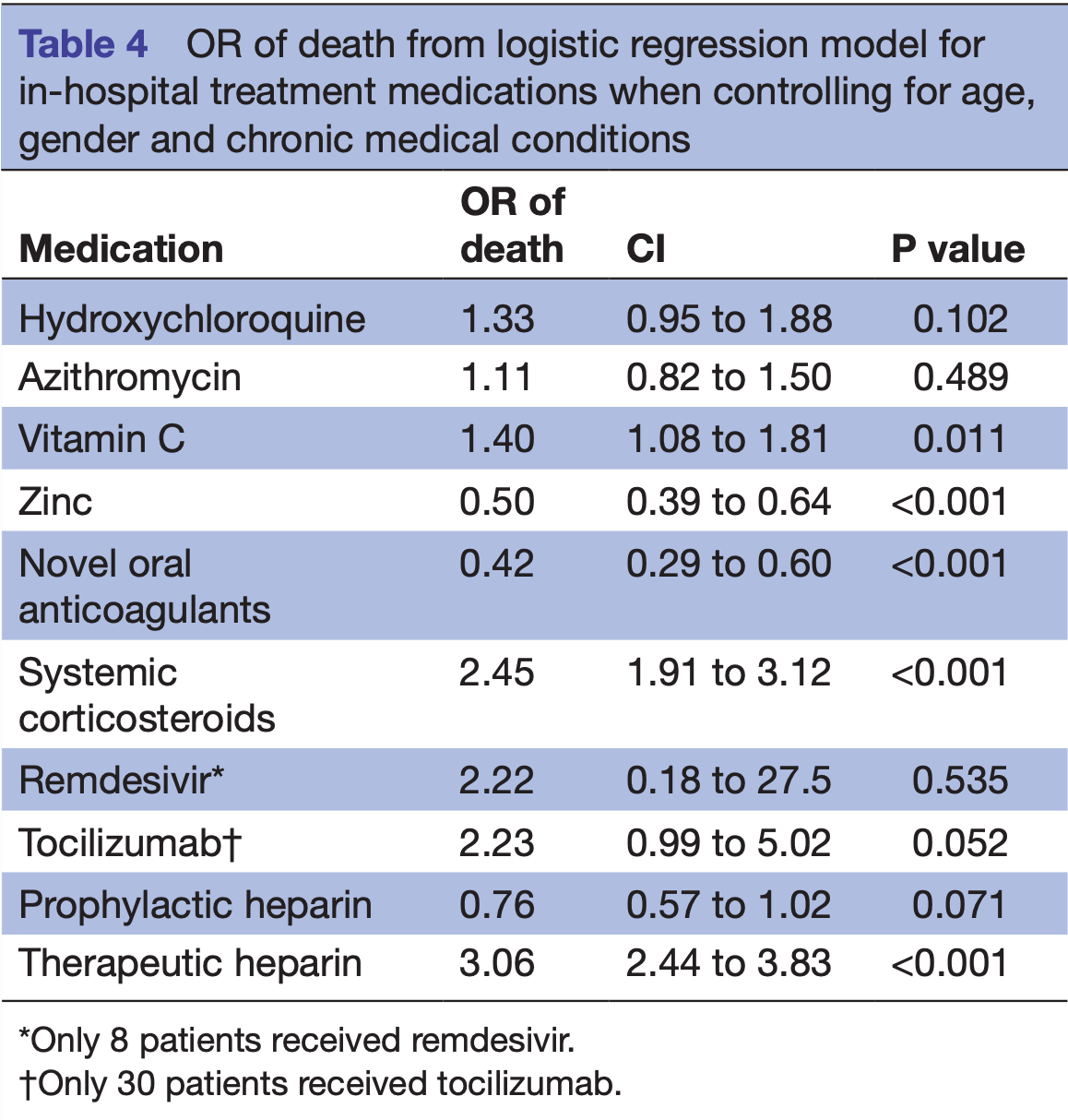
Retrospective database analysis of 3,219 hospitalized patients in the USA. Very different results in the time period analysis (Table S2), and results significantly different to other studies for the same medications (e.g., heparin OR 3.06 [2.44-3.83]) suggest significant confounding by indication and confounding by time.
Gérard, Zhou, Wu, Kamo, Choi, Kim show increased risk of acute kidney injury, Leo, Briciu, Muntean, Petrov show increased risk of liver injury, and Negru, Cheng, Mohammed, Kwok show increased risk of cardiac disorders with remdesivir.
Standard of Care (SOC) for COVID-19 in the study country,
the USA, is very poor with very low average efficacy for approved treatments15.
Only expensive, high-profit treatments were approved for early treatment. Low-cost treatments were excluded, reducing the probability of early treatment due to access and cost barriers, and eliminating complementary and synergistic benefits seen with many low-cost treatments.
This study is excluded in the after exclusion results of meta-analysis:
substantial unadjusted confounding by indication likely; substantial confounding by time possible due to significant changes in SOC and treatment propensity during the study period.
|
risk of death, 85.7% higher, RR 1.86, p = 0.54, treatment 1 of 8 (12.5%), control 515 of 3,211 (16.0%), adjusted per study, odds ratio converted to relative risk, logistic regression.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
1.
Gérard et al., Remdesivir and Acute Renal Failure: A Potential Safety Signal From Disproportionality Analysis of the WHO Safety Database, Clinical Pharmacology & Therapeutics, doi:10.1002/cpt.2145.
2.
Zhou et al., Acute Kidney Injury and Drugs Prescribed for COVID-19 in Diabetes Patients: A Real-World Disproportionality Analysis, Frontiers in Pharmacology, doi:10.3389/fphar.2022.833679.
3.
Wu et al., Acute Kidney Injury Associated With Remdesivir: A Comprehensive Pharmacovigilance Analysis of COVID-19 Reports in FAERS, Frontiers in Pharmacology, doi:10.3389/fphar.2022.692828.
4.
Kamo et al., Association of Antiviral Drugs for the Treatment of COVID-19 With Acute Renal Failure, In Vivo, doi:10.21873/invivo.13637.
5.
Choi et al., Comparative effectiveness of combination therapy with nirmatrelvir–ritonavir and remdesivir versus monotherapy with remdesivir or nirmatrelvir–ritonavir in patients hospitalised with COVID-19: a target trial emulation study, The Lancet Infectious Diseases, doi:10.1016/S1473-3099(24)00353-0.
6.
Kim et al., Investigating the Safety Profile of Fast‐Track COVID‐19 Drugs Using the FDA Adverse Event Reporting System Database: A Comparative Observational Study, Pharmacoepidemiology and Drug Safety, doi:10.1002/pds.70043.
7.
Leo et al., Hepatocellular liver injury in hospitalized patients affected by COVID-19: Presence of different risk factors at different time points, Digestive and Liver Disease, doi:10.1016/j.dld.2021.12.014.
8.
Briciu et al., Evolving Clinical Manifestations and Outcomes in COVID-19 Patients: A Comparative Analysis of SARS-CoV-2 Variant Waves in a Romanian Hospital Setting, Pathogens, doi:10.3390/pathogens12121453.
9.
Muntean et al., Effects of COVID-19 on the Liver and Mortality in Patients with SARS-CoV-2 Pneumonia Caused by Delta and Non-Delta Variants: An Analysis in a Single Centre, Pharmaceuticals, doi:10.3390/ph17010003.
10.
Petrov et al., The Effect of Potentially Hepatotoxic Medicinal Products on Alanine Transaminase Levels in COVID-19 Patients: A Case–Control Study, Safety and Risk of Pharmacotherapy, doi:10.30895/2312-7821-2025-458.
11.
Negru et al., Comparative Pharmacovigilance Analysis of Approved and Repurposed Antivirals for COVID-19: Insights from EudraVigilance Data, Biomedicines, doi:10.3390/biomedicines13061387.
12.
Cheng et al., Cardiovascular Safety of COVID-19 Treatments: A Disproportionality Analysis of Adverse Event Reports from the WHO VigiBase, Infectious Diseases and Therapy, doi:10.1007/s40121-025-01225-z.
13.
Mohammed et al., Bradycardia associated with remdesivir treatment in coronavirus disease 2019 patients: A propensity score-matched analysis, Medicine, doi:10.1097/MD.0000000000044501.
Mulhem et al., 7 Apr 2021, retrospective, database analysis, USA, peer-reviewed, 3 authors.
3219 hospitalised patients with COVID-19 in Southeast Michigan: a retrospective case cohort study
BMJ Open, doi:10.1136/bmjopen-2020-042042
Objective To report the clinical characteristics of patients hospitalised with COVID-19 in Southeast Michigan. Design Retrospective cohort study. Setting Eight hospitals in Southeast Michigan. Participants 3219 hospitalised patients with a positive SARS-CoV-2 infection by nasopharyngeal PCR test from 13 March 2020 until 29 April 2020. Main outcomes measures Outcomes were discharge from the hospital or in-hospital death. Examined predictors included patient demographics, chronic diseases, home medications, mechanical ventilation, in-hospital medications and timeframe of hospital admission. Multivariable logistic regression was conducted to identify risk factors for in-hospital mortality. Results During the study period, 3219 (90.4%) patients were discharged or died in the hospital. The median age was 65.2 (IQR 52.6-77.2) years, the median length of stay in the hospital was 6.0 (IQR 3.2-10.1) days, and 51% were female. Hypertension was the most common chronic disease, occurring in 2386 (74.1%) patients. Overall mortality rate was 16.0%. Blacks represented 52.3% of patients and had a mortality rate of 13.5%. Mortality was highest at 18.5% in the prepeak hospital COVID-19 volume, decreasing to 15.3% during the peak period and to 10.8% in the postpeak period. Multivariable regression showed increasing odds of in-hospital death associated with older age (OR 1.04, 95% CI 1.03 to 1.05, p<0.001) for every increase in 1 year of age and being male (OR 1.47, 95% CI 1.21 to 1.81, p<0.001). Certain chronic diseases increased the odds of in-hospital mortality, especially chronic kidney disease. Administration of vitamin C, corticosteroids and therapeutic heparin in the hospital was associated with higher odds of death. Conclusion In-hospital mortality was highest in early admissions and improved as our experience in treating patients with COVID-19 increased. Blacks were more likely to get admitted to the hospital and to receive mechanical ventilation, but less likely to die in the hospital than whites. COVID-19 was first reported as an outbreak of pneumonia of unknown cause in Wuhan, China in December 2019. 1 The virus responsible was subsequently named SARS-CoV-2. The first confirmed case in the USA was reported on 31 January 2020, and the first case in Michigan was reported on 10 March 2020. 2 As of 1 June 2020, 57 532 cases have
Competing interests None declared. Patient consent for publication Not required.
Ethics approval The study was approved by Beaumont IRB (study ID: 2020-161). Provenance and peer review Not commissioned; externally peer reviewed.
Data availability statement Data available per reasonable request. Supplemental material This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise. Open access This is an open access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited, appropriate credit is given, any changes made indicated, and the use is non-commercial. See: http:// creativecommons. org/ licenses/ by-nc/ 4. 0/.
..
References
Cummings, Epidemiology, clinical course, and outcomes of critically ill adults with COVID-19 in New York City: a prospective cohort study, Lancet
Garg, Kim, Whitaker, Hospitalization Rates and Characteristics of Patients Hospitalized with Laboratory-Confirmed Coronavirus Disease 2019 -COVID-NET, 14 States, MMWR Morb Mortal Wkly Rep, doi:10.15585/mmwr.mm6915e3
Grasselli, Zangrillo, Zanella, Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy region, Italy, JAMA, doi:10.1001/jama.2020.5394
Mackey, Risks and impact of angiotensin-converting enzyme inhibitors or angiotensin-receptor blockers on SARS-CoV-2 infection in adults, Ann Intern Med
Michigan, Gov, None
Petrilli, Jones, Yang, Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in New York City: prospective cohort study, BMJ, doi:10.1136/bmj.m1966
Phelan, Katz, Lo, The Novel Coronavirus Originating in Wuhan, China: Challenges for Global Health Governance, JAMA, doi:10.1001/jama.2020.1097
Richardson, Hirsch, Narasimhan, Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the new York City area, JAMA, doi:10.1001/jama.2020.6775
Sommerstein, Kochen, Messerli, Coronavirus disease 2019 (COVID-19): do angiotensin-converting enzyme Inhibitors/ Angiotensin receptor blockers have a biphasic effect?, J Am Heart Assoc, doi:10.1161/JAHA.120.016509
Suleyman, Fadel, Malette, Clinical characteristics and morbidity associated with coronavirus disease 2019 in a series of patients in metropolitan Detroit, JAMA Netw Open, doi:10.1001/jamanetworkopen.2020.12270
Wu, Mcgoogan, Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72 314 Cases From the Chinese Center for Disease Control and Prevention, JAMA, doi:10.1001/jama.2020.2648
Xie, Tong, Guan, Clinical characteristics of patients who died of coronavirus disease 2019 in China, JAMA Netw Open, doi:10.1001/jamanetworkopen.2020.5619
Yancy, COVID-19 and African Americans, JAMA, doi:10.1001/jama.2020.6548
Zhou, Yu, Du, Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study, Lancet, doi:10.1016/S0140-6736(20)30566-3
DOI record:
{
"DOI": "10.1136/bmjopen-2020-042042",
"ISSN": [
"2044-6055",
"2044-6055"
],
"URL": "http://dx.doi.org/10.1136/bmjopen-2020-042042",
"abstract": "<jats:sec><jats:title>Objective</jats:title><jats:p>To report the clinical characteristics of patients hospitalised with COVID-19 in Southeast Michigan.</jats:p></jats:sec><jats:sec><jats:title>Design</jats:title><jats:p>Retrospective cohort study.</jats:p></jats:sec><jats:sec><jats:title>Setting</jats:title><jats:p>Eight hospitals in Southeast Michigan.</jats:p></jats:sec><jats:sec><jats:title>Participants</jats:title><jats:p>3219 hospitalised patients with a positive SARS-CoV-2 infection by nasopharyngeal PCR test from 13 March 2020 until 29 April 2020.</jats:p></jats:sec><jats:sec><jats:title>Main outcomes measures</jats:title><jats:p>Outcomes were discharge from the hospital or in-hospital death. Examined predictors included patient demographics, chronic diseases, home medications, mechanical ventilation, in-hospital medications and timeframe of hospital admission. Multivariable logistic regression was conducted to identify risk factors for in-hospital mortality.</jats:p></jats:sec><jats:sec><jats:title>Results</jats:title><jats:p>During the study period, 3219 (90.4%) patients were discharged or died in the hospital. The median age was 65.2 (IQR 52.6–77.2) years, the median length of stay in the hospital was 6.0 (IQR 3.2–10.1) days, and 51% were female. Hypertension was the most common chronic disease, occurring in 2386 (74.1%) patients. Overall mortality rate was 16.0%. Blacks represented 52.3% of patients and had a mortality rate of 13.5%. Mortality was highest at 18.5% in the prepeak hospital COVID-19 volume, decreasing to 15.3% during the peak period and to 10.8% in the postpeak period. Multivariable regression showed increasing odds of in-hospital death associated with older age (OR 1.04, 95% CI 1.03 to 1.05, p<0.001) for every increase in 1 year of age and being male (OR 1.47, 95% CI 1.21 to 1.81, p<0.001). Certain chronic diseases increased the odds of in-hospital mortality, especially chronic kidney disease. Administration of vitamin C, corticosteroids and therapeutic heparin in the hospital was associated with higher odds of death.</jats:p></jats:sec><jats:sec><jats:title>Conclusion</jats:title><jats:p>In-hospital mortality was highest in early admissions and improved as our experience in treating patients with COVID-19 increased. Blacks were more likely to get admitted to the hospital and to receive mechanical ventilation, but less likely to die in the hospital than whites.</jats:p></jats:sec>",
"alternative-id": [
"10.1136/bmjopen-2020-042042"
],
"author": [
{
"ORCID": "http://orcid.org/0000-0003-0194-2203",
"affiliation": [],
"authenticated-orcid": false,
"family": "Mulhem",
"given": "Elie",
"sequence": "first"
},
{
"affiliation": [],
"family": "Oleszkowicz",
"given": "Andrew",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Lick",
"given": "David",
"sequence": "additional"
}
],
"container-title": "BMJ Open",
"container-title-short": "BMJ Open",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"bmj.com"
]
},
"created": {
"date-parts": [
[
2021,
4,
7
]
],
"date-time": "2021-04-07T18:33:51Z",
"timestamp": 1617820431000
},
"deposited": {
"date-parts": [
[
2021,
4,
7
]
],
"date-time": "2021-04-07T18:34:04Z",
"timestamp": 1617820444000
},
"indexed": {
"date-parts": [
[
2024,
2,
19
]
],
"date-time": "2024-02-19T13:44:14Z",
"timestamp": 1708350254297
},
"is-referenced-by-count": 8,
"issue": "4",
"issued": {
"date-parts": [
[
2021,
4
]
]
},
"journal-issue": {
"issue": "4",
"published-online": {
"date-parts": [
[
2021,
4,
7
]
]
},
"published-print": {
"date-parts": [
[
2021,
4
]
]
}
},
"language": "en",
"license": [
{
"URL": "http://creativecommons.org/licenses/by-nc/4.0/",
"content-version": "unspecified",
"delay-in-days": 5,
"start": {
"date-parts": [
[
2021,
4,
6
]
],
"date-time": "2021-04-06T00:00:00Z",
"timestamp": 1617667200000
}
}
],
"link": [
{
"URL": "https://syndication.highwire.org/content/doi/10.1136/bmjopen-2020-042042",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "239",
"original-title": [],
"page": "e042042",
"prefix": "10.1136",
"published": {
"date-parts": [
[
2021,
4
]
]
},
"published-online": {
"date-parts": [
[
2021,
4,
7
]
]
},
"published-print": {
"date-parts": [
[
2021,
4
]
]
},
"publisher": "BMJ",
"reference": [
{
"DOI": "10.1001/jama.2020.1097",
"article-title": "The Novel Coronavirus Originating in Wuhan, China: Challenges for Global Health Governance",
"author": "Phelan",
"doi-asserted-by": "crossref",
"first-page": "709-710",
"journal-title": "JAMA",
"key": "2021040709453977000_11.4.e042042.1",
"volume": "323",
"year": "2020"
},
{
"key": "2021040709453977000_11.4.e042042.2",
"unstructured": "Michigan.gov, C.M.D . Available: https://www.michigan.gov/coronavirus/0,9753,7-406-98163_98173-,00.html [Accessed 6 Jan 2020]."
},
{
"DOI": "10.1001/jamanetworkopen.2020.5619",
"article-title": "Clinical characteristics of patients who died of coronavirus disease 2019 in China",
"author": "Xie",
"doi-asserted-by": "crossref",
"journal-title": "JAMA Netw Open",
"key": "2021040709453977000_11.4.e042042.3",
"volume": "3",
"year": "2020"
},
{
"DOI": "10.1001/jama.2020.5394",
"article-title": "Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy region, Italy",
"author": "Grasselli",
"doi-asserted-by": "crossref",
"first-page": "1574",
"journal-title": "JAMA",
"key": "2021040709453977000_11.4.e042042.4",
"volume": "323",
"year": "2020"
},
{
"DOI": "10.1001/jama.2020.6775",
"doi-asserted-by": "publisher",
"key": "2021040709453977000_11.4.e042042.5"
},
{
"DOI": "10.1056/NEJMsa2011686",
"doi-asserted-by": "crossref",
"key": "2021040709453977000_11.4.e042042.6",
"unstructured": "Price-Haywood EG et al . Hospitalization and mortality among black patients and white patients with Covid-19. N Engl J Med 2020."
},
{
"DOI": "10.1001/jamanetworkopen.2020.12270",
"article-title": "Clinical characteristics and morbidity associated with coronavirus disease 2019 in a series of patients in metropolitan Detroit",
"author": "Suleyman",
"doi-asserted-by": "crossref",
"journal-title": "JAMA Netw Open",
"key": "2021040709453977000_11.4.e042042.7",
"volume": "3",
"year": "2020"
},
{
"DOI": "10.1016/S0140-6736(20)30566-3",
"doi-asserted-by": "publisher",
"key": "2021040709453977000_11.4.e042042.8"
},
{
"DOI": "10.1136/bmj.m1966",
"doi-asserted-by": "publisher",
"key": "2021040709453977000_11.4.e042042.9"
},
{
"DOI": "10.15585/mmwr.mm6915e3",
"doi-asserted-by": "publisher",
"key": "2021040709453977000_11.4.e042042.10"
},
{
"DOI": "10.1001/jama.2020.6548",
"doi-asserted-by": "publisher",
"key": "2021040709453977000_11.4.e042042.11"
},
{
"key": "2021040709453977000_11.4.e042042.12",
"unstructured": "New York state department of health. COVID-19 fatalities. Available: https://covid19tracker.health.ny.gov/views/NYS-COVID19-Tracker/NYSDOHCOVID-19Tracker-Fatalities?%3Aembed=yes&%3Atoolbar=no&%3Atabs=n [Accessed 1 Jun 2020]."
},
{
"key": "2021040709453977000_11.4.e042042.13",
"unstructured": "lab, A.R . The color of coronavirus. Available: https://www.apmresearchlab.org/covid/deaths-by-race#reporting [Accessed 16 Jun 2020]."
},
{
"DOI": "10.1016/S0140-6736(20)31189-2",
"doi-asserted-by": "crossref",
"key": "2021040709453977000_11.4.e042042.14",
"unstructured": "Cummings MJ et al . Epidemiology, clinical course, and outcomes of critically ill adults with COVID-19 in New York City: a prospective cohort study. Lancet 2020."
},
{
"DOI": "10.1001/jama.2020.2648",
"article-title": "Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72 314 Cases From the Chinese Center for Disease Control and Prevention",
"author": "Wu",
"doi-asserted-by": "crossref",
"first-page": "1239-1242",
"journal-title": "JAMA",
"key": "2021040709453977000_11.4.e042042.15",
"volume": "323",
"year": "2020"
},
{
"DOI": "10.1161/JAHA.120.016509",
"doi-asserted-by": "publisher",
"key": "2021040709453977000_11.4.e042042.16"
},
{
"DOI": "10.7326/L20-0969",
"doi-asserted-by": "crossref",
"key": "2021040709453977000_11.4.e042042.17",
"unstructured": "Mackey K et al . Risks and impact of angiotensin-converting enzyme inhibitors or angiotensin-receptor blockers on SARS-CoV-2 infection in adults. Ann Intern Med 2020."
}
],
"reference-count": 17,
"references-count": 17,
"relation": {},
"resource": {
"primary": {
"URL": "https://bmjopen.bmj.com/lookup/doi/10.1136/bmjopen-2020-042042"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"General Medicine"
],
"subtitle": [],
"title": "3219 hospitalised patients with COVID-19 in Southeast Michigan: a retrospective case cohort study",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1136/crossmarkpolicy",
"volume": "11"
}
mulhem