Drug prescription patterns and their association with mortality and hospitalization duration in COVID-19 patients: insights from big data
et al., Frontiers in Public Health, doi:10.3389/fpubh.2023.1280434, Dec 2023
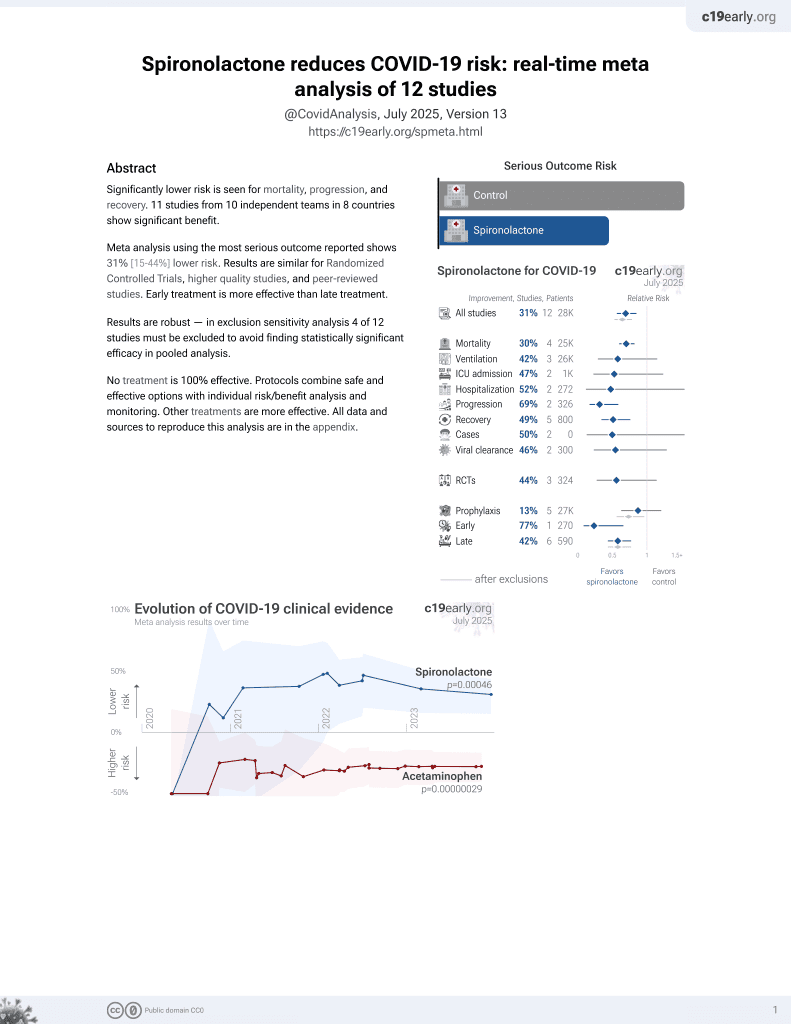
37th treatment shown to reduce risk in
February 2022, now with p = 0.00046 from 12 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
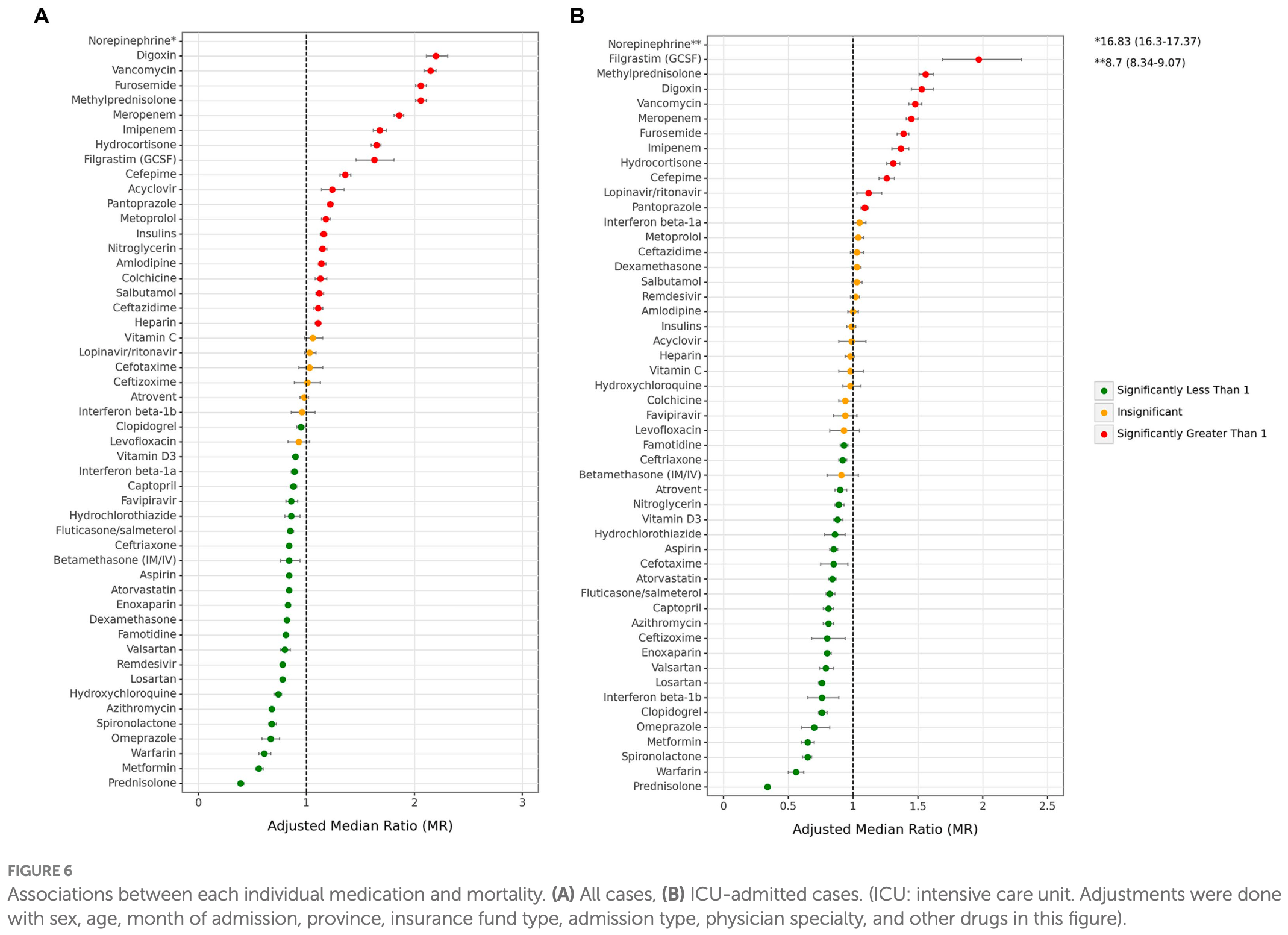
Retrospective study of 917,198 hospitalized COVID-19 cases covered by the Iran Health Insurance Organization over 26 months showing that antithrombotics, corticosteroids, and antivirals reduced mortality while diuretics, antibiotics, and antidiabetics increased it. Confounding makes some results very unreliable. For example, diuretics like furosemide are often used to treat fluid overload, which is more likely in ICU or advanced disease requiring aggressive fluid resuscitation. Hospitalization length has increased risk of significant confounding, for example longer hospitalization increases the chance of receiving a medication, and death may result in shorter hospitalization. Mortality results may be more reliable.
Confounding by indication is likely to be significant for many medications. Authors adjustments have very limited severity information (admission type refers to ward vs. ER department on initial arrival). We can estimate the impact of confounding from typical usage patterns, the prescription frequency, and attenuation or increase of risk for ICU vs. all patients.
|
risk of death, 32.0% lower, OR 0.68, p < 0.001, RR approximated with OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Mehrizi et al., 18 Dec 2023, retrospective, Iran, peer-reviewed, 10 authors, study period 1 February, 2020 - 20 March, 2022.
Contact: rdaroudi@sina.tums.ac.ir.
Drug prescription patterns and their association with mortality and hospitalization duration in COVID-19 patients: insights from big data
Frontiers in Public Health, doi:10.3389/fpubh.2023.1280434
Background: Different medication prescription patterns have been associated with varying course of disease and outcomes in COVID-19. Health claims data is a rich source of information on disease treatment and outcomes. We aimed to investigate drug prescription patterns and their association with mortality and hospitalization via insurance data for a relatively long period of the pandemic in Iran.
Methods: We retrieved hospitalized patients' data from Iran Health Insurance Organization (IHIO) spanning 26 months (2020-2022) nationwide. Included were patients with ICD-10 codes U07.1/U07.2 for confirmed/suspected COVID-19. A case was defined as a single hospitalization event for an individual patient. Multiple hospitalizations of a patient within a 30-day interval were aggregated into a single case, while hospitalizations with intervals exceeding 30 days were treated as independent cases. The Anatomical Therapeutic Chemical (ATC) was used for medications classification. The two main study outcomes were general and intensive care unit (ICU) hospitalization periods and mortality. Besides, various demographic and clinical associate factors were analyzed to derive the associations with medication prescription patterns and study outcomes using accelerated failure time (AFT) and logistic regression models. Results: During the 26 months of the study period, 1,113,678 admissions with COVID-19 diagnosis at hospitals working in company with IHIO were recorded. 917,198 cases were detected from the database, among which 51.91% were females and 48.09% were males. Among the main groups of medications, antithrombotics (55. ), corticosteroids (54.14% [54.04-54.24]), and antibiotics (42.22% [42.12-42.32]) were the top used medications among cases with COVID-19. Investigation of the duration of hospitalization based on main medication groups showed antithrombotics (adjusted median ratio = 0.94 [0.94-0.95]) were significantly associated with shorter periods of overall hospitalization. Also, antithrombotics (adjusted odds ratio = 0.74 [95%CI,
Ethics statement This study was approved by the ethical committee at the School of Public Health, Tehran University of Medical Sciences (code: IR.TUMS. SPH.REC.1401.120). The provided data by IHIO in this study were de-identified and data holder and study investigators were responsible to save the privacy of the patients and users of the IHIO insurance services. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants' legal guardians/next of kin in accordance with the national legislation and institutional requirements.
Author contributions
Conflict of interest The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1280434/ full#supplementary-material
References
Abbasi-Kangevari, Ghanbari, Malekpour, Ghamari, Azadnajafabad et al., Exploring the clinical benefit of ventilation therapy across various patient groups with COVID-19 using real-world data, Sci Rep, doi:10.1038/s41598-023-37912-5
Amraei, Rahimi, COVID-19, renin-angiotensin system and endothelial dysfunction, Cells, doi:10.3390/cells9071652
Azadnajafabad, Ghasemi, Moghaddam, Rezaei, Farzadfar, Noncommunicable Diseases' contribution to the COVID-19 mortality: a global warning on the emerging Syndemics, Arch Iran Med, doi:10.34172/aim.2021.63
Azadnajafabad, Moghaddam, Rezaei, Ghasemi, Naderimagham et al., A report on statistics of an online self-screening platform for COVID-19 and its effectiveness in Iran, Int J Health Policy Manag, doi:10.34172/ijhpm.2020.252
Bansal, Mahapure, Bhurwal, Gupta, Hassanain et al., Mortality benefit of Remdesivir in COVID-19: a systematic review and meta-analysis, Front Med, doi:10.3389/fmed.2020.606429
Beigel, Tomashek, Dodd, Mehta, Zingman et al., Remdesivir for the treatment of Covid-19, N Engl J Med, doi:10.1056/NEJMoa2007764
Best, Kong, Kaplan-Lewis, Brawley, Baden et al., Treatment patterns in US patients hospitalized with COVID-19 and pulmonary involvement, J Med Virol, doi:10.1002/jmv.27049
Biswas, Rahaman, Biswas, Haque, Association of sex, age, and comorbidities with mortality in COVID-19 patients: a systematic review and metaanalysis, Intervirology, doi:10.1159/000512592
Castelnuovo, Costanzo, Antinori, Berselli, Blandi et al., Heparin in COVID-19 patients is associated with reduced in-hospital mortality: the multicenter Italian CORIST study, Thromb Haemost, doi:10.1055/a-1347-6070
Damiri, Shojaee, Dehghani, Shahali, Abbasi et al., National geographical pattern of COVID-19 hospitalization, case fatalities, and associated factors in patients covered by Iran health insurance organization, BMC Public Health, doi:10.1186/s12889-022-13649-0
Davari, Haycox, Walley, The Iranian health insurance system; past experiences, present challenges and future strategies, Iran J Public Health
Ebrahimoghli, Janati, Sadeghi-Bazargani, Hamishehkar, Chronic diseases and multimorbidity in Iran: a study protocol for the use of Iranian health insurance organization's claims database to understand epidemiology, health service utilization, and patient costs, Health Services Outcomes Res Methodol, doi:10.1007/s10742-020-00232-6
Fang, Karakiulakis, Roth, Are patients with hypertension and diabetes mellitus at increased risk for COVID-19 infection?, Lancet Respir Med, doi:10.1016/S2213-2600(20)30116-8
Gbd, Health system performance in Iran: a systematic analysis for the global burden of disease study 2019, Lancet, doi:10.1016/S0140-6736(21)02751-3
Ghosh, Bornman, Zafer, Antimicrobial resistance threats in the emerging COVID-19 pandemic: where do we stand?, J Infect Public Health, doi:10.1016/j.jiph.2021.02.011
Grundeis, Ansems, Dahms, Thieme, Metzendorf et al., Remdesivir for the treatment of COVID-19, Cochrane Database Syst Rev, doi:10.1002/14651858.CD014962.pub2
Gyselinck, Janssens, Verhamme, Vos, Rationale for azithromycin in COVID-19: an overview of existing evidence, BMJ open. Respir Res, doi:10.1136/bmjresp-2020-000806
Hashemi-Meshkini, Koochak, Nikfar, Rezaei-Darzi, Yaghoubifard, Evaluation of COVID-19 treatments in Iran in comparison with local therapeutic recommendations: a population-level study on utilization and costs of prescription drugs, J Res Pharmacy Pract, doi:10.4103/jrpp.jrpp_6_22
Heidari, Sayfouri, Jafari, Consecutive waves of COVID-19 in Iran: various dimensions and probable causes, Disaster Med Public Health Prep, doi:10.1017/dmp.2022.141
Jeon, Seon, Park, Oh, Analysis of risk factors on readmission cases of COVID-19 in the Republic of Korea: using Nationwide health claims data, Int J Environ Res Public Health, doi:10.3390/ijerph17165844
Johns, George, Taburyanskaya, Poon, A review of the evidence for corticosteroids in COVID-19, J Pharm Pract, doi:10.1177/0897190021998502
Keykhaei, Koolaji, Mohammadi, Kalantar, Moghaddam et al., Dissection of non-pharmaceutical interventions implemented by Iran, South Korea, and Turkey in the fight against COVID-19 pandemic, J Diabetes Metab Disord, doi:10.1007/s40200-021-00877-1
Lai, Chen, Ko, Hsueh, Increased antimicrobial resistance during the COVID-19 pandemic, Int J Antimicrob Agents, doi:10.1016/j.ijantimicag.2021.106324
Lee, Yoon, Jang, Lee, Renin-angiotensin system blocker and outcomes of COVID-19: a systematic review and meta-analysis, Thorax, doi:10.1136/thoraxjnl-2020-215322
Levy, Iba, Olson, Corey, Ghadimi et al., COVID-19: thrombosis, thromboinflammation, and anticoagulation considerations, Int J Lab Hematol, doi:10.1111/ijlh.13500
Li, Yang, Yan, Sun, Zeng et al., Metformin in patients with COVID-19: a systematic review and meta-analysis, Front Med, doi:10.3389/fmed.2021.809134
Liu, Wen, Lei, Jiang, Clinical characteristics and antibiotics treatment in suspected bacterial infection patients with COVID-19, Int Immunopharmacol, doi:10.1016/j.intimp.2020.107157
Lohr, Use of insurance claims data in measuring quality of care, Int J Technol Assess Health Care, doi:10.1017/S0266462300000787
Malekpour, Abbasi-Kangevari, Shojaee, Moghaddam, Ghamari et al., Effect of the chronic medication use on outcome measures of hospitalized COVID-19 patients: evidence from big data, Front Public Health, doi:10.3389/fpubh.2023.1061307
Mattos-Silva, Felix, Silva, Robba, Battaglini et al., Pros and cons of corticosteroid therapy for COVID-19 patients, Respir Physiol Neurobiol, doi:10.1016/j.resp.2020.103492
Mehta, An, Andersen, Mansour, Madhira et al., Use of hydroxychloroquine, remdesivir, and dexamethasone among adults hospitalized with COVID-19 in the United States: a retrospective cohort study, Ann Intern Med, doi:10.7326/M21-0857
Meng, Xiao, Zhang, He, Ou et al., Renin-angiotensin system inhibitors improve the clinical outcomes of COVID-19 patients with hypertension, Emerg Microbes Infect, doi:10.1080/22221751.2020.1746200
Mustafa, Kow, Salman, Kanwal, Riaz et al., Pattern of medication utilization in hospitalized patients with COVID-19 in three District Headquarters hospitals in the Punjab province of Pakistan, Explor Res Clin Soc Pharm, doi:10.1016/j.rcsop.2021.100101
Ortiz-Prado, Izquierdo-Condoy, Mora, Vasconez-Gonzalez, Fernandez-Naranjo, Poor regulation, desperation, and misinformation, a countrywide analysis of self-medication and prescription patterns in Ecuador during the COVID-19 pandemic, Res Soc Adm Pharm, doi:10.1016/j.sapharm.2023.08.011
Pilia, Belletti, Fresilli, Finco, Landoni, Efficacy and safety of heparin full-dose anticoagulation in hospitalized non-critically ill COVID-19 patients: a metaanalysis of multicenter randomized controlled trials, J Thromb Thrombolysis, doi:10.1007/s11239-022-02681-x
Pilia, Belletti, Fresilli, Lee, Zangrillo et al., The effect of heparin full-dose anticoagulation on survival of hospitalized, non-critically ill COVID-19 patients: a meta-analysis of high quality studies, Lung, doi:10.1007/s00408-023-00599-6
Pinte, Ceasovschih, Niculae, Stoichitoiu, Ionescu et al., Antibiotic prescription and in-hospital mortality in COVID-19: a prospective multicentre cohort study, J Pers Med, doi:10.3390/jpm12060877
Qian, Li, Peng, Gao, Cai et al., Association between hypertension and prognosis of patients with COVID-19: a systematic review and meta-analysis, Clin Exp Hypertens, doi:10.1080/10641963.2022.2071914
Salah, Naser, Calcaterra, Bassareo, Mehta, The effect of anticoagulation use on mortality in COVID-19 infection, Am J Cardiol, doi:10.1016/j.amjcard.2020.08.005
Sieswerda, De Boer, Bonten, Boersma, Jonkers et al., Recommendations for antibacterial therapy in adults with COVID-19 -an evidence based guideline, Clin Microbiol Infect, doi:10.1016/j.cmi.2020.09.041
Sivaloganathan, Ladikou, Chevassut, COVID-19 mortality in patients on anticoagulants and antiplatelet agents, Br J Haematol, doi:10.1111/bjh.16968
Sultana, Cutroneo, Crisafulli, Puglisi, Caramori et al., Azithromycin in COVID-19 patients: pharmacological mechanism, clinical evidence and prescribing guidelines, Drug Saf, doi:10.1007/s40264-020-00976-7
Torner, The end of COVID-19 public health emergency of international concern (PHEIC): and now what? Vacunas, doi:10.1016/j.vacun.2023.05.002
Valladales-Restrepo, Correa, Bs, Constain-Mosquera, Sabogal-Ortiz et al., Prescription patterns of drugs given to hospitalized COVID-19 patients: a cross-sectional study in Colombia, Antibiotics, doi:10.3390/antibiotics11030333
Wallace, Cirillo, Ryan, Krigbaum, Badathala et al., Association of the patterns of use of medications with mortality of COVID-19 infection: a hospital-based observational study, BMJ Open, doi:10.1136/bmjopen-2021-050051
Wijaya, Andhika, Huang, The use of therapeutic-dose anticoagulation and its effect on mortality in patients with COVID-19: a systematic review, Clin Appl Thromb Hemost, doi:10.1177/1076029620960797
Wise, Covid-19: WHO declares end of global health emergency
Zeng, Zeng, Yang, Liu, Effectiveness of corticosteroids to treat coronavirus disease 2019 symptoms: a meta-analysis, Med Clin, doi:10.1016/j.medcli.2022.03.013
DOI record:
{
"DOI": "10.3389/fpubh.2023.1280434",
"ISSN": [
"2296-2565"
],
"URL": "http://dx.doi.org/10.3389/fpubh.2023.1280434",
"abstract": "<jats:sec><jats:title>Background</jats:title><jats:p>Different medication prescription patterns have been associated with varying course of disease and outcomes in COVID-19. Health claims data is a rich source of information on disease treatment and outcomes. We aimed to investigate drug prescription patterns and their association with mortality and hospitalization via insurance data for a relatively long period of the pandemic in Iran.</jats:p></jats:sec><jats:sec><jats:title>Methods</jats:title><jats:p>We retrieved hospitalized patients’ data from Iran Health Insurance Organization (IHIO) spanning 26 months (2020–2022) nationwide. Included were patients with ICD-10 codes U07.1/U07.2 for confirmed/suspected COVID-19. A case was defined as a single hospitalization event for an individual patient. Multiple hospitalizations of a patient within a 30-day interval were aggregated into a single case, while hospitalizations with intervals exceeding 30 days were treated as independent cases. The Anatomical Therapeutic Chemical (ATC) was used for medications classification. The two main study outcomes were general and intensive care unit (ICU) hospitalization periods and mortality. Besides, various demographic and clinical associate factors were analyzed to derive the associations with medication prescription patterns and study outcomes using accelerated failure time (AFT) and logistic regression models.</jats:p></jats:sec><jats:sec><jats:title>Results</jats:title><jats:p>During the 26 months of the study period, 1,113,678 admissions with COVID-19 diagnosis at hospitals working in company with IHIO were recorded. 917,198 cases were detected from the database, among which 51.91% were females and 48.09% were males. Among the main groups of medications, antithrombotics (55.84% [95% CI: 55.74–55.94]), corticosteroids (54.14% [54.04–54.24]), and antibiotics (42.22% [42.12–42.32]) were the top used medications among cases with COVID-19. Investigation of the duration of hospitalization based on main medication groups showed antithrombotics (adjusted median ratio = 0.94 [0.94–0.95]) were significantly associated with shorter periods of overall hospitalization. Also, antithrombotics (adjusted odds ratio = 0.74 [95%CI, 0.73–0.76]), corticosteroids (0.97 [0.95–0.99]), antivirals (0.82 [0.80–0.83]), and ACE inhibitor/ARB (0.79 [0.77–0.80]) were significantly associated with lower mortality.</jats:p></jats:sec><jats:sec><jats:title>Conclusion</jats:title><jats:p>Over 2 years of investigation, antithrombotics, corticosteroids, and antibiotics were the top medications for hospitalized patients with COVID-19. Trends in medication prescription varied based on various factors across the country. Medication prescriptions could potentially significantly impact the trends of mortality and hospitalization during epidemics, thereby affecting both health and economic burdens.</jats:p></jats:sec>",
"alternative-id": [
"10.3389/fpubh.2023.1280434"
],
"author": [
{
"affiliation": [],
"family": "Mehrizi",
"given": "Reza",
"sequence": "first"
},
{
"affiliation": [],
"family": "Golestani",
"given": "Ali",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Malekpour",
"given": "Mohammad-Reza",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Karami",
"given": "Hossein",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Nasehi",
"given": "Mohammad Mahdi",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Effatpanah",
"given": "Mohammad",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ranjbaran",
"given": "Hossein",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Shahali",
"given": "Zahra",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Sari",
"given": "Ali Akbari",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Daroudi",
"given": "Rajabali",
"sequence": "additional"
}
],
"container-title": "Frontiers in Public Health",
"container-title-short": "Front. Public Health",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"frontiersin.org"
]
},
"created": {
"date-parts": [
[
2023,
12,
18
]
],
"date-time": "2023-12-18T09:42:21Z",
"timestamp": 1702892541000
},
"deposited": {
"date-parts": [
[
2023,
12,
18
]
],
"date-time": "2023-12-18T09:42:27Z",
"timestamp": 1702892547000
},
"indexed": {
"date-parts": [
[
2023,
12,
19
]
],
"date-time": "2023-12-19T00:33:41Z",
"timestamp": 1702946021750
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2023,
12,
18
]
]
},
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
12,
18
]
],
"date-time": "2023-12-18T00:00:00Z",
"timestamp": 1702857600000
}
}
],
"link": [
{
"URL": "https://www.frontiersin.org/articles/10.3389/fpubh.2023.1280434/full",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1965",
"original-title": [],
"prefix": "10.3389",
"published": {
"date-parts": [
[
2023,
12,
18
]
]
},
"published-online": {
"date-parts": [
[
2023,
12,
18
]
]
},
"publisher": "Frontiers Media SA",
"reference": [
{
"author": "Wise",
"key": "ref1",
"volume-title": "Covid-19: WHO declares end of global health emergency",
"year": "2023"
},
{
"DOI": "10.1016/j.vacun.2023.05.002",
"article-title": "The end of COVID-19 public health emergency of international concern (PHEIC): and now what?",
"author": "Torner",
"doi-asserted-by": "publisher",
"first-page": "164",
"journal-title": "Vacunas",
"key": "ref2",
"volume": "24",
"year": "2023"
},
{
"DOI": "10.1016/S0140-6736(21)02751-3",
"article-title": "Health system performance in Iran: a systematic analysis for the global burden of disease study 2019",
"doi-asserted-by": "publisher",
"first-page": "1625",
"journal-title": "Lancet",
"key": "ref3",
"volume": "399",
"year": "2022"
},
{
"DOI": "10.34172/ijhpm.2020.252",
"article-title": "A report on statistics of an online self-screening platform for COVID-19 and its effectiveness in Iran",
"author": "Azadnajafabad",
"doi-asserted-by": "publisher",
"first-page": "1069",
"journal-title": "Int J Health Policy Manag",
"key": "ref4",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.34172/aim.2021.63",
"article-title": "Non-communicable Diseases' contribution to the COVID-19 mortality: a global warning on the emerging Syndemics",
"author": "Azadnajafabad",
"doi-asserted-by": "publisher",
"first-page": "445",
"journal-title": "Arch Iran Med",
"key": "ref5",
"volume": "24",
"year": "2021"
},
{
"DOI": "10.1007/s40200-021-00877-1",
"article-title": "Dissection of non-pharmaceutical interventions implemented by Iran, South Korea, and Turkey in the fight against COVID-19 pandemic",
"author": "Keykhaei",
"doi-asserted-by": "publisher",
"first-page": "1919",
"journal-title": "J Diabetes Metab Disord",
"key": "ref6",
"volume": "20",
"year": "2021"
},
{
"DOI": "10.1017/dmp.2022.141",
"article-title": "Consecutive waves of COVID-19 in Iran: various dimensions and probable causes",
"author": "Heidari",
"doi-asserted-by": "publisher",
"first-page": "e136",
"journal-title": "Disaster Med Public Health Prep",
"key": "ref7",
"volume": "17",
"year": "2022"
},
{
"DOI": "10.1038/s41598-023-37912-5",
"article-title": "Exploring the clinical benefit of ventilation therapy across various patient groups with COVID-19 using real-world data",
"author": "Abbasi-Kangevari",
"doi-asserted-by": "publisher",
"first-page": "10747",
"journal-title": "Sci Rep",
"key": "ref8",
"volume": "13",
"year": "2023"
},
{
"DOI": "10.1017/S0266462300000787",
"article-title": "Use of insurance claims data in measuring quality of care",
"author": "Lohr",
"doi-asserted-by": "publisher",
"first-page": "263",
"journal-title": "Int J Technol Assess Health Care",
"key": "ref9",
"volume": "6",
"year": "1990"
},
{
"DOI": "10.1007/s10742-020-00232-6",
"article-title": "Chronic diseases and multimorbidity in Iran: a study protocol for the use of Iranian health insurance organization’s claims database to understand epidemiology, health service utilization, and patient costs",
"author": "Ebrahimoghli",
"doi-asserted-by": "publisher",
"first-page": "407",
"journal-title": "Health Services Outcomes Res Methodol",
"key": "ref10",
"volume": "21",
"year": "2021"
},
{
"DOI": "10.4103/jrpp.jrpp_6_22",
"article-title": "Evaluation of COVID-19 treatments in Iran in comparison with local therapeutic recommendations: a population-level study on utilization and costs of prescription drugs",
"author": "Hashemi-Meshkini",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "J Res Pharmacy Pract",
"key": "ref11",
"volume": "11",
"year": "2022"
},
{
"DOI": "10.1016/j.sapharm.2023.08.011",
"article-title": "Poor regulation, desperation, and misinformation, a countrywide analysis of self-medication and prescription patterns in Ecuador during the COVID-19 pandemic",
"author": "Ortiz-Prado",
"doi-asserted-by": "publisher",
"first-page": "1579",
"journal-title": "Res Soc Adm Pharm",
"key": "ref12",
"volume": "19",
"year": "2023"
},
{
"DOI": "10.3390/ijerph17165844",
"article-title": "Analysis of risk factors on readmission cases of COVID-19 in the Republic of Korea: using Nationwide health claims data",
"author": "Jeon",
"doi-asserted-by": "publisher",
"first-page": "5844",
"journal-title": "Int J Environ Res Public Health",
"key": "ref13",
"volume": "17",
"year": "2020"
},
{
"DOI": "10.3389/fpubh.2023.1061307",
"article-title": "Effect of the chronic medication use on outcome measures of hospitalized COVID-19 patients: evidence from big data",
"author": "Malekpour",
"doi-asserted-by": "publisher",
"first-page": "1061307",
"journal-title": "Front Public Health",
"key": "ref14",
"volume": "11",
"year": "2023"
},
{
"DOI": "10.1136/bmjopen-2021-050051",
"article-title": "Association of the patterns of use of medications with mortality of COVID-19 infection: a hospital-based observational study",
"author": "Wallace",
"doi-asserted-by": "publisher",
"first-page": "e050051",
"journal-title": "BMJ Open",
"key": "ref15",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.1016/j.rcsop.2021.100101",
"article-title": "Pattern of medication utilization in hospitalized patients with COVID-19 in three District Headquarters hospitals in the Punjab province of Pakistan",
"author": "Mustafa",
"doi-asserted-by": "publisher",
"first-page": "100101",
"journal-title": "Explor Res Clin Soc Pharm",
"key": "ref16",
"volume": "5",
"year": "2022"
},
{
"DOI": "10.3390/antibiotics11030333",
"article-title": "Prescription patterns of drugs given to hospitalized COVID-19 patients: a cross-sectional study in Colombia",
"author": "Valladales-Restrepo",
"doi-asserted-by": "publisher",
"first-page": "333",
"journal-title": "Antibiotics (Basel)",
"key": "ref17",
"volume": "11",
"year": "2022"
},
{
"article-title": "The Iranian health insurance system; past experiences, present challenges and future strategies",
"author": "Davari",
"first-page": "1",
"journal-title": "Iran J Public Health",
"key": "ref18",
"volume": "41",
"year": "2012"
},
{
"key": "ref19",
"year": ""
},
{
"key": "ref20",
"year": "2019"
},
{
"DOI": "10.1186/s12889-022-13649-0",
"article-title": "National geographical pattern of COVID-19 hospitalization, case fatalities, and associated factors in patients covered by Iran health insurance organization",
"author": "Damiri",
"doi-asserted-by": "publisher",
"first-page": "1274",
"journal-title": "BMC Public Health",
"key": "ref21",
"volume": "22",
"year": "2022"
},
{
"key": "ref22",
"year": "2023"
},
{
"key": "ref23",
"volume-title": "Food and Drug Administration (FDA) 0f Iran - drugs list",
"year": "2023"
},
{
"key": "ref24",
"year": "2023"
},
{
"DOI": "10.7326/M21-0857",
"article-title": "Use of hydroxychloroquine, remdesivir, and dexamethasone among adults hospitalized with COVID-19 in the United States: a retrospective cohort study",
"author": "Mehta",
"doi-asserted-by": "publisher",
"first-page": "1395",
"journal-title": "Ann Intern Med",
"key": "ref25",
"volume": "174",
"year": "2021"
},
{
"DOI": "10.1002/jmv.27049",
"article-title": "Treatment patterns in US patients hospitalized with COVID-19 and pulmonary involvement",
"author": "Best",
"doi-asserted-by": "publisher",
"first-page": "5367",
"journal-title": "J Med Virol",
"key": "ref26",
"volume": "93",
"year": "2021"
},
{
"DOI": "10.1007/s40264-020-00976-7",
"article-title": "Azithromycin in COVID-19 patients: pharmacological mechanism, clinical evidence and prescribing guidelines",
"author": "Sultana",
"doi-asserted-by": "publisher",
"first-page": "691",
"journal-title": "Drug Saf",
"key": "ref27",
"volume": "43",
"year": "2020"
},
{
"DOI": "10.1136/bmjresp-2020-000806",
"article-title": "Rationale for azithromycin in COVID-19: an overview of existing evidence. BMJ open",
"author": "Gyselinck",
"doi-asserted-by": "publisher",
"first-page": "e000806",
"journal-title": "Respir Res",
"key": "ref28",
"volume": "8",
"year": "2021"
},
{
"DOI": "10.1016/j.amjcard.2020.08.005",
"article-title": "The effect of anticoagulation use on mortality in COVID-19 infection",
"author": "Salah",
"doi-asserted-by": "publisher",
"first-page": "155",
"journal-title": "Am J Cardiol",
"key": "ref29",
"volume": "134",
"year": "2020"
},
{
"DOI": "10.1055/a-1347-6070",
"article-title": "Heparin in COVID-19 patients is associated with reduced in-hospital mortality: the multicenter Italian CORIST study",
"author": "Di Castelnuovo",
"doi-asserted-by": "publisher",
"first-page": "1054",
"journal-title": "Thromb Haemost",
"key": "ref30",
"volume": "121",
"year": "2021"
},
{
"DOI": "10.1177/1076029620960797",
"article-title": "The use of therapeutic-dose anticoagulation and its effect on mortality in patients with COVID-19: a systematic review",
"author": "Wijaya",
"doi-asserted-by": "publisher",
"first-page": "1076029620960797",
"journal-title": "Clin Appl Thromb Hemost",
"key": "ref31",
"volume": "26",
"year": "2020"
},
{
"DOI": "10.1111/bjh.16968",
"article-title": "COVID-19 mortality in patients on anticoagulants and antiplatelet agents",
"author": "Sivaloganathan",
"doi-asserted-by": "publisher",
"first-page": "e192",
"journal-title": "Br J Haematol",
"key": "ref32",
"volume": "190",
"year": "2020"
},
{
"DOI": "10.1007/s11239-022-02681-x",
"article-title": "Efficacy and safety of heparin full-dose anticoagulation in hospitalized non-critically ill COVID-19 patients: a meta-analysis of multicenter randomized controlled trials",
"author": "Pilia",
"doi-asserted-by": "publisher",
"first-page": "420",
"journal-title": "J Thromb Thrombolysis",
"key": "ref33",
"volume": "54",
"year": "2022"
},
{
"DOI": "10.1007/s00408-023-00599-6",
"article-title": "The effect of heparin full-dose anticoagulation on survival of hospitalized, non-critically ill COVID-19 patients: a meta-analysis of high quality studies",
"author": "Pilia",
"doi-asserted-by": "publisher",
"first-page": "135",
"journal-title": "Lung",
"key": "ref34",
"volume": "201",
"year": "2023"
},
{
"DOI": "10.1111/ijlh.13500",
"article-title": "COVID-19: thrombosis, thromboinflammation, and anticoagulation considerations",
"author": "Levy",
"doi-asserted-by": "publisher",
"first-page": "29",
"journal-title": "Int J Lab Hematol",
"key": "ref35",
"year": "2021"
},
{
"DOI": "10.3390/jpm12060877",
"article-title": "Antibiotic prescription and in-hospital mortality in COVID-19: a prospective multicentre cohort study",
"author": "Pinte",
"doi-asserted-by": "publisher",
"first-page": "877",
"journal-title": "J Pers Med",
"key": "ref36",
"volume": "12",
"year": "2022"
},
{
"DOI": "10.1016/j.intimp.2020.107157",
"article-title": "Clinical characteristics and antibiotics treatment in suspected bacterial infection patients with COVID-19",
"author": "Liu",
"doi-asserted-by": "publisher",
"first-page": "107157",
"journal-title": "Int Immunopharmacol",
"key": "ref37",
"volume": "90",
"year": "2021"
},
{
"DOI": "10.1016/j.cmi.2020.09.041",
"article-title": "Recommendations for antibacterial therapy in adults with COVID-19 - an evidence based guideline",
"author": "Sieswerda",
"doi-asserted-by": "publisher",
"first-page": "61",
"journal-title": "Clin Microbiol Infect",
"key": "ref38",
"volume": "27",
"year": "2021"
},
{
"DOI": "10.1016/j.ijantimicag.2021.106324",
"article-title": "Increased antimicrobial resistance during the COVID-19 pandemic",
"author": "Lai",
"doi-asserted-by": "publisher",
"first-page": "106324",
"journal-title": "Int J Antimicrob Agents",
"key": "ref39",
"volume": "57",
"year": "2021"
},
{
"DOI": "10.1016/j.jiph.2021.02.011",
"article-title": "Antimicrobial resistance threats in the emerging COVID-19 pandemic: where do we stand?",
"author": "Ghosh",
"doi-asserted-by": "publisher",
"first-page": "555",
"journal-title": "J Infect Public Health",
"key": "ref40",
"volume": "14",
"year": "2021"
},
{
"DOI": "10.1056/NEJMoa2021436",
"article-title": "Dexamethasone in hospitalized patients with Covid-19",
"doi-asserted-by": "publisher",
"first-page": "693",
"journal-title": "N Engl J Med",
"key": "ref41",
"volume": "384",
"year": "2021"
},
{
"DOI": "10.1016/j.medcli.2022.03.013",
"article-title": "Effectiveness of corticosteroids to treat coronavirus disease 2019 symptoms: a meta-analysis",
"author": "Zeng",
"doi-asserted-by": "publisher",
"first-page": "575",
"journal-title": "Med Clin",
"key": "ref42",
"volume": "159",
"year": "2022"
},
{
"DOI": "10.1177/0897190021998502",
"article-title": "A review of the evidence for corticosteroids in COVID-19",
"author": "Johns",
"doi-asserted-by": "publisher",
"first-page": "626",
"journal-title": "J Pharm Pract",
"key": "ref43",
"volume": "35",
"year": "2022"
},
{
"DOI": "10.1016/j.resp.2020.103492",
"article-title": "Pros and cons of corticosteroid therapy for COVID-19 patients",
"author": "Mattos-Silva",
"doi-asserted-by": "publisher",
"first-page": "103492",
"journal-title": "Respir Physiol Neurobiol",
"key": "ref44",
"volume": "280",
"year": "2020"
},
{
"DOI": "10.1056/NEJMoa2007764",
"article-title": "Remdesivir for the treatment of Covid-19",
"author": "Beigel",
"doi-asserted-by": "publisher",
"first-page": "1813",
"journal-title": "N Engl J Med",
"key": "ref45",
"volume": "383",
"year": "2020"
},
{
"DOI": "10.3389/fmed.2020.606429",
"article-title": "Mortality benefit of Remdesivir in COVID-19: a systematic review and meta-analysis",
"author": "Bansal",
"doi-asserted-by": "publisher",
"first-page": "606429",
"journal-title": "Front Med (Lausanne)",
"key": "ref46",
"volume": "7",
"year": "2020"
},
{
"DOI": "10.1016/S0140-6736(22)00519-0",
"article-title": "Remdesivir and three other drugs for hospitalised patients with COVID-19: final results of the WHO solidarity randomised trial and updated meta-analyses",
"doi-asserted-by": "publisher",
"first-page": "1941",
"journal-title": "Lancet",
"key": "ref47",
"volume": "399",
"year": "2022"
},
{
"DOI": "10.1002/14651858.CD014962.pub2",
"article-title": "Remdesivir for the treatment of COVID-19",
"author": "Grundeis",
"doi-asserted-by": "publisher",
"first-page": "Cd014962",
"journal-title": "Cochrane Database Syst Rev",
"key": "ref48",
"volume": "1",
"year": "2023"
},
{
"DOI": "10.1159/000512592",
"article-title": "Association of sex, age, and comorbidities with mortality in COVID-19 patients: a systematic review and meta-analysis",
"author": "Biswas",
"doi-asserted-by": "publisher",
"first-page": "36",
"journal-title": "Intervirology",
"key": "ref49",
"volume": "64",
"year": "2021"
},
{
"DOI": "10.3389/fmed.2021.809134",
"article-title": "Metformin in patients with COVID-19: a systematic review and meta-analysis",
"author": "Li",
"doi-asserted-by": "publisher",
"first-page": "704666",
"journal-title": "Front Med",
"key": "ref50",
"volume": "8",
"year": "2021"
},
{
"DOI": "10.1136/thoraxjnl-2020-215322",
"article-title": "Renin-angiotensin system blocker and outcomes of COVID-19: a systematic review and meta-analysis",
"author": "Lee",
"doi-asserted-by": "publisher",
"first-page": "479",
"journal-title": "Thorax",
"key": "ref51",
"volume": "76",
"year": "2021"
},
{
"DOI": "10.1016/S2213-2600(20)30116-8",
"article-title": "Are patients with hypertension and diabetes mellitus at increased risk for COVID-19 infection?",
"author": "Fang",
"doi-asserted-by": "publisher",
"first-page": "e21",
"journal-title": "Lancet Respir Med",
"key": "ref52",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1080/10641963.2022.2071914",
"article-title": "Association between hypertension and prognosis of patients with COVID-19: a systematic review and meta-analysis",
"author": "Qian",
"doi-asserted-by": "publisher",
"first-page": "451",
"journal-title": "Clin Exp Hypertens",
"key": "ref53",
"volume": "44",
"year": "2022"
},
{
"DOI": "10.1080/22221751.2020.1746200",
"article-title": "Renin-angiotensin system inhibitors improve the clinical outcomes of COVID-19 patients with hypertension",
"author": "Meng",
"doi-asserted-by": "publisher",
"first-page": "757",
"journal-title": "Emerg Microbes Infect",
"key": "ref54",
"volume": "9",
"year": "2020"
},
{
"DOI": "10.3390/cells9071652",
"article-title": "COVID-19, renin-angiotensin system and endothelial dysfunction",
"author": "Amraei",
"doi-asserted-by": "publisher",
"first-page": "1652",
"journal-title": "Cells",
"key": "ref55",
"volume": "9",
"year": "2020"
}
],
"reference-count": 55,
"references-count": 55,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.frontiersin.org/articles/10.3389/fpubh.2023.1280434/full"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Public Health, Environmental and Occupational Health"
],
"subtitle": [],
"title": "Drug prescription patterns and their association with mortality and hospitalization duration in COVID-19 patients: insights from big data",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.3389/crossmark-policy",
"volume": "11"
}
mehrizi