Pentoxifylline decreases serum LDH levels and increases lymphocyte count in COVID-19 patients: Results from an external pilot study
et al., International Immunopharmacology, doi:10.1016/j.intimp.2020.107209, Jan 2021
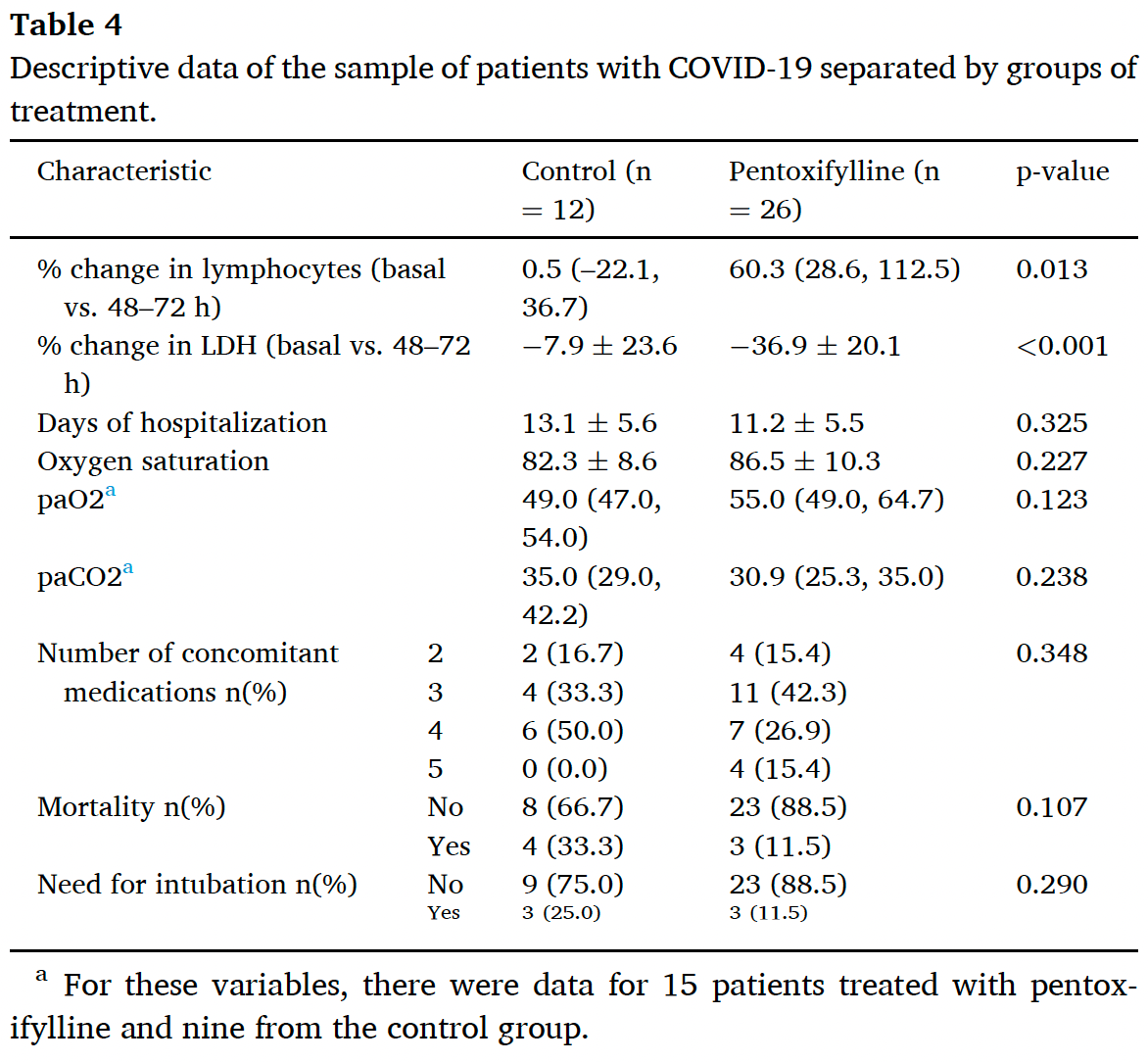
Pilot study of 38 hospitalized COVID-19 patients in Mexico showing pentoxifylline treatment was associated with significantly increased lymphocyte count and decreased LDH levels compared to standard care. The pentoxifylline group (400mg three times daily from admission to discharge) showed trends toward reduced days of hospitalization, lower mortality, and less need for intubation, though these differences did not reach statistical significance. Authors suggest pentoxifylline may help restore immune response equilibrium and reduce tissue damage in COVID-19 through its anti-inflammatory properties and effects on the renin-angiotensin system.
|
risk of death, 65.4% lower, RR 0.35, p = 0.18, treatment 3 of 26 (11.5%), control 4 of 12 (33.3%), NNT 4.6.
|
|
risk of mechanical ventilation, 53.8% lower, RR 0.46, p = 0.36, treatment 3 of 26 (11.5%), control 3 of 12 (25.0%), NNT 7.4.
|
|
hospitalization time, 14.5% lower, relative time 0.85, p = 0.33, treatment mean 11.2 (±5.5) n=26, control mean 13.1 (±5.6) n=12.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Maldonado et al., 31 Jan 2021, Randomized Controlled Trial, Mexico, peer-reviewed, median age 55.3, 9 authors, study period July 2020 - August 2020.
Contact: valentemaldonado@lasallistas.org.mx.
Pentoxifylline decreases serum LDH levels and increases lymphocyte count in COVID-19 patients: Results from an external pilot study
International Immunopharmacology, doi:10.1016/j.intimp.2020.107209
We have previously hypothesized that pentoxifylline could be beneficial for the treatment of COVID-19 given its potential to restore the immune response equilibrium, reduce the impact of the disease on the endothelium and alveolar epithelial cells, and improve the circulatory function. Serum lactate dehydrogenase (LDH) and lymphocyte count are accessible biomarkers that correlate with the severity of COVID-19, the need for hospitalization, and mortality, reflecting the host immune response's contribution to the seriousness of SARS-CoV-2 infection. We carried out this external pilot study on 38 patients with moderate and severe COVID-19 to test the effect pentoxifylline on parameters such as LDH, lymphocyte count, days of hospitalization, mortality, and proportion of patients requiring intubation. Twenty-six patients were randomized to receive 400 mg of pentoxifylline t.i.d. plus standard therapy (pentoxifylline group), while the rest received the standard treatment (control group). Linear regression models were built for statistically significant parameters. Pentoxifylline treatment was associated with a 64.25% increase (CI95% 11.83, 116.68) in lymphocyte count and a 29.61% decrease (CI95% 15.11, 44.10) in serum LDH. Although a trend towards reduced days of hospitalization, mortality, and proportion of patients requiring intubation was observed, no statistically significant difference was found for these parameters. Our findings open the possibility of pentoxifylline being repositioned as a drug for COVID-19 treatment with the advantages of a proven safety profile, availability, and no risk of immunosuppression; however, this evidence needs to be confirmed in a pragmatic randomized controlled trial.
Declaration of Competing Interest The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
Ackermann, Verleden, Kuehnel, Pulmonary Vascular Endothelialitis, Thrombosis, and Angiogenesis in Covid-19, N. Engl. J. Med, doi:10.1056/NEJMoa2015432
Adamzik, Broll, Steinmann, An increased alveolar CD4+CD25+ Foxp3+T regulatory cell ratio in acute respiratory distress syndrome is associated with increased 30-day mortality, Intensive Care Med
Azhar, El-Bassossy, Pentoxifylline alleviates hypertension in metabolic syndrome: effect on low-grade inflammation and angiotensin system, J. Endocrinol. Invest, doi:10.1007/s40618-014-0209-z
Bengsch, Martin, Thimme, Restoration of HBV-specific CD8+ T cell function by PD-1 blockade in inactive carrier patients is linked to T cell differentiation, J. Hepatol, doi:10.1016/j.jhep.2014.07.005
Berman, Duncan, Pentoxifylline inhibits normal human dermal fibroblast in vitro proliferation, collagen, glycosaminoglycan, and fibronectin production, and increases collagenase activity, J. Invest. Dermatol
Bogoch, Watts, Thomas-Bachli, Potential for global spread of a novel coronavirus from China, J. Travel Med
Brie, Sahebkar, Penson, Effects of pentoxifylline on inflammatory markers and blood pressure: a systematic review and meta-analysis of randomized controlled trials, J. Hypertens, doi:10.1097/HJH.0000000000001086
Caricchio, Gallucci, Dass, Zhang, Gallucci et al., Preliminary predictive criteria for COVID-19 cytokine storm, Ann. Rheum. Dis, doi:10.1136/annrheumdis-2020-218323
Chen, Wu, Chen, Yan, Yang et al., Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study, BMJ
Chen, Wu, Guo, Clinical and immunological features of severe and moderate coronavirus disease 2019, J. Clin. Invest, doi:10.1172/JCI137244
Cheng, Grande, Cyclic nucleotide phosphodiesterase (PDE) inhibitors: novel therapeutic agents for progressive renal disease, Exp. Biol. Med
Crommelin, Vorselaars, Van Moorsel, Korenromp, Deneer et al., Anti-TNF therapeutics for the treatment of sarcoidosis, Immunotherapy, doi:10.2217/imt.14.65
D'alessio, Tsushima, Aggarwal, CD4+CD25+Foxp3+ Tregs resolve experimental lung injury in mice and are present in humans with acute lung injury, J. Clin. Invest
Delanian, Porcher, Balla-Mekias, Lefaix, Randomized, placebocontrolled trial of combined pentoxifylline and tocopherol for regression of superficial radiation-induced fibrosis, J. Clin. Oncol
Deremee, Serum lactic dehydrogenase activity and diffuse interstitial pneumonitis, JAMA
Diao, Wang, Tan, Chen, Liu et al., Reduction and functional exhaustion of T cells in patients with coronavirus disease 2019, Front. Immunol
Diao, Wang, Tan, Reduction and functional exhaustion of T cells in patients with coronavirus disease 2019 (COVID-19), Front. Immunol, doi:10.3389/fimmu.2020.00827
Drent, Cobben, Henderson, Wouters, Van Dieijen-Visser, Usefulness of lactate dehydrogenase and its isoenzymes as indicators of lung damage or inflammation, Eur. Respir. J, doi:10.1183/09031936.96.09081736
Duncan, Hasan, Berman, Pentoxifylline, pentifylline, and interferons decrease type I and III procollagen mRNA levels in dermal fibroblasts: evidence for mediation by nuclear factor 1 down-regulation, J. Invest. Dermatol
Fan, Chong, Chan, Hematologic parameters in patients with COVID-19 infection, Am. J. Hematol
Fathi, Rezaei, Lymphopenia in COVID-19: Therapeutic opportunities, Cell Biol. Int, doi:10.1002/cbin.11403
Fernandez, Torres, Miro, Prognostic factors influencing the outcome in Pneumocystis carinii pneumonia in patients with AIDS, Thorax
Ferrari, Motta, Strollo, Banfi, Locatelli, Routine blood tests as a potential diagnostic tool for COVID-19, Clin. Chem. Lab. Med, doi:10.1515/cclm-2020-0398
Fischer, Inhibitory effect of tumor cell-derived lactic acid on human T cells, Blood
Frater, Zini, Onofrio, Rogers, COVID-19 and the clinical hematology laboratory, Int. J. Lab. Hematol, doi:10.1111/ijlh.13229
Frigolet, Torres, Tovar, The renin-angiotensin system in adipose tissue and its metabolic consequences during obesity, J. Nutr. Biochem
Glick, Serum lactate dehydrogenase isoenzyme and total lactate dehydrogenase values in health and disease, and clincal evaluation of these test by means of discriminant analysis, Am. J. Clin. Pathol
Guan, Ni, Hu, Liang, Ou et al., China Medical Treatment Expert Group for Covid-19, Clinical Characteristics of Coronavirus Disease 2019 in China, N. Engl. J. Med, doi:10.1056/NEJMoa2002032
Han, Zhang, Mu, Wei, Jin et al., Lactate dehydrogenase, an independent risk factor of severe COVID-19 patients: a retrospective and observational study, Aging, doi:10.18632/aging.103372
Hanania, Mainwaring, Ghebre, Hanania, Ludwig, Radiationinducedlung injury: assessment and management, Chest, doi:10.1016/j.chest.2019.03.033
Harris, Schulzke, Patole, Pentoxifylline in preterm neonates: a systematic review, Paediatric Drugs
Hendry, Stafford, Arnold, Sangwaiya, Manglam et al., Hypothesis: Pentoxifylline is a potential cytokine modulator therapeutic in COVID-19 patients, Pharmacol. Res. Perspect, doi:10.1002/prp2.631.PMID:32715661;PMCID:PMC7383088
Hirano, Murakami, COVID-19: A New Virus, but a Familiar Receptor and Cytokine Release Syndrome, Immunity, doi:10.1016/j.immuni.2020.04.003
Hoffman, Rogers, Serum and lavage lactate dehydrogenase isoenzymes in pulmonary alveolar proteinosis, Am. Rev. Respir. Dis
Huang, Wang, Li, Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China, Lancet
Jamaluddin, Meng, Sun, Boldogh, Han et al., Angiotensin II induces nuclear factor (NF)-κB1 isoforms to bind the angiotensinogen gene acute phase response element: a stimulus-specific pathway for NF-κB activation, Mol. Endocrinol
Jurisic, Radenkovic, Konjevic, The Actual Role of LDH as Tumor Marker, Biochemical and Clinical Aspects, Adv. Exp. Med. Biol, doi:10.1007/978-94-017-7215-0_8
Kang, Wang, Yang, Elks, Cardinale et al., TNF-α in hypothalamic paraventricular nucleus contributes to sympathoexcitation in heart failure by modulating AT1 receptor and neurotransmitters, Tohoku J. Exp. Med, doi:10.1620/tjem.222.251
Kermali, Khalsa, Pillai, Ismail, Harky, The role of biomarkers in diagnosis of COVID-19 -A systematic review, Life Sci, doi:10.1016/j.lfs.2020.117788
Krugten Van, Cobben, Lamers, Serum LDH: a marker of disease activity and its response to therapy in idiopathic pulmonary fibrosis, Neth. J. Med
Lan, Ge, Yu, Shan, Zhou et al., Structure of the SARS-CoV-2 spike receptor-binding domain bound to the ACE2 receptor, Nature
Lancaster, Dodd, Williamson, Design and analysis of pilot studies: recommendations for good practice, J. Eval. Clin. Pract, doi:10.1111/j.2002.384.doc.x
Lauterbach, Zembala, Pentoxifylline reduces plasma tumour necrosis factoralpha concentration in premature infants with sepsis, Eur. J. Pediatr
Lee, Shim, Kim, Pentoxifylline regulates plasminogen activator inhibitor-1 expression and protein kinase A phosphorylation in radiation-induced lung fibrosis, Biomed. Res. Int, doi:10.1155/2017/1279280
Li, Hu, Sun, Tu, Gong et al., Resolution acute respiratory distress syndrome through reversing the imbalance of Treg/Th17 by targeting the cAMP signaling pathway, Mol. Med. Rep, doi:10.3892/mmr.2016.5222
Liao, IL-19 induces production of IL-6 and TNF-alpha and results in cell apoptosis through TNF-alpha, J. Immunol
Lin, Chen, Chen, Pentoxifylline attenuates tubulointerstitial fibrosis by blocking Smad3/4-activated transcription and profibrogenic effects of connective tissue growth factor, J. Am. Soc. Nephrol
Lindy, Kahanpää, Karhunen, Halme, Uitto, Lactate dehydrogenase isoenzymes during the development of experimental fibrosis, J. Lab. Clin. Med
Lippi, Plebani, Laboratory abnormalities in patients with COVID-2019 infection, Clin. Chem. Lab. Med
Lippi, Plebani, The critical role of laboratory medicine during coronavirus disease 2019 (COVID-19) and other viral outbreaks, Clin. Chem. Lab. Med, doi:10.1515/cclm-2020-0240
Loskutoff, Quigley, PAI-1, fibrosis, and the elusive provisional fibrin matrix, J. Clin. Invest
Lott, Nemensanszky, Lactate dehydrogenase
Lugnier, Cyclic nucleotide phosphodiesterase (PDE) superfamily: a new target for the development of specific therapeutic agents, Pharmacol. Ther
Maldonado, Loza-Mejía, Chávez-Alderete, Repositioning of pentoxifylline as an immunomodulator and regulator of the renin-angiotensin system in the treatment of COVID-19, Med Hypotheses, doi:10.1016/j.mehy.2020.109988
Marques, Zheng, Poulakis, Guzman, Costabel, Pentoxifylline inhibits TNF-alpha production from human alveolar macrophages, Am. J. Respir. Crit. Care Med
Matusiewicz, Williamson, Sime, Plasma lactate dehydrogenase: a marker of disease activity in cryptogenic fibrosing alveolitis and extrinsic allergic alveolitis?, Eur. Respir. J
Meng, Xiao, Zhang, He, Ou et al., Reninangiotensin system inhibitors improve the clinical outcomes of COVID-19 patients with hypertension, Emerg. Microbes Infect
Mo, Xing, Xiao, Deng, Zhao et al., Clinical characteristics of refractory COVID-19 pneumonia in Wuhan, China, Clin. Infect. Dis, doi:10.1093/cid/ciaa270
Moss, Henderson, Enzymes
Muldowney, Chen, Blakemore, Vaughan, Pentoxifylline lowers plasminogen activator inhibitor 1 levels in obese individuals: a pilot study, Angiology
Murakami, Kamimura, Hirano, Pleiotropy and specificity: insights from the interleukin 6 family of cytokines, Immunity
Ozturk, Egehan, Atavci, Kitapci, Pentoxifylline in prevention of radiation induced lung toxicity in patients with breast and lung cancer: a double-blind randomized trial, Int. J. Radiat. Oncol. Biol. Phys
Park, Fontana, Babaali, Steroid-sparing effects of pentoxifylline in pulmonary sarcoidosis, Sarcoidosis, Vasc. Diffuse Lung Dis
Pierrakos, Karanikolas, Scolletta, Karamouzos, Velissaris, Acute respiratory distress syndrome: Pathophysiology and therapeutic options, J. Clin. Med. Res
Qin, Zhou, Hu, Dysregulation of immune response in patients with coronavirus 2019 (COVID-19) in Wuhan, China, Clin. Infect. Dis, doi:10.1093/cid/ciaa248
Quist, Hill, Serum lactate dehydrogenase (LDH) in Pneumocystis carinii pneumonia, tuberculosis and bacterial pneumonia, Chest
Raetsch, Jia, Boigk, Pentoxifylline downregulates profibrogenic cytokines and procollagen I expression in rat secondary biliary fibrosis, Gut
Ruan, Yang, Wang, Jiang, Song, Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China, Intensive Care Med, doi:10.1007/s00134-020-05991-x.publishedMarch3.[PMCfreearticle][PubMed][CrossRef][GoogleScholar
Ruiz-Ortega, Lorenzo, Suzuki, Rupérez, Egido, Proinflammatory actions of angiotensins, Curr. Opin. Nephrol. Hypertens
Schietinger, Greenberg, Tolerance and exhaustion: defining mechanisms of T cell dysfunction, Trends Immunol, doi:10.1016/j.it.2013.10.001
Skurk, Van Harmelen, Hauner, Angiotensin II stimulates the release of interleukin-6 and interleukin-8 from cultured human adipocytes by activation of NF-κB, Arterioscler. Thromb. Vasc. Biol
Smith, Ripps, Lewis, Elevated lactate dehydrogenase values in patients with Pneumocystis carinii pneumonia, Chest
Tan, Wang, Zhang, Ding, Huang et al., Lymphopenia predicts disease severity of COVID-19: A descriptive and predictive study, Signal Transduction and Targeted, Therapy, doi:10.1038/s41392-020-0148-4
Thevarajan, Nguyen, Koutsakos, Druce, Caly et al., Breadth of concomitant immune responses prior to patient recovery: A case report of non-severe COVID-19, Nat. Med, doi:10.1038/s41591-020-0819-2
Tisoncik, Korth, Simmons, Farrar, Martin et al., Into the eye of the cytokine storm, Microbiol. Mol. Biol. Rev, doi:10.1128/MMBR.05015-11.PMID:22390970;PMCID:PMC3294426
Tong, Dai, Chen, Abdoh, Guzman et al., Inhibition of cytokine release from alveolar macrophages in pulmonary sarcoidosis by pentoxifylline: comparison with dexamethasone, Chest
Vaduganathan, Vardeny, Michel, Mcmurray, Pfeffer et al., Renin-Angiotensin-Aldosterone System Inhibitors in Patients with Covid-19, N. Engl. J. Med, doi:10.1056/NEJMsr2005760
Valente, Vernet, Ferrini, L-arginine and phosphodiesterase (PDE) inhibitors counteract fibrosis in the Peyronie's fibrotic plaque and related fibroblast cultures, Nitric Oxide
Vilcek, Lee, Tumor necrosis factor. New insights into the molecular mechanisms of its multiple actions, J. Biol. Chem
Wang, Hu, Hu, Zhu, Liu et al., Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China, JAMA, doi:10.1001/jama.2020.1585.PMID:32031570;PMCID:PMC7042881
Ward, Sp, Pentoxifylline, A review of its pharmacodynamic and pharmacokinetic properties, and its therapeutic efficacy, Drugs, doi:10.2165/00003495-198734010-00003
Xiong, Sun, Liu, Fan, Zhao et al., Clinical and High-Resolution CT Features of the COVID-19 Infection: Comparison of the Initial and Follow-up Changes, Invest. Radiol, doi:10.1097/RLI.0000000000000674.PMID:32134800;PMCID:PMC7147282
Xu, High expression of ACE2 receptor of 2019-nCoV on the epithelial cells of oral mucosa, Int. J. Oral. Sci
Yang, Yu, Xu, Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study, Lancet Respir. Med, doi:10.1016/S2213-2600(20)30079-5.publishedonlineFeb24.[PMCfreearticle][PubMed][CrossRef][GoogleScholar
Yu, Ji, Yan, Cai, Liu et al., The ratio of Th17/Treg cells as a risk indicator in early acute respiratory distress syndrome, Crit. Care, doi:10.1186/s13054-015-0811-2.PMID:25887535;PMCID:PMC4355972
Zabel, Entzian, Dalhoff, Schlaak, Pentoxifylline in treatment of sarcoidosis, Am. J. Respir. Crit. Care Med
Zheng, Zhang, Yang, Zhang, Wang et al., Elevated exhaustion levels and reduced functional diversity of T cells in peripheral blood may predict severe progression in COVID-19 patients, Cell. Mol. Immunol, doi:10.1038/s41423-020-0401
DOI record:
{
"DOI": "10.1016/j.intimp.2020.107209",
"ISSN": [
"1567-5769"
],
"URL": "http://dx.doi.org/10.1016/j.intimp.2020.107209",
"alternative-id": [
"S1567576920336766"
],
"article-number": "107209",
"assertion": [
{
"label": "This article is maintained by",
"name": "publisher",
"value": "Elsevier"
},
{
"label": "Article Title",
"name": "articletitle",
"value": "Pentoxifylline decreases serum LDH levels and increases lymphocyte count in COVID-19 patients: Results from an external pilot study"
},
{
"label": "Journal Title",
"name": "journaltitle",
"value": "International Immunopharmacology"
},
{
"label": "CrossRef DOI link to publisher maintained version",
"name": "articlelink",
"value": "https://doi.org/10.1016/j.intimp.2020.107209"
},
{
"label": "Content Type",
"name": "content_type",
"value": "article"
},
{
"label": "Copyright",
"name": "copyright",
"value": "© 2020 Elsevier B.V. All rights reserved."
}
],
"author": [
{
"affiliation": [],
"family": "Maldonado",
"given": "Valente",
"sequence": "first"
},
{
"affiliation": [],
"family": "Hernandez-Ramírez",
"given": "Claudia",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Oliva-Pérez",
"given": "Eniel Alonso",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Sánchez-Martínez",
"given": "César Omar",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Pimentel-González",
"given": "Jorge Fabián",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Molina-Sánchez",
"given": "José Raúl",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Jiménez-Villalba",
"given": "Yeimmy Zuyenn",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Chávez-Alderete",
"given": "Jaime",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Loza-Mejía",
"given": "Marco A.",
"sequence": "additional"
}
],
"container-title": "International Immunopharmacology",
"container-title-short": "International Immunopharmacology",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"elsevier.com",
"sciencedirect.com"
]
},
"created": {
"date-parts": [
[
2020,
11,
26
]
],
"date-time": "2020-11-26T11:16:04Z",
"timestamp": 1606389364000
},
"deposited": {
"date-parts": [
[
2025,
4,
18
]
],
"date-time": "2025-04-18T04:30:11Z",
"timestamp": 1744950611000
},
"indexed": {
"date-parts": [
[
2025,
5,
2
]
],
"date-time": "2025-05-02T17:50:56Z",
"timestamp": 1746208256068,
"version": "3.40.4"
},
"is-referenced-by-count": 16,
"issued": {
"date-parts": [
[
2021,
1
]
]
},
"language": "en",
"license": [
{
"URL": "https://www.elsevier.com/tdm/userlicense/1.0/",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
1,
1
]
],
"date-time": "2021-01-01T00:00:00Z",
"timestamp": 1609459200000
}
},
{
"URL": "https://www.elsevier.com/legal/tdmrep-license",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
1,
1
]
],
"date-time": "2021-01-01T00:00:00Z",
"timestamp": 1609459200000
}
},
{
"URL": "https://doi.org/10.15223/policy-017",
"content-version": "stm-asf",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
1,
1
]
],
"date-time": "2021-01-01T00:00:00Z",
"timestamp": 1609459200000
}
},
{
"URL": "https://doi.org/10.15223/policy-037",
"content-version": "stm-asf",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
1,
1
]
],
"date-time": "2021-01-01T00:00:00Z",
"timestamp": 1609459200000
}
},
{
"URL": "https://doi.org/10.15223/policy-012",
"content-version": "stm-asf",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
1,
1
]
],
"date-time": "2021-01-01T00:00:00Z",
"timestamp": 1609459200000
}
},
{
"URL": "https://doi.org/10.15223/policy-029",
"content-version": "stm-asf",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
1,
1
]
],
"date-time": "2021-01-01T00:00:00Z",
"timestamp": 1609459200000
}
},
{
"URL": "https://doi.org/10.15223/policy-004",
"content-version": "stm-asf",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
1,
1
]
],
"date-time": "2021-01-01T00:00:00Z",
"timestamp": 1609459200000
}
}
],
"link": [
{
"URL": "https://api.elsevier.com/content/article/PII:S1567576920336766?httpAccept=text/xml",
"content-type": "text/xml",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://api.elsevier.com/content/article/PII:S1567576920336766?httpAccept=text/plain",
"content-type": "text/plain",
"content-version": "vor",
"intended-application": "text-mining"
}
],
"member": "78",
"original-title": [],
"page": "107209",
"prefix": "10.1016",
"published": {
"date-parts": [
[
2021,
1
]
]
},
"published-print": {
"date-parts": [
[
2021,
1
]
]
},
"publisher": "Elsevier BV",
"reference": [
{
"DOI": "10.1093/jtm/taaa011",
"article-title": "Potential for global spread of a novel coronavirus from China",
"author": "Bogoch",
"doi-asserted-by": "crossref",
"issue": "2",
"journal-title": "J. Travel Med.",
"key": "10.1016/j.intimp.2020.107209_b0005",
"volume": "27",
"year": "2020"
},
{
"key": "10.1016/j.intimp.2020.107209_b0010",
"unstructured": "World Health Organization (2020) Coronavirus disease 2019 (COVID-19) situation report–39. World Health Organization, Geneva. Available via https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200228-sitrep-39-covid-19.pdf?sfvrsn=5bbf3e7d_2. Accessed 3 Mar 2020."
},
{
"key": "10.1016/j.intimp.2020.107209_b0015",
"unstructured": "World Health Organization (2020) Coronavirus disease 2019 (COVID-19) situation report–209. World Health Organization, Geneva. Available via https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200228-sitrep-39-covid-19.pdf?sfvrsn=5bbf3e7d_2. Accessed 21 agosto 2020."
},
{
"DOI": "10.1056/NEJMoa2002032",
"article-title": "Clinical Characteristics of Coronavirus Disease 2019 in China",
"author": "Guan",
"doi-asserted-by": "crossref",
"first-page": "1708",
"issue": "18",
"journal-title": "N. Engl. J. Med.",
"key": "10.1016/j.intimp.2020.107209_b0020",
"volume": "382",
"year": "2020"
},
{
"DOI": "10.1016/S0140-6736(20)30183-5",
"article-title": "Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China",
"author": "Huang",
"doi-asserted-by": "crossref",
"first-page": "497",
"issue": "10223",
"journal-title": "Lancet.",
"key": "10.1016/j.intimp.2020.107209_b0025",
"volume": "395",
"year": "2020"
},
{
"article-title": "Lymphopenia predicts disease severity of COVID-19: A descriptive and predictive study. Signal Transduction and Targeted",
"author": "Tan",
"issue": "33",
"journal-title": "Therapy",
"key": "10.1016/j.intimp.2020.107209_b0030",
"volume": "5",
"year": "2020"
},
{
"DOI": "10.1111/ijlh.13229",
"article-title": "COVID-19 and the clinical hematology laboratory",
"author": "Frater",
"doi-asserted-by": "crossref",
"first-page": "11",
"issue": "Suppl 1",
"journal-title": "Int. J. Lab. Hematol.",
"key": "10.1016/j.intimp.2020.107209_b0035",
"volume": "42",
"year": "2020"
},
{
"DOI": "10.1515/cclm-2020-0240",
"article-title": "The critical role of laboratory medicine during coronavirus disease 2019 (COVID-19) and other viral outbreaks",
"author": "Lippi",
"doi-asserted-by": "crossref",
"first-page": "1063",
"issue": "7",
"journal-title": "Clin. Chem. Lab. Med.",
"key": "10.1016/j.intimp.2020.107209_b0040",
"volume": "58",
"year": "2020"
},
{
"DOI": "10.1515/cclm-2020-0198",
"article-title": "Laboratory abnormalities in patients with COVID-2019 infection",
"author": "Lippi",
"doi-asserted-by": "crossref",
"journal-title": "Clin. Chem. Lab. Med.",
"key": "10.1016/j.intimp.2020.107209_b0045",
"year": "2020"
},
{
"article-title": "Hematologic parameters in patients with COVID-19 infection",
"author": "Fan",
"journal-title": "Am. J. Hematol.",
"key": "10.1016/j.intimp.2020.107209_b0050",
"year": "2020"
},
{
"DOI": "10.1128/MMBR.05015-11",
"article-title": "Into the eye of the cytokine storm",
"author": "Tisoncik",
"doi-asserted-by": "crossref",
"first-page": "16",
"issue": "1",
"journal-title": "Microbiol. Mol. Biol. Rev.",
"key": "10.1016/j.intimp.2020.107209_b0055",
"volume": "76",
"year": "2012"
},
{
"article-title": "Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study",
"author": "Chen",
"journal-title": "BMJ",
"key": "10.1016/j.intimp.2020.107209_b0060",
"volume": "368",
"year": "2020"
},
{
"article-title": "Structure of the SARS-CoV-2 spike receptor-binding domain bound to the ACE2 receptor",
"author": "Lan",
"first-page": "1",
"journal-title": "Nature",
"key": "10.1016/j.intimp.2020.107209_b0065",
"year": "2020"
},
{
"DOI": "10.1097/RLI.0000000000000674",
"article-title": "Clinical and High-Resolution CT Features of the COVID-19 Infection: Comparison of the Initial and Follow-up Changes",
"author": "Xiong",
"doi-asserted-by": "crossref",
"first-page": "332",
"issue": "6",
"journal-title": "Invest. Radiol.",
"key": "10.1016/j.intimp.2020.107209_b0070",
"volume": "55",
"year": "2020"
},
{
"DOI": "10.1515/cclm-2020-0398",
"article-title": "Routine blood tests as a potential diagnostic tool for COVID-19",
"author": "Ferrari",
"doi-asserted-by": "crossref",
"first-page": "1095",
"issue": "7",
"journal-title": "Clin. Chem. Lab. Med.",
"key": "10.1016/j.intimp.2020.107209_b0075",
"volume": "58",
"year": "2020"
},
{
"DOI": "10.1007/978-94-017-7215-0_8",
"article-title": "The Actual Role of LDH as Tumor Marker, Biochemical and Clinical Aspects",
"author": "Jurisic",
"doi-asserted-by": "crossref",
"first-page": "115",
"journal-title": "Adv. Exp. Med. Biol.",
"key": "10.1016/j.intimp.2020.107209_b0080",
"volume": "867",
"year": "2015"
},
{
"DOI": "10.18632/aging.103372",
"article-title": "Lactate dehydrogenase, an independent risk factor of severe COVID-19 patients: a retrospective and observational study",
"author": "Han",
"doi-asserted-by": "crossref",
"first-page": "11245",
"issue": "12",
"journal-title": "Aging (Albany NY)",
"key": "10.1016/j.intimp.2020.107209_b0085",
"volume": "12",
"year": "2020"
},
{
"article-title": "Clinical characteristics of refractory COVID-19 pneumonia in Wuhan, China",
"author": "Mo",
"journal-title": "Clin. Infect. Dis.",
"key": "10.1016/j.intimp.2020.107209_b0090",
"year": "2020"
},
{
"DOI": "10.1001/jama.2020.1585",
"article-title": "Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China",
"author": "Wang",
"doi-asserted-by": "crossref",
"first-page": "1061",
"issue": "11",
"journal-title": "JAMA.",
"key": "10.1016/j.intimp.2020.107209_b0095",
"volume": "323",
"year": "2020"
},
{
"article-title": "Temple University COVID-19 Research Group. Preliminary predictive criteria for COVID-19 cytokine storm",
"author": "Caricchio",
"journal-title": "Ann. Rheum. Dis.",
"key": "10.1016/j.intimp.2020.107209_b0100",
"year": "2020"
},
{
"DOI": "10.1002/cbin.11403",
"article-title": "Lymphopenia in COVID-19: Therapeutic opportunities",
"author": "Fathi",
"doi-asserted-by": "crossref",
"first-page": "1792",
"issue": "9",
"journal-title": "Cell Biol. Int.",
"key": "10.1016/j.intimp.2020.107209_b0105",
"volume": "44",
"year": "2020"
},
{
"DOI": "10.1016/S2213-2600(20)30079-5",
"article-title": "Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study",
"author": "Yang",
"doi-asserted-by": "crossref",
"journal-title": "Lancet Respir. Med.",
"key": "10.1016/j.intimp.2020.107209_b0110",
"year": "2020"
},
{
"article-title": "Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China",
"author": "Ruan",
"journal-title": "Intensive Care Med.",
"key": "10.1016/j.intimp.2020.107209_b0115",
"year": "2020"
},
{
"DOI": "10.1016/j.pharmthera.2005.07.003",
"article-title": "Cyclic nucleotide phosphodiesterase (PDE) superfamily: a new target for the development of specific therapeutic agents",
"author": "Lugnier",
"doi-asserted-by": "crossref",
"first-page": "366",
"journal-title": "Pharmacol. Ther.",
"key": "10.1016/j.intimp.2020.107209_b0120",
"volume": "109",
"year": "2006"
},
{
"article-title": "Cyclic nucleotide phosphodiesterase (PDE) inhibitors: novel therapeutic agents for progressive renal disease",
"author": "Cheng",
"first-page": "38",
"journal-title": "Exp. Biol. Med.",
"key": "10.1016/j.intimp.2020.107209_b0125",
"volume": "232",
"year": "2007"
},
{
"DOI": "10.2165/00003495-198734010-00003",
"article-title": "A review of its pharmacodynamic and pharmacokinetic properties, and its therapeutic efficacy",
"author": "Ward",
"doi-asserted-by": "crossref",
"first-page": "50",
"issue": "1",
"journal-title": "Drugs.",
"key": "10.1016/j.intimp.2020.107209_b0130",
"volume": "34",
"year": "1987"
},
{
"DOI": "10.1016/j.mehy.2020.109988",
"article-title": "Repositioning of pentoxifylline as an immunomodulator and regulator of the renin-angiotensin system in the treatment of COVID-19 [published online ahead of print, 2020 Jun 9]",
"author": "Maldonado",
"doi-asserted-by": "crossref",
"first-page": "109988",
"journal-title": "Med Hypotheses.",
"key": "10.1016/j.intimp.2020.107209_b0135",
"volume": "144",
"year": "2020"
},
{
"DOI": "10.2165/11532600-000000000-00000",
"article-title": "Pentoxifylline in preterm neonates: a systematic review",
"author": "Harris",
"doi-asserted-by": "crossref",
"first-page": "301",
"journal-title": "Paediatric Drugs.",
"key": "10.1016/j.intimp.2020.107209_b0140",
"volume": "12",
"year": "2010"
},
{
"DOI": "10.1016/S0021-9258(20)89445-9",
"article-title": "Tumor necrosis factor. New insights into the molecular mechanisms of its multiple actions",
"author": "Vilcek",
"doi-asserted-by": "crossref",
"first-page": "7313",
"journal-title": "J. Biol. Chem.",
"key": "10.1016/j.intimp.2020.107209_b0145",
"volume": "266",
"year": "1991"
},
{
"DOI": "10.1007/BF01955273",
"article-title": "Pentoxifylline reduces plasma tumour necrosis factor-alpha concentration in premature infants with sepsis",
"author": "Lauterbach",
"doi-asserted-by": "crossref",
"first-page": "404",
"journal-title": "Eur. J. Pediatr.",
"key": "10.1016/j.intimp.2020.107209_b0150",
"volume": "155",
"year": "1996"
},
{
"DOI": "10.1164/ajrccm.159.2.9804085",
"article-title": "Pentoxifylline inhibits TNF-alpha production from human alveolar macrophages",
"author": "Marques",
"doi-asserted-by": "crossref",
"first-page": "508",
"journal-title": "Am. J. Respir. Crit. Care Med.",
"key": "10.1016/j.intimp.2020.107209_b0155",
"volume": "159",
"year": "1999"
},
{
"DOI": "10.1378/chest.124.4.1526",
"article-title": "Inhibition of cytokine release from alveolar macrophages in pulmonary sarcoidosis by pentoxifylline: comparison with dexamethasone",
"author": "Tong",
"doi-asserted-by": "crossref",
"first-page": "1526",
"journal-title": "Chest",
"key": "10.1016/j.intimp.2020.107209_b0160",
"volume": "124",
"year": "2003"
},
{
"DOI": "10.2217/imt.14.65",
"article-title": "Anti-TNF therapeutics for the treatment of sarcoidosis",
"author": "Crommelin",
"doi-asserted-by": "crossref",
"first-page": "1127",
"journal-title": "Immunotherapy",
"key": "10.1016/j.intimp.2020.107209_b0165",
"volume": "6",
"year": "2014"
},
{
"DOI": "10.1164/ajrccm.155.5.9154873",
"article-title": "Pentoxifylline in treatment of sarcoidosis",
"author": "Zabel",
"doi-asserted-by": "crossref",
"first-page": "1665",
"journal-title": "Am. J. Respir. Crit. Care Med.",
"key": "10.1016/j.intimp.2020.107209_b0170",
"volume": "155",
"year": "1997"
},
{
"article-title": "Steroid-sparing effects of pentoxifylline in pulmonary sarcoidosis",
"author": "Park",
"first-page": "121",
"journal-title": "Sarcoidosis. Vasc. Diffuse Lung Dis.",
"key": "10.1016/j.intimp.2020.107209_b0175",
"volume": "26",
"year": "2009"
},
{
"DOI": "10.1016/j.niox.2003.12.002",
"article-title": "L-arginine and phosphodiesterase (PDE) inhibitors counteract fibrosis in the Peyronie's fibrotic plaque and related fibroblast cultures",
"author": "Valente",
"doi-asserted-by": "crossref",
"first-page": "229",
"journal-title": "Nitric Oxide",
"key": "10.1016/j.intimp.2020.107209_b0180",
"volume": "9",
"year": "2003"
},
{
"DOI": "10.1136/gut.50.2.241",
"article-title": "Pentoxifylline downregulates profibrogenic cytokines and procollagen I expression in rat secondary biliary fibrosis",
"author": "Raetsch",
"doi-asserted-by": "crossref",
"first-page": "241",
"journal-title": "Gut",
"key": "10.1016/j.intimp.2020.107209_b0185",
"volume": "50",
"year": "2002"
},
{
"DOI": "10.1681/ASN.2005040435",
"article-title": "Pentoxifylline attenuates tubulointerstitial fibrosis by blocking Smad3/4-activated transcription and profibrogenic effects of connective tissue growth factor",
"author": "Lin",
"doi-asserted-by": "crossref",
"first-page": "2702",
"journal-title": "J. Am. Soc. Nephrol.",
"key": "10.1016/j.intimp.2020.107209_b0190",
"volume": "16",
"year": "2005"
},
{
"DOI": "10.1111/1523-1747.ep12712140",
"article-title": "Pentoxifylline inhibits normal human dermal fibroblast in vitro proliferation, collagen, glycosaminoglycan, and fibronectin production, and increases collagenase activity",
"author": "Berman",
"doi-asserted-by": "crossref",
"first-page": "605",
"journal-title": "J. Invest. Dermatol.",
"key": "10.1016/j.intimp.2020.107209_b0195",
"volume": "92",
"year": "1989"
},
{
"DOI": "10.1111/1523-1747.ep12612819",
"article-title": "Pentoxifylline, pentifylline, and interferons decrease type I and III procollagen mRNA levels in dermal fibroblasts: evidence for mediation by nuclear factor 1 down-regulation",
"author": "Duncan",
"doi-asserted-by": "crossref",
"first-page": "282",
"journal-title": "J. Invest. Dermatol.",
"key": "10.1016/j.intimp.2020.107209_b0200",
"volume": "104",
"year": "1995"
},
{
"DOI": "10.1177/0003319712436755",
"article-title": "Pentoxifylline lowers plasminogen activator inhibitor 1 levels in obese individuals: a pilot study",
"author": "Muldowney",
"doi-asserted-by": "crossref",
"first-page": "429",
"journal-title": "Angiology",
"key": "10.1016/j.intimp.2020.107209_b0205",
"volume": "63",
"year": "2012"
},
{
"article-title": "Pentoxifylline regulates plasminogen activator inhibitor- 1 expression and protein kinase A phosphorylation in radiation-induced lung fibrosis",
"author": "Lee",
"first-page": "1279280",
"journal-title": "Biomed. Res. Int.",
"key": "10.1016/j.intimp.2020.107209_b0210",
"volume": "2017",
"year": "2017"
},
{
"DOI": "10.1172/JCI11765",
"article-title": "PAI-1, fibrosis, and the elusive provisional fibrin matrix",
"author": "Loskutoff",
"doi-asserted-by": "crossref",
"first-page": "1441",
"journal-title": "J. Clin. Invest.",
"key": "10.1016/j.intimp.2020.107209_b0215",
"volume": "106",
"year": "2000"
},
{
"DOI": "10.1016/j.chest.2019.03.033",
"article-title": "Radiation-inducedlung injury: assessment and management",
"author": "Hanania",
"doi-asserted-by": "crossref",
"first-page": "150",
"journal-title": "Chest",
"key": "10.1016/j.intimp.2020.107209_b0220",
"volume": "156",
"year": "2019"
},
{
"DOI": "10.1016/S0360-3016(03)01444-5",
"article-title": "Pentoxifylline in prevention of radiation induced lung toxicity in patients with breast and lung cancer: a double-blind randomized trial",
"author": "Ozturk",
"doi-asserted-by": "crossref",
"first-page": "213",
"journal-title": "Int. J. Radiat. Oncol. Biol. Phys.",
"key": "10.1016/j.intimp.2020.107209_b0225",
"volume": "58",
"year": "2004"
},
{
"DOI": "10.1200/JCO.2003.06.064",
"article-title": "Randomized, placebo-controlled trial of combined pentoxifylline and tocopherol for regression of superficial radiation- induced fibrosis",
"author": "Delanian",
"doi-asserted-by": "crossref",
"first-page": "2545",
"journal-title": "J. Clin. Oncol.",
"key": "10.1016/j.intimp.2020.107209_b0230",
"volume": "21",
"year": "2003"
},
{
"DOI": "10.1016/j.jnutbio.2013.07.002",
"article-title": "The renin-angiotensin system in adipose tissue and its metabolic consequences during obesity",
"author": "Frigolet",
"doi-asserted-by": "crossref",
"first-page": "2003",
"journal-title": "J. Nutr. Biochem.",
"key": "10.1016/j.intimp.2020.107209_b0235",
"volume": "24",
"year": "2013"
},
{
"DOI": "10.1097/HJH.0000000000001086",
"article-title": "Effects of pentoxifylline on inflammatory markers and blood pressure: a systematic review and meta-analysis of randomized controlled trials",
"author": "Brie",
"doi-asserted-by": "crossref",
"first-page": "2318",
"journal-title": "J. Hypertens",
"key": "10.1016/j.intimp.2020.107209_b0240",
"volume": "34",
"year": "2016"
},
{
"DOI": "10.1002/prp2.631",
"article-title": "Hypothesis: Pentoxifylline is a potential cytokine modulator therapeutic in COVID-19 patients",
"author": "Hendry",
"doi-asserted-by": "crossref",
"issue": "4",
"journal-title": "Pharmacol. Res. Perspect.",
"key": "10.1016/j.intimp.2020.107209_b0245",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1111/j..2002.384.doc.x",
"article-title": "Design and analysis of pilot studies: recommendations for good practice",
"author": "Lancaster",
"doi-asserted-by": "crossref",
"first-page": "307",
"issue": "2",
"journal-title": "J. Eval. Clin. Pract.",
"key": "10.1016/j.intimp.2020.107209_b0250",
"volume": "10",
"year": "2004"
},
{
"DOI": "10.1172/JCI137244",
"article-title": "Clinical and immunological features of severe and moderate coronavirus disease 2019",
"author": "Chen",
"doi-asserted-by": "crossref",
"first-page": "2620",
"issue": "5",
"journal-title": "J. Clin. Invest.",
"key": "10.1016/j.intimp.2020.107209_b0260",
"volume": "130",
"year": "2020"
},
{
"DOI": "10.1093/cid/ciaa248",
"article-title": "Dysregulation of immune response in patients with coronavirus 2019 (COVID-19) in Wuhan, China",
"author": "Qin",
"doi-asserted-by": "crossref",
"first-page": "762",
"issue": "15",
"journal-title": "Clin. Infect. Dis.",
"key": "10.1016/j.intimp.2020.107209_b0265",
"volume": "71",
"year": "2020"
},
{
"DOI": "10.3389/fimmu.2020.00827",
"article-title": "Reduction and functional exhaustion of T cells in patients with coronavirus disease 2019 (COVID-19)",
"author": "Diao",
"doi-asserted-by": "crossref",
"first-page": "827",
"journal-title": "Front. Immunol.",
"key": "10.1016/j.intimp.2020.107209_b0270",
"volume": "11",
"year": "2020"
},
{
"article-title": "Angiotensin II induces nuclear factor (NF)-κB1 isoforms to bind the angiotensinogen gene acute phase response element: a stimulus-specific pathway for NF-κB activation",
"author": "Jamaluddin",
"first-page": "99",
"issue": "1",
"journal-title": "Mol. Endocrinol.",
"key": "10.1016/j.intimp.2020.107209_b0275",
"volume": "14",
"year": "2000"
},
{
"DOI": "10.1097/00041552-200105000-00005",
"article-title": "Proinflammatory actions of angiotensins",
"author": "Ruiz-Ortega",
"doi-asserted-by": "crossref",
"first-page": "321",
"issue": "3",
"journal-title": "Curr. Opin. Nephrol. Hypertens.",
"key": "10.1016/j.intimp.2020.107209_b0280",
"volume": "10",
"year": "2001"
},
{
"DOI": "10.1161/01.ATV.0000131266.38312.2e",
"article-title": "Angiotensin II stimulates the release of interleukin-6 and interleukin-8 from cultured human adipocytes by activation of NF-κB",
"author": "Skurk",
"doi-asserted-by": "crossref",
"first-page": "1199",
"issue": "7",
"journal-title": "Arterioscler. Thromb. Vasc. Biol.",
"key": "10.1016/j.intimp.2020.107209_b0285",
"volume": "24",
"year": "2004"
},
{
"DOI": "10.1016/j.immuni.2020.04.003",
"article-title": "COVID-19: A New Virus, but a Familiar Receptor and Cytokine Release Syndrome",
"author": "Hirano",
"doi-asserted-by": "crossref",
"first-page": "731",
"issue": "5",
"journal-title": "Immunity.",
"key": "10.1016/j.intimp.2020.107209_b0290",
"volume": "52",
"year": "2020"
},
{
"DOI": "10.1016/j.immuni.2019.03.027",
"article-title": "Pleiotropy and specificity: insights from the interleukin 6 family of cytokines",
"author": "Murakami",
"doi-asserted-by": "crossref",
"first-page": "812",
"issue": "4",
"journal-title": "Immunity",
"key": "10.1016/j.intimp.2020.107209_b0295",
"volume": "50",
"year": "2019"
},
{
"DOI": "10.1056/NEJMsr2005760",
"article-title": "Renin-Angiotensin-Aldosterone System Inhibitors in Patients with Covid-19",
"author": "Vaduganathan",
"doi-asserted-by": "crossref",
"first-page": "1653",
"issue": "17",
"journal-title": "N. Engl. J. Med.",
"key": "10.1016/j.intimp.2020.107209_b0300",
"volume": "382",
"year": "2020"
},
{
"DOI": "10.1080/22221751.2020.1746200",
"article-title": "Li, Renin-angiotensin system inhibitors improve the clinical outcomes of COVID-19 patients with hypertension",
"author": "Meng",
"doi-asserted-by": "crossref",
"first-page": "757",
"issue": "1",
"journal-title": "Emerg. Microbes Infect.",
"key": "10.1016/j.intimp.2020.107209_b0305",
"volume": "9",
"year": "2020"
},
{
"DOI": "10.1016/j.jhep.2014.07.005",
"article-title": "Restoration of HBV-specific CD8+ T cell function by PD-1 blockade in inactive carrier patients is linked to T cell differentiation",
"author": "Bengsch",
"doi-asserted-by": "crossref",
"first-page": "1212",
"issue": "6",
"journal-title": "J. Hepatol.",
"key": "10.1016/j.intimp.2020.107209_b0310",
"volume": "61",
"year": "2014"
},
{
"DOI": "10.1038/s41591-020-0819-2",
"article-title": "Breadth of concomitant immune responses prior to patient recovery: A case report of non-severe COVID-19",
"author": "Thevarajan",
"doi-asserted-by": "crossref",
"first-page": "453",
"issue": "4",
"journal-title": "Nat. Med.",
"key": "10.1016/j.intimp.2020.107209_b0315",
"volume": "26",
"year": "2020"
},
{
"DOI": "10.1038/s41423-020-0401-3",
"article-title": "Elevated exhaustion levels and reduced functional diversity of T cells in peripheral blood may predict severe progression in COVID-19 patients",
"author": "Zheng",
"doi-asserted-by": "crossref",
"first-page": "541",
"issue": "5",
"journal-title": "Cell. Mol. Immunol.",
"key": "10.1016/j.intimp.2020.107209_b0320",
"volume": "17",
"year": "2020"
},
{
"DOI": "10.3389/fimmu.2020.00827",
"article-title": "Reduction and functional exhaustion of T cells in patients with coronavirus disease 2019",
"author": "Diao",
"doi-asserted-by": "crossref",
"first-page": "827",
"journal-title": "Front. Immunol.",
"key": "10.1016/j.intimp.2020.107209_b0325",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.4049/jimmunol.169.8.4288",
"article-title": "IL-19 induces production of IL-6 and TNF-alpha and results in cell apoptosis through TNF-alpha",
"author": "Liao",
"doi-asserted-by": "crossref",
"first-page": "4288",
"journal-title": "J. Immunol.",
"key": "10.1016/j.intimp.2020.107209_b0330",
"volume": "169",
"year": "2002"
},
{
"DOI": "10.1016/j.it.2013.10.001",
"article-title": "Tolerance and exhaustion: defining mechanisms of T cell dysfunction",
"author": "Schietinger",
"doi-asserted-by": "crossref",
"first-page": "51",
"issue": "2",
"journal-title": "Trends Immunol.",
"key": "10.1016/j.intimp.2020.107209_b0335",
"volume": "35",
"year": "2014"
},
{
"DOI": "10.1038/s41368-020-0074-x",
"article-title": "High expression of ACE2 receptor of 2019-nCoV on the epithelial cells of oral mucosa",
"author": "Xu",
"doi-asserted-by": "crossref",
"first-page": "8",
"journal-title": "Int. J. Oral. Sci.",
"key": "10.1016/j.intimp.2020.107209_b0340",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1182/blood-2006-07-035972",
"article-title": "Inhibitory effect of tumor cell-derived lactic acid on human T cells",
"author": "Fischer",
"doi-asserted-by": "crossref",
"first-page": "3812",
"journal-title": "Blood",
"key": "10.1016/j.intimp.2020.107209_b0345",
"volume": "109",
"year": "2007"
},
{
"DOI": "10.1620/tjem.222.251",
"article-title": "TNF-α in hypothalamic paraventricular nucleus contributes to sympathoexcitation in heart failure by modulating AT1 receptor and neurotransmitters",
"author": "Kang",
"doi-asserted-by": "crossref",
"first-page": "251",
"issue": "4",
"journal-title": "Tohoku J. Exp. Med.",
"key": "10.1016/j.intimp.2020.107209_b0350",
"volume": "222",
"year": "2010"
},
{
"DOI": "10.1007/s40618-014-0209-z",
"article-title": "Pentoxifylline alleviates hypertension in metabolic syndrome: effect on low-grade inflammation and angiotensin system",
"author": "Azhar",
"doi-asserted-by": "crossref",
"first-page": "437",
"journal-title": "J. Endocrinol. Invest.",
"key": "10.1016/j.intimp.2020.107209_b0355",
"volume": "38",
"year": "2015"
},
{
"article-title": "Acute respiratory distress syndrome: Pathophysiology and therapeutic options",
"author": "Pierrakos",
"first-page": "7",
"journal-title": "J. Clin. Med. Res",
"key": "10.1016/j.intimp.2020.107209_b0360",
"volume": "4",
"year": "2012"
},
{
"DOI": "10.1007/s00134-013-3036-3",
"article-title": "An increased alveolar CD4+CD25+Foxp3+T regulatory cell ratio in acute respiratory distress syndrome is associated with increased 30-day mortality",
"author": "Adamzik",
"doi-asserted-by": "crossref",
"first-page": "1743",
"journal-title": "Intensive Care Med.",
"key": "10.1016/j.intimp.2020.107209_b0365",
"volume": "39",
"year": "2013"
},
{
"DOI": "10.1172/JCI36498",
"article-title": "CD4+CD25+Foxp3+ Tregs resolve experimental lung injury in mice and are present in humans with acute lung injury",
"author": "D’Alessio",
"doi-asserted-by": "crossref",
"first-page": "2898",
"journal-title": "J. Clin. Invest.",
"key": "10.1016/j.intimp.2020.107209_b0370",
"volume": "119",
"year": "2009"
},
{
"DOI": "10.1186/s13054-015-0811-2",
"article-title": "The ratio of Th17/Treg cells as a risk indicator in early acute respiratory distress syndrome",
"author": "Yu",
"doi-asserted-by": "crossref",
"first-page": "82",
"issue": "1",
"journal-title": "Crit. Care.",
"key": "10.1016/j.intimp.2020.107209_b0375",
"volume": "19",
"year": "2015"
},
{
"DOI": "10.3892/mmr.2016.5222",
"article-title": "Resolution acute respiratory distress syndrome through reversing the imbalance of Treg/Th17 by targeting the cAMP signaling pathway",
"author": "Li",
"doi-asserted-by": "crossref",
"first-page": "343",
"issue": "1",
"journal-title": "Mol. Med. Rep.",
"key": "10.1016/j.intimp.2020.107209_b0380",
"volume": "14",
"year": "2016"
},
{
"DOI": "10.1056/NEJMoa2015432",
"article-title": "Pulmonary Vascular Endothelialitis, Thrombosis, and Angiogenesis in Covid-19",
"author": "Ackermann",
"doi-asserted-by": "crossref",
"first-page": "120",
"issue": "2",
"journal-title": "N. Engl. J. Med.",
"key": "10.1016/j.intimp.2020.107209_b0385",
"volume": "383",
"year": "2020"
},
{
"key": "10.1016/j.intimp.2020.107209_b0390",
"unstructured": "J.A. Lott, E. Nemensanszky, Lactate dehydrogenase, In: J.A. Lott, P.L. Wolf (Eds.), Clinical Enzymology, a case-orianted Aprroach. 1987. pp. 213–244. [Google Scholar]."
},
{
"article-title": "Enzymes",
"author": "Moss",
"first-page": "735",
"key": "10.1016/j.intimp.2020.107209_b0395",
"series-title": "Tietz Textbook of Clinical Chemistry",
"year": "1986"
},
{
"DOI": "10.1093/ajcp/52.3.320",
"article-title": "Serum lactate dehydrogenase isoenzyme and total lactate dehydrogenase values in health and disease, and clincal evaluation of these test by means of discriminant analysis",
"author": "Glick",
"doi-asserted-by": "crossref",
"first-page": "320",
"journal-title": "Am. J. Clin. Pathol.",
"key": "10.1016/j.intimp.2020.107209_b0400",
"volume": "52",
"year": "1969"
},
{
"DOI": "10.1183/09031936.96.09081736",
"article-title": "Usefulness of lactate dehydrogenase and its isoenzymes as indicators of lung damage or inflammation",
"author": "Drent",
"doi-asserted-by": "crossref",
"first-page": "1736",
"issue": "8",
"journal-title": "Eur. Respir. J.",
"key": "10.1016/j.intimp.2020.107209_b0405",
"volume": "9",
"year": "1996"
},
{
"DOI": "10.1378/chest.93.5.987",
"article-title": "Elevated lactate dehydrogenase values in patients with Pneumocystis carinii pneumonia",
"author": "Smith",
"doi-asserted-by": "crossref",
"first-page": "987",
"journal-title": "Chest",
"key": "10.1016/j.intimp.2020.107209_b0410",
"volume": "93",
"year": "1988"
},
{
"DOI": "10.1136/thx.50.6.668",
"article-title": "Prognostic factors influencing the outcome in Pneumocystis carinii pneumonia in patients with AIDS",
"author": "Fernandez",
"doi-asserted-by": "crossref",
"first-page": "668",
"journal-title": "Thorax",
"key": "10.1016/j.intimp.2020.107209_b0415",
"volume": "50",
"year": "1995"
},
{
"DOI": "10.1378/chest.108.2.415",
"article-title": "Serum lactate dehydrogenase (LDH) in Pneumocystis carinii pneumonia, tuberculosis and bacterial pneumonia",
"author": "Quist",
"doi-asserted-by": "crossref",
"first-page": "415",
"journal-title": "Chest",
"key": "10.1016/j.intimp.2020.107209_b0420",
"volume": "108",
"year": "1995"
},
{
"DOI": "10.1164/ajrccm/143.1.42",
"article-title": "Serum and lavage lactate dehydrogenase isoenzymes in pulmonary alveolar proteinosis",
"author": "Hoffman",
"doi-asserted-by": "crossref",
"first-page": "42",
"journal-title": "Am. Rev. Respir. Dis.",
"key": "10.1016/j.intimp.2020.107209_b0425",
"volume": "143",
"year": "1991"
},
{
"DOI": "10.1016/0300-2977(95)00074-7",
"article-title": "Serum LDH: a marker of disease activity and its response to therapy in idiopathic pulmonary fibrosis",
"author": "Krugten van",
"doi-asserted-by": "crossref",
"first-page": "220",
"journal-title": "Neth. J. Med.",
"key": "10.1016/j.intimp.2020.107209_b0430",
"volume": "48",
"year": "1996"
},
{
"article-title": "Lactate dehydrogenase isoenzymes during the development of experimental fibrosis",
"author": "Lindy",
"first-page": "756",
"journal-title": "J. Lab. Clin. Med.",
"key": "10.1016/j.intimp.2020.107209_b0435",
"volume": "76",
"year": "1970"
},
{
"DOI": "10.1183/09031936.93.06091282",
"article-title": "Plasma lactate dehydrogenase: a marker of disease activity in cryptogenic fibrosing alveolitis and extrinsic allergic alveolitis?",
"author": "Matusiewicz",
"doi-asserted-by": "crossref",
"first-page": "1282",
"journal-title": "Eur. Respir. J.",
"key": "10.1016/j.intimp.2020.107209_b0440",
"volume": "6",
"year": "1993"
},
{
"DOI": "10.1001/jama.1968.03140260033015",
"article-title": "Serum lactic dehydrogenase activity and diffuse interstitial pneumonitis",
"author": "DeRemee",
"doi-asserted-by": "crossref",
"first-page": "1193",
"issue": "13",
"journal-title": "JAMA.",
"key": "10.1016/j.intimp.2020.107209_b0445",
"volume": "204",
"year": "1968"
},
{
"key": "#cr-split#-10.1016/j.intimp.2020.107209_b0450.1",
"unstructured": "Clinical findings of 35 cases with novel coronavirus pneumonia outside of Wuhan, [cited 2020 Apr 29]"
},
{
"key": "#cr-split#-10.1016/j.intimp.2020.107209_b0450.2",
"unstructured": "Available from, 2020 Apr 17. https://www.researchsquare.com/article/rs-22554/v1."
},
{
"article-title": "The role of biomarkers in diagnosis of COVID-19 - A systematic review",
"author": "Kermali",
"issue": "254",
"journal-title": "Life Sci.",
"key": "10.1016/j.intimp.2020.107209_b0455",
"volume": "1",
"year": "2020"
}
],
"reference-count": 91,
"references-count": 91,
"relation": {},
"resource": {
"primary": {
"URL": "https://linkinghub.elsevier.com/retrieve/pii/S1567576920336766"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"special_numbering": "C",
"subject": [],
"subtitle": [],
"title": "Pentoxifylline decreases serum LDH levels and increases lymphocyte count in COVID-19 patients: Results from an external pilot study",
"type": "journal-article",
"update-policy": "https://doi.org/10.1016/elsevier_cm_policy",
"volume": "90"
}