The association of remdesivir and in-hospital outcomes for COVID-19 patients treated with steroids
et al., Journal of Antimicrobial Chemotherapy, doi:10.1093/jac/dkab256, Aug 2021
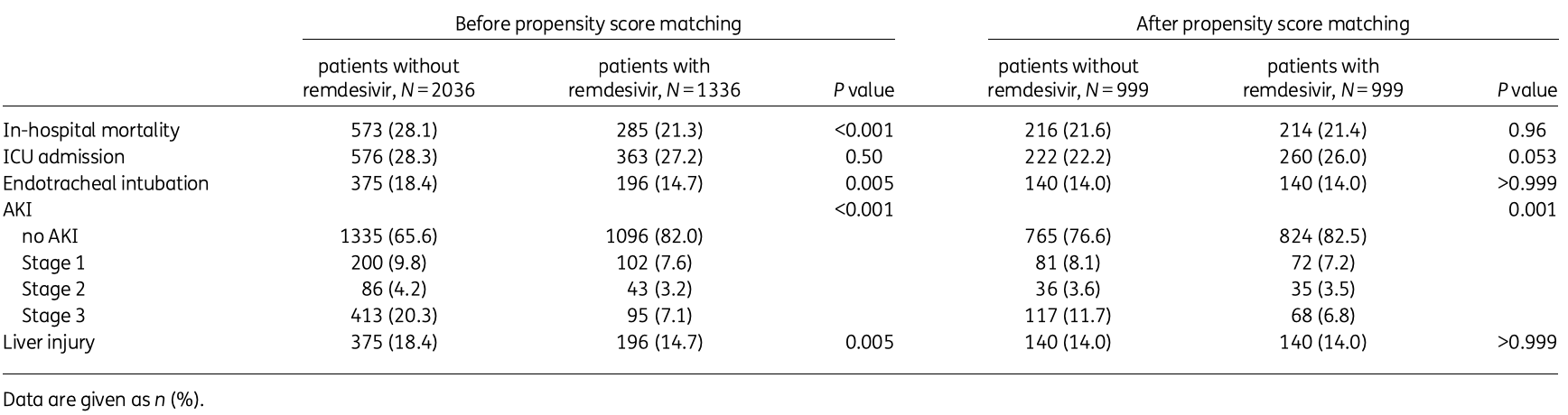
PSM retrospective 3,372 hospitalized patients in the USA treated with steroids, showing no significant difference in mortality with remdesivir, but a lower risk of acute kidney injury.
Gérard, Zhou, Wu, Kamo, Choi, Kim show increased risk of acute kidney injury, Leo, Briciu, Muntean, Petrov show increased risk of liver injury, and Negru, Cheng, Mohammed, Kwok show increased risk of cardiac disorders with remdesivir.
Remdesivir efficacy disappears with longer
followup. Mixed-effects meta-regression of efficacy as a function of
followup duration across all remdesivir studies shows decreasing efficacy with
longer followup15. This may reflect
antiviral efficacy being offset by serious adverse effects of treatment.
Standard of Care (SOC) for COVID-19 in the study country,
the USA, is very poor with very low average efficacy for approved treatments16.
Only expensive, high-profit treatments were approved for early treatment. Low-cost treatments were excluded, reducing the probability of early treatment due to access and cost barriers, and eliminating complementary and synergistic benefits seen with many low-cost treatments.
This may explain in part the very high mortality seen in this study.
Results may differ in countries with improved SOC.
|
risk of death, 0.9% lower, RR 0.99, p = 0.96, treatment 214 of 999 (21.4%), control 216 of 999 (21.6%), NNT 499, PSM.
|
|
risk of mechanical ventilation, no change, RR 1.00, p = 1.00, treatment 140 of 999 (14.0%), control 140 of 999 (14.0%), PSM.
|
|
risk of ICU admission, 17.1% higher, RR 1.17, p = 0.05, treatment 260 of 999 (26.0%), control 222 of 999 (22.2%), PSM.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
1.
Gérard et al., Remdesivir and Acute Renal Failure: A Potential Safety Signal From Disproportionality Analysis of the WHO Safety Database, Clinical Pharmacology & Therapeutics, doi:10.1002/cpt.2145.
2.
Zhou et al., Acute Kidney Injury and Drugs Prescribed for COVID-19 in Diabetes Patients: A Real-World Disproportionality Analysis, Frontiers in Pharmacology, doi:10.3389/fphar.2022.833679.
3.
Wu et al., Acute Kidney Injury Associated With Remdesivir: A Comprehensive Pharmacovigilance Analysis of COVID-19 Reports in FAERS, Frontiers in Pharmacology, doi:10.3389/fphar.2022.692828.
4.
Kamo et al., Association of Antiviral Drugs for the Treatment of COVID-19 With Acute Renal Failure, In Vivo, doi:10.21873/invivo.13637.
5.
Choi et al., Comparative effectiveness of combination therapy with nirmatrelvir–ritonavir and remdesivir versus monotherapy with remdesivir or nirmatrelvir–ritonavir in patients hospitalised with COVID-19: a target trial emulation study, The Lancet Infectious Diseases, doi:10.1016/S1473-3099(24)00353-0.
6.
Kim et al., Investigating the Safety Profile of Fast‐Track COVID‐19 Drugs Using the FDA Adverse Event Reporting System Database: A Comparative Observational Study, Pharmacoepidemiology and Drug Safety, doi:10.1002/pds.70043.
7.
Leo et al., Hepatocellular liver injury in hospitalized patients affected by COVID-19: Presence of different risk factors at different time points, Digestive and Liver Disease, doi:10.1016/j.dld.2021.12.014.
8.
Briciu et al., Evolving Clinical Manifestations and Outcomes in COVID-19 Patients: A Comparative Analysis of SARS-CoV-2 Variant Waves in a Romanian Hospital Setting, Pathogens, doi:10.3390/pathogens12121453.
9.
Muntean et al., Effects of COVID-19 on the Liver and Mortality in Patients with SARS-CoV-2 Pneumonia Caused by Delta and Non-Delta Variants: An Analysis in a Single Centre, Pharmaceuticals, doi:10.3390/ph17010003.
10.
Petrov et al., The Effect of Potentially Hepatotoxic Medicinal Products on Alanine Transaminase Levels in COVID-19 Patients: A Case–Control Study, Safety and Risk of Pharmacotherapy, doi:10.30895/2312-7821-2025-458.
11.
Negru et al., Comparative Pharmacovigilance Analysis of Approved and Repurposed Antivirals for COVID-19: Insights from EudraVigilance Data, Biomedicines, doi:10.3390/biomedicines13061387.
12.
Cheng et al., Cardiovascular Safety of COVID-19 Treatments: A Disproportionality Analysis of Adverse Event Reports from the WHO VigiBase, Infectious Diseases and Therapy, doi:10.1007/s40121-025-01225-z.
13.
Mohammed et al., Bradycardia associated with remdesivir treatment in coronavirus disease 2019 patients: A propensity score-matched analysis, Medicine, doi:10.1097/MD.0000000000044501.
Kuno et al., 9 Aug 2021, retrospective, propensity score matching, USA, peer-reviewed, 6 authors.
The association of remdesivir and in-hospital outcomes for COVID-19 patients treated with steroids
Background: Remdesivir has been shown to decrease SARS-CoV-2 viral loads and the duration of COVID-19 symptoms. However, current evidence regarding the association between remdesivir and in-hospital mortality for patients with COVID-19 steroid treatments is limited. We aimed to investigate whether remdesivir reduces in-hospital mortality among patients with COVID-19 treated with steroids.
Methods: In this retrospective multicentre study, we reviewed the medical records of 3372 patients discharged between 1 March 2020 and 30 March 2021, with laboratory confirmed COVID-19 in the Mount Sinai Health System and treated with steroids. We evaluated the effect of remdesivir on the outcomes using propensity score analyses. Subgroup analyses were conducted by stratification of patients by endotracheal intubation and COVID-19 antibody status. Acute kidney injury (AKI) was defined as an absolute serum creatinine increase of 0.3 mg/dL or a relative increase of 50%. Results: Of the 3372 eligible patients, 1336 (39.6%) received remdesivir. After 1:1 propensity score matching (N = 999 pairs), in-hospital mortality was similar between those with and without remdesivir (21.4% versus 21.6%, respectively, P = 0.96). Remdesivir was not significantly associated with in-hospital mortality regardless of endotracheal intubation or COVID-19 antibody status. However, there was a signal that remdesivir was associated with a reduced risk of AKI in the propensity matched analysis (17.5% versus 23.4%, respectively, P = 0.001). Conclusions: Remdesivir was not associated with reduced risk of in-hospital mortality in patients with COVID-19 treated with steroids but potentially associated with decreased risk of AKI. These findings should be confirmed in prospective studies focusing on COVID-19 patients treated with steroids.
COVID-19 and remdesivir
Author contributions Data curation, full access to all of the data in the study and responsibility taken for the integrity of the data and the accuracy of the data analysis: T.K., M.T. and N.N.E. Study concept and design, and drafting of the manuscript: T.K. Statistical analysis: T.K. and M.T. Administrative, technical, or material support, and study supervision: N.N.E. Acquisition, analysis, or interpretation of data, and critical revision of the manuscript for important intellectual content: all authors.
References
Acosta-Ochoa, Bustamante-Munguira, Mendiluce-Herrero, Impact on outcomes across KDIGO-2012 AKI criteria according to baseline renal function, J Clin Med
Austin, The relative ability of different propensity score methods to balance measured covariates between treated and untreated subjects in observational studies, Med Decis Making
Beigel, Tomashek, Dodd, Remdesivir for the treatment of COVID-19 -final report, N Engl J Med
Chandiramani, Cao, Contrast-induced acute kidney injury, Cardiovasc Interv Ther
Eikelboom, Connolly, Bosch, Rivaroxaban with or without aspirin in stable cardiovascular disease, N Engl J Med
Gabarre, Dumas, Dupont, Acute kidney injury in critically ill patients with COVID-19, Intensive Care Med
Kaka, Macdonald, Greer, Major update: remdesivir for adults with COVID-19: a living systematic review and meta-analysis for the American College of Physicians practice points, Ann Intern Med
Kuno, Takahashi, Egorova, The association between convalescent plasma treatment and survival of patients with COVID-19, J Gen Intern Med, doi:10.1007/s11606-021-06894-3
Lai, Chen, Wang, Clinical efficacy and safety of remdesivir in patients with COVID-19: a systematic review and network meta-analysis of randomized controlled trials, J Antimicrob Chemother, doi:10.1093/jac/dkab093
Levey, Stevens, Schmid, A new equation to estimate glomerular filtration rate, Ann Intern Med
Maeda, Obata, Rizk, Cardiac injury and outcomes of patients with COVID-19 in New York City, Heart Lung Circ
Maeda, Obata, Rizk, The association of interleukin-6 value, interleukin inhibitors, and outcomes of patients with COVID-19 in New York City, J Med Virol
Mehta, Bansal, Bysani, A shorter symptom-onset to remdesivir treatment (SORT) interval is associated with a lower mortality in moderate-to-severe COVID-19: a real-world analysis, Int J Infect Dis
Mehta, Mcauley, Brown, Repurposed Antiviral Drugs for COVID-19 -Interim WHO Solidarity Trial Results, N Engl J Med
Nadim, Forni, Mehta, COVID-19-associated acute kidney injury: consensus report of the 25th Acute Disease Quality Initiative (ADQI) Workgroup, Nat Rev Nephrol
Obata, Maeda, Rizk, Palliative care team involvement in patients with COVID-19 in New York City, Am J Hosp Palliat Care
Petrilli, Jones, Yang, Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in New York City: prospective cohort study, BMJ
Recovery Collaborative Group, Horby, Lim, Emberson, Dexamethasone in hospitalized patients with COVID-19 -Preliminary Report, N Engl J Med
Rezagholizadeh, Khiali, Sarbakhsh, Remdesivir for treatment of COVID-19; an updated systematic review and meta-analysis, Eur J Pharmacol
Rosenberg, Dufort, Udo, Association of treatment with hydroxychloroquine or azithromycin with in-hospital mortality in patients with COVID-19 in New York State, JAMA
So, Steiger, Takahashi, The characteristics and outcomes of critically Ill patients with COVID-19 who received systemic thrombolysis for presumed pulmonary embolism: an observational study, J Thromb Thrombolysis, doi:10.1007/s11239-021-02477-5
Sterne, Murthy, Diaz, Association between administration of systemic corticosteroids and mortality among critically ill patients with COVID-19: a meta-analysis, JAMA
Takahashi, Egorova, Kuno, COVID-19 and influenza testing in New York City, J Med Virol
Wright, Prevention of the cytokine storm in COVID-19, Lancet Infect Dis
Yokoyama, Briasoulis, Takagi, Effect of remdesivir on patients with COVID-19: a network meta-analysis of randomized control trials, Virus Res
Zhu, Zhang, A novel coronavirus from patients with pneumonia in China, 2019, N Engl J Med
DOI record:
{
"DOI": "10.1093/jac/dkab256",
"ISSN": [
"0305-7453",
"1460-2091"
],
"URL": "http://dx.doi.org/10.1093/jac/dkab256",
"abstract": "<jats:title>Abstract</jats:title><jats:sec><jats:title>Background</jats:title><jats:p>Remdesivir has been shown to decrease SARS-CoV-2 viral loads and the duration of COVID-19 symptoms. However, current evidence regarding the association between remdesivir and in-hospital mortality for patients with COVID-19 steroid treatments is limited. We aimed to investigate whether remdesivir reduces in-hospital mortality among patients with COVID-19 treated with steroids.</jats:p></jats:sec><jats:sec><jats:title>Methods</jats:title><jats:p>In this retrospective multicentre study, we reviewed the medical records of 3372 patients discharged between 1 March 2020 and 30 March 2021, with laboratory confirmed COVID-19 in the Mount Sinai Health System and treated with steroids. We evaluated the effect of remdesivir on the outcomes using propensity score analyses. Subgroup analyses were conducted by stratification of patients by endotracheal intubation and COVID-19 antibody status. Acute kidney injury (AKI) was defined as an absolute serum creatinine increase of 0.3 mg/dL or a relative increase of 50%.</jats:p></jats:sec><jats:sec><jats:title>Results</jats:title><jats:p>Of the 3372 eligible patients, 1336 (39.6%) received remdesivir. After 1:1 propensity score matching (N = 999 pairs), in-hospital mortality was similar between those with and without remdesivir (21.4% versus 21.6%, respectively, P = 0.96). Remdesivir was not significantly associated with in-hospital mortality regardless of endotracheal intubation or COVID-19 antibody status. However, there was a signal that remdesivir was associated with a reduced risk of AKI in the propensity matched analysis (17.5% versus 23.4%, respectively, P = 0.001).</jats:p></jats:sec><jats:sec><jats:title>Conclusions</jats:title><jats:p>Remdesivir was not associated with reduced risk of in-hospital mortality in patients with COVID-19 treated with steroids but potentially associated with decreased risk of AKI. These findings should be confirmed in prospective studies focusing on COVID-19 patients treated with steroids.</jats:p></jats:sec>",
"author": [
{
"ORCID": "http://orcid.org/0000-0002-2487-8366",
"affiliation": [
{
"name": "Department of Medicine, Icahn School of Medicine at Mount Sinai, Mount Sinai Beth Israel, New York, NY, USA"
}
],
"authenticated-orcid": false,
"family": "Kuno",
"given": "Toshiki",
"sequence": "first"
},
{
"affiliation": [
{
"name": "Division of Nephrology and Endocrinology, The University of Tokyo, Tokyo, Japan"
}
],
"family": "Miyamoto",
"given": "Yoshihisa",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Health Services Research, University of Tsukuba, Tsukuba, Japan"
}
],
"family": "Iwagami",
"given": "Masao",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Health Services Research, University of Tsukuba, Tsukuba, Japan"
}
],
"family": "Ishimaru",
"given": "Miho",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Medicine, Icahn School of Medicine at Mount Sinai, Mount Sinai Beth Israel, New York, NY, USA"
}
],
"family": "Takahashi",
"given": "Mai",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Population Health Science and Policy, Icahn School of Medicine at Mount Sinai, New York, NY, USA"
}
],
"family": "Egorova",
"given": "Natalia N",
"sequence": "additional"
}
],
"container-title": "Journal of Antimicrobial Chemotherapy",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2021,
7,
2
]
],
"date-time": "2021-07-02T11:24:37Z",
"timestamp": 1625225077000
},
"deposited": {
"date-parts": [
[
2023,
1,
2
]
],
"date-time": "2023-01-02T13:35:13Z",
"timestamp": 1672666513000
},
"indexed": {
"date-parts": [
[
2024,
3,
22
]
],
"date-time": "2024-03-22T16:18:31Z",
"timestamp": 1711124311613
},
"is-referenced-by-count": 13,
"issue": "10",
"issued": {
"date-parts": [
[
2021,
8,
9
]
]
},
"journal-issue": {
"issue": "10",
"published-online": {
"date-parts": [
[
2021,
8,
9
]
]
},
"published-print": {
"date-parts": [
[
2021,
9,
15
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://academic.oup.com/journals/pages/open_access/funder_policies/chorus/standard_publication_model",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
8,
9
]
],
"date-time": "2021-08-09T00:00:00Z",
"timestamp": 1628467200000
}
}
],
"link": [
{
"URL": "http://academic.oup.com/jac/article-pdf/76/10/2690/40394361/dkab256.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "syndication"
},
{
"URL": "http://academic.oup.com/jac/article-pdf/76/10/2690/40394361/dkab256.pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "286",
"original-title": [],
"page": "2690-2696",
"prefix": "10.1093",
"published": {
"date-parts": [
[
2021,
8,
9
]
]
},
"published-online": {
"date-parts": [
[
2021,
8,
9
]
]
},
"published-other": {
"date-parts": [
[
2021,
10,
1
]
]
},
"published-print": {
"date-parts": [
[
2021,
9,
15
]
]
},
"publisher": "Oxford University Press (OUP)",
"reference": [
{
"DOI": "10.1056/NEJMoa2001017",
"article-title": "A novel coronavirus from patients with pneumonia in China, 2019",
"author": "Zhu",
"doi-asserted-by": "crossref",
"first-page": "727",
"journal-title": "N Engl J Med",
"key": "2021091708523184900_dkab256-B1",
"volume": "382",
"year": "2020"
},
{
"article-title": "The association of interleukin-6 value, interleukin inhibitors, and outcomes of patients with COVID-19 in New York City",
"author": "Maeda",
"first-page": "473",
"journal-title": "J Med Virol",
"key": "2021091708523184900_dkab256-B2",
"volume": "93",
"year": "2020"
},
{
"DOI": "10.1016/j.hlc.2020.10.025",
"article-title": "Cardiac injury and outcomes of patients with COVID-19 in New York City",
"author": "Maeda",
"doi-asserted-by": "crossref",
"first-page": "848",
"journal-title": "Heart Lung Circ",
"key": "2021091708523184900_dkab256-B3",
"volume": "30",
"year": "2021"
},
{
"key": "2021091708523184900_dkab256-B4"
},
{
"DOI": "10.1001/jama.2020.8630",
"article-title": "Association of treatment with hydroxychloroquine or azithromycin with in-hospital mortality in patients with COVID-19 in New York State",
"author": "Rosenberg",
"doi-asserted-by": "crossref",
"first-page": "2493",
"journal-title": "JAMA",
"key": "2021091708523184900_dkab256-B5",
"volume": "323",
"year": "2020"
},
{
"author": "Collaborative",
"first-page": "693",
"key": "2021091708523184900_dkab256-B6",
"volume": "384",
"year": "2021"
},
{
"DOI": "10.1001/jama.2020.17023",
"article-title": "Association between administration of systemic corticosteroids and mortality among critically ill patients with COVID-19: a meta-analysis",
"author": "Sterne",
"doi-asserted-by": "crossref",
"first-page": "1330",
"journal-title": "JAMA",
"key": "2021091708523184900_dkab256-B7",
"volume": "324",
"year": "2020"
},
{
"DOI": "10.1056/NEJMoa2007764",
"article-title": "Remdesivir for the treatment of COVID-19 - final report",
"author": "Beigel",
"doi-asserted-by": "crossref",
"first-page": "1813",
"journal-title": "N Engl J Med",
"key": "2021091708523184900_dkab256-B8",
"volume": "383",
"year": "2020"
},
{
"DOI": "10.1016/j.ejphar.2021.173926",
"article-title": "Remdesivir for treatment of COVID-19; an updated systematic review and meta-analysis",
"author": "Rezagholizadeh",
"doi-asserted-by": "crossref",
"first-page": "173926",
"journal-title": "Eur J Pharmacol",
"key": "2021091708523184900_dkab256-B9",
"volume": "897",
"year": "2021"
},
{
"DOI": "10.7326/M20-8148",
"article-title": "Major update: remdesivir for adults with COVID-19: a living systematic review and meta-analysis for the American College of Physicians practice points",
"author": "Kaka",
"doi-asserted-by": "crossref",
"first-page": "663",
"journal-title": "Ann Intern Med",
"key": "2021091708523184900_dkab256-B10",
"volume": "174",
"year": "2021"
},
{
"DOI": "10.1016/j.virusres.2020.198137",
"article-title": "Effect of remdesivir on patients with COVID-19: a network meta-analysis of randomized control trials",
"author": "Yokoyama",
"doi-asserted-by": "crossref",
"first-page": "198137",
"journal-title": "Virus Res",
"key": "2021091708523184900_dkab256-B11",
"volume": "288",
"year": "2020"
},
{
"DOI": "10.1093/jac/dkab093",
"article-title": "Clinical efficacy and safety of remdesivir in patients with COVID-19: a systematic review and network meta-analysis of randomized controlled trials",
"author": "Lai",
"doi-asserted-by": "crossref",
"journal-title": "J Antimicrob Chemother",
"key": "2021091708523184900_dkab256-B12",
"volume": "76",
"year": "2021"
},
{
"DOI": "10.1002/jmv.26500",
"article-title": "COVID-19 and influenza testing in New York City",
"author": "Takahashi",
"doi-asserted-by": "crossref",
"first-page": "698",
"journal-title": "J Med Virol",
"key": "2021091708523184900_dkab256-B13",
"volume": "93",
"year": "2021"
},
{
"DOI": "10.1007/s11606-021-06894-3",
"article-title": "The association between convalescent plasma treatment and survival of patients with COVID-19",
"author": "Kuno",
"doi-asserted-by": "crossref",
"journal-title": "J Gen Intern Med",
"key": "2021091708523184900_dkab256-B14",
"year": "2021"
},
{
"DOI": "10.1007/s11239-021-02477-5",
"article-title": "The characteristics and outcomes of critically Ill patients with COVID-19 who received systemic thrombolysis for presumed pulmonary embolism: an observational study",
"author": "So",
"doi-asserted-by": "crossref",
"journal-title": "J Thromb Thrombolysis",
"key": "2021091708523184900_dkab256-B15",
"year": "2021"
},
{
"DOI": "10.3390/jcm8091323",
"article-title": "Impact on outcomes across KDIGO-2012 AKI criteria according to baseline renal function",
"author": "Acosta-Ochoa",
"doi-asserted-by": "crossref",
"first-page": "1323",
"journal-title": "J Clin Med",
"key": "2021091708523184900_dkab256-B16",
"volume": "8",
"year": "2019"
},
{
"DOI": "10.1007/s12928-020-00660-8",
"article-title": "Contrast-induced acute kidney injury",
"author": "Chandiramani",
"doi-asserted-by": "crossref",
"first-page": "209",
"journal-title": "Cardiovasc Interv Ther",
"key": "2021091708523184900_dkab256-B17",
"volume": "35",
"year": "2020"
},
{
"DOI": "10.1056/NEJMoa1709118",
"article-title": "Rivaroxaban with or without aspirin in stable cardiovascular disease",
"author": "Eikelboom",
"doi-asserted-by": "crossref",
"first-page": "1319",
"journal-title": "N Engl J Med",
"key": "2021091708523184900_dkab256-B18",
"volume": "377",
"year": "2017"
},
{
"DOI": "10.1177/0272989X09341755",
"article-title": "The relative ability of different propensity score methods to balance measured covariates between treated and untreated subjects in observational studies",
"author": "Austin",
"doi-asserted-by": "crossref",
"first-page": "661",
"journal-title": "Med Decis Making",
"key": "2021091708523184900_dkab256-B19",
"volume": "29",
"year": "2009"
},
{
"DOI": "10.1136/bmj.m1966",
"article-title": "Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in New York City: prospective cohort study",
"author": "Petrilli",
"doi-asserted-by": "crossref",
"first-page": "m1966",
"journal-title": "BMJ",
"key": "2021091708523184900_dkab256-B20",
"volume": "369",
"year": "2020"
},
{
"DOI": "10.7326/0003-4819-150-9-200905050-00006",
"article-title": "A new equation to estimate glomerular filtration rate",
"author": "Levey",
"doi-asserted-by": "crossref",
"first-page": "604",
"journal-title": "Ann Intern Med",
"key": "2021091708523184900_dkab256-B21",
"volume": "150",
"year": "2009"
},
{
"DOI": "10.1016/j.ijid.2021.02.092",
"article-title": "A shorter symptom-onset to remdesivir treatment (SORT) interval is associated with a lower mortality in moderate-to-severe COVID-19: a real-world analysis",
"author": "Mehta",
"doi-asserted-by": "crossref",
"first-page": "71",
"journal-title": "Int J Infect Dis",
"key": "2021091708523184900_dkab256-B22",
"volume": "106",
"year": "2021"
},
{
"DOI": "10.1016/S0140-6736(20)30628-0",
"article-title": "COVID-19: consider cytokine storm syndromes and immunosuppression",
"author": "Mehta",
"doi-asserted-by": "crossref",
"first-page": "1033",
"journal-title": "Lancet",
"key": "2021091708523184900_dkab256-B23",
"volume": "395",
"year": "2020"
},
{
"DOI": "10.1056/NEJMoa2023184",
"article-title": "Repurposed Antiviral Drugs for COVID-19 - Interim WHO Solidarity Trial Results",
"author": "Pan",
"doi-asserted-by": "crossref",
"first-page": "497",
"journal-title": "N Engl J Med",
"key": "2021091708523184900_dkab256-B24",
"volume": "384",
"year": "2021"
},
{
"DOI": "10.1016/S1473-3099(20)30376-5",
"article-title": "Prevention of the cytokine storm in COVID-19",
"author": "Wright",
"doi-asserted-by": "crossref",
"first-page": "25",
"journal-title": "Lancet Infect Dis",
"key": "2021091708523184900_dkab256-B25",
"volume": "21",
"year": "2021"
},
{
"DOI": "10.1177/1049909120940986",
"article-title": "Palliative care team involvement in patients with COVID-19 in New York City",
"author": "Obata",
"doi-asserted-by": "crossref",
"first-page": "869",
"journal-title": "Am J Hosp Palliat Care",
"key": "2021091708523184900_dkab256-B26",
"volume": "37",
"year": "2020"
},
{
"DOI": "10.1007/s00134-020-06153-9",
"article-title": "Acute kidney injury in critically ill patients with COVID-19",
"author": "Gabarre",
"doi-asserted-by": "crossref",
"first-page": "1339",
"journal-title": "Intensive Care Med",
"key": "2021091708523184900_dkab256-B27",
"volume": "46",
"year": "2020"
},
{
"DOI": "10.1038/s41581-020-00356-5",
"article-title": "COVID-19-associated acute kidney injury: consensus report of the 25th Acute Disease Quality Initiative (ADQI) Workgroup",
"author": "Nadim",
"doi-asserted-by": "crossref",
"first-page": "747",
"journal-title": "Nat Rev Nephrol",
"key": "2021091708523184900_dkab256-B28",
"volume": "16",
"year": "2020"
}
],
"reference-count": 28,
"references-count": 28,
"relation": {},
"resource": {
"primary": {
"URL": "https://academic.oup.com/jac/article/76/10/2690/6345860"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Infectious Diseases",
"Pharmacology (medical)",
"Pharmacology",
"Microbiology (medical)"
],
"subtitle": [],
"title": "The association of remdesivir and in-hospital outcomes for COVID-19 patients treated with steroids",
"type": "journal-article",
"volume": "76"
}