Antiviral drug treatment profiles and clinical outcomes of COVID-19 patients at public hospitals in Erbil city
et al., Advanced medical journal, doi:10.56056/amj.2024.273, Sep 2024
Retrospective 451 hospitalized COVID-19 patients in Iraq showing no significant difference in mortality with remdesivir treatment.
Gérard, Zhou, Wu, Kamo, Choi, Kim show increased risk of acute kidney injury, Leo, Briciu, Muntean, Petrov show increased risk of liver injury, and Negru, Cheng, Mohammed, Kwok show increased risk of cardiac disorders with remdesivir.
|
risk of death, 8.7% higher, OR 1.09, p = 0.86, treatment 111, control 340, adjusted per study, RR approximated with OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
1.
Gérard et al., Remdesivir and Acute Renal Failure: A Potential Safety Signal From Disproportionality Analysis of the WHO Safety Database, Clinical Pharmacology & Therapeutics, doi:10.1002/cpt.2145.
2.
Zhou et al., Acute Kidney Injury and Drugs Prescribed for COVID-19 in Diabetes Patients: A Real-World Disproportionality Analysis, Frontiers in Pharmacology, doi:10.3389/fphar.2022.833679.
3.
Wu et al., Acute Kidney Injury Associated With Remdesivir: A Comprehensive Pharmacovigilance Analysis of COVID-19 Reports in FAERS, Frontiers in Pharmacology, doi:10.3389/fphar.2022.692828.
4.
Kamo et al., Association of Antiviral Drugs for the Treatment of COVID-19 With Acute Renal Failure, In Vivo, doi:10.21873/invivo.13637.
5.
Choi et al., Comparative effectiveness of combination therapy with nirmatrelvir–ritonavir and remdesivir versus monotherapy with remdesivir or nirmatrelvir–ritonavir in patients hospitalised with COVID-19: a target trial emulation study, The Lancet Infectious Diseases, doi:10.1016/S1473-3099(24)00353-0.
6.
Kim et al., Investigating the Safety Profile of Fast‐Track COVID‐19 Drugs Using the FDA Adverse Event Reporting System Database: A Comparative Observational Study, Pharmacoepidemiology and Drug Safety, doi:10.1002/pds.70043.
7.
Leo et al., Hepatocellular liver injury in hospitalized patients affected by COVID-19: Presence of different risk factors at different time points, Digestive and Liver Disease, doi:10.1016/j.dld.2021.12.014.
8.
Briciu et al., Evolving Clinical Manifestations and Outcomes in COVID-19 Patients: A Comparative Analysis of SARS-CoV-2 Variant Waves in a Romanian Hospital Setting, Pathogens, doi:10.3390/pathogens12121453.
9.
Muntean et al., Effects of COVID-19 on the Liver and Mortality in Patients with SARS-CoV-2 Pneumonia Caused by Delta and Non-Delta Variants: An Analysis in a Single Centre, Pharmaceuticals, doi:10.3390/ph17010003.
10.
Petrov et al., The Effect of Potentially Hepatotoxic Medicinal Products on Alanine Transaminase Levels in COVID-19 Patients: A Case–Control Study, Safety and Risk of Pharmacotherapy, doi:10.30895/2312-7821-2025-458.
11.
Negru et al., Comparative Pharmacovigilance Analysis of Approved and Repurposed Antivirals for COVID-19: Insights from EudraVigilance Data, Biomedicines, doi:10.3390/biomedicines13061387.
12.
Cheng et al., Cardiovascular Safety of COVID-19 Treatments: A Disproportionality Analysis of Adverse Event Reports from the WHO VigiBase, Infectious Diseases and Therapy, doi:10.1007/s40121-025-01225-z.
Kawther et al., 9 Sep 2024, retrospective, Iraq, peer-reviewed, 6 authors, study period December 2020 - December 2021.
Antiviral drug treatment profiles and clinical outcomes of COVID-19 patients at public hospitals in Erbil city
Advanced medical journal, doi:10.56056/amj.2024.273
Background & objectives: The World Health Organization has identified COVID-19 as a rapidly spreading global disease. Some antiviral drugs have shown promising efficacy in treating COVID-19. This study aims to identify the effects of antiviral drugs and compare them with other therapies in COVID-19 patients, while reviewing the clinical outcomes of these treatments. Methods: This observational retrospective case study included 451 COVID-19 patients, comprising 57.0% males and 43% females, conducted in Rizgari, Erbil, at Central Emergency, Rozhawa Emergency, and Emirate Hospitals over one year from December 2020 to December 2021. COVID-19 cases were confirmed using reverse transcriptase polymerase-chain reaction (RT-PCR) assays, and treatment followed the WHO guidelines, involving antivirals (Remdesivir, Favipiravir), broad-spectrum antibiotics (levofloxacin, azithromycin, ceftriaxone, meropenem, imipenem), and supportive treatment with Becozym (Vitamins B1 + B2 + B3 + B5 + B6). Data were recorded in the statistical department of the hospitals.
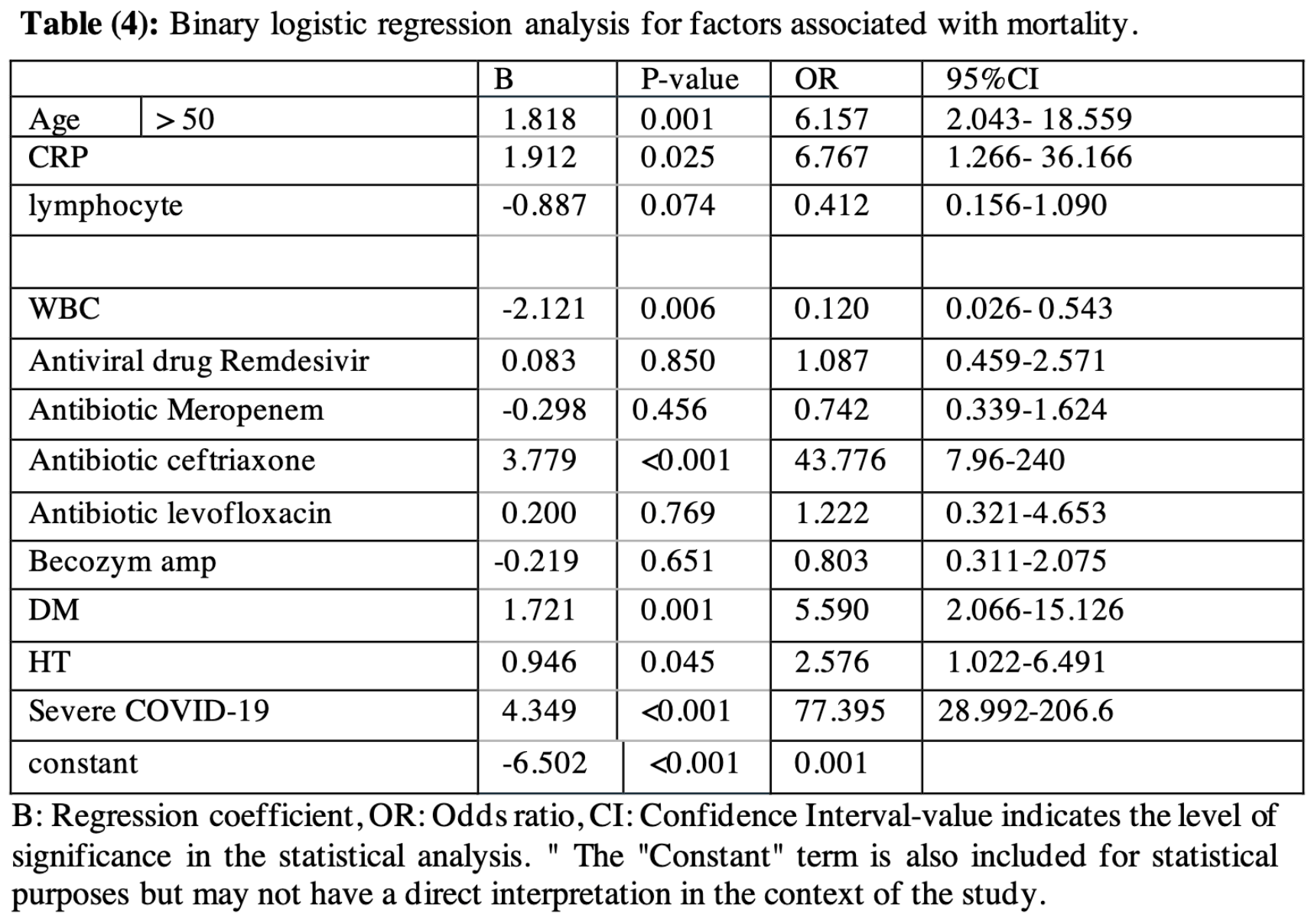
Results: The total age range of the 451 patients was 95 (18-113) with a mean ± SD of 59.408 ± 18.26 years. The death rate was 22.39%. A majority of the survival patients were in the young age group (95.1%), while the death rate was higher in the old age group (more than 75 years). The death rate of patients treated with antiviral drug Remdesivir was 15.30%, while it was 37.93%, 73.45%, 15.25%, and 14.15% in patients on levofloxacin, ceftriaxone, meropenem, and Becozyme, espectively. Logistic regression analysis did not show any role of treatments in decreasing mortality. Conclusions: Significant differences were observed in clinical outcomes; the majority of surviving patients were in the young age group, while older COVID-19 patients had worse illnesses and treatment outcomes. Diabetes and hypertension were significant predictors of COVID-19 mortality. Although Remdesivir treatment showed a statistically significant association between survival and death cohorts, it was not considered a predictor variable for survival. Antibiotics and supplement drugs like Becozyme were also not consid ered predictors of survival for COVID-19 patients.
Conflicts of Interest: None.
References
Adebisi, Ekpenyong, Ntacyabukura, Lowe, Jimoh et al., COVID-19 highlights the need for inclusive responses to public health emergencies in Africa, Am J Trop Med Hyg
Adebisi, Jimoh, Ogunkola, Uwizeyimana, Olayemi et al., The use of antibiotics in COVID-19 management: a rapid review of national treatment guidelines in 10 African countries, Trop Med Health
Beović, Doušak, Ferreira-Coimbra, Antibiotic use in patients with COVID-19: a 'snapshot' Infectious Diseases International Research Initiative (ID-IRI) survey, J Antimicrob Chemother
Bhandari, Shaktawat, Tak, Patel, Shukla et al., Logistic regression analysis to predict mortality risk in COVID-19 patients from routine hematologic parameters, Ibnosina. J Med Biomed Sci
Chen, Zhang, Ju, He, Advances in the research of cytokine storm mechanism induced by Corona virus disease 2019 and the corresponding immunotherapies, Zhonghua Shao Shang Za Zhi
Chowdhary, Tarai, Singh, Sharma, Multidrug-resistant Candida auris infections in critically ill coronavirus disease patients, India, April-July 2020, Emerg Infect Dis
Drożdżal, Rosik, Lechowicz, Machaj, Kotfis et al., FDA approved drugs with pharmacotherapeutic potential for SARS-CoV-2 (COVID-19) therapy, NIH
Gallo Marin, Aghagoli, Lavine, Yang, Siff et al., Predictors of COVID-19 severity: a literature review, Rev Med Virol
Goldman, Lye, Hui, Marks, Bruno et al., Remdesivir for 5 or 10 days in patients with severe Covid-19, NEJM
Guan, Ni, Hu, Liang, Ou et al., Clinical characteristics of coronavirus disease 2019 in China, NEJM
Hasan, Rabbani, Anam, Huq, Polash et al., Impact of high dose of baricitinib in severe COVID-19 pneumonia: a prospective cohort study in Bangladesh, BMC Infectious Diseases
He, Zhao, Dong, Zhuang, Song et al., Effects of severe acute respiratory syndrome (SARS) coronavirus infection on peripheral blood lymphocytes and their subsets, IJID
Hsu, What now for remdesivir, BMJ
Hwaiz, Abdullah, Balaky, Ali, Merza et al., Clinical and hematological characteristics of 300 COVID-19 patients in Erbil, Kurdistan Region, Iraq, Int J Immunopathol Pharmacol
Jafarzadeh, Jafarzadeh, Nozari, Lymophopenia an important immunological abnormality in patients with COVID-19: possible mechanisms, Scand J Immunol
Lippi, Mattiuzzi, Sanchis-Gomar, Henry, Clinical and demographic characteristics of patients dying from COVID-19 in Italy vs China, J. Med. Virol
Mcclave, Sincich, Statistics, None
Mcmahon, Lau, Coldham, Roney, Hagenauer et al., Favipiravir in early symptomatic COVID-19, a randomised placebocontrolled trial, EClinicalMedicine
Nih, Coronavirus disease 2019 (COVID-19) treatment guidelines
Qin, Zhou, Hu, Zhang, Yang et al., Dysregulation of Immune Response in Patients with Coronavirus 2019 (COVID-19) in Wuhan, China, Clin Infect Dis
Rawson, Moore, Zhu, Ranganathan, Skolimowska et al., Bacterial and fungal coinfection in individuals with coronavirus: a rapid review to support COVID-19 antimicrobial prescribing, Clin Infect Dis
Robinson, Liew, Tanner, Grainger, Dwek et al., COVID-19 therapeutics: Challenges and directions for the future, Proc Natl Acad Sci
Satturwar, Fowkes, Farver, Wilson, Eccher et al., Postmortem findings associated with SARS-CoV-2: systematic review and meta-analysis, Am J Surg Pathol
Smith, Dodds, Bentley, Yeo, Rayner, krd factor in repurposing antivirals for COVID-19, doi:10.56056/amj.2024.273https://amj.khcms.edu
Srivastava, Singh, Drug repurposing in COVID-19: a review with past, present and future, Metabolism Open
Wang, Hu, Hu, Zhu, Liu et al., Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China, JAMA
Wiersinga, Rhodes, Cheng, Peacock, Prescott, Pathophysiology, transmission, diagnosis, and treatment of coronavirus disease 2019 (COVID-19): a review, JAMA
Xu, Dong, An, Lv, Yin et al., Clinical and computed tomographic imaging features of novel coronavirus pneumonia caused by SARS-CoV-2, J. Infect
Zhou, Yang, Dong, Lv, Shen et al., Comorbidities and the risk of severe or fatal outcomes associated with coronavirus disease 2019: A systematic review and meta-analysis, IJID
Zhou, Yu, Du, Fan, Liu et al., Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study, Lancet
Zhu, Feng, Jiang, Mi, Yang et al., Correlation between white blood cell count at admission and mortality in COVID-19 patients: a retrospective study, BMC Infectious Diseases
Zhu, Feng, Jiang, Yang, Zhao, Correlation between white blood cell count at admission and mortality in COVID-19 patients: a retrospective study, BMC Infect DisBMC
DOI record:
{
"DOI": "10.56056/amj.2024.273",
"ISSN": [
"2958-8979",
"2957-3580"
],
"URL": "http://dx.doi.org/10.56056/amj.2024.273",
"abstract": "<jats:p>ackground & objectives: The World Health Organization has identified COVID-19 as a rapidly spreading global disease. Some antiviral drugs have shown promising efficacy in treating COVID-19. This study aims to identify the effects of antiviral drugs and compare them with other therapies in COVID-19 patients, while reviewing the clinical outcomes of these treatments. Methods: This observational retrospective case study included 451 COVID-19 patients, comprising 57.0% males and 43% females, conducted in Rizgari, Erbil, at Central Emergency, Rozhawa Emergency, and Emirate Hospitals over one year from December 2020 to December 2021. COVID-19 cases were confirmed using reverse transcriptase polymerase-chain reaction (RT-PCR) assays, and treatment followed the WHO guidelines, involving antivirals (Remdesivir, Favipiravir), broad-spectrum antibiotics (levofloxacin, azithromycin, ceftriaxone, meropenem, imipenem), and supportive treatment with Becozym (Vitamins B1 + B2 + B3 + B5 + B6). Data were recorded in the statistical department of the hospitals. Results: The total age range of the 451 patients was 95 (18-113) with a mean ± SD of 59.408 ± 18.26 years. The death rate was 22.39%. A majority of the survival patients were in the young age group (95.1%), while the death rate was higher in the old age group (more than 75 years). The death rate of patients treated with antiviral drug Remdesivir was 15.30%, while it was 37.93%, 73.45%, 15.25%, and 14.15% in patients on levofloxacin, ceftriaxone, meropenem, and Becozyme, espectively. Logistic regression analysis did not show any role of treatments in decreasing mortality. Conclusions: Significant differences were observed in clinical outcomes; the majority of surviving patients were in the young age group, while older COVID-19 patients had worse illnesses and treatment outcomes. Diabetes and hypertension were significant predictors of COVID-19 mortality. Although Remdesivir treatment showed a statistically significant association between survival and death cohorts, it was not considered a predictor variable for survival. Antibiotics and supplement drugs like Becozyme were also not considered predictors of survival for COVID-19 patients.</jats:p>",
"author": [
{
"affiliation": [],
"name": "Trainee at Infection disease control department of public health, Kurdistan higher council for medical specialties, Rizghary Hospital, Erbil city-Kurdistan region/Iraq",
"sequence": "first"
},
{
"affiliation": [],
"family": "Kawther",
"given": "Ronia Shawksat",
"sequence": "first"
},
{
"affiliation": [],
"family": "Ismael",
"given": "Sherzad Ali",
"sequence": "additional"
},
{
"affiliation": [],
"name": "Assistant Professor in Community Medicine,Chairman of Public Health council, Kurdistan higher council for medical specialties, Erbil City-Kurdistan region/Iraq",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Hassan",
"given": "Maaroof Tahseen",
"sequence": "additional"
},
{
"affiliation": [],
"name": "Assistant Professor in Community Medicine. Program Director of Infection Disease Control Department, Deputy President of Kurdistan higher council for medical specialties, Erbil city-Kurdistan region/Iraq.",
"sequence": "additional"
}
],
"container-title": "Advanced medical journal",
"container-title-short": "adv.med.j.",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2024,
9,
9
]
],
"date-time": "2024-09-09T08:15:43Z",
"timestamp": 1725869743000
},
"deposited": {
"date-parts": [
[
2024,
9,
9
]
],
"date-time": "2024-09-09T08:15:46Z",
"timestamp": 1725869746000
},
"indexed": {
"date-parts": [
[
2024,
9,
10
]
],
"date-time": "2024-09-10T00:24:05Z",
"timestamp": 1725927845673
},
"is-referenced-by-count": 0,
"issue": "3",
"issued": {
"date-parts": [
[
2024,
9,
9
]
]
},
"journal-issue": {
"issue": "3",
"published-online": {
"date-parts": [
[
2024,
9,
9
]
]
},
"published-print": {
"date-parts": [
[
2024,
9,
9
]
]
}
},
"member": "35163",
"original-title": [],
"page": "17-25",
"prefix": "10.56056",
"published": {
"date-parts": [
[
2024,
9,
9
]
]
},
"published-online": {
"date-parts": [
[
2024,
9,
9
]
]
},
"published-print": {
"date-parts": [
[
2024,
9,
9
]
]
},
"publisher": "Kurdistan Higher Council of Medical Specialties",
"reference-count": 0,
"references-count": 0,
"relation": {},
"resource": {
"primary": {
"URL": "https://amj.khcms.edu.krd/index.php/main/article/view/473"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"title": "Antiviral drug treatment profiles and clinical outcomes of COVID-19 patients at public hospitals in Erbil city.",
"type": "journal-article",
"volume": "9"
}