Clinical Course and Outcome of COVID-19 Acute Respiratory Distress Syndrome: Data From a National Repository
et al., Journal of Intensive Care Medicine, doi:10.1177/0885066621994476, Oct 2020 (preprint)
Retrospective 7,816 Veterans Affairs hospitalized patients showing lower mortality with remdesivir.
Gérard, Zhou, Wu, Kamo, Choi, Kim show increased risk of acute kidney injury, Leo, Briciu, Muntean, Petrov show increased risk of liver injury, and Negru, Cheng, Mohammed, Kwok show increased risk of cardiac disorders with remdesivir.
Remdesivir efficacy disappears with longer
followup. Mixed-effects meta-regression of efficacy as a function of
followup duration across all remdesivir studies shows decreasing efficacy with
longer followup15. This may reflect
antiviral efficacy being offset by serious adverse effects of treatment.
Standard of Care (SOC) for COVID-19 in the study country,
the USA, is very poor with very low average efficacy for approved treatments16.
Only expensive, high-profit treatments were approved for early treatment. Low-cost treatments were excluded, reducing the probability of early treatment due to access and cost barriers, and eliminating complementary and synergistic benefits seen with many low-cost treatments.
This may explain in part the very high mortality seen in this study.
Results may differ in countries with improved SOC.
This study is excluded in the after exclusion results of meta-analysis:
very late stage, >50% on oxygen/ventilation at baseline; substantial unadjusted confounding by indication likely; significant confounding by contraindications possible.
|
risk of death, 29.0% lower, HR 0.71, p = 0.03, treatment 63 of 219 (28.8%), control 202 of 424 (47.6%), NNT 5.3, adjusted per study, multivariable.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
1.
Gérard et al., Remdesivir and Acute Renal Failure: A Potential Safety Signal From Disproportionality Analysis of the WHO Safety Database, Clinical Pharmacology & Therapeutics, doi:10.1002/cpt.2145.
2.
Zhou et al., Acute Kidney Injury and Drugs Prescribed for COVID-19 in Diabetes Patients: A Real-World Disproportionality Analysis, Frontiers in Pharmacology, doi:10.3389/fphar.2022.833679.
3.
Wu et al., Acute Kidney Injury Associated With Remdesivir: A Comprehensive Pharmacovigilance Analysis of COVID-19 Reports in FAERS, Frontiers in Pharmacology, doi:10.3389/fphar.2022.692828.
4.
Kamo et al., Association of Antiviral Drugs for the Treatment of COVID-19 With Acute Renal Failure, In Vivo, doi:10.21873/invivo.13637.
5.
Choi et al., Comparative effectiveness of combination therapy with nirmatrelvir–ritonavir and remdesivir versus monotherapy with remdesivir or nirmatrelvir–ritonavir in patients hospitalised with COVID-19: a target trial emulation study, The Lancet Infectious Diseases, doi:10.1016/S1473-3099(24)00353-0.
6.
Kim et al., Investigating the Safety Profile of Fast‐Track COVID‐19 Drugs Using the FDA Adverse Event Reporting System Database: A Comparative Observational Study, Pharmacoepidemiology and Drug Safety, doi:10.1002/pds.70043.
7.
Leo et al., Hepatocellular liver injury in hospitalized patients affected by COVID-19: Presence of different risk factors at different time points, Digestive and Liver Disease, doi:10.1016/j.dld.2021.12.014.
8.
Briciu et al., Evolving Clinical Manifestations and Outcomes in COVID-19 Patients: A Comparative Analysis of SARS-CoV-2 Variant Waves in a Romanian Hospital Setting, Pathogens, doi:10.3390/pathogens12121453.
9.
Muntean et al., Effects of COVID-19 on the Liver and Mortality in Patients with SARS-CoV-2 Pneumonia Caused by Delta and Non-Delta Variants: An Analysis in a Single Centre, Pharmaceuticals, doi:10.3390/ph17010003.
10.
Petrov et al., The Effect of Potentially Hepatotoxic Medicinal Products on Alanine Transaminase Levels in COVID-19 Patients: A Case–Control Study, Safety and Risk of Pharmacotherapy, doi:10.30895/2312-7821-2025-458.
11.
Negru et al., Comparative Pharmacovigilance Analysis of Approved and Repurposed Antivirals for COVID-19: Insights from EudraVigilance Data, Biomedicines, doi:10.3390/biomedicines13061387.
12.
Cheng et al., Cardiovascular Safety of COVID-19 Treatments: A Disproportionality Analysis of Adverse Event Reports from the WHO VigiBase, Infectious Diseases and Therapy, doi:10.1007/s40121-025-01225-z.
13.
Mohammed et al., Bradycardia associated with remdesivir treatment in coronavirus disease 2019 patients: A propensity score-matched analysis, Medicine, doi:10.1097/MD.0000000000044501.
El-Solh et al., 20 Oct 2020, retrospective, database analysis, USA, peer-reviewed, 5 authors.
CLINICAL COURSE AND OUTCOME OF COVID-19 ACUTE RESPIRATORY DISTRESS SYNDROME: DATA FROM A NATIONAL REPOSITORY
doi:10.1101/2020.10.16.20214130
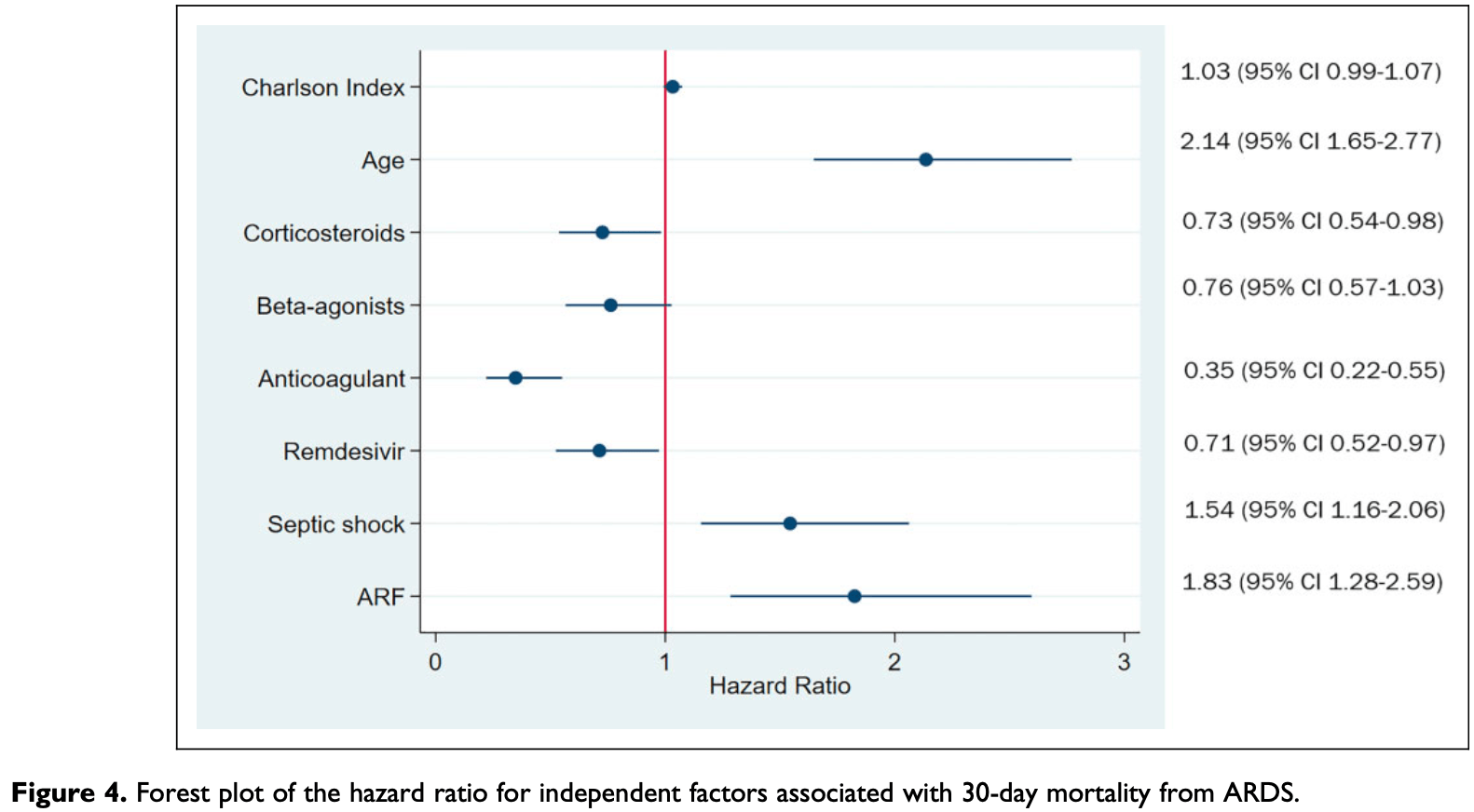
Background: Mortality attributable to coronavirus disease-19 (COVID-19) 2 infection occurs mainly through the development of viral pneumonia-induced acute respiratory distress syndrome (ARDS). Research Question: The objective of the study is to delineate the clinical profile, predictors of disease progression, and 30-day mortality from ARDS using the Veterans Affairs Corporate Data Warehouse. Study Design and Methods: Analysis of a historical cohort of 7,816 hospitalized patients with confirmed COVID-19 infection between January 1, 2020, and August 1, 2020. Main outcomes were progression to ARDS and 30-day mortality from ARDS, respectively. Results: The cohort was comprised predominantly of men (94.5%) with a median age of 69 years (interquartile range [IQR] 60-74 years). 2,184 (28%) were admitted to the intensive care unit and 643 (29.4%) were diagnosed with ARDS. The median Charlson Index was 3 (IQR 1-5). Independent predictors of progression to ARDS were body mass index (BMI)≥ 40 kg/m 2 , diabetes, lymphocyte counts<700x109/L, LDH>450 U/L, ferritin >862 ng/ml, C-reactive protein >11 mg/dL, and Ddimer >1.5 ug/ml. In contrast, the use of an anticoagulant lowered the risk of developing ARDS (OR 0.66 [95% CI 0.49-0.89]. Crude 30-day mortality rate from ARDS was 41% (95% CI 38%-45%). Risk of death from ARDS was significantly higher in those who developed acute renal failure and septic shock. Use of an anticoagulant was associated with two-fold reduction in mortality. Survival benefit was observed in patients who received corticosteroids and/or remdesivir but there was no advantage of combination therapy over either agent alone. Conclusions: Among those hospitalized for COVID-19, nearly one in ten progressed to ARDS. Septic shock, and acute renal failure are the leading causes of death in these patients. Treatment with either remdesivir and corticosteroids reduced the risk of mortality from ARDS. All hospitalized patients with COVID-19 should be placed at a minimum on prophylactic doses of anticoagulation. .
References
Anderson, Geleris, Anderson, Body Mass Index and Risk for Intubation or Death in SARS-CoV-2 Infection: A Retrospective Cohort Study, Ann Intern Med
Angus, Derde, Effect of Hydrocortisone on Mortality and Organ Support in Patients With Severe COVID
Azoulay, Fartoukh, Darmon, Increased mortality in patients with severe SARS-CoV-2 infection admitted within seven days of disease onset, Intensive Care Med
Beigel, Tomashek, Dodd, Remdesivir for the Treatment of Covid-19 -Preliminary Report, N Engl J Med
Charlson, Pompei, Ales, Mackenzie, A new method of classifying prognostic comorbidity in longitudinal studies: development and validation, J Chronic Dis
Chen, Liang, Jiang, Risk Factors of Fatal Outcome in Hospitalized Subjects With Coronavirus Disease 2019 From a Nationwide Analysis in China, Chest
Chen, Wu, Chen, Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study, BMJ. Mar
Dickerson, The obesity paradox in the ICU: real or not?, Crit Care
Feld, Tremblay, Thibaud, Kessler, Naymagon, Ferritin levels in patients with COVID-19: A poor predictor of mortality and hemophagocytic lymphohistiocytosis, Int J Lab Hematol
Fezeu, Julia, Henegar, Obesity is associated with higher risk of intensive care unit admission and death in influenza A (H1N1) patients: a systematic review and metaanalysis, Obes Rev
Fihn, Francis, Clancy, Insights from advanced analytics at the Veterans Health Administration, Health Aff (Millwood)
Fragkou, Belhadi, Peiffer-Smadja, Review of trials currently testing treatment and prevention of COVID-19, Clin Microbiol Infect
Garcia, Fumeaux, Guerci, Prognostic factors associated with mortality risk and disease progression in 639 critically ill patients with COVID-19 in Europe: Initial report of the international RISC-19-ICU prospective observational cohort, EClinicalMedicine
Grasselli, Zangrillo, Zanella, Baseline Characteristics and Outcomes of 1591 Patients Infected With SARS-CoV-2 Admitted to ICUs of the Lombardy Region, Italy, JAMA
Group, Horby, Lim, Dexamethasone in Hospitalized Patients with Covid-19 -Preliminary Report, N Engl J Med
Huang, Wang, Li, Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China, Lancet
Hussman, Cellular and Molecular Pathways of COVID-19 and Potential Points of Therapeutic Intervention, Front Pharmacol
Jang, Hur, Choi, Hong, Lee et al., Prognostic Factors for Severe Coronavirus Disease 2019 in Daegu, Korea, J Korean Med Sci
Jose, Manuel, COVID-19 cytokine storm: the interplay between inflammation and coagulation, Lancet Respir Med. Jun
Kruglikov, Scherer, The Role of Adipocytes and Adipocyte-Like Cells in the Severity of COVID-19 Infections, Obesity (Silver Spring)
Lighter, Phillips, Hochman, Obesity in Patients Younger Than 60 Years Is a Risk Factor for COVID-19 Hospital Admission, Clin Infect Dis
Louie, Jean, Acosta, Samuel, Matyas et al., A review of adult mortality due to 2009 pandemic (H1N1) influenza A in California, PLoS One
Mehta, Mcauley, Brown, COVID-19: consider cytokine storm syndromes and immunosuppression, Lancet. Mar
Moores, Tritschler, Brosnahan, Prevention, Diagnosis, and Treatment of VTE in Patients With Coronavirus Disease 2019: CHEST Guideline and Expert Panel Report, Chest
Nadkarni, Bagiella, Anticoagulation, Mortality, Bleeding and Pathology Among Patients Hospitalized with COVID-19: A Single Health System Study, J Am Coll Cardiol
Organization, International Statistical Classification of Diseases, Tenth Revision
Pan, Cheng, Cao, A Predicting Nomogram for Mortality in Patients With COVID-19, Front Public Health
Petrilli, Jones, Yang, Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in New York City: prospective cohort study, BMJ
Poggiali, Zaino, Immovilli, Lactate dehydrogenase and C-reactive protein as predictors of respiratory failure in CoVID-19 patients, Clin Chim Acta
Rello, Storti, Belliato, Serrano, Clinical phenotypes of SARS-CoV-2: implications for clinicians and researchers, Eur Respir J
Simonnet, Chetboun, Poissy, High Prevalence of Obesity in Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2) Requiring Invasive Mechanical Ventilation, Obesity
Sinha, Matthay, Calfee, Is a "Cytokine Storm" Relevant to COVID-19?, JAMA Intern Med
Sohn, Arnold, Maynard, Hynes, Accuracy and completeness of mortality data in the Department of Veterans Affairs, Popul Health Metr
Tang, Li, Wang, Sun, Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia, J Thromb Haemost
Tomazini, Maia, Cavalcanti, Effect of Dexamethasone on Days Alive and Ventilator-Free in Patients With Moderate or Severe Acute Respiratory Distress Syndrome and COVID-19: The CoDEX Randomized Clinical Trial, JAMA
Wang, Hu, Hu, Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China, JAMA. Mar
Wang, Zuo, Liu, Clinical and laboratory predictors of in-hospital mortality in patients with COVID-19: a cohort study in Wuhan, China, Clin Infect Dis
Wu, Chen, Cai, Risk Factors Associated With Acute Respiratory Distress Syndrome and Death in Patients With Coronavirus Disease 2019 Pneumonia in Wuhan, China, JAMA Intern Med
Zhang, Tan, Ling, Viral and host factors related to the clinical outcome of COVID-19, Nature. Jul
DOI record:
{
"DOI": "10.1177/0885066621994476",
"ISSN": [
"0885-0666",
"1525-1489"
],
"URL": "http://dx.doi.org/10.1177/0885066621994476",
"abstract": "<jats:sec><jats:title>Background:</jats:title><jats:p> Mortality attributable to coronavirus disease-19 (COVID-19) 2 infection occurs mainly through the development of viral pneumonia-induced acute respiratory distress syndrome (ARDS). </jats:p></jats:sec><jats:sec><jats:title>Research Question:</jats:title><jats:p> The objective of the study is to delineate the clinical profile, predictors of disease progression, and 30-day mortality from ARDS using the Veterans Affairs Corporate Data Warehouse. </jats:p></jats:sec><jats:sec><jats:title>Study Design and Methods:</jats:title><jats:p> Analysis of a historical cohort of 7,816 hospitalized patients with confirmed COVID-19 infection between January 1, 2020, and August 1, 2020. Main outcomes were progression to ARDS and 30-day mortality from ARDS, respectively. </jats:p></jats:sec><jats:sec><jats:title>Results:</jats:title><jats:p> The cohort was comprised predominantly of men (94.5%) with a median age of 69 years (interquartile range [IQR] 60-74 years). 2,184 (28%) were admitted to the intensive care unit and 643 (29.4%) were diagnosed with ARDS. The median Charlson Index was 3 (IQR 1-5). Independent predictors of progression to ARDS were body mass index (BMI) ≥40 kg/m<jats:sup>2</jats:sup>, diabetes, lymphocyte counts <700 × 109/L, LDH >450 U/L, ferritin >862 ng/ml, C-reactive protein >11 mg/dL, and D-dimer >1.5 ug/ml. In contrast, the use of an anticoagulant lowered the risk of developing ARDS (OR 0.66 [95% CI 0.49-0.89]. Crude 30-day mortality rate from ARDS was 41% (95% CI 38%-45%). Risk of death from ARDS was significantly higher in those who developed acute renal failure and septic shock. Use of an anticoagulant was associated with 2-fold reduction in mortality. Survival benefit was observed in patients who received corticosteroids and/or remdesivir but there was no advantage of combination therapy over either agent alone. </jats:p></jats:sec><jats:sec><jats:title>Conclusions:</jats:title><jats:p> Among those hospitalized for COVID-19, nearly 1 in 10 progressed to ARDS. Septic shock, and acute renal failure are the leading causes of death in these patients. Treatment with either remdesivir and corticosteroids reduced the risk of mortality from ARDS. All hospitalized patients with COVID-19 should be placed at a minimum on prophylactic doses of anticoagulation. </jats:p></jats:sec>",
"alternative-id": [
"10.1177/0885066621994476"
],
"author": [
{
"ORCID": "http://orcid.org/0000-0003-4237-8776",
"affiliation": [
{
"name": "VA Western New York Healthcare System, Buffalo, NY, USA"
},
{
"name": "Division of Pulmonary, Critical Care, and Sleep Medicine, Department of Medicine, Buffalo, NY, USA"
},
{
"name": "Department of Epidemiology and Environmental Health, School of Medicine and Biomedical Sciences, School of Public Health and Health Professions, State University of New York, Buffalo, NY, USA"
}
],
"authenticated-orcid": false,
"family": "El-Solh",
"given": "Ali A.",
"sequence": "first"
},
{
"affiliation": [
{
"name": "Memphis VA Medical Center, Memphis, TN, USA"
}
],
"family": "Meduri",
"given": "Umberto G.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "VA Western New York Healthcare System, Buffalo, NY, USA"
}
],
"family": "Lawson",
"given": "Yolanda",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "VA Western New York Healthcare System, Buffalo, NY, USA"
}
],
"family": "Carter",
"given": "Michael",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "VA Western New York Healthcare System, Buffalo, NY, USA"
}
],
"family": "Mergenhagen",
"given": "Kari A.",
"sequence": "additional"
}
],
"container-title": "Journal of Intensive Care Medicine",
"container-title-short": "J Intensive Care Med",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"journals.sagepub.com"
]
},
"created": {
"date-parts": [
[
2021,
3,
9
]
],
"date-time": "2021-03-09T09:31:10Z",
"timestamp": 1615282270000
},
"deposited": {
"date-parts": [
[
2021,
5,
21
]
],
"date-time": "2021-05-21T06:39:20Z",
"timestamp": 1621579160000
},
"indexed": {
"date-parts": [
[
2023,
7,
29
]
],
"date-time": "2023-07-29T02:15:42Z",
"timestamp": 1690596942762
},
"is-referenced-by-count": 13,
"issue": "6",
"issued": {
"date-parts": [
[
2021,
3,
9
]
]
},
"journal-issue": {
"issue": "6",
"published-print": {
"date-parts": [
[
2021,
6
]
]
}
},
"language": "en",
"license": [
{
"URL": "http://journals.sagepub.com/page/policies/text-and-data-mining-license",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
3,
9
]
],
"date-time": "2021-03-09T00:00:00Z",
"timestamp": 1615248000000
}
}
],
"link": [
{
"URL": "http://journals.sagepub.com/doi/pdf/10.1177/0885066621994476",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "http://journals.sagepub.com/doi/full-xml/10.1177/0885066621994476",
"content-type": "application/xml",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "http://journals.sagepub.com/doi/pdf/10.1177/0885066621994476",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "179",
"original-title": [],
"page": "664-672",
"prefix": "10.1177",
"published": {
"date-parts": [
[
2021,
3,
9
]
]
},
"published-online": {
"date-parts": [
[
2021,
3,
9
]
]
},
"published-print": {
"date-parts": [
[
2021,
6
]
]
},
"publisher": "SAGE Publications",
"reference": [
{
"DOI": "10.1007/s00134-020-06202-3",
"doi-asserted-by": "publisher",
"key": "bibr3-0885066621994476"
},
{
"DOI": "10.1001/jamainternmed.2020.0994",
"doi-asserted-by": "publisher",
"key": "bibr4-0885066621994476"
},
{
"DOI": "10.1038/s41586-020-2355-0",
"doi-asserted-by": "publisher",
"key": "bibr5-0885066621994476"
},
{
"DOI": "10.1016/S0140-6736(20)30628-0",
"doi-asserted-by": "publisher",
"key": "bibr6-0885066621994476"
},
{
"DOI": "10.1001/jamainternmed.2020.3313",
"doi-asserted-by": "publisher",
"key": "bibr7-0885066621994476"
},
{
"DOI": "10.1183/13993003.01028-2020",
"doi-asserted-by": "publisher",
"key": "bibr8-0885066621994476"
},
{
"DOI": "10.1016/j.cmi.2020.05.019",
"doi-asserted-by": "publisher",
"key": "bibr9-0885066621994476"
},
{
"DOI": "10.1016/j.eclinm.2020.100449",
"doi-asserted-by": "publisher",
"key": "bibr10-0885066621994476"
},
{
"DOI": "10.3346/jkms.2020.35.e209",
"doi-asserted-by": "publisher",
"key": "bibr11-0885066621994476"
},
{
"DOI": "10.1377/hlthaff.2014.0054",
"doi-asserted-by": "publisher",
"key": "bibr12-0885066621994476"
},
{
"author": "Organization",
"key": "bibr14-0885066621994476",
"volume-title": "International Statistical Classification of Diseases, Tenth Revision (ICD-10)",
"year": "1992"
},
{
"DOI": "10.1016/0021-9681(87)90171-8",
"doi-asserted-by": "publisher",
"key": "bibr15-0885066621994476"
},
{
"DOI": "10.1186/1478-7954-4-2",
"doi-asserted-by": "publisher",
"key": "bibr16-0885066621994476"
},
{
"DOI": "10.1111/ijlh.13309",
"doi-asserted-by": "publisher",
"key": "bibr17-0885066621994476"
},
{
"DOI": "10.1016/j.cca.2020.06.012",
"doi-asserted-by": "publisher",
"key": "bibr18-0885066621994476"
},
{
"DOI": "10.1001/jama.2020.5394",
"doi-asserted-by": "publisher",
"key": "bibr19-0885066621994476"
},
{
"DOI": "10.1136/bmj.m1091",
"doi-asserted-by": "publisher",
"key": "bibr20-0885066621994476"
},
{
"DOI": "10.7326/M20-3214",
"doi-asserted-by": "publisher",
"key": "bibr21-0885066621994476"
},
{
"DOI": "10.1002/oby.22831",
"doi-asserted-by": "publisher",
"key": "bibr22-0885066621994476"
},
{
"DOI": "10.1093/cid/ciaa415",
"doi-asserted-by": "publisher",
"key": "bibr23-0885066621994476"
},
{
"DOI": "10.1136/bmj.m1966",
"doi-asserted-by": "publisher",
"key": "bibr24-0885066621994476"
},
{
"DOI": "10.1111/j.1467-789X.2011.00864.x",
"doi-asserted-by": "publisher",
"key": "bibr26-0885066621994476"
},
{
"DOI": "10.1371/journal.pone.0018221",
"doi-asserted-by": "publisher",
"key": "bibr27-0885066621994476"
},
{
"DOI": "10.1002/oby.22856",
"doi-asserted-by": "publisher",
"key": "bibr28-0885066621994476"
},
{
"DOI": "10.1186/cc12715",
"doi-asserted-by": "publisher",
"key": "bibr29-0885066621994476"
},
{
"DOI": "10.1001/jama.2020.1585",
"doi-asserted-by": "publisher",
"key": "bibr30-0885066621994476"
},
{
"DOI": "10.1016/S0140-6736(20)30183-5",
"doi-asserted-by": "publisher",
"key": "bibr31-0885066621994476"
},
{
"DOI": "10.1093/cid/ciaa538",
"doi-asserted-by": "publisher",
"key": "bibr32-0885066621994476"
},
{
"DOI": "10.3389/fpubh.2020.00461",
"doi-asserted-by": "publisher",
"key": "bibr33-0885066621994476"
},
{
"DOI": "10.1016/j.chest.2020.04.010",
"doi-asserted-by": "publisher",
"key": "bibr34-0885066621994476"
},
{
"DOI": "10.3389/fphar.2020.01169",
"doi-asserted-by": "publisher",
"key": "bibr35-0885066621994476"
},
{
"DOI": "10.1016/S2213-2600(20)30216-2",
"doi-asserted-by": "publisher",
"key": "bibr36-0885066621994476"
},
{
"DOI": "10.1111/jth.14768",
"doi-asserted-by": "publisher",
"key": "bibr37-0885066621994476"
},
{
"DOI": "10.1016/j.jacc.2020.08.041",
"doi-asserted-by": "publisher",
"key": "bibr38-0885066621994476"
},
{
"DOI": "10.1016/j.chest.2020.05.559",
"doi-asserted-by": "publisher",
"key": "bibr39-0885066621994476"
},
{
"author": "Group RC",
"first-page": "NEJMoa2021436",
"journal-title": "N Engl J Med",
"key": "bibr40-0885066621994476",
"year": "2020"
},
{
"DOI": "10.1001/jama.2020.17021",
"doi-asserted-by": "publisher",
"key": "bibr41-0885066621994476"
},
{
"DOI": "10.1001/jama.2020.17022",
"doi-asserted-by": "publisher",
"key": "bibr42-0885066621994476"
},
{
"author": "Beigel JH",
"first-page": "994",
"issue": "10",
"journal-title": "N Engl J Med",
"key": "bibr44-0885066621994476",
"volume": "383",
"year": "2020"
}
],
"reference-count": 39,
"references-count": 39,
"relation": {},
"resource": {
"primary": {
"URL": "http://journals.sagepub.com/doi/10.1177/0885066621994476"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Critical Care and Intensive Care Medicine"
],
"subtitle": [],
"title": "Clinical Course and Outcome of COVID-19 Acute Respiratory Distress Syndrome: Data From a National Repository",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1177/sage-journals-update-policy",
"volume": "36"
}
solh