Vitamin D Supplementation and Clinical Outcomes in Severe COVID-19 Patients—Randomized Controlled Trial
et al., Nutrients, doi:10.3390/nu15051234, NCT05384574, Feb 2023
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 136 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Very late stage RCT 155 ICU patients in Croatia with low vitamin D levels, showing no significant differences with 10,000IU cholecalciferol daily. Calcifediol or calcitriol, which avoids several days delay in conversion, may be more successful, especially with this very late stage usage.
The baseline mean age and median WHO scores for the treatment and control groups are both higher than the respective values reported for all patients combined, which is not possible.
The trial was registered after completion in May 2022.
Cholecalciferol was used in this study.
Meta-analysis shows that late stage treatment with calcitriol / calcifediol (or
paricalcitol, alfacalcidol, etc.) is more effective than cholecalciferol: 66% [47‑78%] lower risk vs. 44% [33‑53%] lower risk.
Cholecalciferol requires two hydroxylation steps to become activated - first
in the liver to calcifediol, then in the kidney to calcitriol. Calcitriol,
paricalcitol, and alfacalcidol are active vitamin D analogs that do not
require conversion. This allows them to have more rapid onset of action
compared to cholecalciferol. The time delay for cholecalciferol to increase
serum calcifediol levels can be 2-3 days, and the delay for converting
calcifediol to active calcitriol can be up to 7 days.
This is the 32nd of 40 COVID-19 RCTs for vitamin D, which collectively show efficacy with p=0.0000001.
This is the 113th of 136 COVID-19 controlled studies for vitamin D, which collectively show efficacy with p<0.0000000001.
This study is excluded in the after exclusion results of meta-analysis:
very late stage study using cholecalciferol instead of calcifediol or calcitriol.
|
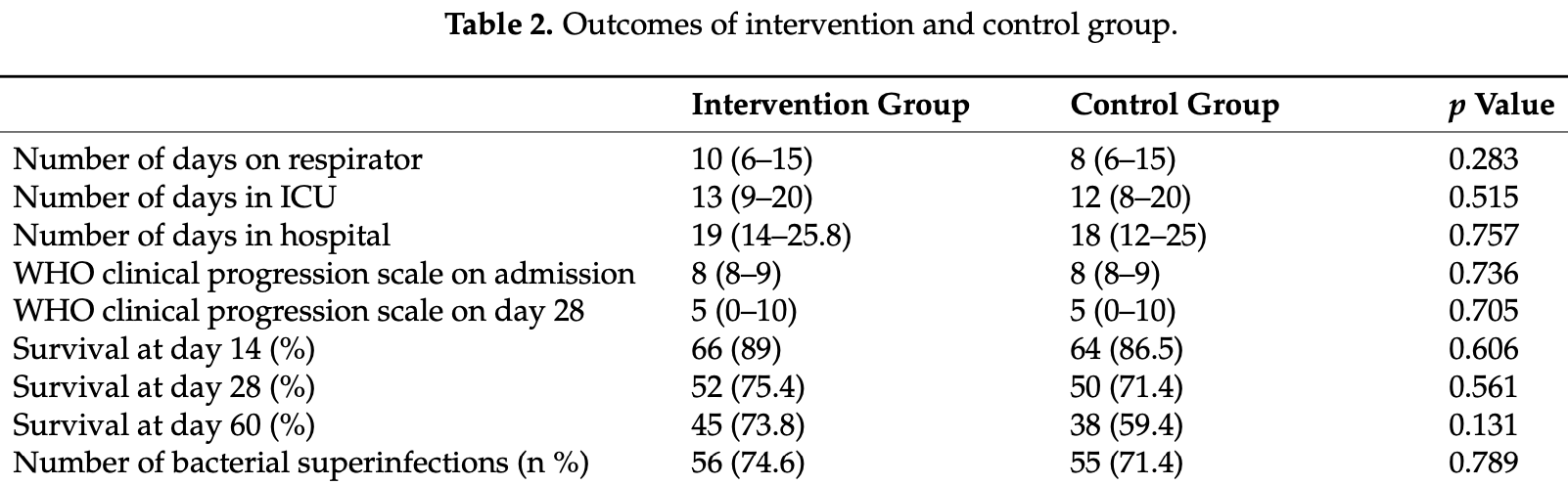
risk of death, 21.0% lower, RR 0.79, p = 0.20, treatment 30 of 75 (40.0%), control 39 of 77 (50.6%), NNT 9.4, day 60.
|
|
risk of death, 12.5% lower, RR 0.87, p = 0.61, treatment 23 of 75 (30.7%), control 27 of 77 (35.1%), NNT 23, day 28.
|
|
risk of death, 28.9% lower, RR 0.71, p = 0.49, treatment 9 of 75 (12.0%), control 13 of 77 (16.9%), NNT 20, day 14.
|
|
WHO score, no change, RR 1.00, p = 0.70, treatment 75, control 77, day 28.
|
|
hospitalization time, 5.6% higher, relative time 1.06, p = 0.76, treatment 75, control 77.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Domazet Bugarin et al., 28 Feb 2023, Randomized Controlled Trial, Croatia, peer-reviewed, 9 authors, study period November 2021 - May 2022, dosage 10,000IU days 1-14, trial NCT05384574 (history).
Contact: lenko.saric@gmail.com (corresponding author).
Vitamin D Supplementation and Clinical Outcomes in Severe COVID-19 Patients—Randomized Controlled Trial
Nutrients, doi:10.3390/nu15051234
COVID-19 symptoms vary from asymptomatic cases to moderate and severe illness with patients needing hospitalization and intensive care treatment. Vitamin D is associated with severity of viral infections and has an immune-modulatory effect in immune response. Observational studies showed a negative association of low vitamin D levels and COVID-19 severity and mortality outcomes. In this study, we aimed to determine whether daily supplementation of vitamin D during intensive care unit (ICU) stay in COVID-19 patients with severe illness affects clinically relevant outcomes. Patients with COVID-19 disease in need of respiratory support admitted to the ICU were eligible for inclusion. Patients with low vitamin D levels were randomized into one of two groups: the intervention group received daily supplementation of vitamin D and the control group did not receive vitamin D supplementation. In total, 155 patients were randomized: 78 into the intervention group and 77 into the control group. There was no statistically significant difference in number of days spent on respiratory support, although the trial was underpowered for the main outcome. There was no difference in any of the secondary outcomes analyzed between two groups. Our study suggests no benefit in vitamin D supplementation to patients with severe COVID-19 disease admitted to the ICU and in need of respiratory support in any of the analyzed outcomes.
References
Ali, Role of vitamin D in preventing of COVID-19 infection, progression and severity, J. Infect. Public Health
Amrein, Hoffmann, Lobmeyr, Martucci, Vitamin D in critical care: Where are we now and what is next?, Curr. Opin. Crit. Care, doi:10.1097/MCC.0000000000000849
Amrein, Papinutti, Mathew, Vila, Parekh, Vitamin D and critical illness: What endocrinology can learn from intensive care and vice versa, Endocr. Connect, doi:10.1530/EC-18-0184
Amrein, Scherkl, Hoffmann, Neuwersch-Sommeregger, Kostenberger et al., deficiency 2.0: An update on the current status worldwide, Eur. J. Clin. Nutr, doi:10.1038/s41430-020-0558-y
Amrein, Schnedl, Holl, Riedl, Christopher et al., Effect of high-dose vitamin D3 on hospital length of stay in critically ill patients with vitamin D deficiency: The VITdAL-ICU randomized clinical trial, JAMA, doi:10.1001/jama.2014.13204
Amrein, Zajic, Schnedl, Waltensdorfer, Fruhwald et al., Vitamin D status and its association with season, hospital and sepsis mortality in critical illness, Crit. Care, doi:10.1186/cc13790
Annweiler, Beaudenon, Gautier, Simon, Dubee et al., COVID-19 and high-dose VITamin D supplementation TRIAL in high-risk older patients (COVIT-TRIAL): Study protocol for a randomized controlled trial, Trials, doi:10.1186/s13063-020-04928-5
Bassatne, Basbous, Chakhtoura, El Zein, Rahme et al., The link between COVID-19 and VItamin D (VIVID): A systematic review and meta-analysis, Metab. Clin. Exp, doi:10.1016/j.metabol.2021.154753
Billington, Burt, Rose, Davison, Gaudet et al., Safety of High-Dose Vitamin D Supplementation: Secondary Analysis of a Randomized Controlled Trial, J. Clin. Endocrinol. Metab, doi:10.1210/clinem/dgz212
Bouillon, Marcocci, Carmeliet, Bikle, White et al., Skeletal and Extraskeletal Actions of Vitamin D: Current Evidence and Outstanding Questions, Endocr. Rev, doi:10.1210/er.2018-00126
Campi, Gennari, Merlotti, Mingiano, Frosali et al., Vitamin D and COVID-19 severity and related mortality: A prospective study in Italy, BMC Infect. Dis, doi:10.1186/s12879-021-06281-7
Cashman, Dowling, Skrabakova, Gonzalez-Gross, Valtuena et al., Vitamin D deficiency in Europe: Pandemic?, Am. J. Clin. Nutr
Christopher, Vitamin D and critical illness outcomes, Curr. Opin. Crit. Care, doi:10.1097/MCC.0000000000000328
Christopher, Vitamin D supplementation in the ICU patient, Curr. Opin. Clin. Nutr. Metab. Care, doi:10.1097/MCO.0000000000000147
Cleveland, Grosse, Shyu, Statistical Models
Cuschieri, The CONSORT statement, Saudi J. Anaesth, doi:10.4103/sja.SJA_559_18
D'ecclesiis, Gavioli, Martinoli, Raimondi, Chiocca et al., Vitamin D and SARS-CoV2 infection, severity and mortality: A systematic review and meta-analysis, PLoS ONE, doi:10.1371/journal.pone.0268396
Da Rocha, Atallah, Aldrighi, Pires, Dos Santos Puga et al., Insufficient evidence for vitamin D use in COVID-19: A rapid systematic review, Int. J. Clin. Pract, doi:10.1111/ijcp.14649
De Haan, Groeneveld, De Geus, Egal, Struijs, Vitamin D deficiency as a risk factor for infection, sepsis and mortality in the critically ill: Systematic review and meta-analysis, Crit. Care, doi:10.1186/s13054-014-0660-4
Fabbri, Infante, Ricordi, Editorial-Vitamin D status: A key modulator of innate immunity and natural defense from acute viral respiratory infections, Eur. Rev. Med. Pharmacol. Sci, doi:10.26355/eurrev_202004_20876
Force, Ranieri, Rubenfeld, Thompson, Ferguson et al., Acute respiratory distress syndrome: The Berlin Definition, JAMA, doi:10.1001/jama.2012.5669
Guven, Gultekin, The effect of high-dose parenteral vitamin D3 on COVID-19-related inhospital mortality in critical COVID-19 patients during intensive care unit admission: An observational cohort study, Eur. J. Clin. Nutr, doi:10.1038/s41430-021-00984-5
Guyatt, Mills, Elbourne, In the era of systematic reviews, does the size of an individual trial still matter, PLoS Med, doi:10.1371/journal.pmed.0050004
Hasanloei, Rahimlou, Eivazloo, Sane, Ayremlou et al., Effect of Oral Versus Intramuscular Vitamin D Replacement on Oxidative Stress and Outcomes in Traumatic Mechanical Ventilated Patients Admitted to Intensive Care Unit, Nutr. Clin. Pract. Off. Publ. Am. Soc. Parenter. Enter. Nutr, doi:10.1002/ncp.10404
Holick, Binkley, Bischoff-Ferrari, Gordon, Hanley et al., Evaluation, treatment, and prevention of vitamin D deficiency: An Endocrine Society clinical practice guideline, J. Clin. Endocrinol. Metab, doi:10.1210/jc.2011-0385
Hollis, Wagner, Clinical review: The role of the parent compound vitamin D with respect to metabolism and function: Why clinical dose intervals can affect clinical outcomes, J. Clin. Endocrinol. Metab, doi:10.1210/jc.2013-2653
Hossein-Nezhad, Holick, Vitamin D for health: A global perspective, Mayo Clin. Proc, doi:10.1016/j.mayocp.2013.05.011
Jolliffe, Camargo, Jr, Sluyter, Aglipay et al., Vitamin D supplementation to prevent acute respiratory infections: Systematic review and meta-analysis of aggregate data from randomised controlled trials, Medrxiv Prepr. Serv. Health Sci, doi:10.1016/S2213-8587(21)00051-6
Kazemi, Mohammadi, Aghababaee, Golzarand, Clark et al., Association of Vitamin D Status with SARS-CoV-2 Infection or COVID-19 Severity: A Systematic Review and Meta-analysis, Adv. Nutr, doi:10.1093/advances/nmab012
Lan, Lai, Chang, Lu, Hung et al., Vitamin D supplementation and the outcomes of critically ill adult patients: A systematic review and meta-analysis of randomized controlled trials, Sci. Rep, doi:10.1038/s41598-020-71271-9
Langlois, ; D'aragon, Manzanares, Vitamin D in the ICU: More sun for critically ill adult patients?, Nutrition, doi:10.1016/j.nut.2018.11.001
Maghbooli, Sahraian, Jamalimoghadamsiahkali, Asadi, Zarei et al., Treatment With 25-Hydroxyvitamin D3 (Calcifediol) Is Associated With a Reduction in the Blood Neutrophil-to-Lymphocyte Ratio Marker of Disease Severity in Hospitalized Patients With COVID-19: A Pilot Multicenter, Randomized, Placebo-Controlled, Double-Blinded Clinical Trial, Endocr. Pract. Off. J. Am. Coll. Endocrinol. Am. Assoc. Clin. Endocrinol, doi:10.1016/j.eprac.2021.09.016
Martineau, Jolliffe, Hooper, Greenberg, Aloia et al., Vitamin D supplementation to prevent acute respiratory tract infections: Systematic review and meta-analysis of individual participant data, BMJ, doi:10.1136/bmj.i6583
Murai, Fernandes, Sales, Pinto, Goessler et al., Effect of a Single High Dose of Vitamin D3 on Hospital Length of Stay in Patients with Moderate to Severe COVID-19: A Randomized Clinical Trial, JAMA, doi:10.1001/jama.2020.26848
Oscanoa, Amado, Vidal, Laird, Ghashut et al., The relationship between the severity and mortality of SARS-CoV-2 infection and 25-hydroxyvitamin D concentration-A metaanalysis, Adv. Respir. Med
Pal, Banerjee, Bhadada, Shetty, Singh et al., Vitamin D supplementation and clinical outcomes in COVID-19: A systematic review and meta-analysis, J. Endocrinol. Investig, doi:10.1007/s40618-021-01614-4
Papazian, Aubron, Brochard, Chiche, Combes et al., Formal guidelines: Management of acute respiratory distress syndrome, Ann. Intensive Care, doi:10.1186/s13613-019-0540-9
Putzu, Belletti, Cassina, Clivio, Monti et al., Vitamin D and outcomes in adult critically ill patients. A systematic review and meta-analysis of randomized trials, J. Crit. Care, doi:10.1016/j.jcrc.2016.10.029
Quesada-Gomez, Entrenas-Castillo, Bouillon, Vitamin D receptor stimulation to reduce acute respiratory distress syndrome (ARDS) in patients with coronavirus SARS-CoV-2 infections: Revised Ms SBMB 2020_166, J. Steroid Biochem. Mol. Biol, doi:10.1016/j.jsbmb.2020.105719
R_Core_Team, R: A Language and Environment for Statistical Computing
Rizzoli, Vitamin D supplementation: Upper limit for safety revisited?, Aging Clin. Exp. Res, doi:10.1007/s40520-020-01678-x
Ross, Manson, Abrams, Aloia, Brannon et al., The 2011 report on dietary reference intakes for calcium and vitamin D from the Institute of Medicine: What clinicians need to know, J. Clin. Endocrinol. Metab, doi:10.1210/jc.2010-2704
Sanders, Stuart, Williamson, Simpson, Kotowicz et al., Annual high-dose oral vitamin D and falls and fractures in older women: A randomized controlled trial, JAMA, doi:10.1001/jama.2010.594
Sarafin, Durazo-Arvizu, Tian, Phinney, Tai et al., Standardizing 25-hydroxyvitamin D values from the Canadian Health Measures Survey, Am. J. Clin. Nutr, doi:10.3945/ajcn.114.103689
Schleicher, Sternberg, Looker, Yetley, Lacher et al., National Estimates of Serum Total 25-Hydroxyvitamin D and Metabolite Concentrations Measured by Liquid Chromatography-Tandem Mass Spectrometry in the US Population during 2007-2010, J. Nutr, doi:10.3945/jn.115.227728
Sengupta, Majumder, Majumder, Role of vitamin D in treating COVID-19-associated coagulopathy: Problems and perspectives, Mol. Cell. Biochem, doi:10.1007/s11010-021-04093-6
Shah, Saxena, Mavalankar, Vitamin D supplementation, COVID-19 and disease severity: A meta-analysis, QJM Monthly J. Assoc. Physicians, doi:10.1093/qjmed/hcab009
Stroehlein, Wallqvist, Iannizzi, Mikolajewska, Metzendorf et al., Vitamin D supplementation for the treatment of COVID-19: A living systematic review, Cochrane Database Syst. Rev, doi:10.1002/14651858.CD015043
Varikasuvu, Thangappazham, Vykunta, Duggina, Manne et al., COVID-19 and vitamin D (Co-VIVID study): A systematic review and meta-analysis of randomized controlled trials, Expert Rev. Anti-Infect. Ther, doi:10.1080/14787210.2022.2035217
Who, None
Zhang, Wan, Sun, Kan, Wang, Association between vitamin D deficiency and mortality in critically ill adult patients: A meta-analysis of cohort studies, Crit. Care, doi:10.1186/s13054-014-0684-9
Zhou, Luo, Qin, The association between vitamin D deficiency and community-acquired pneumonia: A metaanalysis of observational studies, Medicine, doi:10.1097/MD.0000000000017252
DOI record:
{
"DOI": "10.3390/nu15051234",
"ISSN": [
"2072-6643"
],
"URL": "http://dx.doi.org/10.3390/nu15051234",
"abstract": "<jats:p>COVID-19 symptoms vary from asymptomatic cases to moderate and severe illness with patients needing hospitalization and intensive care treatment. Vitamin D is associated with severity of viral infections and has an immune-modulatory effect in immune response. Observational studies showed a negative association of low vitamin D levels and COVID-19 severity and mortality outcomes. In this study, we aimed to determine whether daily supplementation of vitamin D during intensive care unit (ICU) stay in COVID-19 patients with severe illness affects clinically relevant outcomes. Patients with COVID-19 disease in need of respiratory support admitted to the ICU were eligible for inclusion. Patients with low vitamin D levels were randomized into one of two groups: the intervention group received daily supplementation of vitamin D and the control group did not receive vitamin D supplementation. In total, 155 patients were randomized: 78 into the intervention group and 77 into the control group. There was no statistically significant difference in number of days spent on respiratory support, although the trial was underpowered for the main outcome. There was no difference in any of the secondary outcomes analyzed between two groups. Our study suggests no benefit in vitamin D supplementation to patients with severe COVID-19 disease admitted to the ICU and in need of respiratory support in any of the analyzed outcomes.</jats:p>",
"alternative-id": [
"nu15051234"
],
"author": [
{
"ORCID": "http://orcid.org/0000-0002-5889-0478",
"affiliation": [
{
"name": "Department of Anesthesiology, Reanimatology and Intensive Care, University Hospital Split, 21000 Split, Croatia"
}
],
"authenticated-orcid": false,
"family": "Domazet Bugarin",
"given": "Josipa",
"sequence": "first"
},
{
"affiliation": [
{
"name": "Department of Anesthesiology, Reanimatology and Intensive Care, University Hospital Split, 21000 Split, Croatia"
}
],
"family": "Dosenovic",
"given": "Svjetlana",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Anesthesiology, Reanimatology and Intensive Care, University Hospital Split, 21000 Split, Croatia"
}
],
"family": "Ilic",
"given": "Darko",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-3827-2960",
"affiliation": [
{
"name": "Department of Anesthesiology, Reanimatology and Intensive Care, University Hospital Split, 21000 Split, Croatia"
}
],
"authenticated-orcid": false,
"family": "Delic",
"given": "Nikola",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Anesthesiology, Reanimatology and Intensive Care, University Hospital Split, 21000 Split, Croatia"
}
],
"family": "Saric",
"given": "Ivana",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-9882-2250",
"affiliation": [
{
"name": "Intellomics Ltd., 21000 Split, Croatia"
}
],
"authenticated-orcid": false,
"family": "Ugrina",
"given": "Ivo",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Anesthesiology, Reanimatology and Intensive Care, University Hospital Split, 21000 Split, Croatia"
}
],
"family": "Stojanovic Stipic",
"given": "Sanda",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Anesthesiology, Reanimatology and Intensive Care, University Hospital Split, 21000 Split, Croatia"
}
],
"family": "Duplancic",
"given": "Bozidar",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Anesthesiology, Reanimatology and Intensive Care, University Hospital Split, 21000 Split, Croatia"
}
],
"family": "Saric",
"given": "Lenko",
"sequence": "additional"
}
],
"container-title": "Nutrients",
"container-title-short": "Nutrients",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2023,
3,
1
]
],
"date-time": "2023-03-01T06:36:09Z",
"timestamp": 1677652569000
},
"deposited": {
"date-parts": [
[
2023,
3,
10
]
],
"date-time": "2023-03-10T10:26:42Z",
"timestamp": 1678444002000
},
"indexed": {
"date-parts": [
[
2023,
3,
11
]
],
"date-time": "2023-03-11T05:40:46Z",
"timestamp": 1678513246298
},
"is-referenced-by-count": 0,
"issue": "5",
"issued": {
"date-parts": [
[
2023,
2,
28
]
]
},
"journal-issue": {
"issue": "5",
"published-online": {
"date-parts": [
[
2023,
3
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
2,
28
]
],
"date-time": "2023-02-28T00:00:00Z",
"timestamp": 1677542400000
}
}
],
"link": [
{
"URL": "https://www.mdpi.com/2072-6643/15/5/1234/pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1968",
"original-title": [],
"page": "1234",
"prefix": "10.3390",
"published": {
"date-parts": [
[
2023,
2,
28
]
]
},
"published-online": {
"date-parts": [
[
2023,
2,
28
]
]
},
"publisher": "MDPI AG",
"reference": [
{
"key": "ref_1",
"unstructured": "(2021, November 15). WHO. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019."
},
{
"DOI": "10.1186/s12879-021-06281-7",
"doi-asserted-by": "crossref",
"key": "ref_2",
"unstructured": "Campi, I., Gennari, L., Merlotti, D., Mingiano, C., Frosali, A., Giovanelli, L., Torlasco, C., Pengo, M.F., Heilbron, F., and Soranna, D. (2021). Vitamin D and COVID-19 severity and related mortality: A prospective study in Italy. BMC Infect. Dis., 21."
},
{
"DOI": "10.1186/s13063-020-04928-5",
"article-title": "COVID-19 and high-dose VITamin D supplementation TRIAL in high-risk older patients (COVIT-TRIAL): Study protocol for a randomized controlled trial",
"author": "Annweiler",
"doi-asserted-by": "crossref",
"first-page": "1031",
"journal-title": "Trials",
"key": "ref_3",
"volume": "21",
"year": "2020"
},
{
"DOI": "10.1016/j.mayocp.2013.05.011",
"article-title": "Vitamin D for health: A global perspective",
"author": "Holick",
"doi-asserted-by": "crossref",
"first-page": "720",
"journal-title": "Mayo Clin. Proc.",
"key": "ref_4",
"volume": "88",
"year": "2013"
},
{
"DOI": "10.1016/j.metabol.2021.154753",
"article-title": "The link between COVID-19 and VItamin D (VIVID): A systematic review and meta-analysis",
"author": "Bassatne",
"doi-asserted-by": "crossref",
"first-page": "154753",
"journal-title": "Metab. Clin. Exp.",
"key": "ref_5",
"volume": "119",
"year": "2021"
},
{
"DOI": "10.1210/er.2018-00126",
"article-title": "Skeletal and Extraskeletal Actions of Vitamin D: Current Evidence and Outstanding Questions",
"author": "Bouillon",
"doi-asserted-by": "crossref",
"first-page": "1109",
"journal-title": "Endocr. Rev.",
"key": "ref_6",
"volume": "40",
"year": "2019"
},
{
"DOI": "10.1016/j.jsbmb.2020.105719",
"article-title": "Vitamin D receptor stimulation to reduce acute respiratory distress syndrome (ARDS) in patients with coronavirus SARS-CoV-2 infections: Revised Ms SBMB 2020_166",
"author": "Bouillon",
"doi-asserted-by": "crossref",
"first-page": "105719",
"journal-title": "J. Steroid Biochem. Mol. Biol.",
"key": "ref_7",
"volume": "202",
"year": "2020"
},
{
"article-title": "Effect of Oral Versus Intramuscular Vitamin D Replacement on Oxidative Stress and Outcomes in Traumatic Mechanical Ventilated Patients Admitted to Intensive Care Unit",
"author": "Hasanloei",
"first-page": "548",
"journal-title": "Nutr. Clin. Pract. Off. Publ. Am. Soc. Parenter. Enter. Nutr.",
"key": "ref_8",
"volume": "35",
"year": "2020"
},
{
"article-title": "Editorial—Vitamin D status: A key modulator of innate immunity and natural defense from acute viral respiratory infections",
"author": "Fabbri",
"first-page": "4048",
"journal-title": "Eur. Rev. Med. Pharmacol. Sci.",
"key": "ref_9",
"volume": "24",
"year": "2020"
},
{
"DOI": "10.1007/s11010-021-04093-6",
"article-title": "Role of vitamin D in treating COVID-19-associated coagulopathy: Problems and perspectives",
"author": "Sengupta",
"doi-asserted-by": "crossref",
"first-page": "2421",
"journal-title": "Mol. Cell. Biochem.",
"key": "ref_10",
"volume": "476",
"year": "2021"
},
{
"DOI": "10.1016/j.jiph.2020.06.021",
"article-title": "Role of vitamin D in preventing of COVID-19 infection, progression and severity",
"author": "Ali",
"doi-asserted-by": "crossref",
"first-page": "1373",
"journal-title": "J. Infect. Public Health",
"key": "ref_11",
"volume": "13",
"year": "2020"
},
{
"DOI": "10.1097/MD.0000000000017252",
"doi-asserted-by": "crossref",
"key": "ref_12",
"unstructured": "Zhou, Y.F., Luo, B.A., and Qin, L.L. (2019). The association between vitamin D deficiency and community-acquired pneumonia: A meta-analysis of observational studies. Medicine, 98."
},
{
"DOI": "10.1016/j.nut.2018.11.001",
"article-title": "Vitamin D in the ICU: More sun for critically ill adult patients?",
"author": "Langlois",
"doi-asserted-by": "crossref",
"first-page": "173",
"journal-title": "Nutrition",
"key": "ref_13",
"volume": "61",
"year": "2019"
},
{
"DOI": "10.1186/s13054-014-0660-4",
"article-title": "Vitamin D deficiency as a risk factor for infection, sepsis and mortality in the critically ill: Systematic review and meta-analysis",
"author": "Groeneveld",
"doi-asserted-by": "crossref",
"first-page": "660",
"journal-title": "Crit. Care",
"key": "ref_14",
"volume": "18",
"year": "2014"
},
{
"DOI": "10.1186/s13054-014-0684-9",
"article-title": "Association between vitamin D deficiency and mortality in critically ill adult patients: A meta-analysis of cohort studies",
"author": "Zhang",
"doi-asserted-by": "crossref",
"first-page": "684",
"journal-title": "Crit. Care",
"key": "ref_15",
"volume": "18",
"year": "2014"
},
{
"DOI": "10.5603/ARM.a2021.0037",
"article-title": "The relationship between the severity and mortality of SARS-CoV-2 infection and 25-hydroxyvitamin D concentration—A metaanalysis",
"author": "Oscanoa",
"doi-asserted-by": "crossref",
"first-page": "145",
"journal-title": "Adv. Respir. Med.",
"key": "ref_16",
"volume": "89",
"year": "2021"
},
{
"DOI": "10.1093/advances/nmab012",
"article-title": "Association of Vitamin D Status with SARS-CoV-2 Infection or COVID-19 Severity: A Systematic Review and Meta-analysis",
"author": "Kazemi",
"doi-asserted-by": "crossref",
"first-page": "1636",
"journal-title": "Adv. Nutr.",
"key": "ref_17",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.1097/MCC.0000000000000849",
"article-title": "Vitamin D in critical care: Where are we now and what is next?",
"author": "Amrein",
"doi-asserted-by": "crossref",
"first-page": "378",
"journal-title": "Curr. Opin. Crit. Care",
"key": "ref_18",
"volume": "27",
"year": "2021"
},
{
"article-title": "Treatment With 25-Hydroxyvitamin D3 (Calcifediol) Is Associated With a Reduction in the Blood Neutrophil-to-Lymphocyte Ratio Marker of Disease Severity in Hospitalized Patients With COVID-19: A Pilot Multicenter, Randomized, Placebo-Controlled, Double-Blinded Clinical Trial",
"author": "Maghbooli",
"first-page": "1242",
"journal-title": "Endocr. Pract. Off. J. Am. Coll. Endocrinol. Am. Assoc. Clin. Endocrinol.",
"key": "ref_19",
"volume": "27",
"year": "2021"
},
{
"DOI": "10.1007/s40618-021-01614-4",
"article-title": "Vitamin D supplementation and clinical outcomes in COVID-19: A systematic review and meta-analysis",
"author": "Pal",
"doi-asserted-by": "crossref",
"first-page": "53",
"journal-title": "J. Endocrinol. Investig.",
"key": "ref_20",
"volume": "45",
"year": "2021"
},
{
"DOI": "10.1097/MCO.0000000000000147",
"article-title": "Vitamin D supplementation in the ICU patient",
"author": "Christopher",
"doi-asserted-by": "crossref",
"first-page": "187",
"journal-title": "Curr. Opin. Clin. Nutr. Metab. Care",
"key": "ref_21",
"volume": "18",
"year": "2015"
},
{
"DOI": "10.1038/s41598-020-71271-9",
"article-title": "Vitamin D supplementation and the outcomes of critically ill adult patients: A systematic review and meta-analysis of randomized controlled trials",
"author": "Lan",
"doi-asserted-by": "crossref",
"first-page": "14261",
"journal-title": "Sci. Rep.",
"key": "ref_22",
"volume": "10",
"year": "2020"
},
{
"DOI": "10.1001/jama.2020.26848",
"article-title": "Effect of a Single High Dose of Vitamin D3 on Hospital Length of Stay in Patients with Moderate to Severe COVID-19: A Randomized Clinical Trial",
"author": "Murai",
"doi-asserted-by": "crossref",
"first-page": "1053",
"journal-title": "JAMA",
"key": "ref_23",
"volume": "325",
"year": "2021"
},
{
"DOI": "10.1016/j.jcrc.2016.10.029",
"article-title": "Vitamin D and outcomes in adult critically ill patients. A systematic review and meta-analysis of randomized trials",
"author": "Putzu",
"doi-asserted-by": "crossref",
"first-page": "109",
"journal-title": "J. Crit. Care",
"key": "ref_24",
"volume": "38",
"year": "2017"
},
{
"article-title": "Vitamin D supplementation for the treatment of COVID-19: A living systematic review",
"author": "Stroehlein",
"first-page": "CD015043",
"journal-title": "Cochrane Database Syst. Rev.",
"key": "ref_25",
"volume": "5",
"year": "2021"
},
{
"DOI": "10.1097/MCC.0000000000000328",
"article-title": "Vitamin D and critical illness outcomes",
"author": "Christopher",
"doi-asserted-by": "crossref",
"first-page": "332",
"journal-title": "Curr. Opin. Crit. Care",
"key": "ref_26",
"volume": "22",
"year": "2016"
},
{
"DOI": "10.1001/jama.2010.594",
"article-title": "Annual high-dose oral vitamin D and falls and fractures in older women: A randomized controlled trial",
"author": "Sanders",
"doi-asserted-by": "crossref",
"first-page": "1815",
"journal-title": "JAMA",
"key": "ref_27",
"volume": "303",
"year": "2010"
},
{
"DOI": "10.1136/bmj.i6583",
"article-title": "Vitamin D supplementation to prevent acute respiratory tract infections: Systematic review and meta-analysis of individual participant data",
"author": "Martineau",
"doi-asserted-by": "crossref",
"first-page": "i6583",
"journal-title": "BMJ",
"key": "ref_28",
"volume": "356",
"year": "2017"
},
{
"DOI": "10.1210/jc.2013-2653",
"article-title": "Clinical review: The role of the parent compound vitamin D with respect to metabolism and function: Why clinical dose intervals can affect clinical outcomes",
"author": "Hollis",
"doi-asserted-by": "crossref",
"first-page": "4619",
"journal-title": "J. Clin. Endocrinol. Metab.",
"key": "ref_29",
"volume": "98",
"year": "2013"
},
{
"DOI": "10.1530/EC-18-0184",
"article-title": "Vitamin D and critical illness: What endocrinology can learn from intensive care and vice versa",
"author": "Amrein",
"doi-asserted-by": "crossref",
"first-page": "R304",
"journal-title": "Endocr. Connect.",
"key": "ref_30",
"volume": "7",
"year": "2018"
},
{
"DOI": "10.1210/jc.2010-2704",
"article-title": "The 2011 report on dietary reference intakes for calcium and vitamin D from the Institute of Medicine: What clinicians need to know",
"author": "Ross",
"doi-asserted-by": "crossref",
"first-page": "53",
"journal-title": "J. Clin. Endocrinol. Metab.",
"key": "ref_31",
"volume": "96",
"year": "2011"
},
{
"DOI": "10.1210/jc.2011-0385",
"article-title": "Evaluation, treatment, and prevention of vitamin D deficiency: An Endocrine Society clinical practice guideline",
"author": "Holick",
"doi-asserted-by": "crossref",
"first-page": "1911",
"journal-title": "J. Clin. Endocrinol. Metab.",
"key": "ref_32",
"volume": "96",
"year": "2011"
},
{
"DOI": "10.1038/s41430-020-0558-y",
"article-title": "Vitamin D deficiency 2.0: An update on the current status worldwide",
"author": "Amrein",
"doi-asserted-by": "crossref",
"first-page": "1498",
"journal-title": "Eur. J. Clin. Nutr.",
"key": "ref_33",
"volume": "74",
"year": "2020"
},
{
"DOI": "10.1210/clinem/dgz212",
"article-title": "Safety of High-Dose Vitamin D Supplementation: Secondary Analysis of a Randomized Controlled Trial",
"author": "Billington",
"doi-asserted-by": "crossref",
"first-page": "1261",
"journal-title": "J. Clin. Endocrinol. Metab.",
"key": "ref_34",
"volume": "105",
"year": "2020"
},
{
"DOI": "10.1007/s40520-020-01678-x",
"article-title": "Vitamin D supplementation: Upper limit for safety revisited?",
"author": "Rizzoli",
"doi-asserted-by": "crossref",
"first-page": "19",
"journal-title": "Aging Clin. Exp. Res.",
"key": "ref_35",
"volume": "33",
"year": "2021"
},
{
"DOI": "10.1186/s13613-019-0540-9",
"article-title": "Formal guidelines: Management of acute respiratory distress syndrome",
"author": "Papazian",
"doi-asserted-by": "crossref",
"first-page": "69",
"journal-title": "Ann. Intensive Care",
"key": "ref_36",
"volume": "9",
"year": "2019"
},
{
"article-title": "Acute respiratory distress syndrome: The Berlin Definition",
"author": "Force",
"first-page": "2526",
"journal-title": "JAMA",
"key": "ref_37",
"volume": "307",
"year": "2012"
},
{
"key": "ref_38",
"unstructured": "R_Core_Team (2022, July 10). R: A Language and Environment for Statistical Computing. Available online: https://www.R-project.org/."
},
{
"key": "ref_39",
"unstructured": "Chambers, J.M., and Hastie, T.J. (1992). Statistical Models in S, Wadsworth & Brooks/Cole."
},
{
"DOI": "10.4103/sja.SJA_559_18",
"article-title": "The CONSORT statement",
"author": "Cuschieri",
"doi-asserted-by": "crossref",
"first-page": "S27",
"journal-title": "Saudi J. Anaesth.",
"key": "ref_40",
"volume": "13",
"year": "2019"
},
{
"DOI": "10.1371/journal.pmed.0050004",
"doi-asserted-by": "crossref",
"key": "ref_41",
"unstructured": "Guyatt, G.H., Mills, E.J., and Elbourne, D. (2008). In the era of systematic reviews, does the size of an individual trial still matter. PLoS Med., 5."
},
{
"DOI": "10.3945/jn.115.227728",
"article-title": "National Estimates of Serum Total 25-Hydroxyvitamin D and Metabolite Concentrations Measured by Liquid Chromatography-Tandem Mass Spectrometry in the US Population during 2007–2010",
"author": "Schleicher",
"doi-asserted-by": "crossref",
"first-page": "1051",
"journal-title": "J. Nutr.",
"key": "ref_42",
"volume": "146",
"year": "2016"
},
{
"DOI": "10.3945/ajcn.115.120873",
"article-title": "Vitamin D deficiency in Europe: Pandemic?",
"author": "Cashman",
"doi-asserted-by": "crossref",
"first-page": "1033",
"journal-title": "Am. J. Clin. Nutr.",
"key": "ref_43",
"volume": "103",
"year": "2016"
},
{
"DOI": "10.3945/ajcn.114.103689",
"article-title": "Standardizing 25-hydroxyvitamin D values from the Canadian Health Measures Survey",
"author": "Sarafin",
"doi-asserted-by": "crossref",
"first-page": "1044",
"journal-title": "Am. J. Clin. Nutr.",
"key": "ref_44",
"volume": "102",
"year": "2015"
},
{
"DOI": "10.1186/cc13790",
"article-title": "Vitamin D status and its association with season, hospital and sepsis mortality in critical illness",
"author": "Amrein",
"doi-asserted-by": "crossref",
"first-page": "R47",
"journal-title": "Crit. Care",
"key": "ref_45",
"volume": "18",
"year": "2014"
},
{
"article-title": "Vitamin D supplementation to prevent acute respiratory infections: Systematic review and meta-analysis of aggregate data from randomised controlled trials",
"author": "Jolliffe",
"first-page": "276",
"journal-title": "Medrxiv Prepr. Serv. Health Sci.",
"key": "ref_46",
"volume": "9",
"year": "2020"
},
{
"DOI": "10.1001/jama.2014.13204",
"article-title": "Effect of high-dose vitamin D3 on hospital length of stay in critically ill patients with vitamin D deficiency: The VITdAL-ICU randomized clinical trial",
"author": "Amrein",
"doi-asserted-by": "crossref",
"first-page": "1520",
"journal-title": "JAMA",
"key": "ref_47",
"volume": "312",
"year": "2014"
},
{
"article-title": "Insufficient evidence for vitamin D use in COVID-19: A rapid systematic review",
"author": "Atallah",
"first-page": "e14649",
"journal-title": "Int. J. Clin. Pract.",
"key": "ref_48",
"volume": "75",
"year": "2021"
},
{
"DOI": "10.1038/s41430-021-00984-5",
"article-title": "The effect of high-dose parenteral vitamin D3 on COVID-19-related inhospital mortality in critical COVID-19 patients during intensive care unit admission: An observational cohort study",
"author": "Guven",
"doi-asserted-by": "crossref",
"first-page": "1383",
"journal-title": "Eur. J. Clin. Nutr.",
"key": "ref_49",
"volume": "75",
"year": "2021"
},
{
"DOI": "10.1093/qjmed/hcab009",
"article-title": "Vitamin D supplementation, COVID-19 and disease severity: A meta-analysis",
"author": "Shah",
"doi-asserted-by": "crossref",
"first-page": "175",
"journal-title": "QJM Monthly J. Assoc. Physicians",
"key": "ref_50",
"volume": "114",
"year": "2021"
},
{
"DOI": "10.1080/14787210.2022.2035217",
"article-title": "COVID-19 and vitamin D (Co-VIVID study): A systematic review and meta-analysis of randomized controlled trials",
"author": "Varikasuvu",
"doi-asserted-by": "crossref",
"first-page": "907",
"journal-title": "Expert Rev. Anti-Infect. Ther.",
"key": "ref_51",
"volume": "20",
"year": "2022"
},
{
"DOI": "10.1371/journal.pone.0268396",
"doi-asserted-by": "crossref",
"key": "ref_52",
"unstructured": "D’Ecclesiis, O., Gavioli, C., Martinoli, C., Raimondi, S., Chiocca, S., Miccolo, C., Bossi, P., Cortinovis, D., Chiaradonna, F., and Palorini, R. (2022). Vitamin D and SARS-CoV2 infection, severity and mortality: A systematic review and meta-analysis. PLoS ONE, 17."
}
],
"reference-count": 52,
"references-count": 52,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.mdpi.com/2072-6643/15/5/1234"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Food Science",
"Nutrition and Dietetics"
],
"subtitle": [],
"title": "Vitamin D Supplementation and Clinical Outcomes in Severe COVID-19 Patients—Randomized Controlled Trial",
"type": "journal-article",
"volume": "15"
}
