Towards Predicting Length of Stay and Identification of Cohort Risk Factors Using Self-Attention Based Transformers and Association Mining: Covid-19 as Phenotype
et al., Preprints, doi:10.20944/preprints202301.0341.v1, Jan 2023
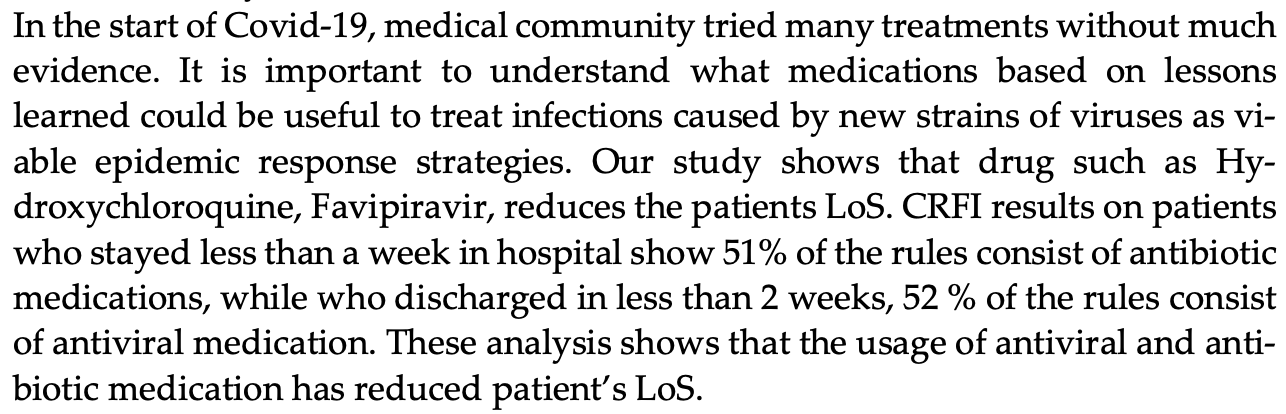
Deep learning model for the prediction of hospitalization time for COVID-19 based on 311 patients in Saudi Arabia. Authors report shorter hospitalization time for HCQ and favipiravir, but do not provide details.
Potential risks of favipiravir include kidney injury1-3, liver injury2-5, cardiovascular events5,6, pulmonary toxicity6,7, and mutagenicity, carcinogenicity, teratogenicity, embryotoxicity, and the creation of dangerous variants8-14.
Study covers HCQ and favipiravir.
1.
Abdulaziz et al., Clinical Features and Prognosis of Acute Kidney Injury in Hospital-Admitted Patients with COVID-19 in Egypt: A Single-Center Experience, Mansoura Medical Journal, doi:10.58775/2735-3990.1433.
2.
Ülger et al., Experimental evaluation of favipiravir (T-705)-induced liver and kidney toxicity in rats, Food and Chemical Toxicology, doi:10.1016/j.fct.2025.115472.
3.
El-Fetouh et al., Experimental Studies on Some Drugs Used in Covid-19 Treatment (Favipiravir and Dexamethasone) in Albino Rats, Journal of Advanced Veterinary Research, 13:10, www.advetresearch.com/index.php/AVR/article/view/1635.
4.
Almutairi et al., Liver Injury in Favipiravir-Treated COVID-19 Patients: Retrospective Single-Center Cohort Study, Tropical Medicine and Infectious Disease, doi:10.3390/tropicalmed8020129.
5.
Siby et al., Temporal Trends in Serious Adverse Events Associated with Oral Antivirals During the COVID-19 Pandemic: Insights from the FAERS Database (2020–2023), Open Forum Infectious Diseases, doi:10.1093/ofid/ofaf695.1825.
6.
Ozhan et al., Evaluation of the cardiopulmonary effects of repurposed COVID-19 therapeutics in healthy rats, Scientific Reports, doi:10.1038/s41598-025-31048-4.
7.
Ülger (B) et al., Evaluation of the effects of favipiravir (T-705) on the lung tissue of healty rats: An experimental study, Food and Chemical Toxicology, doi:10.1016/j.fct.2025.115235.
8.
Zhirnov et al., Favipiravir: the hidden threat of mutagenic action, Journal of microbiology, epidemiology and immunobiology, doi:10.36233/0372-9311-114.
9.
Waters et al., Human genetic risk of treatment with antiviral nucleoside analog drugs that induce lethal mutagenesis: the special case of molnupiravir, Environmental and Molecular Mutagenesis, doi:10.1002/em.22471.
10.
Hadj Hassine et al., Lethal Mutagenesis of RNA Viruses and Approved Drugs with Antiviral Mutagenic Activity, Viruses, doi:10.3390/v14040841.
11.
Shum, C., An investigational study into the drug-associated mutational signature in SARS-CoV-2 viruses, The University of Hong Kong, PhD Thesis, hub.hku.hk/handle/10722/344396.
12.
Shiraki et al., Convenient screening of the reproductive toxicity of favipiravir and antiviral drugs in Caenorhabditis elegans, Heliyon, doi:10.1016/j.heliyon.2024.e35331.
Alam et al., 19 Jan 2023, Saudi Arabia, preprint, 7 authors, study period April 2020 - January 2021.
Contact: mahmood@oakland.edu (corresponding author), mahmood}@oakland.edu, nkaabia}@psmmc.med.sa, ihussain@kfshrc.edu.sa, amalalaidaroos@gmail.com.
Towards Predicting Length of Stay and Identification of Cohort Risk Factors Using Self-Attention Based Transformers and Association Mining: Covid-19 as Phenotype
doi:10.20944/preprints202301.0341.v1
Predicting Length of Stay (LoS) and understanding its underlying factors is essential to minimize the risk of hospital-acquired conditions, improve financial, operational, and clinical outcomes, and to better manage future pandemics. The purpose of this study is to forecast patients' LoS using a deep learning model and analyze cohorts of risk factors minimizing or maximizing LoS. We employed various pre-processing techniques, SMOTE-N to balance data, and Tab-Transformer model to forecast LoS. Finally, Apriori algorithm was applied to analyze cohorts of risk factors influencing LoS at hospital. The Tab-Transformer outperformed the base Machine Learning models with an F1-score (.92), precision (.83), recall (.93), and accuracy (.73) for discharge dataset, and F1score (.84), precision (.75), recall (.98), and accuracy (.77) for deceased dataset. The association mining algorithm was able to identify significant risk factors/indicators belonging to lab, X-Ray, and clinical data such as elevated LDH, and D-Dimer, lymphocytes count, and comorbidities such as hypertension and diabetes responsible for extending patients LoS. It also reveals what treatments has reduced the symptoms of COVID-19 patients leading to reduction in LoS particularly when no vaccines or medication such as Paxlovid were available.
Discharged Dataset
CRFI for Discharged Patients' Category In the discharged patients' category, for LoS ≤ 1 week or Los ≤ 2 weeks, usage of anticoagulant, antibiotics and antiviral medications are important factors and indicates that timely intervention and dosage reduces LoS. For LoS ≤ 3 weeks, some of the important risk factors observed in the rules are elevated level of LDH (>225), D-Dimer (>500) and CRP (between 6 mg/L to 100 mg/L). Observed rules suggest that patients with abnormal values of these factors takes time to recover even if they provided with anticoagulant and antiviral medications. For LoS ≤ 4 weeks, the important risk factors observed are higher lymphocytes count (>1000 cells/µL), elevated PNN count (1000 -7000 mm3), comorbidities such as hypertension, higher respiratory rate (20-28 bps). The mining results on patients who stayed more than 4 weeks in the hospital shows less platelets count (<50000), abnormal X-ray, PTT>14.5, and higher PNN count. We found these patterns along with usage
Conflicts of Interest: The authors declare no conflict of interest.
References
Adab, Haroon, O'hara, Jordan, Comorbidities and covid-19, bmj
Borgelt, Kruse, Induction of association rules: Apriori implementation
Bravata, Perkins, Myers, Arling, Zhang et al., Association of intensive care unit patient load and demand with mortality rates in US Department of Veterans Affairs hospitals during the COVID-19 pandemic, JAMA network open
Chawla, Bowyer, Hall, Kegelmeyer, SMOTE: synthetic minority over-sampling technique, Journal of artificial intelligence research
Churpek, Wendlandt, Zadravecz, Adhikari, Winslow et al., Association between intensive care unit transfer delay and hospital mortality: a multicenter investigation, Journal of hospital medicine
Dan, Li, Zhu, Chen, Quan et al., Machine learning to predict ICU admission, ICU mortality and survivors' length of stay among COVID-19 patients: toward optimal allocation of ICU resources
Dogu, Albayrak, Tuncay, Length of hospital stay prediction with an integrated approach of statisticalbased fuzzy cognitive maps and artificial neural networks, Medical & Biological Engineering & Computing
Harerimana, Kim, Jang, A deep attention model to forecast the Length of Stay and the in-hospital mortality right on admission from ICD codes and demographic data, Journal of Biomedical Informatics
Huang, Khetan, Cvitkovic, Karnin, Tabtransformer: Tabular data modeling using contextual embeddings
Johnson, Pollard, Shen, Lehman, Feng et al., MIMIC-III, a freely accessible critical care database, Scientific data
Kulkarni, Thangam, Amin, Artificial neural network-based prediction of prolonged length of stay and need for post-acute care in acute coronary syndrome patients undergoing percutaneous coronary intervention, European Journal of Clinical Investigation
Lehmann, Prosch, Zehetmayer, Gysan, Bernitzky et al., Impact of persistent D-dimer elevation following recovery from COVID-19, PLoS One
Luo, Lian, Feng, Huang, Zhang, Data mining-based detection of rapid growth in length of stay on COPD patients
Mathieu, Coronavirus (COVID-19) Hospitalizations. Our World in Data
Rajkomar, Oren, Chen, Dai, Hajaj et al., Scalable and accurate deep learning with electronic health records, NPJ digital medicine
Resar, Nolan, Kaczynski, Jensen, Using real-time demand capacity management to improve hospitalwide patient flow, The Joint Commission Journal on Quality and Patient Safety
Statsenko, Al Zahmi, Habuza, Almansoori, Smetanina et al., Impact of Age and Sex on COVID-19 Severity Assessed From Radiologic and Clinical Findings, Frontiers in cellular and infection microbiology
Vekaria, Overton, Wiśniowski, Ahmad, Aparicio-Castro et al., Hospital length of stay for COVID-19 patients: Data-driven methods for forward planning, BMC Infectious Diseases
Wagner, Dupont, Larson, Cash, Farooq, Absolute lymphocyte count is a prognostic marker in Covid-19: a retrospective cohort review, International Journal of Laboratory Hematology
Weiss, Elixhauser, Overview of hospital stays in the United States
Zebin, Chaussalet, Design and implementation of a deep recurrent model for prediction of readmission in urgent care using electronic health records
DOI record:
{
"DOI": "10.20944/preprints202301.0341.v1",
"URL": "http://dx.doi.org/10.20944/preprints202301.0341.v1",
"abstract": "<jats:p>Predicting Length of Stay (LoS) and understanding its underlying factors is essential to minimize the risk of hospital-acquired conditions, improve financial, operational, and clinical outcomes, and to better manage future pandemics. The purpose of this study is to forecast patients&rsquo; LoS using a deep learning model and analyze cohorts of risk factors minimizing or maximizing LoS. We employed various pre-processing techniques, SMOTE-N to balance data, and Tab-Transformer model to forecast LoS. Finally, Apriori algorithm was applied to analyze cohorts of risk factors influencing LoS at hospital. The Tab-Transformer outperformed the base Machine Learning models with an F1-score (.92), precision (.83), recall (.93), and accuracy (.73) for discharge dataset, and F1-score (.84), precision (.75), recall (.98), and accuracy (.77) for deceased dataset. The association mining algorithm was able to identify significant risk factors/indicators belonging to lab, X-Ray, and clinical data such as elevated LDH, and D-Dimer, lymphocytes count, and comorbidities such as hypertension and diabetes responsible for extending patients LoS. It also reveals what treatments has reduced the symptoms of COVID-19 patients leading to reduction in LoS particularly when no vaccines or medication such as Paxlovid were available.</jats:p>",
"accepted": {
"date-parts": [
[
2023,
1,
15
]
]
},
"author": [
{
"ORCID": "http://orcid.org/0000-0002-9495-7051",
"affiliation": [],
"authenticated-orcid": false,
"family": "Alam",
"given": "Fakhare",
"sequence": "first"
},
{
"affiliation": [],
"family": "Ananbeh",
"given": "Obieda",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-7927-3436",
"affiliation": [],
"authenticated-orcid": false,
"family": "Malik",
"given": "Khalid Mahmood",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Odayani",
"given": "Abdulrahman Al",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Hussain",
"given": "Ibrahim Bin",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Kaabia",
"given": "Naoufel",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Aidaroos",
"given": "Amal Al",
"sequence": "additional"
}
],
"container-title": [],
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2023,
1,
19
]
],
"date-time": "2023-01-19T07:01:43Z",
"timestamp": 1674111703000
},
"deposited": {
"date-parts": [
[
2023,
1,
19
]
],
"date-time": "2023-01-19T07:47:40Z",
"timestamp": 1674114460000
},
"group-title": "MEDICINE & PHARMACOLOGY",
"indexed": {
"date-parts": [
[
2023,
1,
20
]
],
"date-time": "2023-01-20T06:12:04Z",
"timestamp": 1674195124596
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2023,
1,
19
]
]
},
"license": [
{
"URL": "http://creativecommons.org/licenses/by/4.0",
"content-version": "unspecified",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
1,
19
]
],
"date-time": "2023-01-19T00:00:00Z",
"timestamp": 1674086400000
}
}
],
"member": "1968",
"original-title": [],
"posted": {
"date-parts": [
[
2023,
1,
19
]
]
},
"prefix": "10.20944",
"published": {
"date-parts": [
[
2023,
1,
19
]
]
},
"publisher": "MDPI AG",
"reference-count": 0,
"references-count": 0,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.preprints.org/manuscript/202301.0341/v1"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subtitle": [],
"subtype": "preprint",
"title": "Towards Predicting Length of Stay and Identification of Cohort Risk Factors Using Self-Attention Based Transformers and Association Mining: Covid-19 as Phenotype",
"type": "posted-content"
}
alam3