Clinical characteristics and risk factors of non-mild outcomes in patients with Omicron variant COVID-19 in Shanghai, China
et al., The Journal of Infection in Developing Countries, doi:10.3855/jidc.18138, Jan 2024
Retrospective 311 COVID-19 patients in China showing significantly slower viral clearance with paxlovid in multivariable analysis.
Resistance. Variants may be resistant to paxlovid1-8. Use may promote the emergence of variants that weaken host immunity and potentially contribute to long COVID9. Confounding by contraindication. Hoertel et al. find that over 50% of patients that died had a contraindication for the use of Paxlovid10. Retrospective studies that do not exclude contraindicated patients may significantly overestimate efficacy. Black box warning. The FDA notes that severe, life-threatening, and/or fatal adverse reactions due to drug interactions have been reported in patients treated with paxlovid11. Kidney and liver injury. Studies show significantly increased risk of acute kidney injury12 and liver injury13,14. Viral rebound. Studies show significantly increased risk of replication-competent viral rebound15-17.
Standard of Care (SOC) for COVID-19 in the study country,
China, is average with moderate efficacy for approved treatments18.
|
risk of no viral clearance, 78.6% higher, OR 1.79, p < 0.001, treatment 138, control 155, adjusted per study, inverted to make OR<1 favor treatment, multivariable, RR approximated with OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
1.
Zhou et al., Nirmatrelvir-resistant SARS-CoV-2 variants with high fitness in an infectious cell culture system, Science Advances, doi:10.1126/sciadv.add7197.
2.
Moghadasi et al., Rapid resistance profiling of SARS-CoV-2 protease inhibitors, npj Antimicrobials and Resistance, doi:10.1038/s44259-023-00009-0.
3.
Jochmans et al., The Substitutions L50F, E166A, and L167F in SARS-CoV-2 3CLpro Are Selected by a Protease Inhibitor In Vitro and Confer Resistance To Nirmatrelvir, mBio, doi:10.1128/mbio.02815-22.
4.
Lopez et al., SARS-CoV-2 Resistance to Small Molecule Inhibitors, Current Clinical Microbiology Reports, doi:10.1007/s40588-024-00229-6.
5.
Zvornicanin et al., Molecular Mechanisms of Drug Resistance and Compensation in SARS-CoV-2 Main Protease: The Interplay Between E166 and L50, bioRxiv, doi:10.1101/2025.01.24.634813.
6.
Vukovikj et al., Impact of SARS-CoV-2 variant mutations on susceptibility to monoclonal antibodies and antiviral drugs: a non-systematic review, April 2022 to October 2024, Eurosurveillance, doi:10.2807/1560-7917.ES.2025.30.10.2400252.
7.
Deschenes et al., Functional and structural characterization of treatment-emergent nirmatrelvir resistance mutations at low frequencies in the main protease (Mpro) reveals a unique evolutionary route for SARS-CoV-2 to gain resistance, The Journal of Infectious Diseases, doi:10.1093/infdis/jiaf294.
8.
Zhou (B) et al., SARS-CoV-2 Mpro inhibitor ensitrelvir: asymmetrical cross-resistance with nirmatrelvir and emerging resistance hotspots, Emerging Microbes & Infections, doi:10.1080/22221751.2025.2552716.
9.
Thomas et al., Nirmatrelvir-Resistant Mutations in SARS-CoV-2 Mpro Enhance Host Immune Evasion via Cleavage of NF-κB Essential Modulator, bioRxiv, doi:10.1101/2024.10.18.619137.
10.
Hoertel et al., Prevalence of Contraindications to Nirmatrelvir-Ritonavir Among Hospitalized Patients With COVID-19 at Risk for Progression to Severe Disease, JAMA Network Open, doi:10.1001/jamanetworkopen.2022.42140.
11.
FDA, Fact sheet for healthcare providers: emergency use authorization for paxlovid, www.fda.gov/media/155050/download.
12.
Kamo et al., Association of Antiviral Drugs for the Treatment of COVID-19 With Acute Renal Failure, In Vivo, doi:10.21873/invivo.13637.
13.
Wang et al., Development and validation of a nomogram to assess the occurrence of liver dysfunction in patients with COVID-19 pneumonia in the ICU, BMC Infectious Diseases, doi:10.1186/s12879-025-10684-1.
14.
Siby et al., Temporal Trends in Serious Adverse Events Associated with Oral Antivirals During the COVID-19 Pandemic: Insights from the FAERS Database (2020–2023), Open Forum Infectious Diseases, doi:10.1093/ofid/ofaf695.1825.
15.
Edelstein et al., SARS-CoV-2 virologic rebound with nirmatrelvir-ritonavir therapy, medRxiv, doi:10.1101/2023.06.23.23288598.
16.
Shah et al., SARS-CoV-2 infectious shedding and rebound among adults with and without oral antiviral use: two case-ascertained prospective household studies, The Lancet Microbe, doi:10.1016/j.lanmic.2025.101227.
Zhu et al., 31 Jan 2024, retrospective, China, peer-reviewed, median age 76.0, 5 authors, study period 26 April, 2022 - 21 May, 2022.
Clinical characteristics and risk factors of non-mild outcomes in patients with Omicron variant COVID-19 in Shanghai, China
The Journal of Infection in Developing Countries, doi:10.3855/jidc.18138
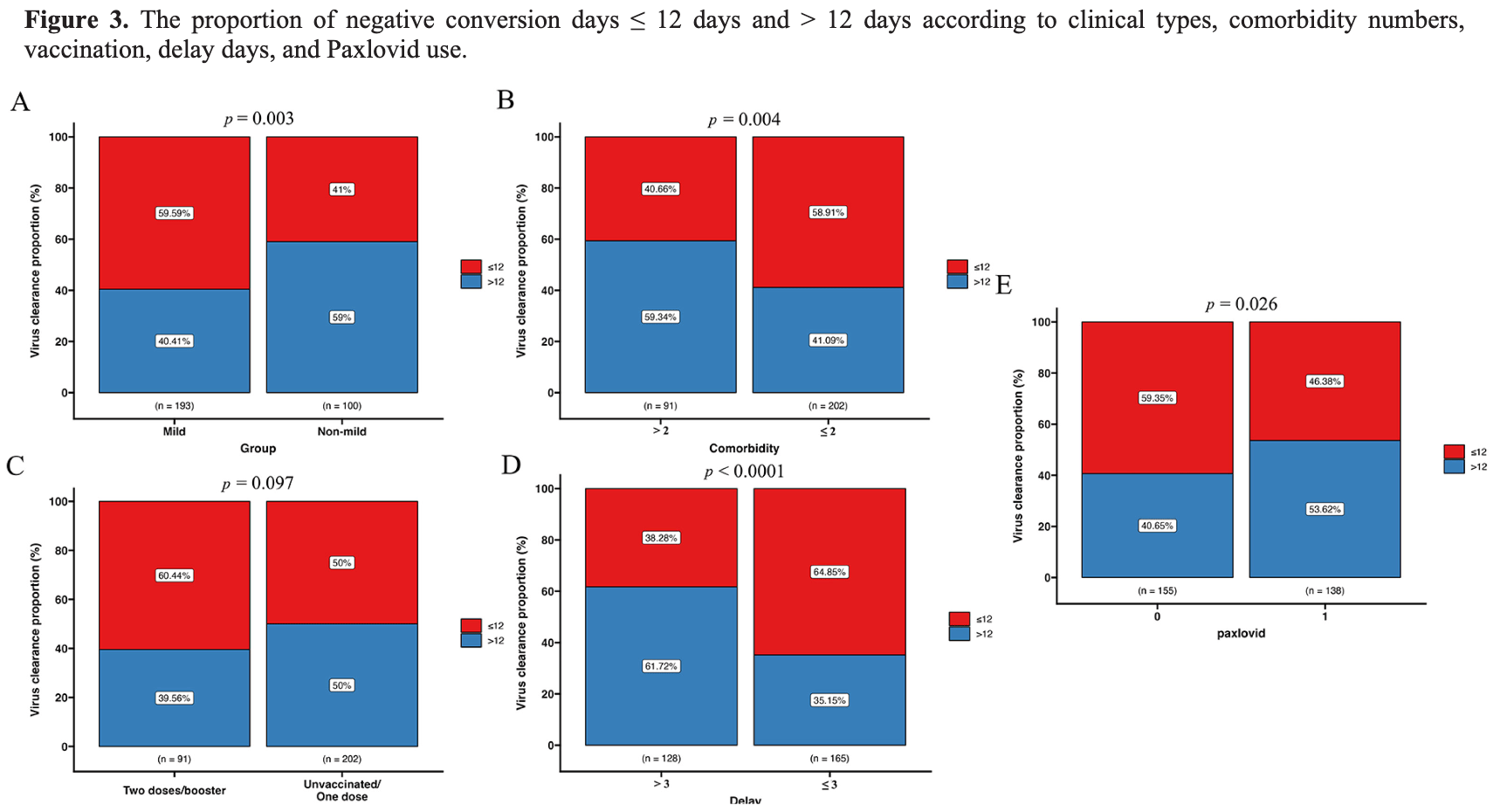
Introduction: The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) Omicron variant rapidly appeared in Shanghai, China in early March 2022. Although a few studies have analyzed the risk factors of the severe type, identifying risk factors for non-mild COVID-19 outcomes (general/severe/critical type) which occur with radiographic evidence of pneumonia is lacking. Methodology: The COVID-19 patients admitted to a district-level designated hospital from April 26 to May 21 were enrolled in this retrospective study. The clinical manifestations and laboratory examinations were analyzed. Logistic regression was employed to evaluate risk factors for non-mild outcomes. Results: Of the 311 patients, 196 (63.0%) were mild and 115 (37.0%) were non-mild. Among them, 215 cases (69.1%) were unvaccinated. Male, ≥ 60 years age, and chronic kidney disease were risk factors of progressing to non-mild. Patients with more than two comorbidities were more likely to become non-mild, whereas two/booster doses vaccinated patients had a lower risk of developing to non-mild. The median negative conversion days (NCDs) were 12 days. Non-mild, > 2 comorbidities, delayed admission (> 3 days), and Paxlovid (Pfizer, Freiburg, Germany) treatment significantly lengthened the NCDs. Conclusions: Our results call for special concern for full and booster vaccination of the elderly, which will effectively protect from progression of COVID-19 to non-mild state. In the meantime, symptomatic COVID-19 patients should be treated as soon as possible.
Conflict of interests: No conflict of interests is declared. Supplementary Figure 1 . Differential indicators from laboratory results among mild, general, severe/critical patients.
Annex -Supplementary Items Supplementary The indicators include lymphocyte count, A/G ratio, myoglobin, troponin T, D-dimer, and inflammatory markers (CRP, IL-6, and IL-10).
References
Albitar, Ballouze, Ooi, Ghadzi, Risk factors for mortality among COVID-19 patients, Diabetes Res Clin Pract, doi:10.1016/j.diabres.2020.108293
Biswas, Rahaman, Biswas, Haque, Association of sex, age, and comorbidities with mortality in COVID-19 patients: a systematic review and meta-analysis, Intervirology, doi:10.1159/000512592
Boucau, Uddin, Marino, Regan, Flynn et al., Characterization of virologic rebound following nirmatrelvir-ritonavir treatment for COVID-19, Clin Infect Dis, doi:10.1101/2022.05.24.22275326
Charness, Gupta, Stack, Strymish, Lindy et al., Rebound of SARS-CoV-2 infection after nirmatrelvir-ritonavir treatment, N Engl J Med, doi:10.1056/NEJMc2206449
Chen, Deng, Fang, Sun, Wu et al., Epidemiological characteristics and transmission dynamics of the outbreak caused by the SARS-CoV-2 Omicron variant in Shanghai, China: a descriptive study, Lancet Reg Health West Pac, doi:10.1016/j.lanwpc.2022.100592
Chen, Liang, Hu, Li, Wang et al., Research progress in methods for detecting neutralizing antibodies against SARS-CoV-2, Anal Biochem, doi:10.1016/j.ab.2023.115199
Chen, Zhou, Dong, Qu, Gong et al., Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study, Lancet, doi:10.1016/S0140-6736(20)30211-7
Cheung, Chan, Jin, Lessons learned from the fifth wave of COVID-19 in Hong Kong in early, Emerg Microbes Infect, doi:10.1080/22221751.2022.2060137
Council, Group, Chronic kidney disease is a key risk factor for severe COVID-19: a call to action by the ERA-EDTA, Nephrol Dial Transplant, doi:10.1093/ndt/gfaa314
Dai, Lee, Nathanson, Leonelli, Petros et al., Viral kinetics of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) Omicron infection in mRNA-vaccinated individuals treated and not treated with nirmatrelvir-ritonavir, medRxiv, doi:10.1101/2022.08.04.22278378
Damayanthi, Prabani, Weerasekara, Factors associated for mortality of older people with COVID 19: a systematic review and meta-analysis, Gerontol Geriatr Med, doi:10.1177/23337214211057392
Gou, Ping, Lei, Yu, Tao et al., Initial clinical characteristics of 146 patients with COVID-19 reported in Guizhou Province, China: a survival analysis, J Infect Dev Ctries, doi:10.3855/jidc.15027
He, Zhu, Fu, Xiao, Zhao et al., Association between COVID-19 vaccination coverage and case fatality ratio: a comparative study -Hong Kong SAR, China and Singapore, December 2021, China CDC Wkly
Huang, Wang, Li, Ren, Zhao et al., Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China, Lancet, doi:10.1016/S0140-6736(20)30183-5
Iketani, Liu, Guo, Chan, Huang et al., Antibody evasion properties of SARS-CoV-2 Omicron sublineages, Nature, doi:10.1038/s41586-022-04594-4
Li, Zhu, Zhang, Liu, Ji et al., Nutritional status is closely related to the severity of COVID-19: a multi-center retrospective study, J Infect Dev Ctries, doi:10.3855/jidc.14178
Liu, Chen, Hou, Li, Cao et al., An inter-correlated cytokine network identified at the center of cytokine storm predicted COVID-19 prognosis, Cytokine, doi:10.1016/j.cyto.2020.155365
Liu, Li, Liu, Luo, Li et al., Developing a multivariable risk prediction model to predict prolonged viral clearance in patients with COVID-19, J Infect, doi:10.1016/j.jinf.2020.12.026
Liu, Mao, Liang, Yang, Lu et al., Association between age and clinical characteristics and outcomes of COVID-19, Eur Respir J, doi:10.1183/13993003.01112-2020
Lu, Zhang, Zhang, He, Yuan et al., Geriatric risk and protective factors for serious COVID-19 outcomes among older adults in Shanghai Omicron wave, Emerg Microbes Infect, doi:10.1080/22221751.2022.2109517
Rostami, Mansouritorghabeh, D-dimer level in COVID-19 infection: a systematic review, Expert Rev Hematol, doi:10.1080/17474086.2020.1831383
Sandoval, Januzzi, Jaffe, Cardiac troponin for assessment of myocardial injury in COVID-19: JACC Review Topic of the Week, J Am Coll Cardiol, doi:10.1016/j.jacc.2020.06.068
Shrestha, Foster, Rawlinson, Tedla, Bull, Evolution of the SARS-CoV-2 omicron variants BA.1 to BA.5: implications for immune escape and transmission, Rev Med Virol, doi:10.1002/rmv.2381
Smith, Hakim, Leung, Xu, Schluter et al., COVID-19 mortality and vaccine coverage -Hong Kong Special Administrative Region, China, MMWR Morb Mortal Wkly Rep, doi:10.15585/mmwr.mm7115e1
Sun, Lin, Wang, Gao, Ye, Paxlovid in patients who are immunocompromised and hospitalised with SARS-CoV-2 infection, Lancet Infect Dis, doi:10.1016/S1473-3099(22)00430-3
Tian, Sun, Zhou, Ye, The global epidemic of SARS-CoV-2 variants and their mutational immune escape, J Med Virol, doi:10.1002/jmv.27376
Wang, Berger, Davis, Kaelber, Volkow et al., COVID-19 rebound after Paxlovid and Molnupiravir during January, doi:10.1101/2022.06.21.22276724
Wang, Chen, Zhao, Feng, Rapid COVID-19 rebound in a severe COVID-19 patient during 20day course of Paxlovid, J Infect, doi:10.1016/j.jinf.2022.08.012
Wang, Guo, Iketani, Nair, Li et al., Antibody evasion by SARS-CoV-2 Omicron subvariants BA.2.12.1, BA.4 and BA.5, doi:10.1038/s41586-022-05053-w
Who, Coronavirus disease (COVID-19) pandemic
Xu, Chen, Yuan, Yi, Ding et al., Factors associated with prolonged viral RNA shedding in patients with coronavirus disease 2019 (COVID-19), Clin Infect Dis, doi:10.1093/cid/ciaa351
Yang, Liao, Yin, Wang, Yue et al., Elevated cardiac biomarkers may be effective prognostic predictors for patients with COVID-19: a multicenter, observational study, Am J Emerg Med, doi:10.1016/j.ajem.2020.10.013
Yao, Cao, Wang, Shi, Liu et al., D-dimer as a biomarker for disease severity and mortality in COVID-19 patients: a case control study, J Intensive Care, doi:10.1186/s40560-020-00466-z
Zhang, Yue, Wang, Wang, Wu et al., The dynamics of immune response in COVID-19 patients with different illness severity, J Med Virol, doi:10.1002/jmv.26504
Zhang, Zhang, Chen, Shanghai's life-saving efforts against the current Omicron wave of the COVID-19 pandemic, Lancet, doi:10.1016/S0140-6736(22)00838-8
Zhang, Zhang, Zhang, SARS-CoV-2 variants, immune escape, and countermeasures, Front Med, doi:10.1007/s11684-021-0906-x
Zhou, Yu, Du, Fan, Liu et al., Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study, Lancet, doi:10.1016/S0140-6736(20)30566-3
DOI record:
{
"DOI": "10.3855/jidc.18138",
"ISSN": [
"1972-2680"
],
"URL": "http://dx.doi.org/10.3855/jidc.18138",
"abstract": "<jats:p>Introduction: The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) Omicron variant rapidly appeared in Shanghai, China in early March 2022. Although a few studies have analyzed the risk factors of the severe type, identifying risk factors for non-mild COVID-19 outcomes (general/severe/critical type) which occur with radiographic evidence of pneumonia is lacking.\nMethodology: The COVID-19 patients admitted to a district-level designated hospital from April 26 to May 21 were enrolled in this retrospective study. The clinical manifestations and laboratory examinations were analyzed. Logistic regression was employed to evaluate risk factors for non-mild outcomes.\nResults: Of the 311 patients, 196 (63.0%) were mild and 115 (37.0%) were non-mild. Among them, 215 cases (69.1%) were unvaccinated. Male, ≥ 60 years age, and chronic kidney disease were risk factors of progressing to non-mild. Patients with more than two comorbidities were more likely to become non-mild, whereas two/booster doses vaccinated patients had a lower risk of developing to non-mild. The median negative conversion days (NCDs) were 12 days. Non-mild, > 2 comorbidities, delayed admission (> 3 days), and Paxlovid (Pfizer, Freiburg, Germany) treatment significantly lengthened the NCDs.\nConclusions: Our results call for special concern for full and booster vaccination of the elderly, which will effectively protect from progression of COVID-19 to non-mild state. In the meantime, symptomatic COVID-19 patients should be treated as soon as possible.</jats:p>",
"author": [
{
"affiliation": [],
"family": "Zhu",
"given": "Wen",
"sequence": "first"
},
{
"affiliation": [],
"family": "Wang",
"given": "Haowei",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Zhou",
"given": "Hai",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-6529-288X",
"affiliation": [],
"authenticated-orcid": false,
"family": "Cheng",
"given": "Lei",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Weng",
"given": "Chao",
"sequence": "additional"
}
],
"container-title": "The Journal of Infection in Developing Countries",
"container-title-short": "J Infect Dev Ctries",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2024,
2,
19
]
],
"date-time": "2024-02-19T21:31:48Z",
"timestamp": 1708378308000
},
"deposited": {
"date-parts": [
[
2024,
2,
19
]
],
"date-time": "2024-02-19T21:31:48Z",
"timestamp": 1708378308000
},
"indexed": {
"date-parts": [
[
2024,
2,
20
]
],
"date-time": "2024-02-20T00:33:54Z",
"timestamp": 1708389234169
},
"is-referenced-by-count": 0,
"issue": "01",
"issued": {
"date-parts": [
[
2024,
1,
31
]
]
},
"journal-issue": {
"issue": "01",
"published-online": {
"date-parts": [
[
2024,
1,
31
]
]
}
},
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0",
"content-version": "unspecified",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2024,
1,
31
]
],
"date-time": "2024-01-31T00:00:00Z",
"timestamp": 1706659200000
}
}
],
"link": [
{
"URL": "https://www.jidc.org/index.php/journal/article/download/18138/3255",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://www.jidc.org/index.php/journal/article/download/18138/3255",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "2222",
"original-title": [],
"page": "44-52",
"prefix": "10.3855",
"published": {
"date-parts": [
[
2024,
1,
31
]
]
},
"published-online": {
"date-parts": [
[
2024,
1,
31
]
]
},
"publisher": "Journal of Infection in Developing Countries",
"reference-count": 0,
"references-count": 0,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.jidc.org/index.php/journal/article/view/18138"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Virology",
"Infectious Diseases",
"General Medicine",
"Microbiology",
"Parasitology"
],
"subtitle": [],
"title": "Clinical characteristics and risk factors of non-mild outcomes in patients with Omicron variant COVID-19 in Shanghai, China",
"type": "journal-article",
"volume": "18"
}