The APOLLO Trial: A Proof-of-Concept Study for Vitamin A Nasal Drops in COVID-19 Related Post-Infectious Olfactory Dysfunction
et al., Chemical Senses, doi:10.1093/chemse/bjag001, APOLLO, ISRCTN13142505, Jan 2026
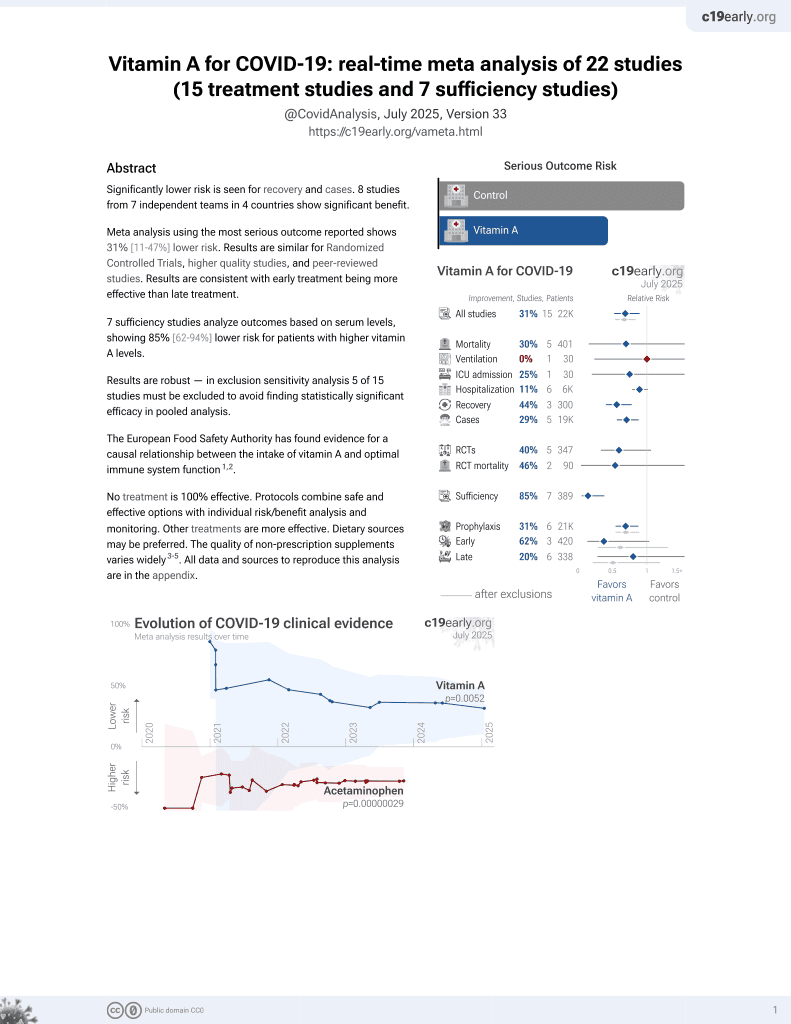
Vitamin A for COVID-19
49th treatment shown to reduce risk in
May 2023, now with p = 0.004 from 14 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
RCT 57 COVID-19 patients with post-infectious olfactory dysfunction showing no significant difference with intranasal vitamin A versus placebo drops. Authors hypothesize that COVID-19's mechanism of damaging sustentacular cells rather than olfactory receptor neurons directly may explain why vitamin A, which promotes olfactory neuron regeneration, did not show a significant effect here.
Standard of Care (SOC) for COVID-19 in the study country,
the United Kingdom, is very poor with very low average efficacy for approved treatments1.
The United Kingdom focused on expensive high-profit treatments, approving only one low-cost early treatment, which required a prescription and had limited adoption. The high-cost prescription treatment strategy reduces the probability of early treatment due to access and cost barriers, and eliminates complementary and synergistic benefits seen with many low-cost treatments.
|
risk of no recovery, 50.4% higher, RR 1.50, p = 0.54, treatment mean 2.58 (±7.19) n=30, control mean 3.88 (±5.17) n=15, ΔTDI.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Yeap et al., 20 Jan 2026, Double Blind Randomized Controlled Trial, placebo-controlled, United Kingdom, peer-reviewed, mean age 47.2, 12 authors, study period July 2022 - October 2022, post-COVID olfactory dysfunction, trial ISRCTN13142505 (APOLLO).
The APOLLO Trial: A Proof-of-Concept Study for Vitamin A Nasal Drops in COVID-19 Related Post-Infectious Olfactory Dysfunction
doi:10.1093/chemse/bjag001/8430749
Post-infectious olfactory dysfunction (PIOD) is common in COVID-19 patients. This two-arm double-blinded randomised controlled trial aimed to establish proof-of-concept for Vitamin A versus placebo as a treatment modality for patients with PIOD. This study compared 9000 IU daily self-administered vitamin A intranasal drops versus peanut oil drops over 12 weeks in COVID-19 patients with PIOD. Outcome measures included: olfactory bulb volume (OBV), olfactory sulcus depth, cerebral functional MRI Blood Oxygen Level Dependent (BOLD) signal, Sniffin' Sticks TDI score, SSParoT, Olfactory
Protocol The published protocol can be found online at: https://rdcu.be/elYva (Kumaresan et al. 2023) .
References
Addison, Philpott, A systematic review of therapeutic options for non-conductive olfactory dysfunction, The Otorhinolaryngologist
Alexander, Lee, Lazar, Field, Diffusion tensor imaging of the brain, Neurotherapeutics
Balmer, Blomhoff, Gene expression regulation by retinoic acid, J Lipid Res
Bonfils, Avan, Faulcon, Malinvaud, Distorted odorant perception: analysis of a series of 56 patients with parosmia, Arch Otolaryngol Head Neck Surg
Boscolo-Rizzo, Hummel, Spinato, Vaira, Menini et al., Olfactory and gustatory function 3 years after mild COVID-19-a cohort psychophysical study, JAMA Otolaryngology-Head & Neck Surgery
Bourganis, Kammona, Alexopoulos, Kiparissides, Recent advances in carrier mediated nose-to-brain delivery of pharmaceutics, European journal of pharmaceutics and biopharmaceutics
Brann, Tsukahara, Weinreb, Lipovsek, Van Den Berge et al., Non-neuronal expression of SARS-CoV-2 entry genes in the olfactory system suggests mechanisms underlying COVID-19-associated anosmia, Sci Adv
Breiman, Random forests, Machine Learning
Butowt, Bartheld, Anosmia in COVID-19: Underlying Mechanisms and Assessment of an Olfactory Route to Brain Infection, Neuroscientist
Chen, Wang, The immune mechanism of the nasal epithelium in COVID-19-related olfactory dysfunction, Front Immunol
Chung, Zhang, Wong, Sridhar, Lee et al., A Pilot Study of Short-Course Oral Vitamin A and Aerosolised Diffuser Olfactory Training for the Treatment of Smell Loss in Long COVID, Brain Sciences
Cusack, Vicente-Grabovetsky, Mitchell, Wild, Auer et al., Automatic analysis (aa): efficient neuroimaging workflows and parallel processing using Matlab and XML, Front Neuroinform
Damm, Schmitl, Müller, Welge-Lüssen, Hummel, Diagnostics and treatment of olfactory dysfunction, Hno
Devanand, Olfactory identification deficits, cognitive decline, and dementia in older adults, The American Journal of Geriatric Psychiatry
Douaud, Lee, Alfaro-Almagro, Arthofer, Wang et al., SARS-CoV-2 is associated with changes in brain structure in UK Biobank, Nature
Duncan, Briggs, Treatment of uncomplicated anosmia by vitamin A, Arch Otolaryngol
Erskine, Philpott, An unmet need: Patients with smell and taste disorders, Clin Otolaryngol
Espehana, Lee, Garden, Klyvyte, Gokani et al., Delivery of topical drugs to the olfactory cleft, Journal of Clinical Medicine
Finlay, Brann, Hachem, Jang, Oliva et al., Persistent post-COVID-19 smell loss is associated with immune cell infiltration and altered gene expression in olfactory epithelium, Science translational medicine
Garden, Espehana, Boak, Gadi, Philpott, Commentary on Patient Advocacy and Research Priorities in Olfactory and Gustatory Disorders, Current otorhinolaryngology reports
Garrett-Laster, Russell, Jacques, Impairment of taste and olfaction in patients with cirrhosis: the role of vitamin A, Hum Nutr Clin Nutr
Genicot, Ap, Gousenbourger, Lambiotte, Sami, Coupled Tensor Decomposition: a Step Towards Robust Components, IEEE proceedings of EUSIPCO
Glibbery, Boak, Turner, Philpott, Comparing Quality of Life in Smell and Taste Disorders with other Chronic Conditions -A Narrative Review Authorea
Gokani, Ta, Espehana, Garden, Klyvyte et al., The growing burden of long COVID in the United Kingdom: Insights from the UK Coronavirus Infection Survey, International forum of allergy & rhinology
Gopinath, Russell, Sue, Flood, Burlutsky et al., Olfactory impairment in older adults is associated with poorer diet quality over 5 years, Eur J Nutr
Gänger, Schindowski, Tailoring formulations for intranasal nose-to-brain delivery: a review on architecture, physico-chemical characteristics and mucociliary clearance of the nasal olfactory mucosa, Pharmaceutics
Güllmar, Seeliger, Gudziol, Teichgräber, Reichenbach et al., Improvement of olfactory function after sinus surgery correlates with white matter properties measured by diffusion tensor imaging, Neuroscience
Han, Winkler, Hummel, Hahner, Gerber et al., Impaired brain response to odors in patients with varied severity of olfactory loss after traumatic brain injury, J Neurol
Harris, Taylor, Thielke, Payne, Gonzalez et al., Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support, J Biomed Inform
Hummel, Whitcroft, Andrews, Altundag, Cinghi et al., a. Position paper on olfactory dysfunction, Rhinol Suppl
Hummel, Whitcroft, Rueter, Haehner, Intranasal vitamin A is beneficial in post-infectious olfactory loss, Eur Arch Otorhinolaryngol
Jafek, Murrow, Michaels, Restrepo, Linschoten, Biopsies of human olfactory epithelium, Chem Senses
Josefsson, Larsson, Nordin, Adolfsson, Olofsson, APOE-ɛ4 effects on longitudinal decline in olfactory and non-olfactory cognitive abilities in middle-aged and old adults, Scientific Reports Apr
Khan, Yoo, Clijsters, Backaert, Vanstapel et al., Visualizing in deceased COVID-19 patients how SARS-CoV-2 attacks the respiratory and olfactory mucosae but spares the olfactory bulb, Cell
Kumaresan, Bengtsson, Sami, Clark, Hummel et al., A double-blinded randomised controlled trial of vitamin A drops to treat post-viral olfactory loss: study protocol for a proof-of-concept study for vitamin A nasal drops in post-viral olfactory loss (APOLLO), Pilot Feasibility Stud
Langstaff, Clark, Salam, Philpott, Cultural Adaptation and Validity of the Sniffin' Sticks Psychophysical Test for the UK Setting, Chemosensory Perception
Langstaff, Pradhan, Clark, Boak, Salam et al., Validation of the olfactory disorders questionnaire for English-speaking patients with olfactory disorders, Clin Otolaryngol
Lechner, Liu, Counsell, Gillespie, Chandrasekharan et al., The burden of olfactory dysfunction during the COVID-19 pandemic in the United Kingdom, Rhinology
Lee, Choi, Lee, Lee, Sohn et al., Microstructural white matter alterations in patients with drug induced parkinsonism, Hum Brain Mapp
Lee, Luke, Boak, Philpott, Impact of olfactory disorders on personal safety and well-being: a cross-sectional observational study, Eur Arch Otorhinolaryngol
Li, Feng, Lin, Huang, Liu et al., Cognition-related white matter integrity dysfunction in Alzheimer's disease with diffusion tensor image, Brain Res Bull
Liu, Welge-Lüssen, Besser, Mueller, Renner, Assessment of odor hedonic perception: the Sniffin' sticks parosmia test (SSParoT), Sci Rep
Lötsch, Brosig, Slobodova, Kringel, Haehner et al., Diagnosed and subjectively perceived long-term effects of COVID-19 infection on olfactory function assessed by supervised machine learning, Chemical Senses
Mclaren, Kawaja, Olfactory Dysfunction and Alzheimer's Disease: A Review, J Alzheimers Dis
Menni, Valdes, Freidin, Sudre, Nguyen et al., Real-time tracking of self-reported symptoms to predict potential COVID-19, Nature Medicine
Mori, Merkonidis, Cuevas, Gudziol, Matsuwaki et al., The administration of nasal drops in the "Kaiteki" position allows for delivery of the drug to the olfactory cleft: a pilot study in healthy subjects, Eur Arch Otorhinolaryngol
Olofsson, Larsson, Roa, Wilson, Laukka, Interaction between odor identification deficit and APOE4 predicts 6-year cognitive decline in elderly individuals, Otolaryngol Head Neck Surg
Parma, Ohla, Veldhuizen, Niv, Kelly et al., More Than Smell-COVID-19 Is Associated With Severe Impairment of Smell, Taste, and Chemesthesis, Chem Senses
Paschaki, Cammas, Muta, Matsuoka, Mak et al., Retinoic acid regulates olfactory progenitor cell fate and differentiation, Neural Dev
Penny, Friston, Ashburner, Kiebel, Nichols, Statistical parametric mapping: T he
DOI record:
{
"DOI": "10.1093/chemse/bjag001",
"ISSN": [
"0379-864X",
"1464-3553"
],
"URL": "http://dx.doi.org/10.1093/chemse/bjag001",
"abstract": "<jats:title>Abstract</jats:title>\n <jats:p>Post-infectious olfactory dysfunction (PIOD) is common in COVID-19 patients. This two-arm double-blinded randomised controlled trial aimed to establish proof-of-concept for Vitamin A versus placebo as a treatment modality for patients with PIOD.</jats:p>\n <jats:p>This study compared 9000 IU daily self-administered vitamin A intranasal drops versus peanut oil drops over 12 weeks in COVID-19 patients with PIOD. Outcome measures included: olfactory bulb volume (OBV), olfactory sulcus depth, cerebral functional MRI Blood Oxygen Level Dependent (BOLD) signal, Sniffin’ Sticks TDI score, SSParoT, Olfactory Disorder Questionnaire (ODQ) score and Brain Derived Neurotropic Factor (BDNF) levels were collected from participants at baseline and after trial intervention at 12 weeks.</jats:p>\n <jats:p>Fifty-seven PIOD were recruited in the trial and allocated to Vitamin A or placebo arm at a 2:1 ratio. After withdrawals and exclusions, 30 participants in the Vitamin A arm and 15 in the placebo arm were analysed. There was no significant difference in the change in OBV between both groups. Aside from an improvement in quality-of-life component of ODQ questionnaire scores (p = 0.01), there were no significant differences in any of the other secondary outcome measures.</jats:p>\n <jats:p>This proof-of-concept trial has demonstrated no significant effect of intranasal Vitamin A on olfactory function in COVID-19 PIOD patients. Further work is required to identify other therapeutic agents in the management of PIOD or evaluate a different PIOD cohort with non-COVID aetiology.</jats:p>",
"article-number": "bjag001",
"author": [
{
"ORCID": "https://orcid.org/0000-0003-4353-1277",
"affiliation": [
{
"name": "Rhinology & Olfactology Research Group, Norwich Medical School, University of East Anglia , Norwich ,",
"place": [
"UK"
]
},
{
"name": "Norfolk Smell & Taste Clinic, James Paget University Hospital NHS Trust , Gorleston ,",
"place": [
"UK"
]
}
],
"authenticated-orcid": false,
"family": "Yeap",
"given": "Z",
"sequence": "first"
},
{
"affiliation": [
{
"name": "Sir Peter Mansfield Imaging Centre, University of Nottingham"
},
{
"name": "Norwich Medical School, University of East Anglia , Norwich ,",
"place": [
"UK"
]
}
],
"family": "Sobhan",
"given": "R",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "School of Psychology, University of East Anglia , Norwich ,",
"place": [
"UK"
]
}
],
"family": "Bengtsson",
"given": "S L",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Norwich Medical School, University of East Anglia , Norwich ,",
"place": [
"UK"
]
}
],
"family": "Sami",
"given": "S",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Norwich Medical School, University of East Anglia , Norwich ,",
"place": [
"UK"
]
}
],
"family": "Clark",
"given": "A B",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Norwich Medical School, University of East Anglia , Norwich ,",
"place": [
"UK"
]
}
],
"family": "Vishwakarma",
"given": "R",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "SmellTaste , Chinor ,",
"place": [
"UK"
]
}
],
"family": "Boardman",
"given": "J",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Norwich Medical School, University of East Anglia , Norwich ,",
"place": [
"UK"
]
}
],
"family": "High",
"given": "J",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Norwich Medical School, University of East Anglia , Norwich ,",
"place": [
"UK"
]
}
],
"family": "Klyvyte",
"given": "G",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Norwich Medical School, University of East Anglia , Norwich ,",
"place": [
"UK"
]
}
],
"family": "Ergisi",
"given": "M",
"sequence": "additional"
},
{
"ORCID": "https://orcid.org/0000-0001-9713-0183",
"affiliation": [
{
"name": "Interdisciplinary Center “Smell and Taste”, Department of Otorhinolaryngology, Technical University of Dresden ,",
"place": [
"Germany"
]
}
],
"authenticated-orcid": false,
"family": "Hummel",
"given": "T",
"sequence": "additional"
},
{
"ORCID": "https://orcid.org/0000-0002-1125-3236",
"affiliation": [
{
"name": "Rhinology & Olfactology Research Group, Norwich Medical School, University of East Anglia , Norwich ,",
"place": [
"UK"
]
},
{
"name": "Norfolk Smell & Taste Clinic, James Paget University Hospital NHS Trust , Gorleston ,",
"place": [
"UK"
]
},
{
"name": "SmellTaste , Chinor ,",
"place": [
"UK"
]
}
],
"authenticated-orcid": false,
"family": "Philpott",
"given": "C M",
"sequence": "additional"
}
],
"container-title": "Chemical Senses",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2026,
1,
18
]
],
"date-time": "2026-01-18T12:35:22Z",
"timestamp": 1768739722000
},
"deposited": {
"date-parts": [
[
2026,
1,
20
]
],
"date-time": "2026-01-20T06:23:12Z",
"timestamp": 1768890192000
},
"indexed": {
"date-parts": [
[
2026,
1,
20
]
],
"date-time": "2026-01-20T20:01:19Z",
"timestamp": 1768939279793,
"version": "3.49.0"
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2026,
1,
20
]
]
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "am",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2026,
1,
20
]
],
"date-time": "2026-01-20T00:00:00Z",
"timestamp": 1768867200000
}
}
],
"link": [
{
"URL": "https://academic.oup.com/chemse/advance-article-pdf/doi/10.1093/chemse/bjag001/66468344/bjag001.pdf",
"content-type": "application/pdf",
"content-version": "am",
"intended-application": "syndication"
},
{
"URL": "https://academic.oup.com/chemse/advance-article-pdf/doi/10.1093/chemse/bjag001/66468344/bjag001.pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "286",
"original-title": [],
"prefix": "10.1093",
"published": {
"date-parts": [
[
2026,
1,
20
]
]
},
"published-online": {
"date-parts": [
[
2026,
1,
20
]
]
},
"publisher": "Oxford University Press (OUP)",
"reference-count": 0,
"references-count": 0,
"relation": {},
"resource": {
"primary": {
"URL": "https://academic.oup.com/chemse/advance-article/doi/10.1093/chemse/bjag001/8430749"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"title": "<b>The APOLLO Trial: A P</b>\n roof-of-Concept Study for Vitamin A Nasal Drops in COVID-19 Related Post-Infectious\n <b>Ol</b>\n factory Dysfunction",
"type": "journal-article"
}