COVID-19 and sunlight: Impact on SARS-CoV-2 transmissibility, morbidity, and mortality
et al., Annals of Medicine and Surgery, doi:10.1016/j.amsu.2021.102419, Jun 2021
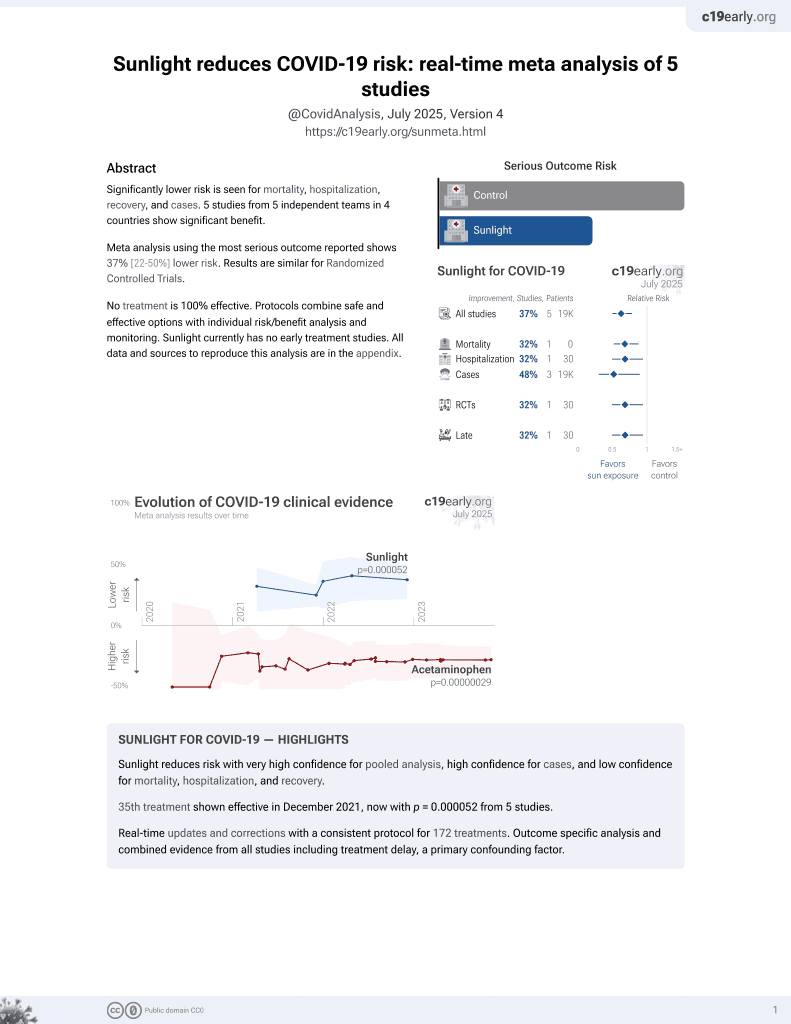
Sunlight for COVID-19
36th treatment shown to reduce risk in
December 2021, now with p = 0.000052 from 5 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Review of evidence for the benefits of sunlight exposure for COVID-19.
1.
Gong et al., Natural and socio-environmental factors in the transmission of COVID-19: a comprehensive analysis of epidemiology and mechanisms, BMC Public Health, doi:10.1186/s12889-024-19749-3.
2.
Limaheluw et al., Associations between meteorological factors and COVID-19: a global scoping review, Frontiers in Public Health, doi:10.3389/fpubh.2024.1183706.
3.
Seheult, R., The Case for Sunlight in COVID 19 Patients: Oxidative Stress, MedCram, www.youtube.com/watch?v=2Zzo4SJopcY&t=268s.
Sharun et al., 30 Jun 2021, peer-reviewed, 3 authors.
Contact: sharunkhansk@gmail.com, kdhama@rediffmail.com.
COVID-19 and sunlight: Impact on SARS-CoV-2 transmissibility, morbidity, and mortality
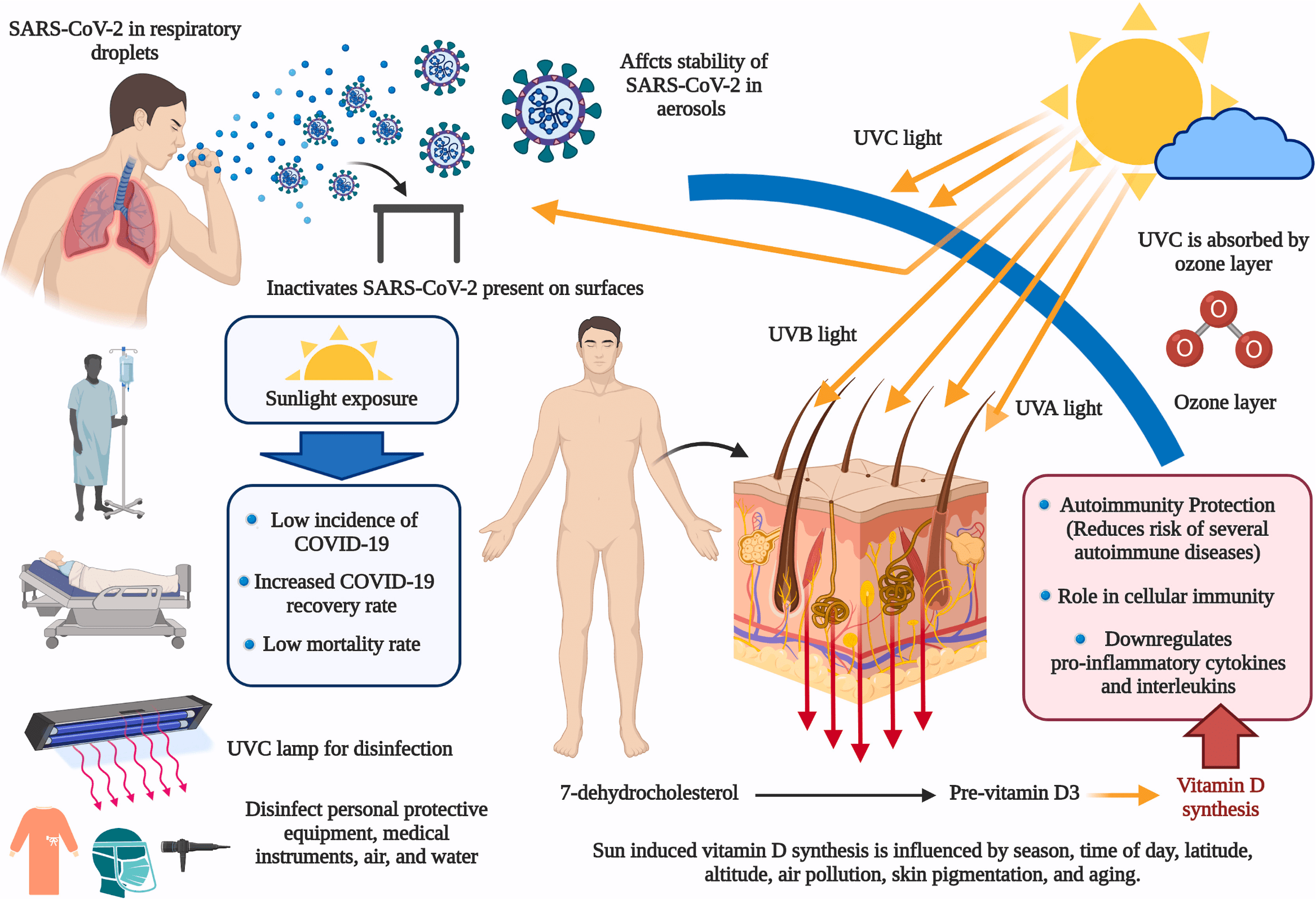
Coronavirus disease 2019 (COVID-19) has already affected millions of people worldwide. There are reports of SARS-CoV-2 transmission as a consequence of environmental contamination. The SARS-CoV-2 laden infective droplets can actively persist on the surface of different materials for several hours to days. Sunlight can affect the stability of SARS-CoV-2 in these aerosols and thereby have an impact on the decay rate of the virus. Solar radiation might play an important role in inactivating SARS-CoV-2 that persists in different surfaces and the environment. Among the different climatological factors, ultraviolet radiation was found to have an important role in determining the spread of SARS-CoV-2. Although ultraviolet radiation C (UVC), UVB, UVA, visible light, and infrared radiation possess germicidal properties, human CoVs including the recently emerged SARS-CoV-2 are inherently sensitive to UVC. However, the successful decontamination using other wavebands requires higher dosages and longer administration times. Furthermore, studies have also identified association between COVID-19 fatalities and the latitude. The intensity of sunlight is highest near the equator, and therefore populations in these regions with more regular exposure to sunlight are less susceptible to vitamin D deficiency. This article has analyzed the potential impact of sunlight in reducing SARS-CoV-2 transmissibility, morbidity, and mortality. It is evident that there exists an interesting link between sunlight exposure, latitude, and vitamin D status with COVID-19 incidence, fatality and recovery rates that requires further investigation.
Author contribution All authors contributed equally -study concept or design, data collection, data analysis or interpretation, writing the paper.
Research registration number 1. Name of the registry: Not applicable. 2. Unique Identifying number or registration ID: Not applicable. 3. Hyperlink to your specific registration (must be publicly accessible and will be checked): Not applicable.
Guarantor Dr. Khan Sharun, Division of Surgery, ICAR-Indian Veterinary Research Institute, Izatnagar, Bareilly-243 122, Uttar Pradesh, India. Email: sharunkhansk@gmail.com. Dr. Kuldeep Dhama, Division of Pathology, ICAR-Indian Veterinary Research Institute, Izatnagar, Bareilly-243 122, Uttar Pradesh, India. Email: kdhama@rediffmail.com.
Provenance and peer review Not Commissioned, internally reviewed.
Consent Not applicable.
Declaration of competing interest All authors declare that there exist no commercial or financial relationships that could, in any way, lead to a potential conflict of interest.
References
Almeida, Faustino, Neves, Antimicrobial photodynamic therapy in the control of COVID-19, Antibiotics, doi:10.3390/antibiotics9060320
Asyary, Veruswati, Sunlight exposure increased Covid-19 recovery rates: a study in the central pandemic area of Indonesia, Sci. Total Environ, doi:10.1016/j.scitotenv.2020.139016
Cacho, Hernández, López-Hoyos, Martínez-Taboada, Can climatic factors explain the differences in COVID-19 incidence and severity across the Spanish regions?: an ecological study, Environ. Health, doi:10.1186/s12940-020-00660-4
Carleton, Cornetet, Huybers, Meng, Proctor, Global evidence for ultraviolet radiation decreasing COVID-19 growth rates, Proc. Natl. Acad. Sci. U. S. A, doi:10.1073/pnas.2012370118
Criscuolo, Diotti, Ferrarese, Alippi, Viscardi et al., Fast inactivation of SARS-CoV-2 by UV-C and ozone exposure on different materials, Dec, Emerg. Microb. Infect, doi:10.1080/22221751.2021.1872354
Dhama, Khan, Tiwari, Sircar, Bhat et al., Coronavirus disease 2019-COVID-19, Clin. Microbiol. Rev, doi:10.1128/CMR.00028-20
Enwemeka, Baker, Greiner, Bumah, Masson-Meyers et al., Antimicrobial photodynamic therapy as a potential treatment against COVID-19: a case for blue light, Photobiomodul Photomed Laser Surg, doi:10.1089/photob.2020.4901
Fernandes, De Lima, Villaverde, Pereira, Carvalho et al., Photobiomodulation: shining light on COVID-19, Photobiomodul Photomed Laser Surg, doi:10.1089/photob.2020.4882
Gidari, Sabbatini, Bastianelli, Pierucci, Busti et al., SARS-CoV-2 survival on surfaces and the effect of UV-C light, Viruses, doi:10.3390/v13030408
Guasp, Laredo, Urra, Higher solar irradiance is associated with a lower incidence of coronavirus disease 2019, Clin. Infect. Dis, doi:10.1093/cid/ciaa575
Heilingloh, Aufderhorst, Schipper, Dittmer, Witzke et al., Susceptibility of SARS-CoV-2 to UV irradiation, Am. J. Infect. Contr, doi:10.1016/j.ajic.2020.07.031
Herman, Biegel, Huang, Inactivation times from 290 to 315 nm UVB in sunlight for SARS coronaviruses CoV and CoV-2 using OMI satellite data for the sunlit Earth, Air Qual Atmos Health, doi:10.1007/s11869-020-00927-2
Horton, Torres, Narla, Lyons, Kohli et al., Spectrum of virucidal activity from ultraviolet to infrared radiation, Photochem. Photobiol. Sci, doi:10.1039/d0pp00221f
Iqbal, Abid, Hussain, Shahzad, Waqas, The effects of regional climatic condition on the spread of COVID-19 at global scale, Sci. Total Environ, doi:10.1016/j.scitotenv.2020.140101
Isaia, Diémoz, Maluta, Fountoulakis, Ceccon et al., Does solar ultraviolet radiation play a role in COVID-19 infection and deaths? An environmental ecological study in Italy, Sci. Total Environ, doi:10.1016/j.scitotenv.2020.143757
Kohlmeier, Avoidance of vitamin D deficiency to slow the COVID-19 pandemic, BMJ Nutr Prev Health, doi:10.1136/bmjnph-2020-000096
Lansiaux, Pébaÿ, Picard, Forget, Covid-19 and vit-d: disease mortality negatively correlates with sunlight exposure, Spat Spatiotemporal Epidemiol, doi:10.1016/j.sste.2020.100362
Li, Guan, Wu, Wang, Zhou et al., Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia, N. Engl. J. Med, doi:10.1056/NEJMoa2001316
Mercola, Grant, Wagner, Evidence regarding vitamin D and risk of COVID-19 and its severity, Nutrients, doi:10.3390/nu12113361
Nakada, Urban, COVID-19 pandemic: environmental and social factors influencing the spread of SARS-CoV-2 in São Paulo, Brazil, Environ. Sci. Pollut. Res. Int, doi:10.1007/s11356-020-10930-w
O'connor, Courtney, Murphy, Shedding light on the myths of ultraviolet radiation in the COVID-19 pandemic, Clin. Exp. Dermatol, doi:10.1111/ced.14456
Rabaan, Al-Ahmed, Sah, Tiwari, Yatoo et al., SARS-CoV-2/COVID-19 and advances in developing potential therapeutics and vaccines to counter this emerging pandemic, Ann. Clin. Microbiol. Antimicrob, doi:10.1186/s12941-020-00384-w
Ran, Zhao, Han, Liao, Wang et al., A re-analysis in exploring the association between temperature and COVID-19 transmissibility: an ecological study with 154 Chinese cities, Eur. Respir. J, doi:10.1183/13993003.01253-2020
Ratnesar-Shumate, Williams, Green, Krause, Holland et al., Simulated sunlight rapidly inactivates SARS-CoV-2 on surfaces, J. Infect. Dis, doi:10.1093/infdis/jiaa274
Rhodes, Dunstan, Laird, Subramanian, Kenny, COVID-19 mortality increases with northerly latitude after adjustment for age suggesting a link with ultraviolet and vitamin D, BMJ Nutr Prev Health, doi:10.1136/bmjnph-2020-000110
Sabino, Ball, Baptista, Dai, Hamblin et al., Light-based technologies for management of COVID-19 pandemic crisis, J. Photochem. Photobiol., B, doi:10.1016/j.jphotobiol.2020.111999
Sagripanti, Lytle, Estimated inactivation of coronaviruses by solar radiation with special reference to COVID-19, Photochem. Photobiol, doi:10.1111/php.13293
Schuit, Ratnesar-Shumate, Yolitz, Williams, Weaver et al., Airborne SARS-CoV-2 is rapidly inactivated by simulated sunlight, J. Infect. Dis, doi:10.1093/infdis/jiaa334
Sharun, Sircar, Malik, Singh, Dhama, How close is SARS-CoV-2 to canine and feline coronaviruses?, J. Small Anim. Pract, doi:10.1111/jsap.13207
Sharun, Tiwari, Natesan, Yatoo, Malik et al., International travel during the COVID-19 pandemic: implications and risks associated with 'Travel Bubbles, J. Trav. Med, doi:10.1093/jtm/taaa184
Sharun, Tiwari, Yatoo, Patel, Natesan et al., Antibody-based immunotherapeutics and use of convalescent plasma to counter COVID-19: advances and prospects, Expet Opin. Biol. Ther, doi:10.1080/14712598.2020.1796963
Tang, Liu, Ren, Wu, Yu et al., Sunlight ultraviolet radiation dose is negatively correlated with the percent positive of SARS-CoV-2 and four other common human coronaviruses in the U.S, Sci. Total Environ, doi:10.1016/j.scitotenv.2020.141816
Vellingiri, Jayaramayya, Iyer, Narayanasamy, Govindasamy et al., COVID-19: a promising cure for the global panic, Sci. Total Environ
Wang, Sun, Zhang, Han, Solar heating to inactivate thermal-sensitive pathogenic microorganisms in vehicles: application to COVID-19, Environ. Chem. Lett, doi:10.1007/s10311-020-01132-4
Whittemore, COVID-19 fatalities, latitude, sunlight, and vitamin D, Am. J. Infect. Contr, doi:10.1016/j.ajic.2020.06.193
DOI record:
{
"DOI": "10.1016/j.amsu.2021.102419",
"ISSN": [
"2049-0801"
],
"URL": "http://dx.doi.org/10.1016/j.amsu.2021.102419",
"alternative-id": [
"S2049080121003691"
],
"article-number": "102419",
"assertion": [
{
"label": "This article is maintained by",
"name": "publisher",
"value": "Elsevier"
},
{
"label": "Article Title",
"name": "articletitle",
"value": "COVID-19 and sunlight: Impact on SARS-CoV-2 transmissibility, morbidity, and mortality"
},
{
"label": "Journal Title",
"name": "journaltitle",
"value": "Annals of Medicine and Surgery"
},
{
"label": "CrossRef DOI link to publisher maintained version",
"name": "articlelink",
"value": "https://doi.org/10.1016/j.amsu.2021.102419"
},
{
"label": "Content Type",
"name": "content_type",
"value": "simple-article"
},
{
"label": "Copyright",
"name": "copyright",
"value": "© 2021 The Authors. Published by Elsevier Ltd on behalf of IJS Publishing Group Ltd."
}
],
"author": [
{
"ORCID": "http://orcid.org/0000-0003-1040-3746",
"affiliation": [],
"authenticated-orcid": false,
"family": "Sharun",
"given": "Khan",
"sequence": "first"
},
{
"affiliation": [],
"family": "Tiwari",
"given": "Ruchi",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Dhama",
"given": "Kuldeep",
"sequence": "additional"
}
],
"container-title": "Annals of Medicine and Surgery",
"container-title-short": "Annals of Medicine and Surgery",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"clinicalkey.jp",
"clinicalkey.com",
"clinicalkey.es",
"clinicalkey.com.au",
"clinicalkey.fr",
"elsevier.com",
"sciencedirect.com"
]
},
"created": {
"date-parts": [
[
2021,
5,
30
]
],
"date-time": "2021-05-30T14:26:12Z",
"timestamp": 1622384772000
},
"deposited": {
"date-parts": [
[
2021,
6,
23
]
],
"date-time": "2021-06-23T10:59:23Z",
"timestamp": 1624445963000
},
"indexed": {
"date-parts": [
[
2022,
12,
19
]
],
"date-time": "2022-12-19T06:49:31Z",
"timestamp": 1671432571140
},
"is-referenced-by-count": 7,
"issued": {
"date-parts": [
[
2021,
6
]
]
},
"language": "en",
"license": [
{
"URL": "https://www.elsevier.com/tdm/userlicense/1.0/",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
6,
1
]
],
"date-time": "2021-06-01T00:00:00Z",
"timestamp": 1622505600000
}
},
{
"URL": "http://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
5,
23
]
],
"date-time": "2021-05-23T00:00:00Z",
"timestamp": 1621728000000
}
}
],
"link": [
{
"URL": "https://api.elsevier.com/content/article/PII:S2049080121003691?httpAccept=text/xml",
"content-type": "text/xml",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://api.elsevier.com/content/article/PII:S2049080121003691?httpAccept=text/plain",
"content-type": "text/plain",
"content-version": "vor",
"intended-application": "text-mining"
}
],
"member": "78",
"original-title": [],
"page": "102419",
"prefix": "10.1016",
"published": {
"date-parts": [
[
2021,
6
]
]
},
"published-print": {
"date-parts": [
[
2021,
6
]
]
},
"publisher": "Elsevier BV",
"reference": [
{
"DOI": "10.1128/CMR.00028-20",
"article-title": "Coronavirus disease 2019-COVID-19",
"author": "Dhama",
"doi-asserted-by": "crossref",
"issue": "4",
"journal-title": "Clin. Microbiol. Rev.",
"key": "10.1016/j.amsu.2021.102419_bib1",
"volume": "33",
"year": "2020"
},
{
"DOI": "10.1093/jtm/taaa184",
"article-title": "International travel during the COVID-19 pandemic: implications and risks associated with 'Travel Bubbles'",
"author": "Sharun",
"doi-asserted-by": "crossref",
"journal-title": "J. Trav. Med.",
"key": "10.1016/j.amsu.2021.102419_bib2",
"year": "2020"
},
{
"DOI": "10.1111/jsap.13207",
"article-title": "How close is SARS-CoV-2 to canine and feline coronaviruses?",
"author": "Sharun",
"doi-asserted-by": "crossref",
"first-page": "523",
"issue": "8",
"journal-title": "J. Small Anim. Pract.",
"key": "10.1016/j.amsu.2021.102419_bib3",
"volume": "61",
"year": "2020"
},
{
"DOI": "10.1186/s12941-020-00384-w",
"article-title": "SARS-CoV-2/COVID-19 and advances in developing potential therapeutics and vaccines to counter this emerging pandemic",
"author": "Rabaan",
"doi-asserted-by": "crossref",
"first-page": "40",
"issue": "1",
"journal-title": "Ann. Clin. Microbiol. Antimicrob.",
"key": "10.1016/j.amsu.2021.102419_bib4",
"volume": "19",
"year": "2020"
},
{
"DOI": "10.1080/14712598.2020.1796963",
"article-title": "Antibody-based immunotherapeutics and use of convalescent plasma to counter COVID-19: advances and prospects",
"author": "Sharun",
"doi-asserted-by": "crossref",
"first-page": "1033",
"issue": "9",
"journal-title": "Expet Opin. Biol. Ther.",
"key": "10.1016/j.amsu.2021.102419_bib5",
"volume": "20",
"year": "2020"
},
{
"DOI": "10.1016/j.scitotenv.2020.138277",
"article-title": "COVID-19: a promising cure for the global panic",
"author": "Vellingiri",
"doi-asserted-by": "crossref",
"first-page": "138277",
"journal-title": "Sci. Total Environ.",
"key": "10.1016/j.amsu.2021.102419_bib6",
"volume": "725",
"year": "2020"
},
{
"DOI": "10.1089/photob.2020.4901",
"article-title": "Antimicrobial photodynamic therapy as a potential treatment against COVID-19: a case for blue light",
"author": "Enwemeka",
"doi-asserted-by": "crossref",
"journal-title": "Photobiomodul Photomed Laser Surg",
"key": "10.1016/j.amsu.2021.102419_bib7",
"year": "2020"
},
{
"DOI": "10.1089/photob.2020.4882",
"article-title": "Photobiomodulation: shining light on COVID-19",
"author": "Fernandes",
"doi-asserted-by": "crossref",
"first-page": "395",
"issue": "7",
"journal-title": "Photobiomodul Photomed Laser Surg",
"key": "10.1016/j.amsu.2021.102419_bib8",
"volume": "38",
"year": "2020"
},
{
"DOI": "10.1093/infdis/jiaa274",
"article-title": "Simulated sunlight rapidly inactivates SARS-CoV-2 on surfaces",
"author": "Ratnesar-Shumate",
"doi-asserted-by": "crossref",
"first-page": "214",
"issue": "2",
"journal-title": "J. Infect. Dis.",
"key": "10.1016/j.amsu.2021.102419_bib9",
"volume": "222",
"year": "2020"
},
{
"DOI": "10.1016/j.jphotobiol.2020.111999",
"article-title": "Light-based technologies for management of COVID-19 pandemic crisis",
"author": "Sabino",
"doi-asserted-by": "crossref",
"first-page": "111999",
"journal-title": "J. Photochem. Photobiol., B",
"key": "10.1016/j.amsu.2021.102419_bib10",
"volume": "212",
"year": "2020"
},
{
"DOI": "10.1093/infdis/jiaa334",
"article-title": "Airborne SARS-CoV-2 is rapidly inactivated by simulated sunlight",
"author": "Schuit",
"doi-asserted-by": "crossref",
"first-page": "564",
"issue": "4",
"journal-title": "J. Infect. Dis.",
"key": "10.1016/j.amsu.2021.102419_bib11",
"volume": "222",
"year": "2020"
},
{
"DOI": "10.1080/22221751.2021.1872354",
"article-title": "Fast inactivation of SARS-CoV-2 by UV-C and ozone exposure on different materials",
"author": "Criscuolo",
"doi-asserted-by": "crossref",
"first-page": "206",
"issue": "1",
"journal-title": "Emerg. Microb. Infect.",
"key": "10.1016/j.amsu.2021.102419_bib12",
"volume": "10",
"year": "2021"
},
{
"DOI": "10.1039/D0PP00221F",
"article-title": "Spectrum of virucidal activity from ultraviolet to infrared radiation",
"author": "Horton",
"doi-asserted-by": "crossref",
"first-page": "1262",
"issue": "10",
"journal-title": "Photochem. Photobiol. Sci.",
"key": "10.1016/j.amsu.2021.102419_bib13",
"volume": "19",
"year": "2020"
},
{
"DOI": "10.1016/j.ajic.2020.07.031",
"article-title": "Susceptibility of SARS-CoV-2 to UV irradiation",
"author": "Heilingloh",
"doi-asserted-by": "crossref",
"first-page": "1273",
"issue": "10",
"journal-title": "Am. J. Infect. Contr.",
"key": "10.1016/j.amsu.2021.102419_bib14",
"volume": "48",
"year": "2020"
},
{
"DOI": "10.1016/j.scitotenv.2020.141816",
"article-title": "Sunlight ultraviolet radiation dose is negatively correlated with the percent positive of SARS-CoV-2 and four other common human coronaviruses in the U.S",
"author": "Tang",
"doi-asserted-by": "crossref",
"first-page": "141816",
"journal-title": "Sci. Total Environ.",
"key": "10.1016/j.amsu.2021.102419_bib15",
"volume": "751",
"year": "2021"
},
{
"DOI": "10.3390/v13030408",
"article-title": "SARS-CoV-2 survival on surfaces and the effect of UV-C light",
"author": "Gidari",
"doi-asserted-by": "crossref",
"first-page": "408",
"issue": "3",
"journal-title": "Viruses",
"key": "10.1016/j.amsu.2021.102419_bib16",
"volume": "13",
"year": "2021"
},
{
"article-title": "Shedding light on the myths of ultraviolet radiation in the COVID-19 pandemic",
"author": "O'Connor",
"journal-title": "Clin. Exp. Dermatol.",
"key": "10.1016/j.amsu.2021.102419_bib17",
"year": "2020"
},
{
"article-title": "Inactivation times from 290 to 315 nm UVB in sunlight for SARS coronaviruses CoV and CoV-2 using OMI satellite data for the sunlit Earth",
"author": "Herman",
"first-page": "1",
"journal-title": "Air Qual Atmos Health",
"key": "10.1016/j.amsu.2021.102419_bib18",
"year": "2020"
},
{
"DOI": "10.1016/j.scitotenv.2020.139016",
"article-title": "Sunlight exposure increased Covid-19 recovery rates: a study in the central pandemic area of Indonesia",
"author": "Asyary",
"doi-asserted-by": "crossref",
"first-page": "139016",
"journal-title": "Sci. Total Environ.",
"key": "10.1016/j.amsu.2021.102419_bib19",
"volume": "729",
"year": "2020"
},
{
"DOI": "10.1016/j.ajic.2020.06.193",
"article-title": "COVID-19 fatalities, latitude, sunlight, and vitamin D",
"author": "Whittemore",
"doi-asserted-by": "crossref",
"first-page": "1042",
"issue": "9",
"journal-title": "Am. J. Infect. Contr.",
"key": "10.1016/j.amsu.2021.102419_bib20",
"volume": "48",
"year": "2020"
},
{
"DOI": "10.3390/nu12113361",
"article-title": "Evidence regarding vitamin D and risk of COVID-19 and its severity",
"author": "Mercola",
"doi-asserted-by": "crossref",
"first-page": "E3361",
"issue": "11",
"journal-title": "Nutrients",
"key": "10.1016/j.amsu.2021.102419_bib21",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1136/bmjnph-2020-000096",
"article-title": "Avoidance of vitamin D deficiency to slow the COVID-19 pandemic",
"author": "Kohlmeier",
"doi-asserted-by": "crossref",
"first-page": "67",
"issue": "1",
"journal-title": "BMJ Nutr Prev Health",
"key": "10.1016/j.amsu.2021.102419_bib22",
"volume": "3",
"year": "2020"
},
{
"DOI": "10.1136/bmjnph-2020-000110",
"article-title": "COVID-19 mortality increases with northerly latitude after adjustment for age suggesting a link with ultraviolet and vitamin D",
"author": "Rhodes",
"doi-asserted-by": "crossref",
"first-page": "118",
"issue": "1",
"journal-title": "BMJ Nutr Prev Health",
"key": "10.1016/j.amsu.2021.102419_bib23",
"volume": "3",
"year": "2020"
},
{
"article-title": "COVID-19 pandemic: environmental and social factors influencing the spread of SARS-CoV-2 in São Paulo, Brazil",
"author": "Nakada",
"first-page": "1",
"journal-title": "Environ. Sci. Pollut. Res. Int.",
"key": "10.1016/j.amsu.2021.102419_bib24",
"year": "2020"
},
{
"DOI": "10.1016/j.sste.2020.100362",
"article-title": "Covid-19 and vit-d: disease mortality negatively correlates with sunlight exposure",
"author": "Lansiaux",
"doi-asserted-by": "crossref",
"first-page": "100362",
"journal-title": "Spat Spatiotemporal Epidemiol",
"key": "10.1016/j.amsu.2021.102419_bib25",
"volume": "35",
"year": "2020"
},
{
"article-title": "Does solar ultraviolet radiation play a role in COVID-19 infection and deaths? An environmental ecological study in Italy",
"author": "Isaia",
"first-page": "143757",
"journal-title": "Sci. Total Environ.",
"key": "10.1016/j.amsu.2021.102419_bib26",
"volume": "20",
"year": "2020"
},
{
"DOI": "10.1093/cid/ciaa575",
"article-title": "Higher solar irradiance is associated with a lower incidence of coronavirus disease 2019",
"author": "Guasp",
"doi-asserted-by": "crossref",
"first-page": "2269",
"issue": "16",
"journal-title": "Clin. Infect. Dis.",
"key": "10.1016/j.amsu.2021.102419_bib27",
"volume": "71",
"year": "2020"
},
{
"DOI": "10.1056/NEJMoa2001316",
"article-title": "Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia",
"author": "Li",
"doi-asserted-by": "crossref",
"first-page": "1199",
"issue": "13",
"journal-title": "N. Engl. J. Med.",
"key": "10.1016/j.amsu.2021.102419_bib28",
"volume": "382",
"year": "2020"
},
{
"DOI": "10.1111/php.13293",
"article-title": "Estimated inactivation of coronaviruses by solar radiation with special reference to COVID-19",
"author": "Sagripanti",
"doi-asserted-by": "crossref",
"first-page": "731",
"issue": "4",
"journal-title": "Photochem. Photobiol.",
"key": "10.1016/j.amsu.2021.102419_bib29",
"volume": "96",
"year": "2020"
},
{
"DOI": "10.1186/s12940-020-00660-4",
"article-title": "Can climatic factors explain the differences in COVID-19 incidence and severity across the Spanish regions?: an ecological study",
"author": "Cacho",
"doi-asserted-by": "crossref",
"first-page": "106",
"issue": "1",
"journal-title": "Environ. Health",
"key": "10.1016/j.amsu.2021.102419_bib30",
"volume": "19",
"year": "2020"
},
{
"DOI": "10.1073/pnas.2012370118",
"article-title": "Global evidence for ultraviolet radiation decreasing COVID-19 growth rates",
"author": "Carleton",
"doi-asserted-by": "crossref",
"issue": "1",
"journal-title": "Proc. Natl. Acad. Sci. U. S. A.",
"key": "10.1016/j.amsu.2021.102419_bib31",
"volume": "118",
"year": "2021"
},
{
"DOI": "10.1016/j.scitotenv.2020.140101",
"article-title": "The effects of regional climatic condition on the spread of COVID-19 at global scale",
"author": "Iqbal",
"doi-asserted-by": "crossref",
"first-page": "140101",
"journal-title": "Sci. Total Environ.",
"key": "10.1016/j.amsu.2021.102419_bib32",
"volume": "739",
"year": "2020"
},
{
"DOI": "10.1183/13993003.01253-2020",
"article-title": "A re-analysis in exploring the association between temperature and COVID-19 transmissibility: an ecological study with 154 Chinese cities",
"author": "Ran",
"doi-asserted-by": "crossref",
"issue": "2",
"journal-title": "Eur. Respir. J.",
"key": "10.1016/j.amsu.2021.102419_bib33",
"volume": "56",
"year": "2020"
},
{
"article-title": "Solar heating to inactivate thermal-sensitive pathogenic microorganisms in vehicles: application to COVID-19",
"author": "Wang",
"first-page": "1",
"journal-title": "Environ. Chem. Lett.",
"key": "10.1016/j.amsu.2021.102419_bib34",
"year": "2020"
},
{
"DOI": "10.3390/antibiotics9060320",
"article-title": "Antimicrobial photodynamic therapy in the control of COVID-19",
"author": "Almeida",
"doi-asserted-by": "crossref",
"first-page": "320",
"issue": "6",
"journal-title": "Antibiotics (Basel)",
"key": "10.1016/j.amsu.2021.102419_bib35",
"volume": "9",
"year": "2020"
}
],
"reference-count": 35,
"references-count": 35,
"relation": {},
"resource": {
"primary": {
"URL": "https://linkinghub.elsevier.com/retrieve/pii/S2049080121003691"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"General Medicine",
"Surgery"
],
"subtitle": [],
"title": "COVID-19 and sunlight: Impact on SARS-CoV-2 transmissibility, morbidity, and mortality",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1016/elsevier_cm_policy",
"volume": "66"
}