Back to the Basics of SARS-CoV-2 Biochemistry: Microvascular Occlusive Glycan Bindings Govern Its Morbidities and Inform Therapeutic Responses
et al., Viruses, doi:10.3390/v16040647, NCT04727424, Apr 2024
31st treatment shown to reduce risk in
November 2021, now with p = 0.00014 from 21 studies, recognized in 2 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
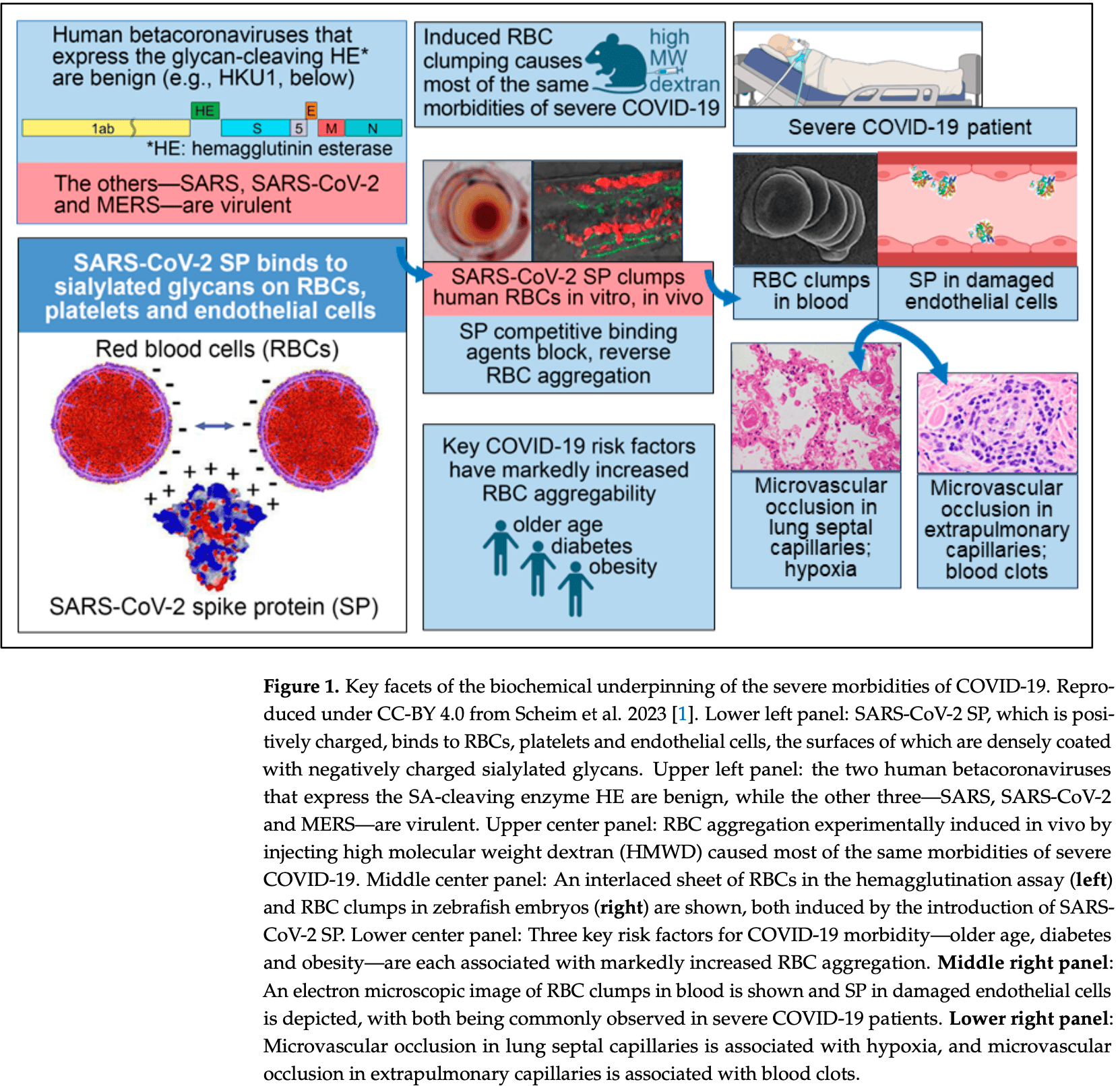
Review of the biochemical underpinnings of the severe morbidities of COVID-19, focusing on the binding of the SARS-CoV-2 spike protein (SP) to sialylated glycans on host cell surfaces. Authors highlight how the SP attaches particularly tightly to the trillions of red blood cells (RBCs), platelets, and endothelial cells in the human body, triggering blood cell aggregation, microvascular occlusion, and vascular damage that lead to the hypoxia, blood clotting, and related morbidities of severe COVID-19. Authors note that RBC aggregation experimentally induced in several animal species caused most of the same morbidities of severe COVID-19, and suggest that the glycan biochemistry is important for understanding the efficacy of certain generic COVID-19 treatments like ivermectin.
The authors suggest that ivermectin may be an effective treatment for COVID-19 due to its ability to competitively bind to the SARS-CoV-2 spike protein and prevent the protein's attachment to host cell glycans. In silico studies found that ivermectin binds with high affinity to multiple sites on the spike protein, especially on the N-terminal domain, which governs the protein's glycan interactions. Clinical studies observed rapid normalization of peripheral oxygen saturation in severe COVID-19 patients treated with ivermectin, which parallels the rapid disaggregation of ivermectin-treated red blood cell clumps in vitro. Authors note that these benefits may be less relevant for milder infections with reduced penetration into the bloodstream.
The authors suggest that treatments targeting the glycan-mediated pathology of COVID-19, particularly those that reduce red blood cell and platelet aggregation, may be beneficial for severe cases. Authors also discuss the potential of hydroxychloroquine and fluvoxamine in this context, as these treatments have been shown to reduce blood cell aggregation.
Review covers ivermectin, HCQ, and fluvoxamine.
1.
Scheim et al., Back to the Basics of SARS-CoV-2 Biochemistry: Microvascular Occlusive Glycan Bindings Govern Its Morbidities and Inform Therapeutic Responses, Viruses, doi:10.3390/v16040647.
2.
Hashimoto, K., Overview of the potential use of fluvoxamine for COVID-19 and long COVID, Discover Mental Health, doi:10.1007/s44192-023-00036-3.
3.
Hashimoto (B) et al., Mechanisms of action of fluvoxamine for COVID-19: a historical review, Molecular Psychiatry, doi:10.1038/s41380-021-01432-3.
4.
Hashimoto (C) et al., Old drug fluvoxamine, new hope for COVID-19, European Archives of Psychiatry and Clinical Neuroscience, doi:10.1007/s00406-021-01326-z.
5.
Hoertel et al., Repurposing antidepressants inhibiting the sphingomyelinase acid/ceramide system against COVID-19: current evidence and potential mechanisms, Molecular Psychiatry, doi:10.1038/s41380-021-01254-3.
Scheim et al., 22 Apr 2024, Australia, peer-reviewed, 8 authors, study period 7 July, 2021 - 1 April, 2023, trial NCT04727424 (history).
Contact: dscheim@alum.mit.edu (corresponding author), p.parry1@uq.edu.au, aldousc@ukzn.ac.za.
Back to the Basics of SARS-CoV-2 Biochemistry: Microvascular Occlusive Glycan Bindings Govern Its Morbidities and Inform Therapeutic Responses
doi:10.3390/v16040000
Consistent with the biochemistry of coronaviruses as well established over decades, SARS-CoV-2 makes its initial attachment to host cells through the binding of its spike protein (SP) to sialylated glycans (containing the monosaccharide sialic acid) on the cell surface. The virus can then slide over and enter via ACE2. SARS-CoV-2 SP attaches particularly tightly to the trillions of red blood cells (RBCs), platelets and endothelial cells in the human body, each cell very densely coated with sialic acid surface molecules but having no ACE2 or minimal ACE2. These interlaced attachments trigger the blood cell aggregation, microvascular occlusion and vascular damage that underlie the hypoxia, blood clotting and related morbidities of severe COVID-19. Notably, the two human betacoronaviruses that express a sialic acid-cleaving enzyme are benign, while the other three-SARS, SARS-CoV-2 and MERS-are virulent. RBC aggregation experimentally induced in several animal species using an injected polysaccharide caused most of the same morbidities of severe COVID-19. This glycan biochemistry is key to disentangling controversies that have arisen over the efficacy of certain generic COVID-19 treatment agents and the safety of SP-based COVID-19 vaccines. More broadly, disregard for the active physiological role of RBCs yields unreliable or erroneous reporting of pharmacokinetic parameters as routinely obtained for most drugs and other bioactive agents using detection in plasma, with whole-blood levels being up to 30-fold higher. Appreciation of the active role of RBCs can elucidate the microvascular underpinnings of other health conditions, including cardiovascular disease, and therapeutic opportunities to address them.
Supplementary Materials: The following are available online at https://www.mdpi.com/article/ 10.3390/v16040000/s1, Table S1 : Changes in SpO2 for 34 COVID-19 patients treated with IVM, doxycycline and zinc, as reported by Stone et al. (2022) , Table S2 : Changes in SpO2 for 19 COVID-19 patients treated with IVM, doxycycline and zinc, as reported by Hazan et al. (2021) , Table S3 : Changes in SpO2 for 19 COVID-19 patients treated with IVM, zinc and vitamin C, with some also given azithromycin and hydroxychloroquine, as reported by Babalola et al. (2021) , Table S4 : Changes in SpO2 for 26 COVID-19 patients treated without IVM using different combinations of lopinavir/ritonavir, remdesivir, azithromycin, enoxaparin, zinc sulfate and vitamin C, as reported by Thairu et al., Table S5 : Means and standard errors of SpO2 changes from day 0 to day 1 and from day 0 to day 2 for the full set of 26 patients from Thairu et al. (2022) and for the subset of 18 patients who were on room air (without oxygen supplementation or ventilation).
Appendix A. Notes and Calculations on Surface Area and Extent of Sialylation of RBCs and Endothelial Cells in Human Vasculature In an average human adult, the blood contains 25 trillion RBCs [34, 35] , each with a surface area of 163 µm 2 [126], yielding a total surface area of about 4075 m 2 . The blood also contains nearly one trillion platelets [190] , and the vasculature is lined with one trillion endothelial cells having a total..
References
Ahmetaj-Shala, Vaja, Atanur, George, Kirkby et al., Cardiorenal Tissues Express SARS-CoV-2 Entry Genes and Basigin (BSG/CD147) Increases with Age in Endothelial Cells, JACC Basic Transl. Sci, doi:10.1016/j.jacbts.2020.09.010
Ali, The effect of ivermectin on some haematological indices in rabbits: Influence of vitamin K treatment, Clin. Exp. Pharmacol. Physiol, doi:10.1111/j.1440-1681.1990.tb01273.x
Alipoor, Mirsaeidi, SARS-CoV-2 cell entry beyond the ACE2 receptor, Mol. Biol. Rep, doi:10.1007/s11033-022-07700-x
Aminpour, Cannariato, Safaeeardebili, Preto, Moracchiato et al., In Silico Analysis of the Multi-Targeted Mode of Action of Ivermectin and Related Compounds, Computation, doi:10.3390/computation10040051
Angell, Industry-Sponsored Clinical Research: A Broken System, JAMA, doi:10.1001/jama.300.9.1069
Assayag, Bova, Kesler, Berliner, Shapira et al., Erythrocyte aggregation as an early biomarker in patients with asymptomatic carotid stenosis, Dis. Markers, doi:10.1155/2008/184647
Babalola, Bingham University, Karu, Personal communication
Babalola, Ndanusa, Adesuyi, Ogedengbe, Thairu et al., A Randomized Controlled Trial of Ivermectin Monotherapy Versus HCQ, IVM, and AZ Combination Therapy in COVID-19 Patients in Nigeria, J. Infect. Dis. Epidemiol, doi:10.23937/2474-3658/1510233
Baker, Richards, Guy, Congdon, Hasan et al., The SARS-CoV-2 Spike Protein Binds Sialic Acids and Enables Rapid Detection in a Lateral Flow Point of Care Diagnostic Device, ACS Cent. Sci, doi:10.1021/acscentsci.0c00855
Baraka, Mahmoud, Marschke, Geary, Homeida et al., Ivermectin distribution in the plasma and tissues of patients infected with Onchocerca volvulus, Eur. J. Clin. Pharmacol, doi:10.1007/s002280050131
Barnard, Alford-Lawrence, Buchholz, Wasik, Laclair et al., Modified Sialic Acids on Mucus and Erythrocytes Inhibit Influenza A Virus Hemagglutinin and Neuraminidase Functions, J. Virol, doi:10.1128/JVI.01567-19
Baum, Ward, Conway, Natural selection on the erythrocyte surface, Mol. Biol. Evol, doi:10.1093/oxfordjournals.molbev.a004075
Bellone, Siegel, Scheim, Santin, Increased von Willebrand and Factor VIII plasma levels in gynecologic patients with Post-Acute-COVID-Sequela (PASC)/Long COVID, Gynecol. Oncol. Rep, doi:10.1016/j.gore.2024.101324
Bergqvist, Domeij-Nyberg, Distribution of chloroquine and its metabolite desethyl-chloroquine in human blood cells and its implication for the quantitative determination of these compounds in serum and plasma, J. Chromatogr, doi:10.1016/S0378-4347(00)86110-1
Berndt, Kyle, Ling, The Long Shadow of Patent Expiration: Generic Entry and Rx-to-OTC Switches, Scanner Data and Price Indexes
Berzuini, Bianco, Migliorini, Maggioni, Valenti et al., Red blood cell morphology in patients with COVID-19-related anaemia, Blood Transfus
Biagiotti, Pirla, Magnani, Drug transport by red blood cells, Front. Physiol, doi:10.3389/fphys.2023.1308632
Biasutto, Marotta, Garbisa, Zoratti, Paradisi, Determination of Quercetin and Resveratrol in Whole Blood -Implications for Bioavailability Studies, Molecules, doi:10.3390/molecules15096570
Bicher, Blood Cell Aggregation in Thrombotic Processes; Chapter I: Red cell aggregation in thrombotic disease, trauma and shock
Biddinger, Emdin, Haas, Wang, Hindy et al., Association of Habitual Alcohol Intake with Risk of Cardiovascular Disease, JAMA Netw. Open, doi:10.1001/jamanetworkopen.2022.3849
Bjoerk, Intonti, Nordlund, Correlation between sludge in the bulbar conjunctiva and the mesentery, Ann. Surg
Born, Palinski, Unusually high concentrations of sialic acids on the surface of vascular endothelia, Br. J. Exp. Pathol
Borody, Clancy, Combination Therapy For COVID-19 Based on Ivermectin in an Australian Population, Trialsite News
Boschi, Scheim, Bancod, Militello, Bideau et al., SARS-CoV-2 Spike Protein Induces Hemagglutination: Implications for COVID-19 Morbidities and Therapeutics and for Vaccine Adverse Effects, Int. J. Mol. Sci, doi:10.3390/ijms232415480
Brogna, Cristoni, Marino, Montano, Viduto et al., Detection of recombinant Spike protein in the blood of individuals vaccinated against SARS-CoV-2: Possible molecular mechanisms, PROTEOMICS -Clin. Appl, doi:10.1002/prca.202300048
Byrnes, Wolberg, Red blood cells in thrombosis, Blood, doi:10.1182/blood-2017-03-745349
Campbell, Boilard, Rondina, Is there a role for the ACE2 receptor in SARS-CoV-2 interactions with platelets?, J. Thromb. Haemost, doi:10.1111/jth.15156
Campbell, History of avermectin and ivermectin, with notes on the history of other macrocyclic lactone antiparasitic agents, Curr. Pharm. Biotechnol, doi:10.2174/138920112800399095
Carvalho, Lerner, Resveratrol in Rheumatological Diseases: A Systematic Review, Eur. J. Rheumatol
Catalgol, Batirel, Taga, Ozer, Resveratrol: French paradox revisited, Front. Pharmacol, doi:10.3389/fphar.2012.00141
Cecchi, Ferraris, Desludging Action of Hydroxychloroquine in R.A, Acta Rheumatol. Scand
Chaccour, Hammann, Rabinovich, Ivermectin to reduce malaria transmission I. Pharmacokinetic and pharmacodynamic considerations regarding efficacy and safety, Malar. J, doi:10.1186/s12936-017-1801-4
Chahla, Medina Ruiz, Ortega, Morales Rn, Barreiro et al., Intensive Treatment with Ivermectin and Iota-Carrageenan as Pre-exposure Prophylaxis for COVID-19 in Health Care Workers From Tucuman, Argentina, European Congress of Clinical Microbiology and Infectious Diseases, doi:10.1097/MJT.0000000000001433
Chamie, Hibberd, Scheim, COVID-19 Excess Deaths in Peru's 25 States in 2020: Nationwide Trends, Confounding Factors, and Correlations with the Extent of Ivermectin Treatment by State, Cureus, doi:10.7759/cureus.43168
Chang, Lindstrom, Olson, Belew, Analysis of HIV Wild-Type and Mutant Structures via in Silico Docking against Diverse Ligand Libraries, J. Chem. Inf. Model, doi:10.1021/ci700044s
Chiu, Chen, Hsu, Hua, Tseng et al., Changes of ECG parameters after BNT162b2 vaccine in the senior high school students, Eur. J. Pediatr, doi:10.1007/s00431-022-04786-0
Cognetti, Miller, Monitoring Serum Spike Protein with Disposable Photonic Biosensors Following SARS-CoV-2 Vaccination, Sensors, doi:10.3390/s21175857
Cohen, Varki, Chapter Three-Modulation of Glycan Recognition by Clustered Saccharide Patches
Cohen, Varki, The sialome-far more than the sum of its parts, Omics, doi:10.1089/omi.2009.0148
Cosic, Cosic, Loncarevic, RRM Prediction of Erythrocyte Band3 Protein as Alternative Receptor for SARS-CoV-2 Virus, Appl. Sci, doi:10.3390/app10114053
Craddock, Mahajan, Spikes, Krishnamachary, Ram et al., Persistent circulation of soluble and extracellular vesicle-linked Spike protein in individuals with postacute sequelae of COVID-19, J. Med. Virol, doi:10.1002/jmv.28568
D'agnillo, Walters, Xiao, Sheng, Scherler et al., Lung epithelial and endothelial damage, loss of tissue repair, inhibition of fibrinolysis, and cellular senescence in fatal COVID-19, Sci. Transl. Med, doi:10.1126/scitranslmed.abj7790
Dal Canto, Ceriello, Rydén, Ferrini, Hansen et al., Diabetes as a cardiovascular risk factor: An overview of global trends of macro and micro vascular complications, Eur. J. Prev. Cardiol, doi:10.1177/2047487319878371
De Boer, Meijer, Wijnstok, Jonk, Houben et al., Microvascular Dysfunction: A Potential Mechanism in the Pathogenesis of Obesity-associated Insulin Resistance and Hypertension, Microcirculation, doi:10.1111/j.1549-8719.2011.00130.x
Ditzel, Angioscopic Changes in the Smaller Blood Vessels in Diabetes Mellitus and their Relationship to Aging, Circulation, doi:10.1161/01.CIR.14.3.386
Duthaler, Suenderhauf, Karlsson, Hussner, Meyer Zu Schwabedissen et al., Population pharmacokinetics of oral ivermectin in venous plasma and dried blood spots in healthy volunteers, Br. J. Clin. Pharmacol, doi:10.1111/bcp.13840
Edwards, Pierangeli, Liu, Barker, Anderson et al., Hydroxychloroquine Reverses Thrombogenic Properties of Antiphospholipid Antibodies in Mice, Circulation, doi:10.1161/01.CIR.96.12.4380
Email, Fullegar, Reis, Edmund Fordham, Screenshot, Email Addresses Redacted
Erikssen, Liestol, Bjornholt, Stormorken, Thaulow et al., Erythrocyte sedimentation rate: A possible marker of atherosclerosis and a strong predictor of coronary heart disease mortality, Eur. Heart J, doi:10.1053/euhj.2000.2148
Eslick, Tilden, Arora, Torres, Clancy, Clinical and economic impact of "triple therapy" for Helicobacter pylori eradication on peptic ulcer disease in Australia, Helicobacter, doi:10.1111/hel.12751
Faksova, Walsh, Jiang, Griffin, Phillips et al., COVID-19 vaccines and adverse events of special interest: A multinational Global Vaccine Data Network (GVDN) cohort study of 99 million vaccinated individuals, Vaccine, doi:10.1016/j.vaccine.2024.01.100
Favaron, Ince, Hilty, Ergin, Van Der Zee et al., Capillary Leukocytes, Microaggregates, and the Response to Hypoxemia in the Microcirculation of Coronavirus Disease 2019 Patients, Crit. Care Med, doi:10.1097/CCM.0000000000004862
Feenstra, Shapiro, None
Food, None, Clinical Pharmacology/Biopharmaceutics Review
Gagneux, Varki, Evolutionary considerations in relating oligosaccharide diversity to biological function, Glycobiology, doi:10.1093/glycob/9.8.747
Gal, Praksch, Kenyeres, Rabai, Toth et al., Hemorheological Alterations in Patients with Heart Failure with Reduced Ejection Fraction Treated by Resveratrol, Cardiovasc. Ther, doi:10.1155/2020/7262474
Gameil, Marzouk, Elsebaie, Rozaik, Long-term clinical and biochemical residue after COVID-19 recovery. Egypt, Liver J, doi:10.1186/s43066-021-00144-1
Gan, Zinno, Piano, Gunsalus, Omicron Spike Protein Has a Positive Electrostatic Surface That Promotes ACE2 Recognition and Antibody Escape, Front. Virol, doi:10.3389/fviro.2022.894531
Ganier, Du-Harpur, Harun, Wan, Arthurs et al., CD147 (BSG) but not ACE2 expression is detectable in vascular endothelial cells within single cell RNA sequencing datasets derived from multiple tissues in healthy individuals, bioRxiv, doi:10.1101/2020.05.29.123513
Gedik, Bozdogan, Yavuz, Durmaz, Erol, The assesment of retina and optic disc vascular structures in people who received CoronaVac vaccine, Photodiagnosis Photodyn. Ther, doi:10.1016/j.pdpdt.2022.102742
Gedik, Erol, Suren, Yavuz, Kucuk et al., Evaluation of retinal and optic disc vascular structures in individuals before and after Pfizer-BioNTech vaccination, Microvasc. Res, doi:10.1016/j.mvr.2023.104500
George, Borody, Andrews, Devine, Moore-Jones et al., Cure of duodenal ulcer after eradication of Helicobacter pylori, Med. J. Aust, doi:10.5694/j.1326-5377.1990.tb136833.x
Ghahramani, Tabrizi, Lankarani, Kashani, Rezaei et al., Laboratory features of severe vs. non-severe COVID-19 patients in Asian populations: A systematic review and meta-analysis, Eur. J. Med. Res, doi:10.1186/s40001-020-00432-3
González Canga, Sahagún Prieto, Diez Liébana, Fernández Martínez, Sierra et al., The Pharmacokinetics and Interactions of Ivermectin in Humans-A Mini-review, AAPS J, doi:10.1208/s12248-007-9000-9
Goshua, Pine, Meizlish, Chang, Zhang et al., Endotheliopathy in COVID-19-associated coagulopathy: Evidence from a single-centre, cross-sectional study, Lancet Haematol, doi:10.1016/S2352-3026(20)30216-7
Gossen, Zhang, Nikolov, Fernando, King, Binding behavior of receptor binding domain of the SARS-CoV-2 virus and ivermectin, Sci. Rep, doi:10.1038/s41598-024-53086-0
Gotzsche, False individual patient data and zombie randomised controlled trials submitted to Anaesthesia, Anaesthesia, doi:10.1111/anae.15263
Grobler, Maphumulo, Grobbelaar, Bredenkamp, Laubscher et al., COVID-19: The Rollercoaster of Fibrin(Ogen), D-Dimer, Von Willebrand Factor, P-Selectin and Their Interactions with Endothelial Cells, Platelets and Erythrocytes, Int. J. Mol. Sci, doi:10.3390/ijms21145168
Gundry, Abstract 10712: Observational Findings of PULS Cardiac Test Findings for Inflammatory Markers in Patients Receiving mRNA Vaccines, Circulation, doi:10.1161/circ.144.suppl_1.10712
Guzzo, Furtek, Porras, Chen, Tipping et al., Safety, tolerability, and pharmacokinetics of escalating high doses of ivermectin in healthy adult subjects, J. Clin. Pharmacol, doi:10.1177/009127002237994
Haider, Bengs, Schade, Wijnen, Portmann et al., Myocardial 18F-FDG Uptake Pattern for Cardiovascular Risk Stratification in Patients Undergoing Oncologic PET/CT, J. Clin. Med, doi:10.3390/jcm9072279
Hao, Ma, Li, Wang, Gao et al., Binding of the SARS-CoV-2 spike protein to glycans, Sci. Bull, doi:10.1016/j.scib.2021.01.010
Harbi, Hussien, Hawasawi, Alshdoukhi, Chopra et al., Red Blood Cells and Lipoproteins: Important Reservoirs and Transporters of Polyphenols and Their Metabolites, J. Agric. Food Chem, doi:10.1021/acs.jafc.0c02601
Hassan, Tarek, COVID 19 m-RNA (Pfizer) vaccination impairs cardiac functions in adult male rats, Bull. Egypt. Soc. Physiol. Sci, doi:10.21608/besps.2023.213045.1144
Haugaard, Dreyer, Ottosen, Gislason, Kofoed et al., Use of hydroxychloroquine and risk of major adverse cardiovascular events in patients with lupus erythematosus: A Danish nationwide cohort study, J. Am. Acad. Dermatol, doi:10.1016/j.jaad.2020.12.013
Hayward, Yu, Little, Gbinigie, Shanyinde et al., Ivermectin for COVID-19 in adults in the community (PRINCIPLE): An open, randomised, controlled, adaptive platform trial of short-and longer-term outcomes, doi:10.1016/S0140-6736(15)60696-1
Hazan, Dave, Gunaratne, Dolai, Clancy et al., Effectiveness of ivermectin-based multidrug therapy in severely hypoxic, ambulatory COVID-19 patients, Future Microbiol, doi:10.2217/fmb-2022-0014
Helms, Tacquard, Severac, Leonard-Lorant, Ohana et al., High risk of thrombosis in patients with severe SARS-CoV-2 infection: A multicenter prospective cohort study, Intensive Care Med, doi:10.1007/s00134-020-06062-x
Hikmet, Méar, Edvinsson, Micke, Uhlén et al., The protein expression profile of ACE2 in human tissues, Mol. Syst. Biol, doi:10.15252/msb.20209610
Hilton, Blood platelets, Sci. Prog
Hinderling, Red blood cells: A neglected compartment in pharmacokinetics and pharmacodynamics, Pharmacol. Rev
Hsieh, Wu, Resveratrol: Biological and pharmaceutical properties as anticancer molecule, Biofactors, doi:10.1002/biof.105
Hui, Ho, Cheung, Ng, Ching et al., SARS-CoV-2 Omicron variant replication in human bronchus and lung ex vivo, Nature, doi:10.1038/s41586-022-04479-6
Hulswit, De Haan, Bosch, Chapter Two-Coronavirus Spike Protein and Tropism Changes
Ioannidis, Evidence-based medicine has been hijacked: A report to David Sackett, J. Clin. Epidemiol, doi:10.1016/j.jclinepi.2016.02.012
Jaffe, Cell biology of endothelial cells, Human. Pathol, doi:10.1016/S0046-8177(87)80005-9
Jorge, Lu, Choi, Esdaile, Lacaille et al., Hydroxychloroquine Use and Cardiovascular Events Among Patients with Systemic Lupus Erythematosus and Rheumatoid Arthritis, Arthritis Care Res, doi:10.1002/acr.24850
Jousilahti, Vartiainen, Tuomilehto, Puska, Sex, Age, Cardiovascular Risk Factors, and Coronary Heart Disease, Circulation, doi:10.1161/01.CIR.99.9.1165
Kassirer, Commercialism and Medicine: An Overview, Camb. Q. Healthc. Ethics, doi:10.1017/S0963180107070478
Kaya, Nalbant, Kılıçcıo Glu, Çayır, Yaylacı et al., The prognostic significance of erythrocyte sedimentation rate in COVID-19, Rev. Assoc. Med. Bras, doi:10.1590/1806-9282.20210618
Kim, Kearns, Rosenfeld, Votapka, Casalino et al., SARS-CoV-2 evolved variants optimize binding to cellular glycocalyx, Cell Rep. Phys. Sci, doi:10.1016/j.xcrp.2023.101346
Knisely, Bloch, Eliot, Warner, Sludged, None, Blood. Science, doi:10.1126/science.106.2758.431
Koehler, Delguste, Sieben, Gillet, Alsteens, Initial Step of Virus Entry: Virion Binding to Cell-Surface Glycans, Annu. Rev. Virol, doi:10.1146/annurev-virology-122019-070025
Koren, Kohen, Ginsburg, Polyphenols enhance total oxidant-scavenging capacities of human blood by binding to red blood cells, Exp. Biol. Med, doi:10.1258/ebm.2010.009370
Krumholz, Ross, Presler, Egilman, What have we learnt from Vioxx, BMJ, doi:10.1136/bmj.39024.487720.68
Krumholz, Wu, Sawano, Shah, Zhou et al., Post-Vaccination Syndrome: A Descriptive Analysis of Reported Symptoms and Patient Experiences After COVID-19 Immunization, medRxiv, doi:10.1101/2023.11.09.23298266
Kurt, Altunceki, Contribution of Erythrocyte Sedimentation Rate to Predict Disease Severity and Outcome in COVID-19 Patients, Can. J. Infect. Dis. Med. Microbiol, doi:10.1155/2022/6510952
Lam, Reilly, Rux, Murphy, Kuri-Cervantes et al., Erythrocytes identify complement activation in patients with COVID-19, Am. J. Physiol. Lung Cell. Mol. Physiol, doi:10.1152/ajplung.00231.2021
Lapić, Rogić, Plebani, Erythrocyte sedimentation rate is associated with severe coronavirus disease 2019 (COVID-19): A pooled analysis, Clin. Chem. Lab. Med, doi:10.1515/cclm-2020-0620
Lehrer, Rheinstein, Ivermectin Docks to the SARS-CoV-2 Spike Receptor-binding Domain Attached to ACE2, Vivo, doi:10.21873/invivo.12134
Levine, Levine, Sharp, Brooks, Theory of the electrokinetic behavior of human erythrocytes, Biophys. J, doi:10.1016/S0006-3495(83)84378-1
Li, Chen, Zhao, Lung, Ye et al., Intravenous Injection of Coronavirus Disease 2019 (COVID-19) mRNA Vaccine Can Induce Acute Myopericarditis in Mouse Model, Clin. Infect. Diseases, doi:10.1093/cid/ciab707
Liu, Han, Blair, Kenst, Qin et al., SARS-CoV-2 Infects Endothelial Cells In Vivo and In Vitro, Front. Cell Infect. Microbiol, doi:10.3389/fcimb.2021.701278
Lowenstein, Solomon, Severe COVID-19 Is a Microvascular Disease, Circulation, doi:10.1161/CIRCULATIONAHA.120.050354
Lyke, Atmar, Islas, Posavad, Szydlo et al., Rapid decline in vaccine-boosted neutralizing antibodies against SARS-CoV-2 Omicron variant, Cell Rep. Med, doi:10.1016/j.xcrm.2022.100679
López-Medina, López, Hurtado, Dávalos, Ramirez et al., Effect of Ivermectin on Time to Resolution of Symptoms Among Adults with Mild COVID-19: A Randomized Clinical Trial, JAMA, doi:10.1001/jama.2021.3071
Madow, Use of antimalarial drugs as "desludging" agents in vascular disease processes: Preliminary report, JAMA, doi:10.1001/jama.1960.03020150054010
Magro, Mulvey, Berlin, Nuovo, Salvatore et al., Complement associated microvascular injury and thrombosis in the pathogenesis of severe COVID-19 infection: A report of five cases, Transl. Res, doi:10.1016/j.trsl.2020.04.007
Mahat, Panda, Rathore, Swain, Yadav et al., The dynamics of inflammatory markers in coronavirus disease-2019 (COVID-19) patients: A systematic review and meta-analysis, Clin. Epidemiol. Glob. Health, doi:10.1016/j.cegh.2021.100727
Makary, The Real Data Behind the New COVID Vaccines the White House is Pushing
Manne, Denorme, Middleton, Portier, Rowley et al., Platelet Gene Expression and Function in COVID-19 Patients, Blood, doi:10.1182/blood.2020007214
Mansanguan, Charunwatthana, Piyaphanee, Dechkhajorn, Poolcharoen et al., Cardiovascular Manifestation of the BNT162b2 mRNA COVID-19 Vaccine in Adolescents, Trop. Med. Infect. Dis, doi:10.3390/tropicalmed7080196
Mccarthy, Kory, Bigtree, War on Ivermectin: The Medicine that Saved Millions and Could Have Ended the Pandemic
Mccracken, Saginc, He, Huseynov, Daniels et al., Lack of Evidence of Angiotensin-Converting Enzyme 2 Expression and Replicative Infection by SARS-CoV-2 in Human Endothelial Cells, Circulation, doi:10.1161/CIRCULATIONAHA.120.052824
Melkumyants, Buryachkovskaya, Lomakin, Antonova, Serebruany, Mild COVID-19 and Impaired Blood Cell-Endothelial Crosstalk: Considering Long-Term Use of Antithrombotics?, Thromb. Haemost, doi:10.1055/a-1551-9911
Michel, Martin-Ventura, Red Blood Cells and Hemoglobin in Human Atherosclerosis and Related Arterial Diseases, Int. J. Mol. Sci, doi:10.3390/ijms21186756
Muhl, He, Sun, Andaloussi Mäe, Pietilä et al., The SARS-CoV-2 receptor ACE2 is expressed in mouse pericytes but not endothelial cells: Implications for COVID-19 vascular research, Stem Cell Rep, doi:10.1016/j.stemcr.2022.03.016
Munoz, Ballester, Antonijoan, Gich, Rodriguez et al., Safety and pharmacokinetic profile of fixed-dose ivermectin with an innovative 18mg tablet in healthy adult volunteers, PLoS Negl. Trop. Dis, doi:10.1371/journal.pntd.0006020
Nader, Nougier, Boisson, Poutrel, Catella et al., Increased blood viscosity and red blood cell aggregation in patients with COVID-19, Am. J. Hematol, doi:10.1002/ajh.26440
Nakahara, Iwabuchi, Miyazawa, Tonda, Shiga et al., Assessment of Myocardial (18)F-FDG Uptake at PET/CT in Asymptomatic SARS-CoV-2-vaccinated and Nonvaccinated Patients, Radiology, doi:10.1148/radiol.230743
Natali, L'abbate, Ferrannini, Erythrocyte sedimentation rate, coronary atherosclerosis, and cardiac mortality, Eur. Heart J, doi:10.1016/S0195-668X(02)00741-8
Nemkov, Reisz, Xia, Zimring, ; D'alessandro, Red blood cells as an organ? How deep omics characterization of the most abundant cell in the human body highlights other systemic metabolic functions beyond oxygen transport, Expert Rev. Proteom, doi:10.1080/14789450.2018.1531710
Neu, Bauer, Stehle, Viruses and sialic acids: Rules of engagement, Curr. Opin. Struct. Biol, doi:10.1016/j.sbi.2011.08.009
Nicosia, Ligresti, Caporarello, Akilesh, Ribatti, COVID-19 Vasculopathy: Mounting Evidence for an Indirect Mechanism of Endothelial Injury, Am. J. Pathol, doi:10.1016/j.ajpath.2021.05.007
Nie, Sahoo, Netz, Herrmann, Ballauff et al., Charge Matters: Mutations in Omicron Variant Favor Binding to Cells, ChemBioChem, doi:10.1002/cbic.202100681
Ogata, Cheng, Desjardins, Senussi, Sherman et al., Circulating Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Vaccine Antigen Detected in the Plasma of mRNA-1273 Vaccine Recipients, Clin. Infect. Dis, doi:10.1093/cid/ciab465
Okerblom, Varki, Biochemical, Cellular, Physiological, and Pathological Consequences of Human Loss of N-Glycolylneuraminic Acid, ChemBioChem, doi:10.1002/cbic.201700077
Oomen, Farkas, Roman, Van Der Beek, Luiten et al., Resveratrol preserves cerebrovascular density and cognitive function in aging mice, Front. Aging Neurosci, doi:10.3389/neuro.24.004.2009
Panigada, Bottino, Tagliabue, Grasselli, Novembrino et al., Hypercoagulability of COVID-19 patients in intensive care unit: A report of thromboelastography findings and other parameters of hemostasis, J. Thromb. Haemost, doi:10.1111/jth.14850
Parry, Lefringhausen, Turni, Neil, Cosford et al., Spikeopathy': COVID-19 Spike Protein Is Pathogenic, from Both Virus and Vaccine mRNA, Biomedicines, doi:10.3390/biomedicines11082287
Patterson, Francisco, Yogendra, Long, Pise et al., Persistence of SARS-CoV-2 S1 Protein in CD16+ Monocytes in Post-Acute Sequelae of COVID-19 (PASC) up to 15 Months Post-Infection, Front. Immunol, doi:10.3389/fimmu.2021.746021
Peacock, Brown, Zhou, Thakur, Sukhova et al., The altered entry pathway and antigenic distance of the SARS-CoV-2 Omicron variant map to separate domains of spike protein, bioRxiv, doi:10.1101/2021.12.31.474653
Powell-Wiley, Poirier, Burke, Després, Gordon-Larsen et al., Obesity and Cardiovascular Disease: A Scientific Statement From the American Heart Association, Circulation, doi:10.1161/CIR.0000000000000973
Qing, Hantak, Perlman, Gallagher, Distinct Roles for Sialoside and Protein Receptors in Coronavirus Infection, mBio, doi:10.1128/mBio.02764-19
Rabai, Detterich, Wenby, Toth, Meiselman, Effects of ethanol on red blood cell rheological behavior, Clin. Hemorheol. Microcirc, doi:10.3233/CH-2012-1632
Rauch, Labreuche, Lassalle, Goutay, Caplan et al., Coagulation biomarkers are independent predictors of increased oxygen requirements in COVID-19, J. Thromb. Haemost, doi:10.1111/jth.15067
Reis, Moreira Silva, Medeiros Silva, Thabane, Cruz Milagres et al., Effect of early treatment with metformin on risk of emergency care and hospitalization among patients with COVID-19: The TOGETHER randomized platform clinical trial, Lancet Reg. Health Am, doi:10.1016/j.lana.2021.100142
Reis, Moreira Silva, Medeiros Silva, Thabane, Milagres et al., Effect of Early Treatment with Ivermectin among Patients with COVID-19, N. Engl. J. Med, doi:10.1056/NEJMoa2115869
Reis, Moreira Silva, Medeiros Silva, Thabane, Milagres et al., Effect of early treatment with fluvoxamine on risk of emergency care and hospitalisation among patients with COVID-19: The TOGETHER randomised, platform clinical trial, Lancet Glob. Health, doi:10.1016/S2214-109X(21)00448-4
Renaud, De Lorgeril, Wine, alcohol, platelets, and the French paradox for coronary heart disease, Lancet, doi:10.1016/0140-6736(92)91277-F
Robson, Bioinformatics studies on a function of the SARS-CoV-2 spike glycoprotein as the binding of host sialic acid glycans, Comput. Biol. Med, doi:10.1016/j.compbiomed.2020.103849
Rodríguez Mega, Latin America's embrace of an unproven COVID treatment is hindering drug trials, Nature, doi:10.1038/d41586-020-02958-2
Saltelli, Dankel, Di Fiore, Holland, Pigeon, Science, the endless frontier of regulatory capture, Futures, doi:10.1016/j.futures.2021.102860
Santin, Scheim, Mccullough, Yagisawa, Borody, Ivermectin: A multifaceted drug of Nobel prize-honored distinction with indicated efficacy against a new global scourge, COVID-19, New Microbes New Infect, doi:10.1016/j.nmni.2021.100924
Saritas, Yorgun, Gokpinar, Effects of Sinovac-Coronavac and Pfizer-BioNTech mRNA vaccines on choroidal and retinal vascular system, Photodiagnosis Photodyn. Ther, doi:10.1016/j.pdpdt.2023.103702
Scheim, A Deadly Embrace: Hemagglutination Mediated by SARS-CoV-2 Spike Protein at its 22 N-Glycosylation Sites, Red Blood Cell Surface Sialoglycoproteins, and Antibody, Int. J. Mol. Sci, doi:10.3390/ijms23052558
Scheim, Aldous, Osimani, Fordham, Hoy, When Characteristics of Clinical Trials Require Per-Protocol as Well as Intention-to-Treat Outcomes to Draw Reliable Conclusions: Three Examples, J. Clin. Med, doi:10.3390/jcm12113625
Scheim, Discredit, Destroy": The targeting of doctors and scientists who reported the deadly toxicities of a painkilling drug, OSF Prepr, doi:10.31219/osf.io/bxk7d
Scheim, Hibberd, Chamie-Quintero, Protocol violations in López-Medina et al.: 38 switched ivermectin (IVM) and placebo doses, failure of blinding, ubiquitous IVM use OTC in Cali, and nearly identical AEs for the IVM and control groups, doi:10.31219/osf.io/u7ewz
Scheim, Vottero, Santin, Hirsh, Sialylated Glycan Bindings from SARS-CoV-2 Spike Protein to Blood and Endothelial Cells Govern the Severe Morbidities of COVID-19, Int. J. Mol. Sci, doi:10.3390/ijms242317039
Scholkmann, May, COVID-19, post-acute COVID-19 syndrome (PACS, "long COVID") and post-COVID-19 vaccination syndrome (PCVS, "post-COVIDvac-syndrome"): Similarities and differences, Pathol.-Res. Pract, doi:10.1016/j.prp.2023.154497
Schultheiß, Willscher, Paschold, Gottschick, Klee et al., Liquid biomarkers of macrophage dysregulation and circulating spike protein illustrate the biological heterogeneity in patients with post-acute sequelae of COVID-19, J. Med. Virol, doi:10.1002/jmv.28364
Schultze, Wahn, Klenk, Herrler, Isolated HE-protein from hemagglutinating encephalomyelitis virus and bovine coronavirus has receptor-destroying and receptor-binding activity, Virology, doi:10.1016/0042-6822(91)90026-8
Seet, Quek, Ooi, Sengupta, Lakshminarasappa et al., Positive impact of oral hydroxychloroquine and povidone-iodine throat spray for COVID-19 prophylaxis: An open-label randomized trial, Int. J. Infect. Dis, doi:10.1016/j.ijid.2021.04.035
Sender, Fuchs, Milo, Revised Estimates for the Number of Human and Bacteria Cells in the Body, PLoS Biol, doi:10.1371/journal.pbio.1002533
Shapiro, Levy, The association between hydroxychloroquine treatment and cardiovascular morbidity among rheumatoid arthritis patients, Oncotarget, doi:10.18632/oncotarget.23570
Shi, Hua, Xu, Ren, Resveratrol improves treatment outcome and laboratory parameters in patients with Takayasu arteritis: A randomized double-blind and placebo-controlled trial, Immunobiology, doi:10.1016/j.imbio.2016.10.008
Shilts, Crozier, Greenwood, Lehner, Wright, No evidence for basigin/CD147 as a direct SARS-CoV-2 spike binding receptor, Sci. Rep, doi:10.1038/s41598-020-80464-1
Shouman, Hegazy, Nafae, Ragab, Samra et al., Use of Ivermectin as a Prophylactic Option in Asymptomatic Family Close Contacts with Patients of COVID-19 (NCT number: 04422561), J. Clin. Diagn. Res
Shrestha, Burke, Nowacki, Gordon, Risk of Coronavirus Disease 2019 (COVID-19) among those up-to-date and not up-to-date on COVID-19 vaccination by US CDC criteria, PLoS ONE, doi:10.1371/journal.pone.0293449
Shrestha, Burke, Nowacki, Simon, Hagen et al., Effectiveness of the Coronavirus Disease 2019 Bivalent Vaccine, Open Forum Infect. Dis, doi:10.1093/ofid/ofad209
Singh, Satchell, Neal, Mckenzie, Tooke et al., Glomerular endothelial glycocalyx constitutes a barrier to protein permeability, J. Am. Soc. Nephrol, doi:10.1681/ASN.2007010119
Soares, Grosso, Ereño-Orbea, Coelho, Marcelo, Molecular Recognition Insights of Sialic Acid Glycans by Distinct Receptors Unveiled by NMR and Molecular Modeling, Front. Mol. Biosci, doi:10.3389/fmolb.2021.727847
Steinbrook, Kassirer, Angell, Justifying conflicts of interest in medical journals: A very bad idea, BMJ, doi:10.1136/bmj.h2942
Stencel-Baerenwald, Reiss, Reiter, Stehle, Dermody, The sweet spot: Defining virus-sialic acid interactions, Nat. Rev. Microbiol, doi:10.1038/nrmicro3346
Stone, Ndarukwa, Scheim, Dancis, Dancis et al., Changes in SpO2 on Room Air for 34 Severe COVID-19 Patients after Ivermectin-Based Combination Treatment: 62% Normalization within 24 Hours, Biologics, doi:10.3390/biologics2030015
Ströh, Stehle, Glycan Engagement by Viruses: Receptor Switches and Specificity, Annu. Rev. Virol, doi:10.1146/annurev-virology-031413-085417
Swank, Senussi, Manickas-Hill, Yu, Li et al., Persistent circulating SARS-CoV-2 spike Is associated with post-acute COVID-19 sequelae, Clin. Infect. Dis, doi:10.1093/cid/ciac722
Thairu, Babalola, Ajayi, Ndanusa, Ogedengbe et al., A comparison of Ivermectin and Non Ivermectin based regimen for COVID-19 in Abuja: Effects on virus clearance, Days-to-Discharge and Mortality, J. Pharm. Res. Int, doi:10.9734/jpri/2022/v34i44A36328
Thompson, De Vries, Paulson, Virus recognition of glycan receptors, Curr. Opin. Virol, doi:10.1016/j.coviro.2019.01.004
Thon, Italiano, Platelets: Production, Morphology and Ultrastructure, doi:10.1007/978-3-642-29423-5_1
Turpin, Catan, Meilhac, Bourdon, Canonne-Hergaux et al., Erythrocytes: Central Actors in Multiple Scenes of Atherosclerosis, Int. J. Mol. Sci, doi:10.3390/ijms22115843
Unione, Moure, Lenza, Oyenarte, Ereño-Orbea et al., The SARS-CoV-2 Spike Glycoprotein Directly Binds Exogeneous Sialic Acids: A NMR View, Angew. Chem. Int. Ed, doi:10.1002/anie.202201432
Urata, Ikeda, Yamazaki, Ueno, Katayama et al., Senescent endothelial cells are predisposed to SARS-CoV-2 infection and subsequent endothelial dysfunction, Sci. Rep, doi:10.1038/s41598-022-15976-z
Varki, Gagneux, Multifarious roles of sialic acids in immunity, Ann. N. Y. Acad. Sci, doi:10.1111/j.1749-6632.2012.06517.x
Vernon Jeffords, Knisely, Concerning the Geometric Shapes of Arteries and Arterioles: A Contribution to the Biophysics of Health, Disease, and Death, Angiology, doi:10.1177/000331975600700202
Viitala, Järnefelt, The red cell surface revisited, Trends Biochem. Sci, doi:10.1016/0968-0004(85)90067-2
Walle, Bioavailability of resveratrol, Ann. N. Y. Acad. Sci, doi:10.1111/j.1749-6632.2010.05842.x
Wang, Chen, Zhang, Deng, Lian et al., CD147-spike protein is a novel route for SARS-CoV-2 infection to host cells, Signal Transduct. Target. Ther, doi:10.1038/s41392-020-00426-x
Watanabe, Bowden, Wilson, Crispin, Exploitation of glycosylation in enveloped virus pathobiology, Biochim. Biophys. Acta (BBA)-Gen. Subj, doi:10.1016/j.bbagen.2019.05.012
Weisel, Litvinov, Red blood cells: The forgotten player in hemostasis and thrombosis, J. Thromb. Haemost, doi:10.1111/jth.14360
Wemple, Opinion: Bogus Oklahoma ivermectin story was just too good to check, Washington Post
Yagisawa, Foster, Hanaki, Omura, Global Trends in Clinical Studies of Ivermectin in COVID-19, Jpn. J. Antibiot
Yao, Li, He, Civelek, Li, Likely Common Role of Hypoxia in Driving 18F-FDG Uptake in Cancer, Myocardial Ischemia, Inflammation and Infection, Cancer Biother. Radiopharm
Yatscoff, Legatt, Keenan, Chackowsky, Blood distribution of rapamycin, Transplantation, doi:10.1097/00007890-199311000-00029
Yatscoff, Legatt, Kneteman, Therapeutic monitoring of rapamycin: A new immunosuppressive drug, Ther. Drug Monit, doi:10.1097/00007691-199312000-00004
Yonker, Swank, Bartsch, Burns, Kane et al., Circulating Spike Protein Detected in Post-COVID-19 mRNA Vaccine Myocarditis, Circulation, doi:10.1161/CIRCULATIONAHA.122.061025
Yu, Armstrong, Tripette, Meiselman, Cloutier, A local increase in red blood cell aggregation can trigger deep vein thrombosis: Evidence based on quantitative cellular ultrasound imaging, J. Thromb. Haemost, doi:10.1111/j.1538-7836.2010.04164.x
Zhao, Stockwell, Roemer, Naimi, Chikritzhs, Alcohol Consumption and Mortality From Coronary Heart Disease: An Updated Meta-Analysis of Cohort Studies, J. Stud. Alcohol. Drugs, doi:10.15288/jsad.2017.78.375
Zheng, Zhao, Li, Guo, Sheng et al., SARS-CoV-2 spike protein causes blood coagulation and thrombosis by competitive binding to heparan sulfate, Int. J. Biol. Macromol, doi:10.1016/j.ijbiomac.2021.10.112
Østergaard, SARS-CoV-2 related microvascular damage and symptoms during and after COVID-19: Consequences of capillary transit-time changes, tissue hypoxia and inflammation, Physiol. Rep, doi:10.14814/phy2.14726
DOI record:
{
"DOI": "10.3390/v16040647",
"ISSN": [
"1999-4915"
],
"URL": "http://dx.doi.org/10.3390/v16040647",
"abstract": "<jats:p>Consistent with the biochemistry of coronaviruses as well established over decades, SARS-CoV-2 makes its initial attachment to host cells through the binding of its spike protein (SP) to sialylated glycans (containing the monosaccharide sialic acid) on the cell surface. The virus can then slide over and enter via ACE2. SARS-CoV-2 SP attaches particularly tightly to the trillions of red blood cells (RBCs), platelets and endothelial cells in the human body, each cell very densely coated with sialic acid surface molecules but having no ACE2 or minimal ACE2. These interlaced attachments trigger the blood cell aggregation, microvascular occlusion and vascular damage that underlie the hypoxia, blood clotting and related morbidities of severe COVID-19. Notably, the two human betacoronaviruses that express a sialic acid-cleaving enzyme are benign, while the other three—SARS, SARS-CoV-2 and MERS—are virulent. RBC aggregation experimentally induced in several animal species using an injected polysaccharide caused most of the same morbidities of severe COVID-19. This glycan biochemistry is key to disentangling controversies that have arisen over the efficacy of certain generic COVID-19 treatment agents and the safety of SP-based COVID-19 vaccines. More broadly, disregard for the active physiological role of RBCs yields unreliable or erroneous reporting of pharmacokinetic parameters as routinely obtained for most drugs and other bioactive agents using detection in plasma, with whole-blood levels being up to 30-fold higher. Appreciation of the active role of RBCs can elucidate the microvascular underpinnings of other health conditions, including cardiovascular disease, and therapeutic opportunities to address them.</jats:p>",
"alternative-id": [
"v16040647"
],
"author": [
{
"ORCID": "http://orcid.org/0000-0001-6841-7054",
"affiliation": [
{
"name": "US Public Health Service, Commissioned Corps, Inactive Reserve, Blacksburg, VA 24060, USA"
}
],
"authenticated-orcid": false,
"family": "Scheim",
"given": "David E.",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0003-1086-0138",
"affiliation": [
{
"name": "Children’s Health Research Clinical Unit, Faculty of Medicine, The University of Queensland, South Brisbane, QLD 4101, Australia"
},
{
"name": "Department of Psychiatry, Flinders University, Bedford Park, SA 5042, Australia"
}
],
"authenticated-orcid": false,
"family": "Parry",
"given": "Peter I.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Kolling Institute, Faculty of Medicine and Health, The University of Sydney, St Leonards, NSW 2064, Australia"
}
],
"family": "Rabbolini",
"given": "David J.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "College of Health Sciences, University of KwaZulu-Natal, Durban 4041, South Africa"
}
],
"family": "Aldous",
"given": "Colleen",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0009-0009-9427-1947",
"affiliation": [
{
"name": "Satoshi Omura Memorial Research Institute, Kitasato University, Tokyo 108-8641, Japan"
},
{
"name": "Louis Pasteur Center for Medical Research, Kyoto 606-8225, Japan"
}
],
"authenticated-orcid": false,
"family": "Yagisawa",
"given": "Morimasa",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Emeritus Professor, School of Medicine and Public Health, University of Newcastle, Newcastle, NE1 7RU, Australia"
}
],
"family": "Clancy",
"given": "Robert",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-0519-4698",
"affiliation": [
{
"name": "Centre for Digestive Diseases, Five Dock, NSW 2046, Australia"
}
],
"authenticated-orcid": false,
"family": "Borody",
"given": "Thomas J.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Emeritus Professor of Medicine, University of Queensland, Herston, QLD 4029, Australia"
}
],
"family": "Hoy",
"given": "Wendy E.",
"sequence": "additional"
}
],
"container-title": "Viruses",
"container-title-short": "Viruses",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2024,
4,
22
]
],
"date-time": "2024-04-22T13:53:52Z",
"timestamp": 1713794032000
},
"deposited": {
"date-parts": [
[
2024,
4,
22
]
],
"date-time": "2024-04-22T14:05:13Z",
"timestamp": 1713794713000
},
"indexed": {
"date-parts": [
[
2024,
4,
23
]
],
"date-time": "2024-04-23T00:37:09Z",
"timestamp": 1713832629606
},
"is-referenced-by-count": 0,
"issue": "4",
"issued": {
"date-parts": [
[
2024,
4,
22
]
]
},
"journal-issue": {
"issue": "4",
"published-online": {
"date-parts": [
[
2024,
4
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2024,
4,
22
]
],
"date-time": "2024-04-22T00:00:00Z",
"timestamp": 1713744000000
}
}
],
"link": [
{
"URL": "https://www.mdpi.com/1999-4915/16/4/647/pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1968",
"original-title": [],
"page": "647",
"prefix": "10.3390",
"published": {
"date-parts": [
[
2024,
4,
22
]
]
},
"published-online": {
"date-parts": [
[
2024,
4,
22
]
]
},
"publisher": "MDPI AG",
"reference": [
{
"DOI": "10.3390/ijms242317039",
"doi-asserted-by": "crossref",
"key": "ref_1",
"unstructured": "Scheim, D.E., Vottero, P., Santin, A.D., and Hirsh, A.G. (2023). Sialylated Glycan Bindings from SARS-CoV-2 Spike Protein to Blood and Endothelial Cells Govern the Severe Morbidities of COVID-19. Int. J. Mol. Sci., 24."
},
{
"DOI": "10.3390/biomedicines11082287",
"doi-asserted-by": "crossref",
"key": "ref_2",
"unstructured": "Parry, P.I., Lefringhausen, A., Turni, C., Neil, C.J., Cosford, R., Hudson, N.J., and Gillespie, J. (2023). ‘Spikeopathy’: COVID-19 Spike Protein Is Pathogenic, from Both Virus and Vaccine mRNA. Biomedicines, 11."
},
{
"DOI": "10.1016/j.compbiomed.2020.103849",
"doi-asserted-by": "crossref",
"key": "ref_3",
"unstructured": "Robson, B. (2020). Bioinformatics studies on a function of the SARS-CoV-2 spike glycoprotein as the binding of host sialic acid glycans. Comput. Biol. Med., 122."
},
{
"DOI": "10.3390/ijms23052558",
"doi-asserted-by": "crossref",
"key": "ref_4",
"unstructured": "Scheim, D.E. (2022). A Deadly Embrace: Hemagglutination Mediated by SARS-CoV-2 Spike Protein at its 22 N-Glycosylation Sites, Red Blood Cell Surface Sialoglycoproteins, and Antibody. Int. J. Mol. Sci., 23."
},
{
"DOI": "10.1016/j.prp.2023.154497",
"article-title": "COVID-19, post-acute COVID-19 syndrome (PACS, “long COVID”) and post-COVID-19 vaccination syndrome (PCVS, “post-COVIDvac-syndrome”): Similarities and differences",
"author": "Scholkmann",
"doi-asserted-by": "crossref",
"first-page": "154497",
"journal-title": "Pathol.—Res. Pract.",
"key": "ref_5",
"volume": "246",
"year": "2023"
},
{
"DOI": "10.1016/j.sbi.2011.08.009",
"article-title": "Viruses and sialic acids: Rules of engagement",
"author": "Neu",
"doi-asserted-by": "crossref",
"first-page": "610",
"journal-title": "Curr. Opin. Struct. Biol.",
"key": "ref_6",
"volume": "21",
"year": "2011"
},
{
"DOI": "10.1111/j.1749-6632.2012.06517.x",
"article-title": "Multifarious roles of sialic acids in immunity",
"author": "Varki",
"doi-asserted-by": "crossref",
"first-page": "16",
"journal-title": "Ann. N. Y. Acad. Sci.",
"key": "ref_7",
"volume": "1253",
"year": "2012"
},
{
"DOI": "10.1002/cbic.201700077",
"article-title": "Biochemical, Cellular, Physiological, and Pathological Consequences of Human Loss of N-Glycolylneuraminic Acid",
"author": "Okerblom",
"doi-asserted-by": "crossref",
"first-page": "1155",
"journal-title": "ChemBioChem",
"key": "ref_8",
"volume": "18",
"year": "2017"
},
{
"DOI": "10.3390/app10114053",
"doi-asserted-by": "crossref",
"key": "ref_9",
"unstructured": "Cosic, I., Cosic, D., and Loncarevic, I. (2020). RRM Prediction of Erythrocyte Band3 Protein as Alternative Receptor for SARS-CoV-2 Virus. Appl. Sci., 10."
},
{
"DOI": "10.1182/blood.2020007214",
"article-title": "Platelet Gene Expression and Function in COVID-19 Patients",
"author": "Manne",
"doi-asserted-by": "crossref",
"first-page": "1317",
"journal-title": "Blood",
"key": "ref_10",
"volume": "136",
"year": "2020"
},
{
"DOI": "10.1111/jth.15156",
"article-title": "Is there a role for the ACE2 receptor in SARS-CoV-2 interactions with platelets?",
"author": "Campbell",
"doi-asserted-by": "crossref",
"first-page": "46",
"journal-title": "J. Thromb. Haemost.",
"key": "ref_11",
"volume": "19",
"year": "2021"
},
{
"DOI": "10.1016/j.jacbts.2020.09.010",
"article-title": "Cardiorenal Tissues Express SARS-CoV-2 Entry Genes and Basigin (BSG/CD147) Increases with Age in Endothelial Cells",
"author": "Vaja",
"doi-asserted-by": "crossref",
"first-page": "1111",
"journal-title": "JACC Basic Transl. Sci.",
"key": "ref_12",
"volume": "5",
"year": "2020"
},
{
"DOI": "10.1101/2020.05.29.123513",
"doi-asserted-by": "crossref",
"key": "ref_13",
"unstructured": "Ganier, C., Du-Harpur, X., Harun, N., Wan, B., Arthurs, C., Luscombe, N., Watt, F., and Lynch, M. (2020). CD147 (BSG) but not ACE2 expression is detectable in vascular endothelial cells within single cell RNA sequencing datasets derived from multiple tissues in healthy individuals. bioRxiv."
},
{
"DOI": "10.1161/CIRCULATIONAHA.120.052824",
"article-title": "Lack of Evidence of Angiotensin-Converting Enzyme 2 Expression and Replicative Infection by SARS-CoV-2 in Human Endothelial Cells",
"author": "McCracken",
"doi-asserted-by": "crossref",
"first-page": "865",
"journal-title": "Circulation",
"key": "ref_14",
"volume": "143",
"year": "2021"
},
{
"DOI": "10.1016/j.stemcr.2022.03.016",
"article-title": "The SARS-CoV-2 receptor ACE2 is expressed in mouse pericytes but not endothelial cells: Implications for COVID-19 vascular research",
"author": "Muhl",
"doi-asserted-by": "crossref",
"first-page": "1089",
"journal-title": "Stem Cell Rep.",
"key": "ref_15",
"volume": "17",
"year": "2022"
},
{
"DOI": "10.1038/s41598-022-15976-z",
"article-title": "Senescent endothelial cells are predisposed to SARS-CoV-2 infection and subsequent endothelial dysfunction",
"author": "Urata",
"doi-asserted-by": "crossref",
"first-page": "11855",
"journal-title": "Sci. Rep.",
"key": "ref_16",
"volume": "12",
"year": "2022"
},
{
"DOI": "10.1016/j.ajpath.2021.05.007",
"article-title": "COVID-19 Vasculopathy: Mounting Evidence for an Indirect Mechanism of Endothelial Injury",
"author": "Nicosia",
"doi-asserted-by": "crossref",
"first-page": "1374",
"journal-title": "Am. J. Pathol.",
"key": "ref_17",
"volume": "191",
"year": "2021"
},
{
"DOI": "10.3389/fcimb.2021.701278",
"doi-asserted-by": "crossref",
"key": "ref_18",
"unstructured": "Liu, F., Han, K., Blair, R., Kenst, K., Qin, Z., Upcin, B., Wörsdörfer, P., Midkiff, C.C., Mudd, J., and Belyaeva, E. (2021). SARS-CoV-2 Infects Endothelial Cells In Vivo and In Vitro. Front. Cell Infect. Microbiol., 11."
},
{
"article-title": "Unusually high concentrations of sialic acids on the surface of vascular endothelia",
"author": "Born",
"first-page": "543",
"journal-title": "Br. J. Exp. Pathol.",
"key": "ref_19",
"volume": "66",
"year": "1985"
},
{
"DOI": "10.1111/j.1538-7836.2010.04164.x",
"article-title": "A local increase in red blood cell aggregation can trigger deep vein thrombosis: Evidence based on quantitative cellular ultrasound imaging",
"author": "Yu",
"doi-asserted-by": "crossref",
"first-page": "481",
"journal-title": "J. Thromb. Haemost.",
"key": "ref_20",
"volume": "9",
"year": "2011"
},
{
"DOI": "10.1111/jth.14360",
"article-title": "Red blood cells: The forgotten player in hemostasis and thrombosis",
"author": "Weisel",
"doi-asserted-by": "crossref",
"first-page": "271",
"journal-title": "J. Thromb. Haemost.",
"key": "ref_21",
"volume": "17",
"year": "2019"
},
{
"DOI": "10.1182/blood-2017-03-745349",
"article-title": "Red blood cells in thrombosis",
"author": "Byrnes",
"doi-asserted-by": "crossref",
"first-page": "1795",
"journal-title": "Blood",
"key": "ref_22",
"volume": "130",
"year": "2017"
},
{
"DOI": "10.1002/ajh.26440",
"article-title": "Increased blood viscosity and red blood cell aggregation in patients with COVID-19",
"author": "Nader",
"doi-asserted-by": "crossref",
"first-page": "283",
"journal-title": "Am. J. Hematol.",
"key": "ref_23",
"volume": "97",
"year": "2022"
},
{
"DOI": "10.1016/bs.aivir.2016.08.004",
"article-title": "Chapter Two—Coronavirus Spike Protein and Tropism Changes",
"author": "Ziebuhr",
"doi-asserted-by": "crossref",
"first-page": "29",
"journal-title": "Advances in Virus Research",
"key": "ref_24",
"volume": "Volume 96",
"year": "2016"
},
{
"DOI": "10.1146/annurev-virology-122019-070025",
"article-title": "Initial Step of Virus Entry: Virion Binding to Cell-Surface Glycans",
"author": "Koehler",
"doi-asserted-by": "crossref",
"first-page": "143",
"journal-title": "Annu. Rev. Virol.",
"key": "ref_25",
"volume": "7",
"year": "2020"
},
{
"DOI": "10.1128/mBio.02764-19",
"article-title": "Distinct Roles for Sialoside and Protein Receptors in Coronavirus Infection",
"author": "Qing",
"doi-asserted-by": "crossref",
"first-page": "e02764-19",
"journal-title": "mBio",
"key": "ref_26",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.1146/annurev-virology-031413-085417",
"article-title": "Glycan Engagement by Viruses: Receptor Switches and Specificity",
"author": "Stehle",
"doi-asserted-by": "crossref",
"first-page": "285",
"journal-title": "Annu. Rev. Virol.",
"key": "ref_27",
"volume": "1",
"year": "2014"
},
{
"DOI": "10.1093/glycob/9.8.747",
"article-title": "Evolutionary considerations in relating oligosaccharide diversity to biological function",
"author": "Gagneux",
"doi-asserted-by": "crossref",
"first-page": "747",
"journal-title": "Glycobiology",
"key": "ref_28",
"volume": "9",
"year": "1999"
},
{
"DOI": "10.1021/acscentsci.0c00855",
"article-title": "The SARS-CoV-2 Spike Protein Binds Sialic Acids and Enables Rapid Detection in a Lateral Flow Point of Care Diagnostic Device",
"author": "Baker",
"doi-asserted-by": "crossref",
"first-page": "2046",
"journal-title": "ACS Cent. Sci.",
"key": "ref_29",
"volume": "6",
"year": "2020"
},
{
"DOI": "10.1002/anie.202201432",
"article-title": "The SARS-CoV-2 Spike Glycoprotein Directly Binds Exogeneous Sialic Acids: A NMR View",
"author": "Unione",
"doi-asserted-by": "crossref",
"first-page": "e202201432",
"journal-title": "Angew. Chem. Int. Ed.",
"key": "ref_30",
"volume": "61",
"year": "2022"
},
{
"DOI": "10.1038/s41392-020-00426-x",
"article-title": "CD147-spike protein is a novel route for SARS-CoV-2 infection to host cells",
"author": "Wang",
"doi-asserted-by": "crossref",
"first-page": "283",
"journal-title": "Signal Transduct. Target. Ther.",
"key": "ref_31",
"volume": "5",
"year": "2020"
},
{
"DOI": "10.1126/scitranslmed.abj7790",
"article-title": "Lung epithelial and endothelial damage, loss of tissue repair, inhibition of fibrinolysis, and cellular senescence in fatal COVID-19",
"author": "Walters",
"doi-asserted-by": "crossref",
"first-page": "eabj7790",
"journal-title": "Sci. Transl. Med.",
"key": "ref_32",
"volume": "13",
"year": "2021"
},
{
"article-title": "SARS-CoV-2 related microvascular damage and symptoms during and after COVID-19: Consequences of capillary transit-time changes, tissue hypoxia and inflammation",
"first-page": "e14726",
"journal-title": "Physiol. Rep.",
"key": "ref_33",
"volume": "9",
"year": "2021"
},
{
"DOI": "10.1080/14789450.2018.1531710",
"article-title": "Red blood cells as an organ? How deep omics characterization of the most abundant cell in the human body highlights other systemic metabolic functions beyond oxygen transport",
"author": "Nemkov",
"doi-asserted-by": "crossref",
"first-page": "855",
"journal-title": "Expert Rev. Proteom.",
"key": "ref_34",
"volume": "15",
"year": "2018"
},
{
"DOI": "10.1101/036103",
"doi-asserted-by": "crossref",
"key": "ref_35",
"unstructured": "Sender, R., Fuchs, S., and Milo, R. (2016). Revised Estimates for the Number of Human and Bacteria Cells in the Body. PLoS Biol., 14."
},
{
"article-title": "Blood platelets",
"author": "Hilton",
"first-page": "59",
"journal-title": "Sci. Prog.",
"key": "ref_36",
"volume": "66",
"year": "1979"
},
{
"DOI": "10.1016/0968-0004(85)90067-2",
"article-title": "The red cell surface revisited",
"author": "Viitala",
"doi-asserted-by": "crossref",
"first-page": "392",
"journal-title": "Trends Biochem. Sci.",
"key": "ref_37",
"volume": "10",
"year": "1985"
},
{
"DOI": "10.1093/oxfordjournals.molbev.a004075",
"article-title": "Natural selection on the erythrocyte surface",
"author": "Baum",
"doi-asserted-by": "crossref",
"first-page": "223",
"journal-title": "Mol. Biol. Evol.",
"key": "ref_38",
"volume": "19",
"year": "2002"
},
{
"DOI": "10.1101/2022.11.24.517882",
"doi-asserted-by": "crossref",
"key": "ref_39",
"unstructured": "Boschi, C., Scheim, D.E., Bancod, A., Militello, M., Bideau, M.L., Colson, P., Fantini, J., and Scola, B.L. (2022). SARS-CoV-2 Spike Protein Induces Hemagglutination: Implications for COVID-19 Morbidities and Therapeutics and for Vaccine Adverse Effects. Int. J. Mol. Sci., 23."
},
{
"DOI": "10.1152/ajplung.00231.2021",
"article-title": "Erythrocytes identify complement activation in patients with COVID-19",
"author": "Lam",
"doi-asserted-by": "crossref",
"first-page": "L485",
"journal-title": "Am. J. Physiol. Lung Cell. Mol. Physiol.",
"key": "ref_40",
"volume": "321",
"year": "2021"
},
{
"DOI": "10.1016/j.ijbiomac.2021.10.112",
"article-title": "SARS-CoV-2 spike protein causes blood coagulation and thrombosis by competitive binding to heparan sulfate",
"author": "Zheng",
"doi-asserted-by": "crossref",
"first-page": "1124",
"journal-title": "Int. J. Biol. Macromol.",
"key": "ref_41",
"volume": "193",
"year": "2021"
},
{
"DOI": "10.1016/j.scib.2021.01.010",
"article-title": "Binding of the SARS-CoV-2 spike protein to glycans",
"author": "Hao",
"doi-asserted-by": "crossref",
"first-page": "1205",
"journal-title": "Sci. Bull.",
"key": "ref_42",
"volume": "66",
"year": "2021"
},
{
"DOI": "10.1038/s41598-020-80464-1",
"article-title": "No evidence for basigin/CD147 as a direct SARS-CoV-2 spike binding receptor",
"author": "Shilts",
"doi-asserted-by": "crossref",
"first-page": "413",
"journal-title": "Sci. Rep.",
"key": "ref_43",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.1161/CIRCULATIONAHA.120.050354",
"article-title": "Severe COVID-19 Is a Microvascular Disease",
"author": "Lowenstein",
"doi-asserted-by": "crossref",
"first-page": "1609",
"journal-title": "Circulation",
"key": "ref_44",
"volume": "142",
"year": "2020"
},
{
"DOI": "10.1016/j.trsl.2020.04.007",
"article-title": "Complement associated microvascular injury and thrombosis in the pathogenesis of severe COVID-19 infection: A report of five cases",
"author": "Magro",
"doi-asserted-by": "crossref",
"first-page": "1",
"journal-title": "Transl. Res.",
"key": "ref_45",
"volume": "220",
"year": "2020"
},
{
"DOI": "10.20944/preprints202007.0142.v1",
"doi-asserted-by": "crossref",
"key": "ref_46",
"unstructured": "Grobler, C., Maphumulo, S.C., Grobbelaar, L.M., Bredenkamp, J.C., Laubscher, G.J., Lourens, P.J., Steenkamp, J., Kell, D.B., and Pretorius, E. (2020). COVID-19: The Rollercoaster of Fibrin(Ogen), D-Dimer, Von Willebrand Factor, P-Selectin and Their Interactions with Endothelial Cells, Platelets and Erythrocytes. Int. J. Mol. Sci., 21."
},
{
"DOI": "10.1055/a-1551-9911",
"article-title": "Mild COVID-19 and Impaired Blood Cell–Endothelial Crosstalk: Considering Long-Term Use of Antithrombotics?",
"author": "Melkumyants",
"doi-asserted-by": "crossref",
"first-page": "123",
"journal-title": "Thromb. Haemost.",
"key": "ref_47",
"volume": "122",
"year": "2022"
},
{
"article-title": "Red blood cell morphology in patients with COVID-19-related anaemia",
"author": "Berzuini",
"first-page": "34",
"journal-title": "Blood Transfus.",
"key": "ref_48",
"volume": "19",
"year": "2021"
},
{
"DOI": "10.1097/CCM.0000000000004862",
"article-title": "Capillary Leukocytes, Microaggregates, and the Response to Hypoxemia in the Microcirculation of Coronavirus Disease 2019 Patients",
"author": "Favaron",
"doi-asserted-by": "crossref",
"first-page": "661",
"journal-title": "Crit. Care Med.",
"key": "ref_49",
"volume": "49",
"year": "2021"
},
{
"DOI": "10.1016/j.cegh.2021.100727",
"article-title": "The dynamics of inflammatory markers in coronavirus disease-2019 (COVID-19) patients: A systematic review and meta-analysis",
"author": "Mahat",
"doi-asserted-by": "crossref",
"first-page": "100727",
"journal-title": "Clin. Epidemiol. Glob. Health",
"key": "ref_50",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.1590/1806-9282.20210618",
"article-title": "The prognostic significance of erythrocyte sedimentation rate in COVID-19",
"author": "Kaya",
"doi-asserted-by": "crossref",
"first-page": "1305",
"journal-title": "Rev. Assoc. Med. Bras.",
"key": "ref_51",
"volume": "67",
"year": "2021"
},
{
"DOI": "10.1515/cclm-2020-0620",
"article-title": "Erythrocyte sedimentation rate is associated with severe coronavirus disease 2019 (COVID-19): A pooled analysis",
"author": "Plebani",
"doi-asserted-by": "crossref",
"first-page": "1146",
"journal-title": "Clin. Chem. Lab. Med.",
"key": "ref_52",
"volume": "58",
"year": "2020"
},
{
"DOI": "10.1155/2022/6510952",
"doi-asserted-by": "crossref",
"key": "ref_53",
"unstructured": "Kurt, C., and Altunceki, C.Y.A. (2022). Contribution of Erythrocyte Sedimentation Rate to Predict Disease Severity and Outcome in COVID-19 Patients. Can. J. Infect. Dis. Med. Microbiol., 2022."
},
{
"DOI": "10.1186/s43066-021-00144-1",
"article-title": "Long-term clinical and biochemical residue after COVID-19 recovery",
"author": "Gameil",
"doi-asserted-by": "crossref",
"first-page": "74",
"journal-title": "Egypt. Liver J.",
"key": "ref_54",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.1186/s40001-020-00432-3",
"article-title": "Laboratory features of severe vs. non-severe COVID-19 patients in Asian populations: A systematic review and meta-analysis",
"author": "Ghahramani",
"doi-asserted-by": "crossref",
"first-page": "30",
"journal-title": "Eur. J. Med. Res.",
"key": "ref_55",
"volume": "25",
"year": "2020"
},
{
"DOI": "10.1007/s00134-020-06062-x",
"article-title": "High risk of thrombosis in patients with severe SARS-CoV-2 infection: A multicenter prospective cohort study",
"author": "Helms",
"doi-asserted-by": "crossref",
"first-page": "1089",
"journal-title": "Intensive Care Med.",
"key": "ref_56",
"volume": "46",
"year": "2020"
},
{
"DOI": "10.1111/jth.14850",
"article-title": "Hypercoagulability of COVID-19 patients in intensive care unit: A report of thromboelastography findings and other parameters of hemostasis",
"author": "Panigada",
"doi-asserted-by": "crossref",
"first-page": "1738",
"journal-title": "J. Thromb. Haemost.",
"key": "ref_57",
"volume": "18",
"year": "2020"
},
{
"DOI": "10.1016/j.gore.2024.101324",
"article-title": "Increased von Willebrand and Factor VIII plasma levels in gynecologic patients with Post-Acute-COVID-Sequela (PASC)/Long COVID",
"author": "Bellone",
"doi-asserted-by": "crossref",
"first-page": "101324",
"journal-title": "Gynecol. Oncol. Rep.",
"key": "ref_58",
"volume": "51",
"year": "2024"
},
{
"DOI": "10.1161/01.CIR.14.3.386",
"article-title": "Angioscopic Changes in the Smaller Blood Vessels in Diabetes Mellitus and their Relationship to Aging",
"author": "Ditzel",
"doi-asserted-by": "crossref",
"first-page": "386",
"journal-title": "Circulation",
"key": "ref_59",
"volume": "14",
"year": "1956"
},
{
"DOI": "10.1111/j.1549-8719.2011.00130.x",
"article-title": "Microvascular Dysfunction: A Potential Mechanism in the Pathogenesis of Obesity-associated Insulin Resistance and Hypertension",
"author": "Meijer",
"doi-asserted-by": "crossref",
"first-page": "5",
"journal-title": "Microcirculation",
"key": "ref_60",
"volume": "19",
"year": "2012"
},
{
"key": "ref_61",
"unstructured": "Bicher, H.I. (1972). Blood Cell Aggregation in Thrombotic Processes, C. C. Thomas. Chapter I: Red cell aggregation in thrombotic disease, trauma and shock."
},
{
"DOI": "10.1177/000331975600700202",
"article-title": "Concerning the Geometric Shapes of Arteries and Arterioles: A Contribution to the Biophysics of Health, Disease, and Death",
"author": "Knisely",
"doi-asserted-by": "crossref",
"first-page": "105",
"journal-title": "Angiology",
"key": "ref_62",
"volume": "7",
"year": "1956"
},
{
"DOI": "10.1093/cid/ciab707",
"article-title": "Intravenous Injection of Coronavirus Disease 2019 (COVID-19) mRNA Vaccine Can Induce Acute Myopericarditis in Mouse Model",
"author": "Li",
"doi-asserted-by": "crossref",
"first-page": "1933",
"journal-title": "Clin. Infect. Diseases",
"key": "ref_63",
"volume": "74",
"year": "2022"
},
{
"article-title": "COVID 19 m-RNA (Pfizer) vaccination impairs cardiac functions in adult male rats",
"author": "Hassan",
"first-page": "211",
"journal-title": "Bull. Egypt. Soc. Physiol. Sci.",
"key": "ref_64",
"volume": "43",
"year": "2023"
},
{
"DOI": "10.1016/j.pdpdt.2022.102742",
"article-title": "The assesment of retina and optic disc vascular structures in people who received CoronaVac vaccine",
"author": "Gedik",
"doi-asserted-by": "crossref",
"first-page": "102742",
"journal-title": "Photodiagnosis Photodyn. Ther.",
"key": "ref_65",
"volume": "38",
"year": "2022"
},
{
"DOI": "10.1016/j.pdpdt.2023.103702",
"article-title": "Effects of Sinovac-Coronavac and Pfizer-BioNTech mRNA vaccines on choroidal and retinal vascular system",
"author": "Saritas",
"doi-asserted-by": "crossref",
"first-page": "103702",
"journal-title": "Photodiagnosis Photodyn. Ther.",
"key": "ref_66",
"volume": "43",
"year": "2023"
},
{
"DOI": "10.1016/j.mvr.2023.104500",
"article-title": "Evaluation of retinal and optic disc vascular structures in individuals before and after Pfizer-BioNTech vaccination",
"author": "Gedik",
"doi-asserted-by": "crossref",
"first-page": "104500",
"journal-title": "Microvasc. Res.",
"key": "ref_67",
"volume": "147",
"year": "2023"
},
{
"DOI": "10.3390/jcm9072279",
"doi-asserted-by": "crossref",
"key": "ref_68",
"unstructured": "Haider, A., Bengs, S., Schade, K., Wijnen, W.J., Portmann, A., Etter, D., Fröhlich, S., Warnock, G.I., Treyer, V., and Burger, I.A. (2020). Myocardial 18F-FDG Uptake Pattern for Cardiovascular Risk Stratification in Patients Undergoing Oncologic PET/CT. J. Clin. Med., 9."
},
{
"article-title": "Likely Common Role of Hypoxia in Driving 18F-FDG Uptake in Cancer, Myocardial Ischemia, Inflammation and Infection",
"author": "Yao",
"first-page": "624",
"journal-title": "Cancer Biother. Radiopharm.",
"key": "ref_69",
"volume": "36",
"year": "2021"
},
{
"DOI": "10.1148/radiol.230743",
"article-title": "Assessment of Myocardial (18)F-FDG Uptake at PET/CT in Asymptomatic SARS-CoV-2-vaccinated and Nonvaccinated Patients",
"author": "Nakahara",
"doi-asserted-by": "crossref",
"first-page": "e230743",
"journal-title": "Radiology",
"key": "ref_70",
"volume": "308",
"year": "2023"
},
{
"DOI": "10.1161/circ.144.suppl_1.10712",
"article-title": "Abstract 10712: Observational Findings of PULS Cardiac Test Findings for Inflammatory Markers in Patients Receiving mRNA Vaccines",
"author": "Gundry",
"doi-asserted-by": "crossref",
"first-page": "A10712",
"journal-title": "Circulation",
"key": "ref_71",
"volume": "144",
"year": "2021"
},
{
"DOI": "10.1002/prca.202300048",
"article-title": "Detection of recombinant Spike protein in the blood of individuals vaccinated against SARS-CoV-2: Possible molecular mechanisms",
"author": "Brogna",
"doi-asserted-by": "crossref",
"first-page": "e2300048",
"journal-title": "PROTEOMICS—Clin. Appl.",
"key": "ref_72",
"volume": "17",
"year": "2023"
},
{
"DOI": "10.1161/CIRCULATIONAHA.122.061025",
"article-title": "Circulating Spike Protein Detected in Post–COVID-19 mRNA Vaccine Myocarditis",
"author": "Yonker",
"doi-asserted-by": "crossref",
"first-page": "867",
"journal-title": "Circulation",
"key": "ref_73",
"volume": "147",
"year": "2023"
},
{
"DOI": "10.1016/j.vaccine.2024.01.100",
"article-title": "COVID-19 vaccines and adverse events of special interest: A multinational Global Vaccine Data Network (GVDN) cohort study of 99 million vaccinated individuals",
"author": "Faksova",
"doi-asserted-by": "crossref",
"first-page": "2200",
"journal-title": "Vaccine",
"key": "ref_74",
"volume": "42",
"year": "2024"
},
{
"DOI": "10.1101/2023.11.09.23298266",
"doi-asserted-by": "crossref",
"key": "ref_75",
"unstructured": "Krumholz, H.M., Wu, Y., Sawano, M., Shah, R., Zhou, T., Arun, A.S., Khosla, P., Kaleem, S., Anushree, V., and Bornali, B. (2023). Post-Vaccination Syndrome: A Descriptive Analysis of Reported Symptoms and Patient Experiences After COVID-19 Immunization. medRxiv."
},
{
"DOI": "10.1007/s00431-022-04786-0",
"article-title": "Changes of ECG parameters after BNT162b2 vaccine in the senior high school students",
"author": "Chiu",
"doi-asserted-by": "crossref",
"first-page": "1155",
"journal-title": "Eur. J. Pediatr.",
"key": "ref_76",
"volume": "182",
"year": "2023"
},
{
"DOI": "10.20944/preprints202208.0151.v1",
"doi-asserted-by": "crossref",
"key": "ref_77",
"unstructured": "Mansanguan, S., Charunwatthana, P., Piyaphanee, W., Dechkhajorn, W., Poolcharoen, A., and Mansanguan, C. (2022). Cardiovascular Manifestation of the BNT162b2 mRNA COVID-19 Vaccine in Adolescents. Trop. Med. Infect. Dis., 7."
},
{
"DOI": "10.2174/138920112800399095",
"article-title": "History of avermectin and ivermectin, with notes on the history of other macrocyclic lactone antiparasitic agents",
"author": "Campbell",
"doi-asserted-by": "crossref",
"first-page": "853",
"journal-title": "Curr. Pharm. Biotechnol.",
"key": "ref_78",
"volume": "13",
"year": "2012"
},
{
"article-title": "Global Trends in Clinical Studies of Ivermectin in COVID-19",
"author": "Yagisawa",
"first-page": "44",
"journal-title": "Jpn. J. Antibiot.",
"key": "ref_79",
"volume": "74",
"year": "2021"
},
{
"DOI": "10.1038/s41598-024-53086-0",
"article-title": "Binding behavior of receptor binding domain of the SARS-CoV-2 virus and ivermectin",
"author": "Gossen",
"doi-asserted-by": "crossref",
"first-page": "2743",
"journal-title": "Sci. Rep.",
"key": "ref_80",
"volume": "14",
"year": "2024"
},
{
"DOI": "10.3390/computation10040051",
"doi-asserted-by": "crossref",
"key": "ref_81",
"unstructured": "Aminpour, M., Cannariato, M., Safaeeardebili, M.E., Preto, J., Moracchiato, A., Doria, D., Donato, F., Zizzi, E.A., Deriu, M.A., and Scheim, D.E. (2022). In Silico Analysis of the Multi-Targeted Mode of Action of Ivermectin and Related Compounds. Computation, 10."
},
{
"DOI": "10.21873/invivo.12134",
"article-title": "Ivermectin Docks to the SARS-CoV-2 Spike Receptor-binding Domain Attached to ACE2",
"author": "Lehrer",
"doi-asserted-by": "crossref",
"first-page": "3023",
"journal-title": "In Vivo",
"key": "ref_82",
"volume": "34",
"year": "2020"
},
{
"DOI": "10.3390/biologics2030015",
"article-title": "Changes in SpO2 on Room Air for 34 Severe COVID-19 Patients after Ivermectin-Based Combination Treatment: 62% Normalization within 24 Hours",
"author": "Stone",
"doi-asserted-by": "crossref",
"first-page": "196",
"journal-title": "Biologics",
"key": "ref_83",
"volume": "2",
"year": "2022"
},
{
"DOI": "10.9734/jpri/2022/v34i44A36328",
"article-title": "A comparison of Ivermectin and Non Ivermectin based regimen for COVID-19 in Abuja: Effects on virus clearance, Days-to-Discharge and Mortality",
"author": "Thairu",
"doi-asserted-by": "crossref",
"first-page": "1",
"journal-title": "J. Pharm. Res. Int.",
"key": "ref_84",
"volume": "34",
"year": "2022"
},
{
"key": "ref_85",
"unstructured": "Babalola, O.E. (Personal communication, 2022). (Bingham University, New Karu, Nigeria), Personal communication."
},
{
"DOI": "10.2217/fmb-2022-0014",
"article-title": "Effectiveness of ivermectin-based multidrug therapy in severely hypoxic, ambulatory COVID-19 patients",
"author": "Hazan",
"doi-asserted-by": "crossref",
"first-page": "339",
"journal-title": "Future Microbiol.",
"key": "ref_86",
"volume": "17",
"year": "2022"
},
{
"DOI": "10.23937/2474-3658/1510233",
"article-title": "A Randomized Controlled Trial of Ivermectin Monotherapy Versus HCQ, IVM, and AZ Combination Therapy in COVID-19 Patients in Nigeria",
"author": "Babalola",
"doi-asserted-by": "crossref",
"first-page": "233",
"journal-title": "J. Infect. Dis. Epidemiol.",
"key": "ref_87",
"volume": "7",
"year": "2021"
},
{
"key": "ref_88",
"unstructured": "Statistics Kingdom (2024, January 30). Mann Whitney U Test Calculator. Available online: http://www.statskingdom.com/170median_mann_whitney.html."
},
{
"key": "ref_89",
"unstructured": "Borody, T.J., and Clancy, R.L. (2024, March 29). Combination Therapy For COVID-19 Based on Ivermectin in an Australian Population. Trialsite News, 19 October 2021. Available online: https://www.trialsitenews.com/a/combination-therapy-for-covid-19-based-on-ivermectin-in-an-australian-population."
},
{
"DOI": "10.1016/j.nmni.2021.100924",
"article-title": "Ivermectin: A multifaceted drug of Nobel prize-honored distinction with indicated efficacy against a new global scourge, COVID-19",
"author": "Santin",
"doi-asserted-by": "crossref",
"first-page": "100924",
"journal-title": "New Microbes New Infect.",
"key": "ref_90",
"volume": "43",
"year": "2021"
},
{
"DOI": "10.1001/jama.2021.3071",
"article-title": "Effect of Ivermectin on Time to Resolution of Symptoms Among Adults with Mild COVID-19: A Randomized Clinical Trial",
"author": "Hurtado",
"doi-asserted-by": "crossref",
"first-page": "1426",
"journal-title": "JAMA",
"key": "ref_91",
"volume": "325",
"year": "2021"
},
{
"DOI": "10.1056/NEJMoa2115869",
"article-title": "Effect of Early Treatment with Ivermectin among Patients with COVID-19",
"author": "Reis",
"doi-asserted-by": "crossref",
"first-page": "1721",
"journal-title": "N. Engl. J. Med.",
"key": "ref_92",
"volume": "386",
"year": "2022"
},
{
"DOI": "10.3390/jcm12113625",
"doi-asserted-by": "crossref",
"key": "ref_93",
"unstructured": "Scheim, D.E., Aldous, C., Osimani, B., Fordham, E.J., and Hoy, W.E. (2023). When Characteristics of Clinical Trials Require Per-Protocol as Well as Intention-to-Treat Outcomes to Draw Reliable Conclusions: Three Examples. J. Clin. Med., 12."
},
{
"DOI": "10.31219/osf.io/u7ewz",
"doi-asserted-by": "crossref",
"key": "ref_94",
"unstructured": "Scheim, D.E., Hibberd, J.A., and Chamie-Quintero, J.J. (2021). Protocol violations in López-Medina et al.: 38 switched ivermectin (IVM) and placebo doses, failure of blinding, ubiquitous IVM use OTC in Cali, and nearly identical AEs for the IVM and control groups. OSF Prepr."
},
{
"DOI": "10.1038/d41586-020-02958-2",
"article-title": "Latin America’s embrace of an unproven COVID treatment is hindering drug trials",
"doi-asserted-by": "crossref",
"first-page": "481",
"journal-title": "Nature",
"key": "ref_95",
"volume": "586",
"year": "2020"
},
{
"key": "ref_96",
"unstructured": "U.S. Food & Drug Administration (2023, October 30). Memorandum Explaining Basis for Declining Request for Emergency Use Authorization of Fluvoxamine Maleate, Available online: https://www.accessdata.fda.gov/drugsatfda_docs/nda/2020/EUA%20110%20Fluvoxamine%20Decisional%20Memo_Redacted.pdf."
},
{
"key": "ref_97",
"unstructured": "NIH COVID-19 Treatment Guidelines (2023, October 30). NIH COVID-19 Treatment Guidelines. Fluvoxamine: Selected Clinical Data, Limitations and Interpretation. Table 4c. 16 December 2021, Available online: https://www.covid19treatmentguidelines.nih.gov/tables/fluvoxamine-data/."
},
{
"key": "ref_98",
"unstructured": "TOGETHER Trial DSS and Data Repository Screenshots (2023, October 30). Date-Time Stamped Screenshots from Publications of the TOGETHER trial (NCT04727424). Available online: https://drive.google.com/file/d/1pBZ1GihxW_ROB3Aid6tFMplqAyMYOGDl/preview."
},
{
"key": "ref_99",
"unstructured": "(2023, October 30). Email from Sarah Fullegar, Sent June 7, 2022, to Edmund Fordham, Screenshot, Email Addresses Redacted. Available online: https://drive.google.com/file/d/1lUsSRf1KX-pa9T5EX4HbegdK8mYNQ_Ty/preview."
},
{
"key": "ref_100",
"unstructured": "Letter from 66 Scientists and Physicians to the Coauthors of Reis et al (2023, October 30). 2022 and to others as Identified in the Correspondence, as Emailed on May 10, 2022, Together with the Email Thread of Follow-up Correspondence through July 19, 2022, with All But Certain Publicly Available Email Addresses Redacted. Available online: https://drive.google.com/file/d/1eSez1YNIf26PHAPX6oHpw-UFg-QY1cfd/preview."
},
{
"DOI": "10.1016/S2214-109X(21)00448-4",
"article-title": "Effect of early treatment with fluvoxamine on risk of emergency care and hospitalisation among patients with COVID-19: The TOGETHER randomised, platform clinical trial",
"author": "Reis",
"doi-asserted-by": "crossref",
"first-page": "e42",
"journal-title": "Lancet Glob. Health",
"key": "ref_101",
"volume": "10",
"year": "2022"
},
{
"article-title": "Effect of early treatment with metformin on risk of emergency care and hospitalization among patients with COVID-19: The TOGETHER randomized platform clinical trial",
"author": "Reis",
"first-page": "100142",
"journal-title": "Lancet Reg. Health Am.",
"key": "ref_102",
"volume": "6",
"year": "2022"
},
{
"DOI": "10.1016/j.jinf.2024.106130",
"article-title": "Ivermectin for COVID-19 in adults in the community (PRINCIPLE): An open, randomised, controlled, adaptive platform trial of short- and longer-term outcomes",
"author": "Hayward",
"doi-asserted-by": "crossref",
"first-page": "106130",
"journal-title": "J. Infect.",
"key": "ref_103",
"volume": "88",
"year": "2024"
},
{
"key": "ref_104",
"unstructured": "c19ivm.org (2024, March 04). PRINCIPLE: Significantly Improved Recovery and Lower Long COVID with Ivermectin. Available online: https://c19ivm.org/principleivm.html."
},
{
"DOI": "10.1016/S0140-6736(15)60696-1",
"article-title": "Offline: What is medicine’s 5 sigma?",
"author": "Horton",
"doi-asserted-by": "crossref",
"first-page": "1380",
"journal-title": "Lancet",
"key": "ref_105",
"volume": "385",
"year": "2015"
},
{
"DOI": "10.1016/j.jclinepi.2016.02.012",
"article-title": "Evidence-based medicine has been hijacked: A report to David Sackett",
"author": "Ioannidis",
"doi-asserted-by": "crossref",
"first-page": "82",
"journal-title": "J. Clin. Epidemiol.",
"key": "ref_106",
"volume": "73",
"year": "2016"
},
{
"key": "ref_107",
"unstructured": "Gotzsche, P. (2013). Deadly Medicines and Organised Crime: How Big Pharma Has Corrupted Healthcare, CRC Press. [1st ed.]. Chapter 19."
},
{
"DOI": "10.1111/anae.15263",
"article-title": "False individual patient data and zombie randomised controlled trials submitted to Anaesthesia",
"author": "Carlisle",
"doi-asserted-by": "crossref",
"first-page": "472",
"journal-title": "Anaesthesia",
"key": "ref_108",
"volume": "76",
"year": "2021"
},
{
"DOI": "10.1016/j.futures.2021.102860",
"article-title": "Science, the endless frontier of regulatory capture",
"author": "Saltelli",
"doi-asserted-by": "crossref",
"first-page": "102860",
"journal-title": "Futures",
"key": "ref_109",
"volume": "135",
"year": "2022"
},
{
"DOI": "10.1136/bmj.h2942",
"article-title": "Justifying conflicts of interest in medical journals: A very bad idea",
"author": "Steinbrook",
"doi-asserted-by": "crossref",
"first-page": "h2942",
"journal-title": "BMJ",
"key": "ref_110",
"volume": "350",
"year": "2015"
},
{
"DOI": "10.1001/jama.300.9.1069",
"article-title": "Industry-Sponsored Clinical Research: A Broken System",
"author": "Angell",
"doi-asserted-by": "crossref",
"first-page": "1069",
"journal-title": "JAMA",
"key": "ref_111",
"volume": "300",
"year": "2008"
},
{
"DOI": "10.1017/S0963180107070478",
"article-title": "Commercialism and Medicine: An Overview",
"author": "Kassirer",
"doi-asserted-by": "crossref",
"first-page": "377",
"journal-title": "Camb. Q. Healthc. Ethics",
"key": "ref_112",
"volume": "16",
"year": "2007"
},
{
"DOI": "10.1136/bmj.39024.487720.68",
"article-title": "What have we learnt from Vioxx?",
"author": "Krumholz",
"doi-asserted-by": "crossref",
"first-page": "120",
"journal-title": "BMJ",
"key": "ref_113",
"volume": "334",
"year": "2007"
},
{
"DOI": "10.5694/j.1326-5377.1990.tb136833.x",
"article-title": "Cure of duodenal ulcer after eradication of Helicobacter pylori",
"author": "George",
"doi-asserted-by": "crossref",
"first-page": "145",
"journal-title": "Med. J. Aust.",
"key": "ref_114",
"volume": "153",
"year": "1990"
},
{
"DOI": "10.1111/hel.12751",
"article-title": "Clinical and economic impact of “triple therapy” for Helicobacter pylori eradication on peptic ulcer disease in Australia",
"author": "Eslick",
"doi-asserted-by": "crossref",
"first-page": "e12751",
"journal-title": "Helicobacter",
"key": "ref_115",
"volume": "25",
"year": "2020"
},
{
"DOI": "10.7208/chicago/9780226239668.001.0001",
"doi-asserted-by": "crossref",
"key": "ref_116",
"unstructured": "Feenstra, R.C., and Shapiro, M.D. (2003). Scanner Data and Price Indexes, University of Chicago Press."
},
{
"key": "ref_117",
"unstructured": "Wemple, E. (2023, October 30). Opinion: Bogus Oklahoma ivermectin story was just too good to check. Washington Post, 9 September 2021. Available online: https://www.washingtonpost.com/opinions/2021/09/09/bogus-oklahoma-ivermectin-story-was-just-too-good-check/."
},
{
"key": "ref_118",
"unstructured": "McCarthy, J., Kory, P.D., and Bigtree, D. (2023). War on Ivermectin: The Medicine that Saved Millions and Could Have Ended the Pandemic, Skyhorse. Chapter 33."
},
{
"key": "ref_119",
"unstructured": "Pfeiffer, M.B., and Bonvie, L. (2023, October 30). Horse-Bleep: How 4 Calls on Animal Ivermectin Launched a False FDA-Media Attack on a Life-Saving Human Medicine. rescue.substack.com, 16 October 2021. Available online: https://rescue.substack.com/p/horse-bleep-how-4-calls-on-animal."
},
{
"DOI": "10.31219/osf.io/bxk7d",
"doi-asserted-by": "crossref",
"key": "ref_120",
"unstructured": "Scheim, D.E. (2023). “Discredit,” “Neutralize,” “Destroy”: The targeting of doctors and scientists who reported the deadly toxicities of a painkilling drug. OSF Prepr."
},
{
"article-title": "COVID-19 Excess Deaths in Peru’s 25 States in 2020: Nationwide Trends, Confounding Factors, and Correlations with the Extent of Ivermectin Treatment by State",
"author": "Chamie",
"first-page": "e43168",
"journal-title": "Cureus",
"key": "ref_121",
"volume": "15",
"year": "2023"
},
{
"DOI": "10.1111/bcp.13840",
"article-title": "Population pharmacokinetics of oral ivermectin in venous plasma and dried blood spots in healthy volunteers",
"author": "Duthaler",
"doi-asserted-by": "crossref",
"first-page": "626",
"journal-title": "Br. J. Clin. Pharmacol.",
"key": "ref_122",
"volume": "85",
"year": "2019"
},
{
"DOI": "10.1097/00007890-199311000-00029",
"article-title": "Blood distribution of rapamycin",
"author": "Yatscoff",
"doi-asserted-by": "crossref",
"first-page": "1202",
"journal-title": "Transplantation",
"key": "ref_123",
"volume": "56",
"year": "1993"
},
{
"DOI": "10.1097/00007691-199312000-00004",
"article-title": "Therapeutic monitoring of rapamycin: A new immunosuppressive drug",
"author": "Yatscoff",
"doi-asserted-by": "crossref",
"first-page": "478",
"journal-title": "Ther. Drug Monit.",
"key": "ref_124",
"volume": "15",
"year": "1993"
},
{
"key": "ref_125",
"unstructured": "U.S. Food & Drug Administration (2024, January 29). Clinical Pharmacology/Biopharmaceutics Review, NDA: 21,083; Sirolimus (Rapamune), Available online: https://www.accessdata.fda.gov/drugsatfda_docs/nda/99/21083A_Rapamune_clinphrmr.pdf."
},
{
"article-title": "Red blood cells: A neglected compartment in pharmacokinetics and pharmacodynamics",
"author": "Hinderling",
"first-page": "279",
"journal-title": "Pharmacol. Rev.",
"key": "ref_126",
"volume": "49",
"year": "1997"
},
{
"DOI": "10.3389/fphys.2023.1308632",
"article-title": "Drug transport by red blood cells",
"author": "Biagiotti",
"doi-asserted-by": "crossref",
"first-page": "1308632",
"journal-title": "Front. Physiol.",
"key": "ref_127",
"volume": "14",
"year": "2023"
},
{
"DOI": "10.1021/acs.jafc.0c02601",
"article-title": "Red Blood Cells and Lipoproteins: Important Reservoirs and Transporters of Polyphenols and Their Metabolites",
"author": "Harbi",
"doi-asserted-by": "crossref",
"first-page": "7005",
"journal-title": "J. Agric. Food Chem.",
"key": "ref_128",
"volume": "68",
"year": "2020"
},
{
"DOI": "10.1093/cid/ciab465",
"article-title": "Circulating Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Vaccine Antigen Detected in the Plasma of mRNA-1273 Vaccine Recipients",
"author": "Ogata",
"doi-asserted-by": "crossref",
"first-page": "715",
"journal-title": "Clin. Infect. Dis.",
"key": "ref_129",
"volume": "74",
"year": "2022"
},
{
"DOI": "10.3390/s21175857",
"doi-asserted-by": "crossref",
"key": "ref_130",
"unstructured": "Cognetti, J.S., and Miller, B.L. (2021). Monitoring Serum Spike Protein with Disposable Photonic Biosensors Following SARS-CoV-2 Vaccination. Sensors, 21."
},
{
"DOI": "10.1161/01.CIR.99.9.1165",
"article-title": "Sex, Age, Cardiovascular Risk Factors, and Coronary Heart Disease",
"author": "Jousilahti",
"doi-asserted-by": "crossref",
"first-page": "1165",
"journal-title": "Circulation",
"key": "ref_131",
"volume": "99",
"year": "1999"
},
{
"DOI": "10.1177/2047487319878371",
"article-title": "Diabetes as a cardiovascular risk factor: An overview of global trends of macro and micro vascular complications",
"author": "Ceriello",
"doi-asserted-by": "crossref",
"first-page": "25",
"journal-title": "Eur. J. Prev. Cardiol.",
"key": "ref_132",
"volume": "26",
"year": "2019"
},
{
"article-title": "Obesity and Cardiovascular Disease: A Scientific Statement From the American Heart Association",
"author": "Poirier",
"first-page": "e984",
"journal-title": "Circulation",
"key": "ref_133",
"volume": "143",
"year": "2021"
},
{
"DOI": "10.3390/ijms21186756",
"doi-asserted-by": "crossref",
"key": "ref_134",
"unstructured": "Michel, J.-B., and Martin-Ventura, J.L. (2020). Red Blood Cells and Hemoglobin in Human Atherosclerosis and Related Arterial Diseases. Int. J. Mol. Sci., 21."
},
{
"DOI": "10.3390/ijms22115843",
"doi-asserted-by": "crossref",
"key": "ref_135",
"unstructured": "Turpin, C., Catan, A., Meilhac, O., Bourdon, E., Canonne-Hergaux, F., and Rondeau, P. (2021). Erythrocytes: Central Actors in Multiple Scenes of Atherosclerosis. Int. J. Mol. Sci., 22."
},
{
"DOI": "10.1016/S0195-668X(02)00741-8",
"article-title": "Erythrocyte sedimentation rate, coronary atherosclerosis, and cardiac mortality",
"author": "Natali",
"doi-asserted-by": "crossref",
"first-page": "639",
"journal-title": "Eur. Heart J.",
"key": "ref_136",
"volume": "24",
"year": "2003"
},
{
"DOI": "10.1155/2008/184647",
"article-title": "Erythrocyte aggregation as an early biomarker in patients with asymptomatic carotid stenosis",
"author": "Assayag",
"doi-asserted-by": "crossref",
"first-page": "33",
"journal-title": "Dis. Markers",
"key": "ref_137",
"volume": "24",
"year": "2008"
},
{
"DOI": "10.1053/euhj.2000.2148",
"article-title": "Erythrocyte sedimentation rate: A possible marker of atherosclerosis and a strong predictor of coronary heart disease mortality",
"author": "Erikssen",
"doi-asserted-by": "crossref",
"first-page": "1614",
"journal-title": "Eur. Heart J.",
"key": "ref_138",
"volume": "21",
"year": "2000"
},
{
"DOI": "10.1258/ebm.2010.009370",
"article-title": "Polyphenols enhance total oxidant-scavenging capacities of human blood by binding to red blood cells",
"author": "Koren",
"doi-asserted-by": "crossref",
"first-page": "689",
"journal-title": "Exp. Biol. Med.",
"key": "ref_139",
"volume": "235",
"year": "2010"
},
{
"DOI": "10.1155/2020/7262474",
"article-title": "Hemorheological Alterations in Patients with Heart Failure with Reduced Ejection Fraction Treated by Resveratrol",
"author": "Gal",
"doi-asserted-by": "crossref",
"first-page": "7262474",
"journal-title": "Cardiovasc. Ther.",
"key": "ref_140",
"volume": "2020",
"year": "2020"
},
{
"DOI": "10.5152/eurjrheum.2023.23064",
"article-title": "Resveratrol in Rheumatological Diseases: A Systematic Review",
"author": "Carvalho",
"doi-asserted-by": "crossref",
"first-page": "163",
"journal-title": "Eur. J. Rheumatol.",
"key": "ref_141",
"volume": "10",
"year": "2023"
},
{
"DOI": "10.1016/j.imbio.2016.10.008",
"article-title": "Resveratrol improves treatment outcome and laboratory parameters in patients with Takayasu arteritis: A randomized double-blind and placebo-controlled trial",
"author": "Shi",
"doi-asserted-by": "crossref",
"first-page": "164",
"journal-title": "Immunobiology",
"key": "ref_142",
"volume": "222",
"year": "2017"
},
{
"DOI": "10.3389/neuro.24.004.2009",
"article-title": "Resveratrol preserves cerebrovascular density and cognitive function in aging mice",
"author": "Oomen",
"doi-asserted-by": "crossref",
"first-page": "900",
"journal-title": "Front. Aging Neurosci.",
"key": "ref_143",
"volume": "1",
"year": "2009"
},
{
"DOI": "10.3390/molecules15096570",
"article-title": "Determination of Quercetin and Resveratrol in Whole Blood—Implications for Bioavailability Studies",
"author": "Biasutto",
"doi-asserted-by": "crossref",
"first-page": "6570",
"journal-title": "Molecules",
"key": "ref_144",
"volume": "15",
"year": "2010"
},
{
"key": "ref_145",
"unstructured": "Oregon State University, Linus Pauling Institute (2024, January 30). Micronutrient Information Center: Resveratrol. 11 June 2015. Available online: https://lpi.oregonstate.edu/mic/dietary-factors/phytochemicals/resveratrol."
},
{
"DOI": "10.1002/biof.105",
"article-title": "Resveratrol: Biological and pharmaceutical properties as anticancer molecule",
"author": "Hsieh",
"doi-asserted-by": "crossref",
"first-page": "360",
"journal-title": "Biofactors",
"key": "ref_146",
"volume": "36",
"year": "2010"
},
{
"DOI": "10.1111/j.1749-6632.2010.05842.x",
"article-title": "Bioavailability of resveratrol",
"author": "Walle",
"doi-asserted-by": "crossref",
"first-page": "9",
"journal-title": "Ann. N. Y. Acad. Sci.",
"key": "ref_147",
"volume": "1215",
"year": "2011"
},
{
"DOI": "10.1016/S0378-4347(00)86110-1",
"article-title": "Distribution of chloroquine and its metabolite desethyl-chloroquine in human blood cells and its implication for the quantitative determination of these compounds in serum and plasma",
"author": "Bergqvist",
"doi-asserted-by": "crossref",
"first-page": "137",
"journal-title": "J. Chromatogr.",
"key": "ref_148",
"volume": "272",
"year": "1983"
},
{
"DOI": "10.1001/jama.1960.03020150054010",
"article-title": "Use of antimalarial drugs as “desludging” agents in vascular disease processes: Preliminary report",
"author": "Madow",
"doi-asserted-by": "crossref",
"first-page": "1630",
"journal-title": "JAMA",
"key": "ref_149",
"volume": "172",
"year": "1960"
},
{
"article-title": "Desludging Action of Hydroxychloroquine in R.A",
"author": "Cecchi",
"first-page": "214",
"journal-title": "Acta Rheumatol. Scand.",
"key": "ref_150",
"volume": "8",
"year": "1962"
},
{
"DOI": "10.1161/01.CIR.96.12.4380",
"article-title": "Hydroxychloroquine Reverses Thrombogenic Properties of Antiphospholipid Antibodies in Mice",
"author": "Edwards",
"doi-asserted-by": "crossref",
"first-page": "4380",
"journal-title": "Circulation",
"key": "ref_151",
"volume": "96",
"year": "1997"
},
{
"DOI": "10.1016/j.jaad.2020.12.013",
"article-title": "Use of hydroxychloroquine and risk of major adverse cardiovascular events in patients with lupus erythematosus: A Danish nationwide cohort study",
"author": "Haugaard",
"doi-asserted-by": "crossref",
"first-page": "930",
"journal-title": "J. Am. Acad. Dermatol.",
"key": "ref_152",
"volume": "84",
"year": "2021"
},
{
"DOI": "10.1002/acr.24850",
"article-title": "Hydroxychloroquine Use and Cardiovascular Events Among Patients with Systemic Lupus Erythematosus and Rheumatoid Arthritis",
"author": "Jorge",
"doi-asserted-by": "crossref",
"first-page": "743",
"journal-title": "Arthritis Care Res.",
"key": "ref_153",
"volume": "75",
"year": "2023"
},
{
"DOI": "10.18632/oncotarget.23570",
"article-title": "The association between hydroxychloroquine treatment and cardiovascular morbidity among rheumatoid arthritis patients",
"author": "Shapiro",
"doi-asserted-by": "crossref",
"first-page": "6615",
"journal-title": "Oncotarget",
"key": "ref_154",
"volume": "9",
"year": "2017"
},
{
"DOI": "10.3389/fphar.2012.00141",
"article-title": "Resveratrol: French paradox revisited",
"author": "Catalgol",
"doi-asserted-by": "crossref",
"first-page": "141",
"journal-title": "Front. Pharmacol.",
"key": "ref_155",
"volume": "3",
"year": "2012"
},
{
"DOI": "10.3233/CH-2012-1632",
"article-title": "Effects of ethanol on red blood cell rheological behavior",
"author": "Rabai",
"doi-asserted-by": "crossref",
"first-page": "87",
"journal-title": "Clin. Hemorheol. Microcirc.",
"key": "ref_156",
"volume": "56",
"year": "2014"
},
{
"DOI": "10.1016/0140-6736(92)91277-F",
"article-title": "Wine, alcohol, platelets, and the French paradox for coronary heart disease",
"author": "Renaud",
"doi-asserted-by": "crossref",
"first-page": "1523",
"journal-title": "Lancet",
"key": "ref_157",
"volume": "339",
"year": "1992"
},
{
"DOI": "10.1001/jamanetworkopen.2022.3849",
"article-title": "Association of Habitual Alcohol Intake with Risk of Cardiovascular Disease",
"author": "Biddinger",
"doi-asserted-by": "crossref",
"first-page": "e223849",
"journal-title": "JAMA Netw. Open",
"key": "ref_158",
"volume": "5",
"year": "2022"
},
{
"DOI": "10.15288/jsad.2017.78.375",
"article-title": "Alcohol Consumption and Mortality From Coronary Heart Disease: An Updated Meta-Analysis of Cohort Studies",
"author": "Zhao",
"doi-asserted-by": "crossref",
"first-page": "375",
"journal-title": "J. Stud. Alcohol. Drugs",
"key": "ref_159",
"volume": "78",
"year": "2017"
},
{
"DOI": "10.1007/s11033-022-07700-x",
"article-title": "SARS-CoV-2 cell entry beyond the ACE2 receptor",
"author": "Alipoor",
"doi-asserted-by": "crossref",
"first-page": "10715",
"journal-title": "Mol. Biol. Rep.",
"key": "ref_160",
"volume": "49",
"year": "2022"
},
{
"DOI": "10.1016/j.xcrp.2023.101346",
"article-title": "SARS-CoV-2 evolved variants optimize binding to cellular glycocalyx",
"author": "Kim",
"doi-asserted-by": "crossref",
"first-page": "101346",
"journal-title": "Cell Rep. Phys. Sci.",
"key": "ref_161",
"volume": "4",
"year": "2023"
},
{
"DOI": "10.1002/cbic.202100681",
"doi-asserted-by": "crossref",
"key": "ref_162",
"unstructured": "Nie, C., Sahoo, A.K., Netz, R.R., Herrmann, A., Ballauff, M., and Haag, R. (2022). Charge Matters: Mutations in Omicron Variant Favor Binding to Cells. ChemBioChem, 23."
},
{
"DOI": "10.3389/fviro.2022.894531",
"doi-asserted-by": "crossref",
"key": "ref_163",
"unstructured": "Gan, H.H., Zinno, J., Piano, F., and Gunsalus, K.C. (2022). Omicron Spike Protein Has a Positive Electrostatic Surface That Promotes ACE2 Recognition and Antibody Escape. Front. Virol., 2."
},
{
"DOI": "10.1016/B978-0-12-800097-7.00003-8",
"article-title": "Chapter Three—Modulation of Glycan Recognition by Clustered Saccharide Patches",
"author": "Jeon",
"doi-asserted-by": "crossref",
"first-page": "75",
"journal-title": "International Review of Cell and Molecular Biology",
"key": "ref_164",
"volume": "Volume 308",
"year": "2014"
},
{
"DOI": "10.3389/fmolb.2021.727847",
"doi-asserted-by": "crossref",
"key": "ref_165",
"unstructured": "Soares, C.O., Grosso, A.S., Ereño-Orbea, J., Coelho, H., and Marcelo, F. (2021). Molecular Recognition Insights of Sialic Acid Glycans by Distinct Receptors Unveiled by NMR and Molecular Modeling. Front. Mol. Biosci., 8."
},
{
"DOI": "10.1038/nrmicro3346",
"article-title": "The sweet spot: Defining virus–sialic acid interactions",
"author": "Reiss",
"doi-asserted-by": "crossref",
"first-page": "739",
"journal-title": "Nat. Rev. Microbiol.",
"key": "ref_166",
"volume": "12",
"year": "2014"
},
{
"DOI": "10.1089/omi.2009.0148",
"article-title": "The sialome—far more than the sum of its parts",
"author": "Cohen",
"doi-asserted-by": "crossref",
"first-page": "455",
"journal-title": "Omics",
"key": "ref_167",
"volume": "14",
"year": "2010"
},
{
"DOI": "10.1016/j.bbagen.2019.05.012",
"article-title": "Exploitation of glycosylation in enveloped virus pathobiology",
"author": "Watanabe",
"doi-asserted-by": "crossref",
"first-page": "1480",
"journal-title": "Biochim. Biophys. Acta (BBA)—Gen. Subj.",
"key": "ref_168",
"volume": "1863",
"year": "2019"
},
{
"DOI": "10.1016/0042-6822(91)90026-8",
"article-title": "Isolated HE-protein from hemagglutinating encephalomyelitis virus and bovine coronavirus has receptor-destroying and receptor-binding activity",
"author": "Schultze",
"doi-asserted-by": "crossref",
"first-page": "221",
"journal-title": "Virology",
"key": "ref_169",
"volume": "180",
"year": "1991"
},
{
"DOI": "10.1016/j.coviro.2019.01.004",
"article-title": "Virus recognition of glycan receptors",
"author": "Thompson",
"doi-asserted-by": "crossref",
"first-page": "117",
"journal-title": "Curr. Opin. Virol.",
"key": "ref_170",
"volume": "34",
"year": "2019"
},
{
"DOI": "10.1128/JVI.01567-19",
"article-title": "Modified Sialic Acids on Mucus and Erythrocytes Inhibit Influenza A Virus Hemagglutinin and Neuraminidase Functions",
"author": "Barnard",
"doi-asserted-by": "crossref",
"first-page": "10",
"journal-title": "J. Virol.",
"key": "ref_171",
"volume": "94",
"year": "2020"
},
{
"DOI": "10.1038/s41586-022-04479-6",
"article-title": "SARS-CoV-2 Omicron variant replication in human bronchus and lung ex vivo",
"author": "Hui",
"doi-asserted-by": "crossref",
"first-page": "715",
"journal-title": "Nature",
"key": "ref_172",
"volume": "603",
"year": "2022"
},
{
"DOI": "10.1101/2021.12.31.474653",
"doi-asserted-by": "crossref",
"key": "ref_173",
"unstructured": "Peacock, T.P., Brown, J.C., Zhou, J., Thakur, N., Sukhova, K., Newman, J., Kugathasan, R., Yan, A.W.C., Furnon, W., and De Lorenzo, G. (2022). The altered entry pathway and antigenic distance of the SARS-CoV-2 Omicron variant map to separate domains of spike protein. bioRxiv."
},
{
"key": "ref_174",
"unstructured": "Makary, M. (2023, October 30). The Real Data Behind the New COVID Vaccines the White House is Pushing. New York Post, 14 September 2023. Available online: https://nypost.com/2023/09/14/the-real-data-behind-the-new-covid-vaccines-the-white-house-is-pushing/."
},
{
"key": "ref_175",
"unstructured": "(2024, February 23). NIH Media Advisory, 19 July 2022. Vaccine-Induced Immune Response to Omicron Wanes Substantially Over Time, Available online: https://www.nih.gov/news-events/news-releases/vaccine-induced-immune-response-omicron-wanes-substantially-over-time."
},
{
"DOI": "10.1016/j.xcrm.2022.100679",
"article-title": "Rapid decline in vaccine-boosted neutralizing antibodies against SARS-CoV-2 Omicron variant",
"author": "Lyke",
"doi-asserted-by": "crossref",
"first-page": "100679",
"journal-title": "Cell Rep. Med.",
"key": "ref_176",
"volume": "3",
"year": "2022"
},
{
"DOI": "10.1101/2023.06.09.23290893",
"doi-asserted-by": "crossref",
"key": "ref_177",
"unstructured": "Shrestha, N.K., Burke, P.C., Nowacki, A.S., and Gordon, S.M. (2023). Risk of Coronavirus Disease 2019 (COVID-19) among those up-to-date and not up-to-date on COVID-19 vaccination by US CDC criteria. PLoS ONE, 18."
},
{
"DOI": "10.1093/ofid/ofad209",
"article-title": "Effectiveness of the Coronavirus Disease 2019 Bivalent Vaccine",
"author": "Shrestha",
"doi-asserted-by": "crossref",
"first-page": "ofad209",
"journal-title": "Open Forum Infect. Dis.",
"key": "ref_178",
"volume": "10",
"year": "2023"
},
{
"DOI": "10.1093/cid/ciac722",
"article-title": "Persistent circulating SARS-CoV-2 spike Is associated with post-acute COVID-19 sequelae",
"author": "Swank",
"doi-asserted-by": "crossref",
"first-page": "e487",
"journal-title": "Clin. Infect. Dis.",
"key": "ref_179",
"volume": "76",
"year": "2022"
},
{
"DOI": "10.1002/jmv.28364",
"article-title": "Liquid biomarkers of macrophage dysregulation and circulating spike protein illustrate the biological heterogeneity in patients with post-acute sequelae of COVID-19",
"author": "Willscher",
"doi-asserted-by": "crossref",
"first-page": "e28364",
"journal-title": "J. Med. Virol.",
"key": "ref_180",
"volume": "95",
"year": "2023"
},
{
"DOI": "10.3389/fimmu.2021.746021",
"article-title": "Persistence of SARS-CoV-2 S1 Protein in CD16+ Monocytes in Post-Acute Sequelae of COVID-19 (PASC) up to 15 Months Post-Infection",
"author": "Patterson",
"doi-asserted-by": "crossref",
"first-page": "5526",
"journal-title": "Front. Immunol.",
"key": "ref_181",
"volume": "12",
"year": "2022"
},
{
"DOI": "10.1002/jmv.28568",
"article-title": "Persistent circulation of soluble and extracellular vesicle-linked Spike protein in individuals with postacute sequelae of COVID-19",
"author": "Craddock",
"doi-asserted-by": "crossref",
"first-page": "e28568",
"journal-title": "J. Med. Virol.",
"key": "ref_182",
"volume": "95",
"year": "2023"
},
{
"article-title": "Use of Ivermectin as a Prophylactic Option in Asymptomatic Family Close Contacts with Patients of COVID-19 (NCT number: 04422561)",
"author": "Shouman",
"first-page": "OC27",
"journal-title": "J. Clin. Diagn. Res.",
"key": "ref_183",
"volume": "15",
"year": "2021"
},
{
"DOI": "10.1016/j.ijid.2021.04.035",
"article-title": "Positive impact of oral hydroxychloroquine and povidone-iodine throat spray for COVID-19 prophylaxis: An open-label randomized trial",
"author": "Seet",
"doi-asserted-by": "crossref",
"first-page": "314",
"journal-title": "Int. J. Infect. Dis.",
"key": "ref_184",
"volume": "106",
"year": "2021"
},
{
"DOI": "10.1097/MJT.0000000000001433",
"article-title": "Intensive Treatment with Ivermectin and Iota-Carrageenan as Pre-exposure Prophylaxis for COVID-19 in Health Care Workers From Tucuman, Argentina",
"author": "Chahla",
"doi-asserted-by": "crossref",
"first-page": "e601",
"journal-title": "Am. J. Ther.",
"key": "ref_185",
"volume": "28",
"year": "2021"
},
{
"key": "ref_186",
"unstructured": "Desort-Henin, V., Kostova, A., Babiker, E.A., Caramel, A., and Malamut, R. (2023, July 03). The SAIVE Trial, Post-Exposure use of ivermectin in COVID-19 prevention: Efficacy and Safety Results. Poster Presentation, European Congress of Clinical Microbiology and Infectious Diseases. Available online: https://www.medincell.com/wp-content/uploads/2023/04/Poster-SAIVE-April2023-OK3.pdf."
},
{
"key": "ref_187",
"unstructured": "The Nobel Assembly at Karolinska Institutet (2023, October 10). The 2015 Nobel Prize in Physiology or Medicine—Press release. 5 October 2015. Available online: https://www.nobelprize.org/prizes/medicine/2015/press-release/."
},
{
"DOI": "10.1097/00000658-196403000-00017",
"article-title": "Correlation between sludge in the bulbar conjunctiva and the mesentery",
"author": "Bjoerk",
"doi-asserted-by": "crossref",
"first-page": "428",
"journal-title": "Ann. Surg.",
"key": "ref_188",
"volume": "159",
"year": "1964"
},
{
"DOI": "10.1126/science.106.2758.431",
"article-title": "Sludged Blood",
"author": "Knisely",
"doi-asserted-by": "crossref",
"first-page": "431",
"journal-title": "Science",
"key": "ref_189",
"volume": "106",
"year": "1947"
},
{
"DOI": "10.1007/978-3-642-29423-5",
"doi-asserted-by": "crossref",
"key": "ref_190",
"unstructured": "Gresele, P., Born, G.V.R., Patrono, C., and Page, C.P. (2012). Antiplatelet Agents, Springer."
},
{
"DOI": "10.1016/S0046-8177(87)80005-9",
"article-title": "Cell biology of endothelial cells",
"author": "Jaffe",
"doi-asserted-by": "crossref",
"first-page": "234",
"journal-title": "Human. Pathol.",
"key": "ref_191",
"volume": "18",
"year": "1987"
},
{
"DOI": "10.1016/S0006-3495(83)84378-1",
"article-title": "Theory of the electrokinetic behavior of human erythrocytes",
"author": "Levine",
"doi-asserted-by": "crossref",
"first-page": "127",
"journal-title": "Biophys. J.",
"key": "ref_192",
"volume": "42",
"year": "1983"
},
{
"DOI": "10.1681/ASN.2007010119",
"article-title": "Glomerular endothelial glycocalyx constitutes a barrier to protein permeability",
"author": "Singh",
"doi-asserted-by": "crossref",
"first-page": "2885",
"journal-title": "J. Am. Soc. Nephrol.",
"key": "ref_193",
"volume": "18",
"year": "2007"
},
{
"DOI": "10.15252/msb.20209610",
"doi-asserted-by": "crossref",
"key": "ref_194",
"unstructured": "Hikmet, F., Méar, L., Edvinsson, Å., Micke, P., Uhlén, M., and Lindskog, C. (2020). The protein expression profile of ACE2 in human tissues. Mol. Syst. Biol., 16."
},
{
"DOI": "10.1016/S2352-3026(20)30216-7",
"article-title": "Endotheliopathy in COVID-19-associated coagulopathy: Evidence from a single-centre, cross-sectional study",
"author": "Goshua",
"doi-asserted-by": "crossref",
"first-page": "e575",
"journal-title": "Lancet Haematol.",
"key": "ref_195",
"volume": "7",
"year": "2020"
},
{
"DOI": "10.1111/jth.15067",
"article-title": "Coagulation biomarkers are independent predictors of increased oxygen requirements in COVID-19",
"author": "Rauch",
"doi-asserted-by": "crossref",
"first-page": "2942",
"journal-title": "J. Thromb. Haemost.",
"key": "ref_196",
"volume": "18",
"year": "2020"
},
{
"DOI": "10.1021/ci700044s",
"article-title": "Analysis of HIV Wild-Type and Mutant Structures via in Silico Docking against Diverse Ligand Libraries",
"author": "Chang",
"doi-asserted-by": "crossref",
"first-page": "1258",
"journal-title": "J. Chem. Inf. Model.",
"key": "ref_197",
"volume": "47",
"year": "2007"
},
{
"DOI": "10.1186/s12936-017-1801-4",
"article-title": "Ivermectin to reduce malaria transmission I. Pharmacokinetic and pharmacodynamic considerations regarding efficacy and safety",
"author": "Chaccour",
"doi-asserted-by": "crossref",
"first-page": "161",
"journal-title": "Malar. J.",
"key": "ref_198",
"volume": "16",
"year": "2017"
},
{
"DOI": "10.1177/009127002237994",
"article-title": "Safety, tolerability, and pharmacokinetics of escalating high doses of ivermectin in healthy adult subjects",
"author": "Guzzo",
"doi-asserted-by": "crossref",
"first-page": "1122",
"journal-title": "J. Clin. Pharmacol.",
"key": "ref_199",
"volume": "42",
"year": "2002"
},
{
"DOI": "10.1208/s12248-007-9000-9",
"article-title": "The Pharmacokinetics and Interactions of Ivermectin in Humans—A Mini-review",
"doi-asserted-by": "crossref",
"first-page": "42",
"journal-title": "AAPS J.",
"key": "ref_200",
"volume": "10",
"year": "2008"
},
{
"DOI": "10.1371/journal.pntd.0006020",
"doi-asserted-by": "crossref",
"key": "ref_201",
"unstructured": "Munoz, J., Ballester, M.R., Antonijoan, R.M., Gich, I., Rodriguez, M., Colli, E., Gold, S., and Krolewiecki, A.J. (2018). Safety and pharmacokinetic profile of fixed-dose ivermectin with an innovative 18mg tablet in healthy adult volunteers. PLoS Negl. Trop. Dis., 12."
},
{
"DOI": "10.1007/s002280050131",
"article-title": "Ivermectin distribution in the plasma and tissues of patients infected with Onchocerca volvulus",
"author": "Baraka",
"doi-asserted-by": "crossref",
"first-page": "407",
"journal-title": "Eur. J. Clin. Pharmacol.",
"key": "ref_202",
"volume": "50",
"year": "1996"
},
{
"DOI": "10.1111/j.1440-1681.1990.tb01273.x",
"article-title": "The effect of ivermectin on some haematological indices in rabbits: Influence of vitamin K treatment",
"author": "Ali",
"doi-asserted-by": "crossref",
"first-page": "735",
"journal-title": "Clin. Exp. Pharmacol. Physiol.",
"key": "ref_203",
"volume": "17",
"year": "1990"
}
],
"reference-count": 203,
"references-count": 203,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.mdpi.com/1999-4915/16/4/647"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"title": "Back to the Basics of SARS-CoV-2 Biochemistry: Microvascular Occlusive Glycan Bindings Govern Its Morbidities and Inform Therapeutic Responses",
"type": "journal-article",
"volume": "16"
}
scheim6
