Parallel use of human stem cell lung and heart models provide insights for SARS-CoV-2 treatment
et al., Stem Cell Reports, doi:10.1016/j.stemcr.2023.05.007, Jun 2023
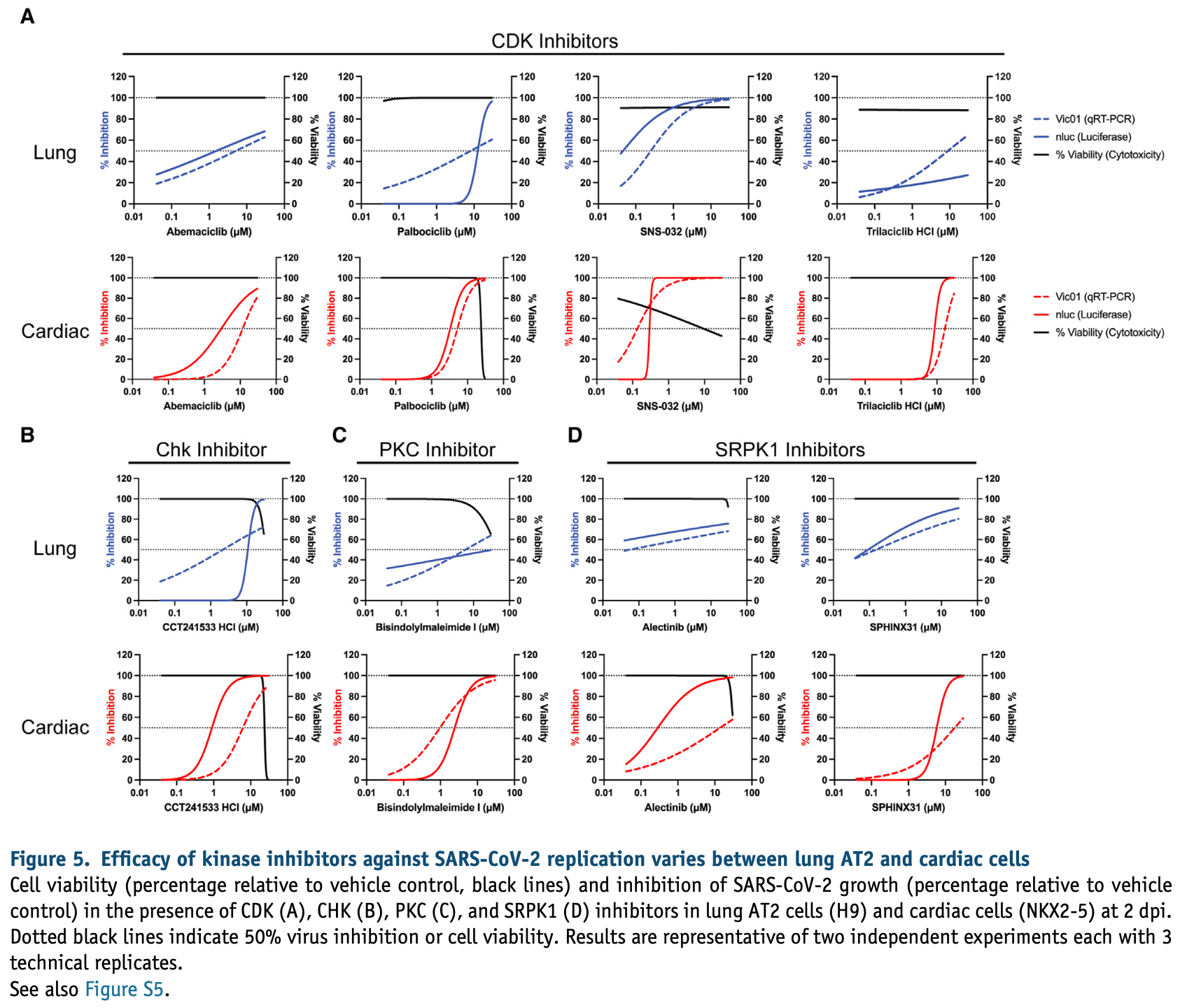
In vitro study showing that SARS-CoV-2 cell entry differs across cell types. ACE2 was required for infection in both lung and cardiac cells, but TMPRSS2 cleavage was required in lung cells, while the endosomal pathway was required in cardiac cells.
Authors show that antiviral activity and cytotoxicity can be significantly different in cardiac and lung cells, and in the commonly used African monkey kidney-derived Vero cells.
These results highlight that, especially after SARS-CoV-2 spreads beyond the upper respiratory tract, a combination of treatments affecting different pathways may be more effective.
Gérard, Zhou, Wu, Kamo, Choi, Kim show increased risk of acute kidney injury, Leo, Briciu, Muntean, Petrov show increased risk of liver injury, and Negru, Cheng, Mohammed, Kwok show increased risk of cardiac disorders with remdesivir.
Study covers HCQ, remdesivir, and favipiravir.
1.
Gérard et al., Remdesivir and Acute Renal Failure: A Potential Safety Signal From Disproportionality Analysis of the WHO Safety Database, Clinical Pharmacology & Therapeutics, doi:10.1002/cpt.2145.
2.
Zhou et al., Acute Kidney Injury and Drugs Prescribed for COVID-19 in Diabetes Patients: A Real-World Disproportionality Analysis, Frontiers in Pharmacology, doi:10.3389/fphar.2022.833679.
3.
Wu et al., Acute Kidney Injury Associated With Remdesivir: A Comprehensive Pharmacovigilance Analysis of COVID-19 Reports in FAERS, Frontiers in Pharmacology, doi:10.3389/fphar.2022.692828.
4.
Kamo et al., Association of Antiviral Drugs for the Treatment of COVID-19 With Acute Renal Failure, In Vivo, doi:10.21873/invivo.13637.
5.
Choi et al., Comparative effectiveness of combination therapy with nirmatrelvir–ritonavir and remdesivir versus monotherapy with remdesivir or nirmatrelvir–ritonavir in patients hospitalised with COVID-19: a target trial emulation study, The Lancet Infectious Diseases, doi:10.1016/S1473-3099(24)00353-0.
6.
Kim et al., Investigating the Safety Profile of Fast‐Track COVID‐19 Drugs Using the FDA Adverse Event Reporting System Database: A Comparative Observational Study, Pharmacoepidemiology and Drug Safety, doi:10.1002/pds.70043.
7.
Leo et al., Hepatocellular liver injury in hospitalized patients affected by COVID-19: Presence of different risk factors at different time points, Digestive and Liver Disease, doi:10.1016/j.dld.2021.12.014.
8.
Briciu et al., Evolving Clinical Manifestations and Outcomes in COVID-19 Patients: A Comparative Analysis of SARS-CoV-2 Variant Waves in a Romanian Hospital Setting, Pathogens, doi:10.3390/pathogens12121453.
9.
Muntean et al., Effects of COVID-19 on the Liver and Mortality in Patients with SARS-CoV-2 Pneumonia Caused by Delta and Non-Delta Variants: An Analysis in a Single Centre, Pharmaceuticals, doi:10.3390/ph17010003.
10.
Petrov et al., The Effect of Potentially Hepatotoxic Medicinal Products on Alanine Transaminase Levels in COVID-19 Patients: A Case–Control Study, Safety and Risk of Pharmacotherapy, doi:10.30895/2312-7821-2025-458.
11.
Negru et al., Comparative Pharmacovigilance Analysis of Approved and Repurposed Antivirals for COVID-19: Insights from EudraVigilance Data, Biomedicines, doi:10.3390/biomedicines13061387.
12.
Cheng et al., Cardiovascular Safety of COVID-19 Treatments: A Disproportionality Analysis of Adverse Event Reports from the WHO VigiBase, Infectious Diseases and Therapy, doi:10.1007/s40121-025-01225-z.
Rudraraju et al., 1 Jun 2023, Australia, peer-reviewed, 28 authors.
Contact: enzo.porrello@mcri.edu.au (corresponding author), jose.polo@monash.edu, sean.humphrey@mcri.edu.au, mirana.ramialison@mcri.edu.au, david.elliott@mcri.edu.au, kanta.subbarao@influenzacentre.org.
In vitro studies are an important part of preclinical research, however results may be very different in vivo.
Parallel use of human stem cell lung and heart models provide insights for SARS-CoV-2 treatment
Stem Cell Reports, doi:10.1016/j.stemcr.2023.05.007
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) primarily infects the respiratory tract, but pulmonary and cardiac complications occur in severe coronavirus disease 2019 . To elucidate molecular mechanisms in the lung and heart, we conducted paired experiments in human stem cell-derived lung alveolar type II (AT2) epithelial cell and cardiac cultures infected with SARS-CoV-2. With CRISPR-Cas9-mediated knockout of ACE2, we demonstrated that angiotensin-converting enzyme 2 (ACE2) was essential for SARS-CoV-2 infection of both cell types but that further processing in lung cells required TMPRSS2, while cardiac cells required the endosomal pathway. Host responses were significantly different; transcriptome profiling and phosphoproteomics responses depended strongly on the cell type. We identified several antiviral compounds with distinct antiviral and toxicity profiles in lung AT2 and cardiac cells, highlighting the importance of using several relevant cell types for evaluation of antiviral drugs. Our data provide new insights into rational drug combinations for effective treatment of a virus that affects multiple organ systems.
EXPERIMENTAL PROCEDURES
Resource availability Corresponding authors Enzo R. Porrello, Jose M. Polo, Sean J. Humphrey, Mirana Ramialison, David A. Elliott or Kanta Subbarao are the corresponding authors for this paper.
Cells African green monkey kidney epithelial (Vero cells, ATCC Cat. CCL-81), Vero hSLAM (Merck, Cat. 04091501), Calu-3 (ATCC, Cat. HTB-55), and VeroE6-TMPRSS2 (CellBank Australia, Cat. JCRB1819) cells were cultured at 37 C and 5% CO 2. Vero cell media: minimum essential medium (MEM; Media Preparation Unit, Peter Doherty Institute) supplemented with 5% fetal bovine serum (FBS; Bovogen, Cat. SFBS), 50 U/mL penicillin and 50 mg/mL streptomycin (PenStrep, Thermo Fisher Scientific, Cat. 15070-063), 2 mM GlutaMAX (Thermo Fisher Scientific, Cat. 35050061), and 15 mM HEPES (Thermo Fisher Scientific, Cat. 15630130) . Vero hSLAM cell media: MEM supplemented with 7% FBS, PenStrep, 2 mM GlutaMAX, 15 mM HEPES, and 0.4 mg/mL G418 Sulfate (Gibco, Cat. 10131027). Calu-3 cell media: MEM containing L-glutamine and sodium bicarbonate (Sigma, Cat. M4655) supplemented with 10% FBS, PenStrep, 13 non-essential amino acids (Gibco, Cat. 11140050), and sodium pyruvate (Fisher Scientific, Cat. BP356-100). VeroE6-TMPRSS2 cell media: Dulbecco's MEM (DMEM; Media Preparation Unit, Peter Doherty Institute) supplemented with 10% FBS, PenStrep, 2 mM GlutaMAX, and 1 mg/ mL G418 Sulfate. (Hou et al., 2020) . SARS-CoV-2 VIC01 was propagated in Vero and Vero hSLAM cells in Vero infection..
References
Anderson, Kaplan, Bell, Koutsis, Haynes et al., NKX2-5 regulates human cardiomyogenesis via a HEY2 dependent transcriptional network, Nat. Commun, doi:10.1038/s41467-018-03714-x
Bailey, Dmytrenko, Greenberg, Bredemeyer, Ma et al., SARS-CoV-2 infects human engineered heart tissues and models COVID-19 myocarditis, JACC Basic Transl Sci, doi:10.1016/j.jacbts.2021.01.002
Bojkova, Wagner, Shumliakivska, Aslan, Saleem et al., SARS-CoV-2 infects and induces cytotoxic effects in human cardiomyocytes, Cardiovasc. Res, doi:10.1093/cvr/cvaa267
Bouhaddou, Memon, Meyer, White, Rezelj et al., The global phosphorylation landscape of SARS-CoV-2 infection, Cell, doi:10.1016/j.cell.2020.06.034
Chen, Bobrovitz, Premji, Koopmans, Fisman et al., SARS-CoV-2 shedding dynamics across the respiratory tract, sex, and disease severity for adult and pediatric COVID-19, Elife, doi:10.7554/eLife.70458
Chen, Gao, Wang, Wei, An iTSCderived placental model of SARS-CoV-2 infection reveals ACE2-dependent susceptibility in syncytiotrophoblasts, bioRxiv, doi:10.1101/2021.10.27.465224
Deinhardt-Emmer, Wittschieber, Sanft, Kleemann, Elschner et al., Early postmortem mapping of SARS-CoV-2 RNA in patients with COVID-19 and the correlation with tissue damage, Elife, doi:10.7554/eLife.60361
Dobin, Davis, Schlesinger, Drenkow, Zaleski et al., STAR: ultrafast universal RNA-seq aligner, Bioinformatics, doi:10.1093/bioinformatics/bts635
Elliott, Braam, Koutsis, Ng, Jenny et al., NKX2-5(eGFP/w) hESCs for isolation of human cardiac progenitors and cardiomyocytes, Nat. Methods, doi:10.1038/nmeth.1740
Goyal, Choi, Pinheiro, Schenck, Chen et al., Clinical characteristics of Covid-19 in New York City, N. Engl. J. Med, doi:10.1056/NEJMc2010419
Gunst, Staerke, Pahus, Kristensen, Bodilsen et al., Efficacy of the TMPRSS2 inhibitor camostat mesilate in patients hospitalized with Covid-19-a double-blind randomized controlled trial, EClinicalMedicine, doi:10.1016/j.eclinm.2021.100849
Hamming, Timens, Bulthuis, Lely, Navis et al., Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis, J. Pathol, doi:10.1002/path.1570
Hoffmann, Kleine-Weber, Schroeder, Kru ¨ger, Herrler et al., SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor, Cell, doi:10.1016/j.cell.2020.05.042
Howe, Achuthan, Allen, Allen, Alvarez-Jarreta et al., Ensembl 2021, Nucleic Acids Res, doi:10.1093/nar/gkaa942
Huang, Hume, Abo, Werder, Villacorta-Martin et al., SARS-CoV-2 infection of pluripotent stem cell-derived human lung alveolar type 2 cells elicits a rapid epithelial-intrinsic inflammatory response, Cell Stem Cell, doi:10.1016/j.stem.2020.09.013
Humphrey, Karayel, James, Mann, High-throughput and high-sensitivity phosphoproteomics with the EasyPhos platform, Nat. Protoc, doi:10.1038/s41596-018-0014-9
Jacob, Morley, Hawkins, Mccauley, Jean et al., Differentiation of human pluripotent stem cells into functional lung alveolar epithelial cells, Cell Stem Cell, doi:10.1016/j.stem.2017.08.014
Katsura, Sontake, Tata, Kobayashi, Edwards et al., Human lung stem cell-based alveolospheres provide insights into SARS-CoV-2-mediated interferon responses and pneumocyte dysfunction, Cell Stem Cell, doi:10.1016/j.stem.2020.10.005
Lazzerini, Laghi-Pasini, Boutjdir, Capecchi, Inflammatory cytokines and cardiac arrhythmias: the lesson from COVID-19, Nat. Rev. Immunol, doi:10.1038/s41577-022-00714-3
Lee, Huang, Rastegari, Rengganaten, Liu et al., Tumor necrosis factor-alpha exacerbates viral entry in SARS-CoV2-infected iPSC-derived cardiomyocytes, Int. J. Mol. Sci, doi:10.3390/ijms22189869
Lei, Dong, Ma, Wang, Xiao et al., Activation and evasion of type I interferon responses by SARS-CoV-2, Nat. Commun, doi:10.1038/s41467-020-17665-9
Li, Renner, Comar, Whelan, Reyes et al., SARS-CoV-2 induces double-stranded RNAmediated innate immune responses in respiratory epithelialderived cells and cardiomyocytes, doi:10.1073/pnas.2022643118
Liao, Smyth, Shi, featureCounts: an efficient general purpose program for assigning sequence reads to genomic features, Bioinformatics, doi:10.1093/bioinformatics/btt656
Lopes, Garcia-Herna ´ndez, Lorenzini, Futema, Chumakova et al., Alpha-protein kinase 3 (ALPK3) truncating variants are a cause of autosomal dominant hypertrophic cardiomyopathy, Eur. Heart J, doi:10.1093/eurheartj/ehab424
Marchiano, Hsiang, Khanna, Higashi, Whitmore et al., SARS-CoV-2 infects human pluripotent stem cellderived cardiomyocytes, impairing electrical and mechanical function, Stem Cell Rep, doi:10.1016/j.stemcr.2021.02.008
Mills, Titmarsh, Koenig, Parker, Ryall et al., Functional screening in human cardiac organoids reveals a metabolic mechanism for cardiomyocyte cell cycle arrest, Proc. Natl. Acad. Sci. USA, doi:10.1073/pnas.1707316114
Montaser, Lalmanach, Mach, CA-074, but not its methyl ester CA-074Me, is a selective inhibitor of cathepsin B within living cells, Biol. Chem, doi:10.1515/BC.2002.147
Mulay, Konda, Garcia, Jr, Yao et al., SARS-CoV-2 infection of primary human lung epithelium for COVID-19 modeling and drug discovery, Cell Rep, doi:10.1016/j.celrep.2021.109055
Muus, Luecken, Eraslan, Sikkema, Waghray et al., Single-cell meta-analysis of SARS-CoV-2 entry genes across tissues and demographics, Nat. Med, doi:10.1038/s41591-020-01227-z
Nalbandian, Sehgal, Gupta, Madhavan, Mcgroder et al., Post-acute COVID-19 syndrome, Nat. Med, doi:10.1038/s41591-021-01283-z
Navaratnarajah, Pease, Halfmann, Taye, Barkhymer et al., Highly efficient SARS-CoV-2 infection of human cardiomyocytes: spike protein-mediated cell fusion and its inhibition, J. Virol, doi:10.1128/JVI.01368-21
Ou, Liu, Lei, Li, Mi et al., Characterization of spike glycoprotein of SARS-CoV-2 on virus entry and its immune cross-reactivity with SARS-CoV, Nat. Commun, doi:10.1038/s41467-020-15562-9
Perez-Bermejo, Kang, Rockwood, Simoneau, Joy et al., SARS-CoV-2 infection of human iPSC-derived cardiac cells reflects cytopathic features in hearts of patients with COVID-19, Sci. Transl. Med, doi:10.1126/scitranslmed.abf7872
Phelan, Anderson, Howden, Wong, Hickey et al., ALPK3-deficient cardiomyocytes generated from patientderived induced pluripotent stem cells and mutant human embryonic stem cells display abnormal calcium handling and establish that ALPK3 deficiency underlies familial cardiomyopathy, Eur. Heart J, doi:10.1093/eurheartj/ehw160
Pruijssers, George, Scha ¨fer, Leist, Gralinksi et al., Remdesivir inhibits SARS-CoV-2 in human lung cells and chimeric SARS-CoV expressing the SARS-CoV-2 RNA polymerase in mice, Cell Rep, doi:10.1016/j.celrep.2020.107940
Puntmann, Carerj, Wieters, Fahim, Arendt et al., Outcomes of cardiovascular magnetic resonance imaging in patients recently recovered from coronavirus disease 2019 (COVID-19), JAMA Cardiol, doi:10.1001/jamacardio.2020.3557
Qi, Qian, Zhang, Zhang, Single cell RNA sequencing of 13 human tissues identify cell types and receptors of human coronaviruses, Biochem. Biophys. Res. Commun, doi:10.1016/j.bbrc.2020.03.044
Robinson, Alkass, Bergmann, Maguire, Roderick et al., Genes encoding ACE2, TMPRSS2 and related proteins mediating SARS-CoV-2 viral entry are upregulated with age in human cardiomyocytes, J. Mol. Cell. Cardiol, doi:10.1016/j.yjmcc.2020.08.009
Robinson, Mccarthy, Smyth, edgeR: a Bioconductor package for differential expression analysis of digital gene expression data, Bioinformatics, doi:10.1093/bioinformatics/btp616
Sampaio, Chauveau, Hertzog, Bridgeman, Fowler et al., The RNA sensor MDA5 detects SARS-CoV-2 infection, Sci. Rep, doi:10.1038/s41598-021-92940-3
Schneider, Pease, Navaratnarajah, Halfmann, Clemens et al., SARS-CoV-2 direct cardiac damage through spike-mediated cardiomyocyte fusion
Shang, Wan, Luo, Ye, Geng et al., Cell entry mechanisms of SARS-CoV-2, Proc. Natl. Acad. Stem Cell Reports j
Shao, Shang, Luo, Shi, Zhao et al., Myocardial injury is associated with higher mortality in patients
Sharma, Garcia, Jr, Wang, Plummer et al., Human iPSCderived cardiomyocytes are susceptible to SARS-CoV-2 infection, Cell Rep. Med, doi:10.1016/j.xcrm.2020.100052
Shemesh, Aktepe, Deerain, Mcauley, Audsley et al., SARS-CoV-2 suppresses IFNbeta production mediated by NSP1, 5, 6, 15, ORF6 and ORF7b but does not suppress the effects of added interferon, PLoS Pathog, doi:10.1371/journal.ppat.1009800
Shi, Qin, Shen, Cai, Liu et al., Association of cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan, JAMA Cardiol, doi:10.1001/jamacardio.2020.0950
Sungnak, Huang, Be ´cavin, Berg, Queen et al., SARS-CoV-2 entry factors are highly expressed in nasal epithelial cells together with innate immune genes, Nat. Med, doi:10.1038/s41591-020-0868-6
Tiwari, Wang, Smith, Carlin, Revealing tissue-specific SARS-CoV-2 infection and host responses using human stem cell-derived lung and cerebral organoids, Stem Cell Rep, doi:10.1016/j.stemcr.2021.02.005
Tohyama, Hattori, Sano, Hishiki, Nagahata et al., Distinct metabolic flow enables large-scale purification of mouse and human pluripotent stem cell-derived cardiomyocytes, Cell Stem Cell, doi:10.1016/j.stem.2012.09.013
Uhle ´n, Fagerberg, Hallstro ¨m, Lindskog, Oksvold et al., Proteomics. Tissue-based map of the human proteome, Science, doi:10.1126/science.1260419
Wang, Mannan, Xiao, Abdulfatah, Qiao et al., Characterization of SARS-CoV-2 and host entry factors distribution in a COVID-19 autopsy series, Commun. Med. 1, doi:10.1038/s43856-021-00025-z
Williams, Colzani, Macrae, Robinson, Bloor et al., Human embryonic stem cell-derived cardiomyocyte platform screens inhibitors of SARS-CoV-2 infection, Commun. Biol, doi:10.1038/s42003-021-02453-y
Xia, Cao, Xie, Zhang, Chen et al., Evasion of type I interferon by SARS-CoV-2, Cell Rep, doi:10.1016/j.celrep.2020.108234
Yang, Chen, Zhou, Mediators of SARS-CoV-2 entry are preferentially enriched in cardiomyocytes, Hereditas, doi:10.1186/s41065-020-00168-4
Yaron, Heaton, Levy, Johnson, Jordan et al., The FDA-approved drug Alectinib compromises SARS-CoV-2 nucleocapsid phosphorylation and inhibits viral infection in vitro, bioRxiv, doi:10.1101/2020.08.14.251207
Youk, Kim, Evans, Jeong, Hur et al., Three-dimensional human alveolar stem cell culture models reveal infection response to SARS-CoV-2, Cell Stem Cell, doi:10.1016/j.stem.2020.10.004
Zhang, Bastard, Liu, Le Pen, Moncada-Velez et al., Inborn errors of type I IFN immunity in patients with life-threatening COVID-19, Science, doi:10.1126/science.abd4570
Zhou, Yang, Wang, Hu, Zhang et al., Addendum: a pneumonia outbreak associated with a new coronavirus of probable bat origin, Nature, doi:10.1038/s41586-020-2951-z
Zhou, Zhou, Pache, Chang, Khodabakhshi et al., Metascape provides a biologist-oriented resource for the analysis of systems-level datasets, Nat. Commun, doi:10.1038/s41467-019-09234-6
Zou, Chen, Zou, Han, Hao et al., Single-cell RNA-seq data analysis on the receptor ACE2 expression reveals the potential risk of different human organs vulnerable to 2019-nCoV infection, Front. Med, doi:10.1007/s11684-020-0754-0
DOI record:
{
"DOI": "10.1016/j.stemcr.2023.05.007",
"ISSN": [
"2213-6711"
],
"URL": "http://dx.doi.org/10.1016/j.stemcr.2023.05.007",
"alternative-id": [
"S2213671123001856"
],
"assertion": [
{
"label": "This article is maintained by",
"name": "publisher",
"value": "Elsevier"
},
{
"label": "Article Title",
"name": "articletitle",
"value": "Parallel use of human stem cell lung and heart models provide insights for SARS-CoV-2 treatment"
},
{
"label": "Journal Title",
"name": "journaltitle",
"value": "Stem Cell Reports"
},
{
"label": "CrossRef DOI link to publisher maintained version",
"name": "articlelink",
"value": "https://doi.org/10.1016/j.stemcr.2023.05.007"
},
{
"label": "Content Type",
"name": "content_type",
"value": "article"
},
{
"label": "Copyright",
"name": "copyright",
"value": "© 2023 The Authors."
}
],
"author": [
{
"affiliation": [],
"family": "Rudraraju",
"given": "Rajeev",
"sequence": "first"
},
{
"affiliation": [],
"family": "Gartner",
"given": "Matthew J.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Neil",
"given": "Jessica A.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Stout",
"given": "Elizabeth S.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Chen",
"given": "Joseph",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Needham",
"given": "Elise J.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "See",
"given": "Michael",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Mackenzie-Kludas",
"given": "Charley",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Yang Lee",
"given": "Leo Yi",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Wang",
"given": "Mingyang",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Pointer",
"given": "Hayley",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Karavendzas",
"given": "Kathy",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Abu-Bonsrah",
"given": "Dad",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Drew",
"given": "Damien",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Yang Sun",
"given": "Yu Bo",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Tan",
"given": "Jia Ping",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Sun",
"given": "Guizhi",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Salavaty",
"given": "Abbas",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Charitakis",
"given": "Natalie",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Nim",
"given": "Hieu T.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Currie",
"given": "Peter D.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Tham",
"given": "Wai-Hong",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Porrello",
"given": "Enzo",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Polo",
"given": "Jose M.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Humphrey",
"given": "Sean J.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ramialison",
"given": "Mirana",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-1052-7407",
"affiliation": [],
"authenticated-orcid": false,
"family": "Elliott",
"given": "David A.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Subbarao",
"given": "Kanta",
"sequence": "additional"
}
],
"container-title": "Stem Cell Reports",
"container-title-short": "Stem Cell Reports",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"cell.com",
"elsevier.com",
"sciencedirect.com"
]
},
"created": {
"date-parts": [
[
2023,
6,
13
]
],
"date-time": "2023-06-13T14:50:01Z",
"timestamp": 1686667801000
},
"deposited": {
"date-parts": [
[
2023,
6,
16
]
],
"date-time": "2023-06-16T21:43:53Z",
"timestamp": 1686951833000
},
"indexed": {
"date-parts": [
[
2023,
6,
17
]
],
"date-time": "2023-06-17T04:22:28Z",
"timestamp": 1686975748920
},
"is-referenced-by-count": 0,
"issue": "6",
"issued": {
"date-parts": [
[
2023,
6
]
]
},
"journal-issue": {
"issue": "6",
"published-print": {
"date-parts": [
[
2023,
6
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://www.elsevier.com/tdm/userlicense/1.0/",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
6,
1
]
],
"date-time": "2023-06-01T00:00:00Z",
"timestamp": 1685577600000
}
},
{
"URL": "http://creativecommons.org/licenses/by-nc-nd/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
5,
11
]
],
"date-time": "2023-05-11T00:00:00Z",
"timestamp": 1683763200000
}
}
],
"link": [
{
"URL": "https://api.elsevier.com/content/article/PII:S2213671123001856?httpAccept=text/xml",
"content-type": "text/xml",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://api.elsevier.com/content/article/PII:S2213671123001856?httpAccept=text/plain",
"content-type": "text/plain",
"content-version": "vor",
"intended-application": "text-mining"
}
],
"member": "78",
"original-title": [],
"page": "1308-1324",
"prefix": "10.1016",
"published": {
"date-parts": [
[
2023,
6
]
]
},
"published-print": {
"date-parts": [
[
2023,
6
]
]
},
"publisher": "Elsevier BV",
"reference": [
{
"DOI": "10.1038/s41467-018-03714-x",
"article-title": "NKX2-5 regulates human cardiomyogenesis via a HEY2 dependent transcriptional network",
"author": "Anderson",
"doi-asserted-by": "crossref",
"first-page": "1373",
"journal-title": "Nat. Commun.",
"key": "10.1016/j.stemcr.2023.05.007_bib1",
"volume": "9",
"year": "2018"
},
{
"DOI": "10.1016/j.jacbts.2021.01.002",
"article-title": "SARS-CoV-2 infects human engineered heart tissues and models COVID-19 myocarditis",
"author": "Bailey",
"doi-asserted-by": "crossref",
"first-page": "331",
"journal-title": "JACC Basic Transl Sci",
"key": "10.1016/j.stemcr.2023.05.007_bib2",
"volume": "6",
"year": "2021"
},
{
"DOI": "10.1093/cvr/cvaa267",
"article-title": "SARS-CoV-2 infects and induces cytotoxic effects in human cardiomyocytes",
"author": "Bojkova",
"doi-asserted-by": "crossref",
"first-page": "2207",
"journal-title": "Cardiovasc. Res.",
"key": "10.1016/j.stemcr.2023.05.007_bib3",
"volume": "116",
"year": "2020"
},
{
"DOI": "10.1016/j.cell.2020.06.034",
"article-title": "The global phosphorylation landscape of SARS-CoV-2 infection",
"author": "Bouhaddou",
"doi-asserted-by": "crossref",
"first-page": "685",
"journal-title": "Cell",
"key": "10.1016/j.stemcr.2023.05.007_bib4",
"volume": "182",
"year": "2020"
},
{
"article-title": "An iTSC-derived placental model of SARS-CoV-2 infection reveals ACE2-dependent susceptibility in syncytiotrophoblasts",
"author": "Chen",
"journal-title": "bioRxiv",
"key": "10.1016/j.stemcr.2023.05.007_bib5",
"year": "2021"
},
{
"DOI": "10.7554/eLife.70458",
"article-title": "SARS-CoV-2 shedding dynamics across the respiratory tract, sex, and disease severity for adult and pediatric COVID-19",
"author": "Chen",
"doi-asserted-by": "crossref",
"first-page": "e70458",
"journal-title": "Elife",
"key": "10.1016/j.stemcr.2023.05.007_bib6",
"volume": "10",
"year": "2021"
},
{
"DOI": "10.7554/eLife.60361",
"article-title": "Early postmortem mapping of SARS-CoV-2 RNA in patients with COVID-19 and the correlation with tissue damage",
"author": "Deinhardt-Emmer",
"doi-asserted-by": "crossref",
"first-page": "e60361",
"journal-title": "Elife",
"key": "10.1016/j.stemcr.2023.05.007_bib7",
"volume": "10",
"year": "2021"
},
{
"DOI": "10.1093/bioinformatics/bts635",
"article-title": "STAR: ultrafast universal RNA-seq aligner",
"author": "Dobin",
"doi-asserted-by": "crossref",
"first-page": "15",
"journal-title": "Bioinformatics",
"key": "10.1016/j.stemcr.2023.05.007_bib8",
"volume": "29",
"year": "2013"
},
{
"DOI": "10.1038/nmeth.1740",
"article-title": "NKX2-5(eGFP/w) hESCs for isolation of human cardiac progenitors and cardiomyocytes",
"author": "Elliott",
"doi-asserted-by": "crossref",
"first-page": "1037",
"journal-title": "Nat. Methods",
"key": "10.1016/j.stemcr.2023.05.007_bib9",
"volume": "8",
"year": "2011"
},
{
"DOI": "10.1056/NEJMc2010419",
"article-title": "Clinical characteristics of Covid-19 in New York City",
"author": "Goyal",
"doi-asserted-by": "crossref",
"first-page": "2372",
"journal-title": "N. Engl. J. Med.",
"key": "10.1016/j.stemcr.2023.05.007_bib10",
"volume": "382",
"year": "2020"
},
{
"DOI": "10.1016/j.eclinm.2021.100849",
"article-title": "Efficacy of the TMPRSS2 inhibitor camostat mesilate in patients hospitalized with Covid-19-a double-blind randomized controlled trial",
"author": "Gunst",
"doi-asserted-by": "crossref",
"first-page": "100849",
"journal-title": "EClinicalMedicine",
"key": "10.1016/j.stemcr.2023.05.007_bib11",
"volume": "35",
"year": "2021"
},
{
"DOI": "10.1002/path.1570",
"article-title": "Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis",
"author": "Hamming",
"doi-asserted-by": "crossref",
"first-page": "631",
"journal-title": "J. Pathol.",
"key": "10.1016/j.stemcr.2023.05.007_bib12",
"volume": "203",
"year": "2004"
},
{
"DOI": "10.1016/j.cell.2020.02.052",
"article-title": "SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor",
"author": "Hoffmann",
"doi-asserted-by": "crossref",
"first-page": "271",
"journal-title": "Cell",
"key": "10.1016/j.stemcr.2023.05.007_bib13",
"volume": "181",
"year": "2020"
},
{
"DOI": "10.1016/j.cell.2020.05.042",
"article-title": "SARS-CoV-2 reverse genetics reveals a variable infection gradient in the respiratory tract",
"author": "Hou",
"doi-asserted-by": "crossref",
"first-page": "429",
"journal-title": "Cell",
"key": "10.1016/j.stemcr.2023.05.007_bib14",
"volume": "182",
"year": "2020"
},
{
"DOI": "10.1093/nar/gkaa942",
"article-title": "Ensembl 2021",
"author": "Howe",
"doi-asserted-by": "crossref",
"first-page": "D884",
"journal-title": "Nucleic Acids Res.",
"key": "10.1016/j.stemcr.2023.05.007_bib15",
"volume": "49",
"year": "2021"
},
{
"DOI": "10.1016/j.stem.2020.09.013",
"article-title": "SARS-CoV-2 infection of pluripotent stem cell-derived human lung alveolar type 2 cells elicits a rapid epithelial-intrinsic inflammatory response",
"author": "Huang",
"doi-asserted-by": "crossref",
"first-page": "962",
"journal-title": "Cell Stem Cell",
"key": "10.1016/j.stemcr.2023.05.007_bib16",
"volume": "27",
"year": "2020"
},
{
"DOI": "10.1038/s41596-018-0014-9",
"article-title": "High-throughput and high-sensitivity phosphoproteomics with the EasyPhos platform",
"author": "Humphrey",
"doi-asserted-by": "crossref",
"first-page": "1897",
"journal-title": "Nat. Protoc.",
"key": "10.1016/j.stemcr.2023.05.007_bib17",
"volume": "13",
"year": "2018"
},
{
"DOI": "10.1016/j.stem.2017.08.014",
"article-title": "Differentiation of human pluripotent stem cells into functional lung alveolar epithelial cells",
"author": "Jacob",
"doi-asserted-by": "crossref",
"first-page": "472",
"journal-title": "Cell Stem Cell",
"key": "10.1016/j.stemcr.2023.05.007_bib18",
"volume": "21",
"year": "2017"
},
{
"DOI": "10.1016/j.stem.2020.10.005",
"article-title": "Human lung stem cell-based alveolospheres provide insights into SARS-CoV-2-mediated interferon responses and pneumocyte dysfunction",
"author": "Katsura",
"doi-asserted-by": "crossref",
"first-page": "890",
"journal-title": "Cell Stem Cell",
"key": "10.1016/j.stemcr.2023.05.007_bib19",
"volume": "27",
"year": "2020"
},
{
"DOI": "10.1038/s41577-022-00714-3",
"article-title": "Inflammatory cytokines and cardiac arrhythmias: the lesson from COVID-19",
"author": "Lazzerini",
"doi-asserted-by": "crossref",
"first-page": "270",
"journal-title": "Nat. Rev. Immunol.",
"key": "10.1016/j.stemcr.2023.05.007_bib20",
"volume": "22",
"year": "2022"
},
{
"DOI": "10.3390/ijms22189869",
"article-title": "Tumor necrosis factor-alpha exacerbates viral entry in SARS-CoV2-infected iPSC-derived cardiomyocytes",
"author": "Lee",
"doi-asserted-by": "crossref",
"first-page": "9869",
"journal-title": "Int. J. Mol. Sci.",
"key": "10.1016/j.stemcr.2023.05.007_bib21",
"volume": "22",
"year": "2021"
},
{
"DOI": "10.1038/s41467-020-17665-9",
"article-title": "Activation and evasion of type I interferon responses by SARS-CoV-2",
"author": "Lei",
"doi-asserted-by": "crossref",
"first-page": "3810",
"journal-title": "Nat. Commun.",
"key": "10.1016/j.stemcr.2023.05.007_bib22",
"volume": "11",
"year": "2020"
},
{
"article-title": "SARS-CoV-2 induces double-stranded RNA-mediated innate immune responses in respiratory epithelial-derived cells and cardiomyocytes",
"author": "Li",
"journal-title": "Proc. Natl. Acad. Sci. USA",
"key": "10.1016/j.stemcr.2023.05.007_bib23",
"volume": "118",
"year": "2021"
},
{
"DOI": "10.1093/bioinformatics/btt656",
"article-title": "featureCounts: an efficient general purpose program for assigning sequence reads to genomic features",
"author": "Liao",
"doi-asserted-by": "crossref",
"first-page": "923",
"journal-title": "Bioinformatics",
"key": "10.1016/j.stemcr.2023.05.007_bib24",
"volume": "30",
"year": "2014"
},
{
"DOI": "10.1093/eurheartj/ehab424",
"article-title": "Alpha-protein kinase 3 (ALPK3) truncating variants are a cause of autosomal dominant hypertrophic cardiomyopathy",
"author": "Lopes",
"doi-asserted-by": "crossref",
"first-page": "3063",
"journal-title": "Eur. Heart J.",
"key": "10.1016/j.stemcr.2023.05.007_bib25",
"volume": "42",
"year": "2021"
},
{
"DOI": "10.1016/j.stemcr.2021.02.008",
"article-title": "SARS-CoV-2 infects human pluripotent stem cell-derived cardiomyocytes, impairing electrical and mechanical function",
"author": "Marchiano",
"doi-asserted-by": "crossref",
"first-page": "478",
"journal-title": "Stem Cell Rep.",
"key": "10.1016/j.stemcr.2023.05.007_bib26",
"volume": "16",
"year": "2021"
},
{
"DOI": "10.1073/pnas.1707316114",
"article-title": "Functional screening in human cardiac organoids reveals a metabolic mechanism for cardiomyocyte cell cycle arrest",
"author": "Mills",
"doi-asserted-by": "crossref",
"first-page": "E8372",
"journal-title": "Proc. Natl. Acad. Sci. USA",
"key": "10.1016/j.stemcr.2023.05.007_bib27",
"volume": "114",
"year": "2017"
},
{
"DOI": "10.1515/BC.2002.147",
"article-title": "CA-074, but not its methyl ester CA-074Me, is a selective inhibitor of cathepsin B within living cells",
"author": "Montaser",
"doi-asserted-by": "crossref",
"first-page": "1305",
"journal-title": "Biol. Chem.",
"key": "10.1016/j.stemcr.2023.05.007_bib28",
"volume": "383",
"year": "2002"
},
{
"DOI": "10.1016/j.celrep.2021.109055",
"article-title": "SARS-CoV-2 infection of primary human lung epithelium for COVID-19 modeling and drug discovery",
"author": "Mulay",
"doi-asserted-by": "crossref",
"first-page": "109055",
"journal-title": "Cell Rep.",
"key": "10.1016/j.stemcr.2023.05.007_bib29",
"volume": "35",
"year": "2021"
},
{
"DOI": "10.1038/s41591-020-01227-z",
"article-title": "Single-cell meta-analysis of SARS-CoV-2 entry genes across tissues and demographics",
"author": "Muus",
"doi-asserted-by": "crossref",
"first-page": "546",
"journal-title": "Nat. Med.",
"key": "10.1016/j.stemcr.2023.05.007_bib30",
"volume": "27",
"year": "2021"
},
{
"DOI": "10.1038/s41591-021-01283-z",
"article-title": "Post-acute COVID-19 syndrome",
"author": "Nalbandian",
"doi-asserted-by": "crossref",
"first-page": "601",
"journal-title": "Nat. Med.",
"key": "10.1016/j.stemcr.2023.05.007_bib31",
"volume": "27",
"year": "2021"
},
{
"DOI": "10.1128/JVI.01368-21",
"article-title": "Highly efficient SARS-CoV-2 infection of human cardiomyocytes: spike protein-mediated cell fusion and its inhibition",
"author": "Navaratnarajah",
"doi-asserted-by": "crossref",
"first-page": "e0136821",
"journal-title": "J. Virol.",
"key": "10.1016/j.stemcr.2023.05.007_bib32",
"volume": "95",
"year": "2021"
},
{
"DOI": "10.1038/s41467-020-15562-9",
"article-title": "Characterization of spike glycoprotein of SARS-CoV-2 on virus entry and its immune cross-reactivity with SARS-CoV",
"author": "Ou",
"doi-asserted-by": "crossref",
"first-page": "1620",
"journal-title": "Nat. Commun.",
"key": "10.1016/j.stemcr.2023.05.007_bib33",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.1126/scitranslmed.abf7872",
"article-title": "SARS-CoV-2 infection of human iPSC-derived cardiac cells reflects cytopathic features in hearts of patients with COVID-19",
"author": "Perez-Bermejo",
"doi-asserted-by": "crossref",
"first-page": "eabf7872",
"journal-title": "Sci. Transl. Med.",
"key": "10.1016/j.stemcr.2023.05.007_bib34",
"volume": "13",
"year": "2021"
},
{
"DOI": "10.1093/eurheartj/ehw160",
"article-title": "ALPK3-deficient cardiomyocytes generated from patient-derived induced pluripotent stem cells and mutant human embryonic stem cells display abnormal calcium handling and establish that ALPK3 deficiency underlies familial cardiomyopathy",
"author": "Phelan",
"doi-asserted-by": "crossref",
"first-page": "2586",
"journal-title": "Eur. Heart J.",
"key": "10.1016/j.stemcr.2023.05.007_bib35",
"volume": "37",
"year": "2016"
},
{
"DOI": "10.1016/j.celrep.2020.107940",
"article-title": "Remdesivir inhibits SARS-CoV-2 in human lung cells and chimeric SARS-CoV expressing the SARS-CoV-2 RNA polymerase in mice",
"author": "Pruijssers",
"doi-asserted-by": "crossref",
"first-page": "107940",
"journal-title": "Cell Rep.",
"key": "10.1016/j.stemcr.2023.05.007_bib36",
"volume": "32",
"year": "2020"
},
{
"DOI": "10.1001/jamacardio.2020.3557",
"article-title": "Outcomes of cardiovascular magnetic resonance imaging in patients recently recovered from coronavirus disease 2019 (COVID-19)",
"author": "Puntmann",
"doi-asserted-by": "crossref",
"first-page": "1265",
"journal-title": "JAMA Cardiol.",
"key": "10.1016/j.stemcr.2023.05.007_bib37",
"volume": "5",
"year": "2020"
},
{
"DOI": "10.1016/j.bbrc.2020.03.044",
"article-title": "Single cell RNA sequencing of 13 human tissues identify cell types and receptors of human coronaviruses",
"author": "Qi",
"doi-asserted-by": "crossref",
"first-page": "135",
"journal-title": "Biochem. Biophys. Res. Commun.",
"key": "10.1016/j.stemcr.2023.05.007_bib38",
"volume": "526",
"year": "2020"
},
{
"DOI": "10.1016/j.yjmcc.2020.08.009",
"article-title": "Genes encoding ACE2, TMPRSS2 and related proteins mediating SARS-CoV-2 viral entry are upregulated with age in human cardiomyocytes",
"author": "Robinson",
"doi-asserted-by": "crossref",
"first-page": "88",
"journal-title": "J. Mol. Cell. Cardiol.",
"key": "10.1016/j.stemcr.2023.05.007_bib39",
"volume": "147",
"year": "2020"
},
{
"DOI": "10.1093/bioinformatics/btp616",
"article-title": "edgeR: a Bioconductor package for differential expression analysis of digital gene expression data",
"author": "Robinson",
"doi-asserted-by": "crossref",
"first-page": "139",
"journal-title": "Bioinformatics",
"key": "10.1016/j.stemcr.2023.05.007_bib40",
"volume": "26",
"year": "2010"
},
{
"DOI": "10.1038/s41598-021-92940-3",
"article-title": "The RNA sensor MDA5 detects SARS-CoV-2 infection",
"author": "Sampaio",
"doi-asserted-by": "crossref",
"first-page": "13638",
"journal-title": "Sci. Rep.",
"key": "10.1016/j.stemcr.2023.05.007_bib41",
"volume": "11",
"year": "2021"
},
{
"article-title": "SARS-CoV-2 direct cardiac damage through spike-mediated cardiomyocyte fusion",
"author": "Schneider",
"journal-title": "Research Square",
"key": "10.1016/j.stemcr.2023.05.007_bib42",
"year": "2020"
},
{
"DOI": "10.1073/pnas.2003138117",
"article-title": "Cell entry mechanisms of SARS-CoV-2",
"author": "Shang",
"doi-asserted-by": "crossref",
"first-page": "11727",
"journal-title": "Proc. Natl. Acad. Sci. USA",
"key": "10.1016/j.stemcr.2023.05.007_bib43",
"volume": "117",
"year": "2020"
},
{
"article-title": "Myocardial injury is associated with higher mortality in patients with coronavirus disease 2019: a meta-analysis",
"author": "Shao",
"first-page": "224",
"journal-title": "J. Geriatr. Cardiol.",
"key": "10.1016/j.stemcr.2023.05.007_bib44",
"volume": "17",
"year": "2020"
},
{
"DOI": "10.1016/j.xcrm.2020.100052",
"article-title": "Human iPSC-derived cardiomyocytes are susceptible to SARS-CoV-2 infection",
"author": "Sharma",
"doi-asserted-by": "crossref",
"first-page": "100052",
"journal-title": "Cell Rep. Med.",
"key": "10.1016/j.stemcr.2023.05.007_bib45",
"volume": "1",
"year": "2020"
},
{
"DOI": "10.1371/journal.ppat.1009800",
"article-title": "SARS-CoV-2 suppresses IFNbeta production mediated by NSP1, 5, 6, 15, ORF6 and ORF7b but does not suppress the effects of added interferon",
"author": "Shemesh",
"doi-asserted-by": "crossref",
"first-page": "e1009800",
"journal-title": "PLoS Pathog.",
"key": "10.1016/j.stemcr.2023.05.007_bib46",
"volume": "17",
"year": "2021"
},
{
"DOI": "10.1001/jamacardio.2020.0950",
"article-title": "Association of cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan, China",
"author": "Shi",
"doi-asserted-by": "crossref",
"first-page": "802",
"journal-title": "JAMA Cardiol.",
"key": "10.1016/j.stemcr.2023.05.007_bib47",
"volume": "5",
"year": "2020"
},
{
"DOI": "10.1038/s41591-020-0868-6",
"article-title": "SARS-CoV-2 entry factors are highly expressed in nasal epithelial cells together with innate immune genes",
"author": "Sungnak",
"doi-asserted-by": "crossref",
"first-page": "681",
"journal-title": "Nat. Med.",
"key": "10.1016/j.stemcr.2023.05.007_bib48",
"volume": "26",
"year": "2020"
},
{
"DOI": "10.1016/j.stemcr.2021.02.005",
"article-title": "Revealing tissue-specific SARS-CoV-2 infection and host responses using human stem cell-derived lung and cerebral organoids",
"author": "Tiwari",
"doi-asserted-by": "crossref",
"first-page": "437",
"journal-title": "Stem Cell Rep.",
"key": "10.1016/j.stemcr.2023.05.007_bib49",
"volume": "16",
"year": "2021"
},
{
"DOI": "10.1016/j.stem.2012.09.013",
"article-title": "Distinct metabolic flow enables large-scale purification of mouse and human pluripotent stem cell-derived cardiomyocytes",
"author": "Tohyama",
"doi-asserted-by": "crossref",
"first-page": "127",
"journal-title": "Cell Stem Cell",
"key": "10.1016/j.stemcr.2023.05.007_bib50",
"volume": "12",
"year": "2013"
},
{
"DOI": "10.1126/science.1260419",
"article-title": "Proteomics. Tissue-based map of the human proteome",
"author": "Uhlén",
"doi-asserted-by": "crossref",
"first-page": "1260419",
"journal-title": "Science",
"key": "10.1016/j.stemcr.2023.05.007_bib51",
"volume": "347",
"year": "2015"
},
{
"DOI": "10.1038/s43856-021-00025-z",
"article-title": "Characterization of SARS-CoV-2 and host entry factors distribution in a COVID-19 autopsy series",
"author": "Wang",
"doi-asserted-by": "crossref",
"first-page": "24",
"journal-title": "Commun. Med.",
"key": "10.1016/j.stemcr.2023.05.007_bib52",
"volume": "1",
"year": "2021"
},
{
"DOI": "10.1038/s42003-021-02453-y",
"article-title": "Human embryonic stem cell-derived cardiomyocyte platform screens inhibitors of SARS-CoV-2 infection",
"author": "Williams",
"doi-asserted-by": "crossref",
"first-page": "926",
"journal-title": "Commun. Biol.",
"key": "10.1016/j.stemcr.2023.05.007_bib53",
"volume": "4",
"year": "2021"
},
{
"DOI": "10.1016/j.celrep.2020.108234",
"article-title": "Evasion of type I interferon by SARS-CoV-2",
"author": "Xia",
"doi-asserted-by": "crossref",
"first-page": "108234",
"journal-title": "Cell Rep.",
"key": "10.1016/j.stemcr.2023.05.007_bib54",
"volume": "33",
"year": "2020"
},
{
"DOI": "10.1186/s41065-020-00168-4",
"article-title": "Mediators of SARS-CoV-2 entry are preferentially enriched in cardiomyocytes",
"author": "Yang",
"doi-asserted-by": "crossref",
"first-page": "4",
"journal-title": "Hereditas",
"key": "10.1016/j.stemcr.2023.05.007_bib55",
"volume": "158",
"year": "2021"
},
{
"article-title": "The FDA-approved drug Alectinib compromises SARS-CoV-2 nucleocapsid phosphorylation and inhibits viral infection in vitro",
"author": "Yaron",
"journal-title": "bioRxiv",
"key": "10.1016/j.stemcr.2023.05.007_bib56",
"year": "2020"
},
{
"DOI": "10.1016/j.stem.2020.10.004",
"article-title": "Three-dimensional human alveolar stem cell culture models reveal infection response to SARS-CoV-2",
"author": "Youk",
"doi-asserted-by": "crossref",
"first-page": "905",
"journal-title": "Cell Stem Cell",
"key": "10.1016/j.stemcr.2023.05.007_bib57",
"volume": "27",
"year": "2020"
},
{
"DOI": "10.1126/science.abd4570",
"article-title": "Inborn errors of type I IFN immunity in patients with life-threatening COVID-19",
"author": "Zhang",
"doi-asserted-by": "crossref",
"first-page": "eabd4570",
"journal-title": "Science",
"key": "10.1016/j.stemcr.2023.05.007_bib58",
"volume": "370",
"year": "2020"
},
{
"DOI": "10.1038/s41586-020-2951-z",
"article-title": "Addendum: a pneumonia outbreak associated with a new coronavirus of probable bat origin",
"author": "Zhou",
"doi-asserted-by": "crossref",
"first-page": "E6",
"journal-title": "Nature",
"key": "10.1016/j.stemcr.2023.05.007_bib59",
"volume": "588",
"year": "2020"
},
{
"DOI": "10.1038/s41467-019-09234-6",
"article-title": "Metascape provides a biologist-oriented resource for the analysis of systems-level datasets",
"author": "Zhou",
"doi-asserted-by": "crossref",
"first-page": "1523",
"journal-title": "Nat. Commun.",
"key": "10.1016/j.stemcr.2023.05.007_bib60",
"volume": "10",
"year": "2019"
},
{
"DOI": "10.1007/s11684-020-0754-0",
"article-title": "Single-cell RNA-seq data analysis on the receptor ACE2 expression reveals the potential risk of different human organs vulnerable to 2019-nCoV infection",
"author": "Zou",
"doi-asserted-by": "crossref",
"first-page": "185",
"journal-title": "Front. Med.",
"key": "10.1016/j.stemcr.2023.05.007_bib61",
"volume": "14",
"year": "2020"
}
],
"reference-count": 61,
"references-count": 61,
"relation": {},
"resource": {
"primary": {
"URL": "https://linkinghub.elsevier.com/retrieve/pii/S2213671123001856"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Cell Biology",
"Developmental Biology",
"Genetics",
"Biochemistry"
],
"subtitle": [],
"title": "Parallel use of human stem cell lung and heart models provide insights for SARS-CoV-2 treatment",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1016/elsevier_cm_policy",
"volume": "18"
}
rudraraju