The Association Between Metformin Use and Outcomes of Hospitalized COVID-19 Patients
et al., ResearchGate, 7/2025, Jul 2025
Metformin for COVID-19
3rd treatment shown to reduce risk in
July 2020, now with p < 0.00000000001 from 110 studies.
Lower risk for mortality, ventilation, ICU, hospitalization, progression, recovery, and viral clearance.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 285 hospitalized COVID-19 patients in Taiwan with 41 treated with metformin, showing no significant difference in mortality with metformin use. Authors note higher ventilation with use ≥17.5 days, however this requires hospitalization ≥17.5 days, which may be independently associated with more serious cases and ventilation.
Although the 33% lower mortality is not statistically significant, it is consistent with the significant 36% lower mortality [32‑40%] from meta-analysis of the 74 mortality results to date.
|
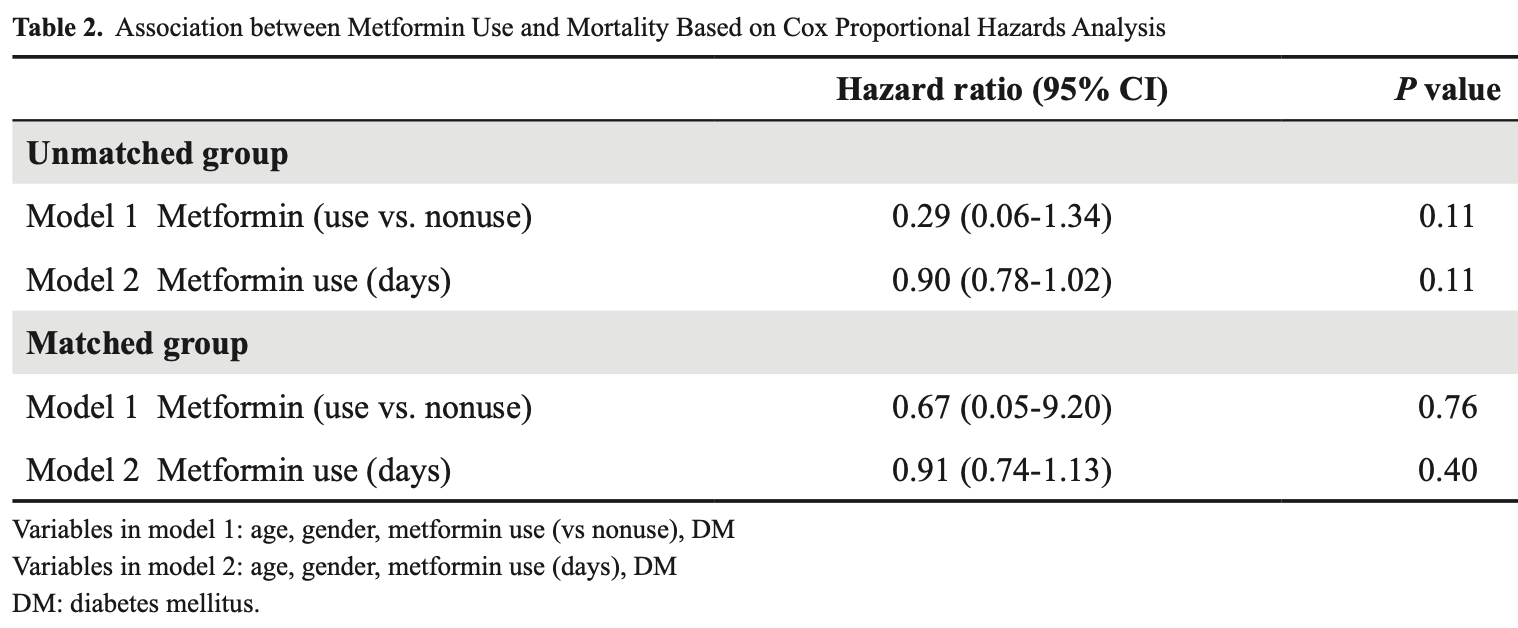
risk of death, 33.0% lower, HR 0.67, p = 0.76, treatment 41, control 41, propensity score matching, Cox proportional hazards.
|
|
risk of mechanical ventilation, 45.0% higher, HR 1.45, p = 0.52, treatment 41, control 41, propensity score matching, Cox proportional hazards.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Lin et al., 26 Jul 2025, retrospective, Taiwan, peer-reviewed, mean age 62.3, 11 authors, study period 1 May, 2021 - 30 June, 2021.
The Association Between Metformin Use and Outcomes of Hospitalized COVID-19 Patients
Background: Metformin is a widely prescribed medication for type 2 diabetes; however, therapeutic effects beyond glucose control have been reported. Recent studies have suggested its potential in alleviating symptoms of post-COVID-19 condition (long COVID), and possibly shortening the duration of the disease. We conducted this study to investigate whether metformin use could improve the outcomes of hospitalized COVID-19 patients.
Methods: We included patients diagnosed with COVID-19 infection at MacKay Memorial Hospital from May to June 2021. We categorized the patients into metformin and nonmetformin use groups, regardless of their diabetes mellitus status. Results: A total of 285 patients were included. After propensity score matching, 82 patients were enrolled for analysis, including 41 patients in each group. Cox proportional hazards analysis showed that mortality was not related to metformin use (adjusted hazard ra io a con ence in er al p=0.76) or duration of metformin use (aHR: 0.91, 95% CI: 0.74-1.13, p=0.40). However, patients with a longer duration of metformin use had a higher risk of receiving invasive mechanical ventilation support (aHR: 1.08, 95% CI: 1.03-1.13, p=0.003).
Conclusion: Our findings showed that mortality was not significantly associated with metformin use or its duration. However, patients with a longer duration of metformin use appeared to have a higher risk of requiring invasive mechanical ventilation support. Consequently, the duration of metformin use may be linked to the progression of COVID-19. Further studies are warranted to clarify the relevance of metformin use in the treatment of
References
Bramante, Buse, Liebovitz, Outpatient treatment of COVID-19 and incidence of post-COVID-19 condition over 10 months (COVID-OUT): a multicentre, randomised, quadruple-blind, parallel-group, phase 3 trial, Lancet Infect Dis
Chen, Lee, Cia, A review of treatment of coronavirus disease 2019 (COVID-19): therapeutic repurposing and unmet clinical needs, Front Pharmacol
Cory, Emmons, Yarbro, Metformin suppresses monocyte immunometabolic activation by SARS-CoV-2 spike protein subunit 1, Front Immunol
Erickson, Fenno, Barzilai, Metformin for treatment of acute COVID-19: systematic review of clinical trial data against SARS-CoV-2, Diabetes Care
Guo, Gao, Xie, Effects of metformin on COVID-19 patients with type 2 diabetes: a retrospective study, Diabetes Metab Syndr Obes
Kamyshnyi, Matskevych, Lenchuk, Metformin to decrease COVID-19 severity and mortality: molecular mechanisms and therapeutic potential, Biomed Pharmacother
Maiese, The mechanistic target of rapamycin (mTOR): novel considerations as an antiviral treatment, Curr Neurovasc Res
Malhotra, Hepokoski, Mccowen, ACE2, metformin, and COVID-19, iScience
Pence, Atypical monocytes in COVID-19: lighting the fire of cytokine storm?, J Leukoc Biol
Samuel, Varghese, Büsselberg, Therapeutic potential of metformin in COVID-19: reasoning for its protective role, Trends Microbiol
Taher, El-Masry, Abouelkheir, Antiinflammatory effect of metformin against an experimental model of LPS-induced cytokine storm, Exp Ther Med
Treskova-Schwarzbach, Haas, Reda, Preexisting health conditions and severe COVID-19 outcomes: an umbrella review approach and metaanalysis of global evidence, BMC Med
Wise, Covid-19: metformin reduces the risk of developing long term symptoms by 40%, study finds, BMJ
Zangiabadian, Nejadghaderi, Zahmatkesh, The efficacy and potential mechanisms of metformin in the treatment of COVID-19 in the diabetics: a systematic review, Front Endocrinol
