Efficacy of physiological seawater nasal irrigation for the treatment of children with SARS-CoV-2 Omicron BA.2 variant infection: a randomized controlled trial
et al., World Journal of Pediatrics, doi:10.1007/s12519-023-00749-z, Sep 2023
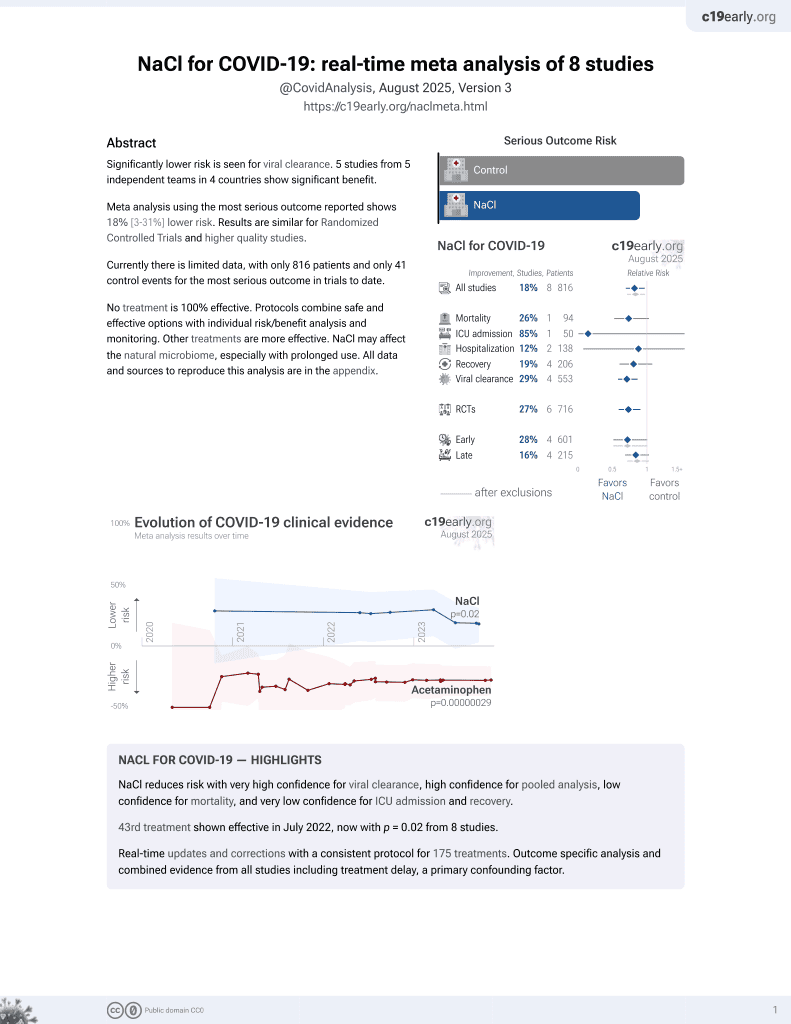
NaCl for COVID-19
44th treatment shown to reduce risk in
July 2022, now with p = 0.0028 from 9 studies.
Lower risk for progression and viral clearance.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
RCT 403 children in China with mild/asymptomatic COVID-19, showing significantly faster viral clearance with physiological seawater nasal irrigation.
Standard of Care (SOC) for COVID-19 in the study country,
China, is average with moderate efficacy for approved treatments1.
|
risk of no viral clearance, 24.8% lower, HR 0.75, p = 0.11, treatment 204, control 199, inverted to make HR<1 favor treatment, viral clearance, day 5.
|
|
risk of no viral clearance, 21.3% lower, HR 0.79, p = 0.02, treatment 204, control 199, inverted to make HR<1 favor treatment, shorter viral shedding duration, day 5.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Lin et al., 10 Sep 2023, Randomized Controlled Trial, China, peer-reviewed, 10 authors, average treatment delay 3.72 days.
The Association Between Metformin Use and Outcomes of Hospitalized COVID-19 Patients
Background: Metformin is a widely prescribed medication for type 2 diabetes; however, therapeutic effects beyond glucose control have been reported. Recent studies have suggested its potential in alleviating symptoms of post-COVID-19 condition (long COVID), and possibly shortening the duration of the disease. We conducted this study to investigate whether metformin use could improve the outcomes of hospitalized COVID-19 patients.
Methods: We included patients diagnosed with COVID-19 infection at MacKay Memorial Hospital from May to June 2021. We categorized the patients into metformin and nonmetformin use groups, regardless of their diabetes mellitus status. Results: A total of 285 patients were included. After propensity score matching, 82 patients were enrolled for analysis, including 41 patients in each group. Cox proportional hazards analysis showed that mortality was not related to metformin use (adjusted hazard ra io a con ence in er al p=0.76) or duration of metformin use (aHR: 0.91, 95% CI: 0.74-1.13, p=0.40). However, patients with a longer duration of metformin use had a higher risk of receiving invasive mechanical ventilation support (aHR: 1.08, 95% CI: 1.03-1.13, p=0.003).
Conclusion: Our findings showed that mortality was not significantly associated with metformin use or its duration. However, patients with a longer duration of metformin use appeared to have a higher risk of requiring invasive mechanical ventilation support. Consequently, the duration of metformin use may be linked to the progression of COVID-19. Further studies are warranted to clarify the relevance of metformin use in the treatment of
References
Bramante, Buse, Liebovitz, Outpatient treatment of COVID-19 and incidence of post-COVID-19 condition over 10 months (COVID-OUT): a multicentre, randomised, quadruple-blind, parallel-group, phase 3 trial, Lancet Infect Dis
Chen, Lee, Cia, A review of treatment of coronavirus disease 2019 (COVID-19): therapeutic repurposing and unmet clinical needs, Front Pharmacol
Cory, Emmons, Yarbro, Metformin suppresses monocyte immunometabolic activation by SARS-CoV-2 spike protein subunit 1, Front Immunol
Erickson, Fenno, Barzilai, Metformin for treatment of acute COVID-19: systematic review of clinical trial data against SARS-CoV-2, Diabetes Care
Guo, Gao, Xie, Effects of metformin on COVID-19 patients with type 2 diabetes: a retrospective study, Diabetes Metab Syndr Obes
Kamyshnyi, Matskevych, Lenchuk, Metformin to decrease COVID-19 severity and mortality: molecular mechanisms and therapeutic potential, Biomed Pharmacother
Maiese, The mechanistic target of rapamycin (mTOR): novel considerations as an antiviral treatment, Curr Neurovasc Res
Malhotra, Hepokoski, Mccowen, ACE2, metformin, and COVID-19, iScience
Pence, Atypical monocytes in COVID-19: lighting the fire of cytokine storm?, J Leukoc Biol
Samuel, Varghese, Büsselberg, Therapeutic potential of metformin in COVID-19: reasoning for its protective role, Trends Microbiol
Taher, El-Masry, Abouelkheir, Antiinflammatory effect of metformin against an experimental model of LPS-induced cytokine storm, Exp Ther Med
Treskova-Schwarzbach, Haas, Reda, Preexisting health conditions and severe COVID-19 outcomes: an umbrella review approach and metaanalysis of global evidence, BMC Med
Wise, Covid-19: metformin reduces the risk of developing long term symptoms by 40%, study finds, BMJ
Zangiabadian, Nejadghaderi, Zahmatkesh, The efficacy and potential mechanisms of metformin in the treatment of COVID-19 in the diabetics: a systematic review, Front Endocrinol
DOI record:
{
"DOI": "10.1007/s12519-023-00749-z",
"ISSN": [
"1708-8569",
"1867-0687"
],
"URL": "http://dx.doi.org/10.1007/s12519-023-00749-z",
"alternative-id": [
"749"
],
"assertion": [
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Received",
"name": "received",
"order": 1,
"value": "3 January 2023"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Accepted",
"name": "accepted",
"order": 2,
"value": "14 July 2023"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "First Online",
"name": "first_online",
"order": 3,
"value": "10 September 2023"
},
{
"group": {
"label": "Declarations",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 1
},
{
"group": {
"label": "Conflict of interest",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 2,
"value": "No financial or non-financial benefits have been received or will be received from any party related directly or indirectly to the subject of this article."
},
{
"group": {
"label": "Ethical approval",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 3,
"value": "The study was approved by the ethics committee of the Shanghai Children's Medical Center and conducted according to the Declaration of Helsinki guidelines (SCMCIRB-K2022036-1)."
}
],
"author": [
{
"affiliation": [],
"family": "Lin",
"given": "Ji-Lei",
"sequence": "first"
},
{
"affiliation": [],
"family": "Zhang",
"given": "Fen",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Li",
"given": "Yan-Bo",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Yuan",
"given": "Shu-Hua",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Wu",
"given": "Jin-Hong",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Zhang",
"given": "Jing",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Zhang",
"given": "Lei",
"sequence": "additional"
},
{
"affiliation": [],
"family": "He",
"given": "Yi",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Chen",
"given": "Jie",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-0944-2692",
"affiliation": [],
"authenticated-orcid": false,
"family": "Yin",
"given": "Yong",
"sequence": "additional"
}
],
"container-title": "World Journal of Pediatrics",
"container-title-short": "World J Pediatr",
"content-domain": {
"crossmark-restriction": false,
"domain": [
"link.springer.com"
]
},
"created": {
"date-parts": [
[
2023,
9,
10
]
],
"date-time": "2023-09-10T18:01:48Z",
"timestamp": 1694368908000
},
"deposited": {
"date-parts": [
[
2023,
9,
10
]
],
"date-time": "2023-09-10T18:03:00Z",
"timestamp": 1694368980000
},
"funder": [
{
"award": [
"PW2021E-06"
],
"name": "Health and Family Planning Research Project of Pudong New Area Health Committee"
}
],
"indexed": {
"date-parts": [
[
2023,
9,
11
]
],
"date-time": "2023-09-11T21:27:42Z",
"timestamp": 1694467662266
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2023,
9,
10
]
]
},
"language": "en",
"license": [
{
"URL": "https://www.springernature.com/gp/researchers/text-and-data-mining",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
9,
10
]
],
"date-time": "2023-09-10T00:00:00Z",
"timestamp": 1694304000000
}
},
{
"URL": "https://www.springernature.com/gp/researchers/text-and-data-mining",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
9,
10
]
],
"date-time": "2023-09-10T00:00:00Z",
"timestamp": 1694304000000
}
}
],
"link": [
{
"URL": "https://link.springer.com/content/pdf/10.1007/s12519-023-00749-z.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://link.springer.com/article/10.1007/s12519-023-00749-z/fulltext.html",
"content-type": "text/html",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://link.springer.com/content/pdf/10.1007/s12519-023-00749-z.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "297",
"original-title": [],
"prefix": "10.1007",
"published": {
"date-parts": [
[
2023,
9,
10
]
]
},
"published-online": {
"date-parts": [
[
2023,
9,
10
]
]
},
"publisher": "Springer Science and Business Media LLC",
"reference": [
{
"DOI": "10.1016/j.jinf.2022.08.034",
"doi-asserted-by": "crossref",
"key": "749_CR1",
"unstructured": "Yin Y, Lin J, Yuan S, Tong S, Chen E, Zheng J, et al. The relationship between early isolation and the duration of viral shedding of mild and asymptomatic infection with SARS-CoV-2 Omicron BA.2 variant. J Infect. 2022;85:e184–6."
},
{
"DOI": "10.1056/NEJMoa2202826",
"author": "AM Price",
"doi-asserted-by": "publisher",
"first-page": "1899",
"journal-title": "N Engl J Med",
"key": "749_CR2",
"unstructured": "Price AM, Olson SM, Newhams MM, Halasa NB, Boom JA, Sahni LC, et al. BNT162b2 protection against the omicron variant in children and adolescents. N Engl J Med. 2022;386:1899–909.",
"volume": "386",
"year": "2022"
},
{
"DOI": "10.1038/s41593-020-00758-5",
"author": "J Meinhardt",
"doi-asserted-by": "publisher",
"first-page": "168",
"journal-title": "Nat Neurosci",
"key": "749_CR3",
"unstructured": "Meinhardt J, Radke J, Dittmayer C, Franz J, Thomas C, Mothes R, et al. Olfactory transmucosal SARS-CoV-2 invasion as a port of central nervous system entry in individuals with COVID-19. Nat Neurosci. 2021;24:168–75.",
"volume": "24",
"year": "2021"
},
{
"DOI": "10.1002/alr.22587",
"author": "ST Moein",
"doi-asserted-by": "publisher",
"first-page": "944",
"journal-title": "Int Forum Allergy Rhinol",
"key": "749_CR4",
"unstructured": "Moein ST, Hashemian SM, Mansourafshar B, Khorram-Tousi A, Tabarsi P, Doty RL. Smell dysfunction: a biomarker for COVID-19. Int Forum Allergy Rhinol. 2020;10:944–50.",
"volume": "10",
"year": "2020"
},
{
"DOI": "10.1111/all.14665",
"author": "M Wang",
"doi-asserted-by": "publisher",
"first-page": "789",
"journal-title": "Allergy",
"key": "749_CR5",
"unstructured": "Wang M, Bu X, Fang G, Luan G, Huang Y, Akdis CA, et al. Distinct expression of SARS-CoV-2 receptor ACE2 correlates with endotypes of chronic rhinosinusitis with nasal polyps. Allergy. 2021;76:789–803.",
"volume": "76",
"year": "2021"
},
{
"author": "KC DeGeorge",
"first-page": "281",
"issue": "5",
"journal-title": "Am Fam Physician",
"key": "749_CR6",
"unstructured": "DeGeorge KC, Ring DJ, Dalrymple SN. Treatment of the Common Cold. Am Fam Physician. 2019;100:281–9.",
"volume": "100",
"year": "2019"
},
{
"DOI": "10.1177/01455613221123737",
"doi-asserted-by": "crossref",
"key": "749_CR7",
"unstructured": "Baxter AL, Schwartz KR, Johnson RW, Kuchinski AM, Swartout KM, Srinivasa Rao ASR, et al. Rapid initiation of nasal saline irrigation to reduce severity in high-risk COVID+ outpatients. Ear Nose Throat J. 2022;1455613221123737."
},
{
"DOI": "10.1016/j.isci.2022.105475",
"doi-asserted-by": "crossref",
"key": "749_CR8",
"unstructured": "Yuan L, Zhu H, Zhou M, Ma J, Liu X, Wu K, et al. Nasal irrigation efficiently attenuates SARS-CoV-2 Omicron infection, transmission and lung injury in the Syrian hamster model. iScience. 2022;25:105475."
},
{
"DOI": "10.3390/md20050330",
"doi-asserted-by": "crossref",
"key": "749_CR9",
"unstructured": "Štanfel D, Kalogjera L, Ryazantsev SV, Hlača K, Radtsig EY, Teimuraz R, et al. The Role of Seawater and Saline Solutions in Treatment of Upper Respiratory Conditions. Mar Drugs. 2022;20:330."
},
{
"DOI": "10.14715/cmb/2020.66.5.11",
"doi-asserted-by": "crossref",
"key": "749_CR10",
"unstructured": "Zhang Y, Li W. Effects of oral desloratadine citrate disodium combined with physiological seawater nasal irrigation on IgE levels, IL-4, IL-6, IL-13 and IFN-γ expression and treatment of intermittent allergic rhinitis. Cell Mol Biol (Noisy-le-grand). 2020;66:54–8."
},
{
"DOI": "10.1177/00034894211025411",
"author": "Y Atar",
"doi-asserted-by": "publisher",
"first-page": "427",
"issue": "4",
"journal-title": "Ann Otol Rhinol Laryngol",
"key": "749_CR11",
"unstructured": "Atar Y, Karaketir S, Aydogdu I, Sari H, Bircan HS, Uyar Y, et al. Comparison of isotonic seawater nasal spray containing chamomile liquid extract and other isotonic seawater nasal washing solutions for allergic rhinitis. Ann Otol Rhinol Laryngol. 2022;131:427–34.",
"volume": "131",
"year": "2022"
},
{
"DOI": "10.3390/pharmaceutics14112502",
"doi-asserted-by": "crossref",
"key": "749_CR12",
"unstructured": "Cegolon L, Mastrangelo G, Emanuelli E, Camerotto R, Spinato G, Frezza D. Early Negativization of SARS-CoV-2 Infection by Nasal Spray of Seawater plus Additives: The RENAISSANCE Open-Label Controlled Clinical Trial. Pharmaceutics. 2022;14:2502."
},
{
"DOI": "10.1002/jmv.28767",
"doi-asserted-by": "crossref",
"key": "749_CR13",
"unstructured": "Yin Y, Lin J, Yuan S, Tong S, He Y, Dong B,etl al.: Vaccination status for mild and asymptomatic infections with SARS-CoV-2 Omicron BA.2 variant in Shanghai. Journal of Medical Virology. 2023;95:e28767."
},
{
"DOI": "10.1002/14651858.CD006821.pub3",
"doi-asserted-by": "crossref",
"key": "749_CR14",
"unstructured": "King D, Mitchell B, Williams CP, Spurling GK. Saline nasal irrigation for acute upper respiratory tract infections. Cochrane Database Syst Rev. 2015;2015:Cd006821."
},
{
"DOI": "10.1016/j.jcf.2018.01.001",
"author": "AT Trimble",
"doi-asserted-by": "publisher",
"first-page": "650",
"issue": "5",
"journal-title": "J Cyst Fibros",
"key": "749_CR15",
"unstructured": "Trimble AT, Whitney Brown A, Laube BL, Lechtzin N, Zeman KL, Wu J, et al. Hypertonic saline has a prolonged effect on mucociliary clearance in adults with cystic fibrosis. J Cyst Fibros. 2018;17:650–6.",
"volume": "17",
"year": "2018"
},
{
"DOI": "10.1007/s00405-008-0807-5",
"doi-asserted-by": "crossref",
"key": "749_CR16",
"unstructured": "Süslü N, Bajin MD, Süslü AE, Oğretmenoğlu O. Effects of buffered 2.3%, buffered 0.9%, and nonbuffered 0.9% irrigation solutions on nasal mucosa after septoplasty. Eur Arch Otorhinolaryngol. 2009;266:685–9."
},
{
"DOI": "10.1016/j.otohns.2004.05.026",
"author": "BK Keojampa",
"doi-asserted-by": "publisher",
"first-page": "679",
"issue": "5",
"journal-title": "Otolaryngol Head Neck Surg",
"key": "749_CR17",
"unstructured": "Keojampa BK, Nguyen MH, Ryan MW. Effects of buffered saline solution on nasal mucociliary clearance and nasal airway patency. Otolaryngol Head Neck Surg. 2004;131:679–82.",
"volume": "131",
"year": "2004"
},
{
"DOI": "10.1016/j.anorl.2015.08.001",
"doi-asserted-by": "crossref",
"key": "749_CR18",
"unstructured": "Bastier PL, Lechot A, Bordenave L, Durand M, de Gabory L. Nasal irrigation: from empiricism to evidence-based medicine. A review. Eur Ann Otorhinolaryngol Head Neck Dis. 2015;132:281–5."
},
{
"DOI": "10.1021/acsptsci.1c00080",
"author": "RRG Machado",
"doi-asserted-by": "publisher",
"first-page": "1514",
"issue": "5",
"journal-title": "ACS Pharmacol Transl Sci",
"key": "749_CR19",
"unstructured": "Machado RRG, Glaser T, Araujo DB, Petiz LL, Oliveira DBL, Durigon GS, et al. Inhibition of severe acute respiratory syndrome coronavirus 2 replication by hypertonic saline solution in lung and kidney epithelial cells. ACS Pharmacol Transl Sci. 2021;4:1514–27.",
"volume": "4",
"year": "2021"
},
{
"DOI": "10.1177/2058738420941757",
"author": "M Casale",
"doi-asserted-by": "publisher",
"first-page": "205873842094175",
"journal-title": "Int J Immunopathol Pharmacol",
"key": "749_CR20",
"unstructured": "Casale M, Rinaldi V, Sabatino L, Moffa A, Ciccozzi M. Could nasal irrigation and oral rinse reduce the risk for COVID-19 infection? Int J Immunopathol Pharmacol. 2020;34:2058738420941757.",
"volume": "34",
"year": "2020"
},
{
"DOI": "10.1002/14651858.CD013627.pub2",
"doi-asserted-by": "crossref",
"key": "749_CR21",
"unstructured": "Burton MJ, Clarkson JE, Goulao B, Glenny AM, McBain AJ, Schilder AG,et al. Antimicrobial mouthwashes (gargling) and nasal sprays administered to patients with suspected or confirmed COVID-19 infection to improve patient outcomes and to protect healthcare workers treating them. Cochrane Database Syst Rev. 2020;9:Cd013627."
},
{
"DOI": "10.1007/s00228-021-03102-3",
"author": "S Huijghebaert",
"doi-asserted-by": "publisher",
"first-page": "1275",
"issue": "9",
"journal-title": "Eur J Clin Pharmacol",
"key": "749_CR22",
"unstructured": "Huijghebaert S, Hoste L, Vanham G. Essentials in saline pharmacology for nasal or respiratory hygiene in times of COVID-19. Eur J Clin Pharmacol. 2021;77:1275–93.",
"volume": "77",
"year": "2021"
},
{
"DOI": "10.3389/fneur.2021.794471",
"author": "G Spinato",
"doi-asserted-by": "publisher",
"journal-title": "Front Neurol",
"key": "749_CR23",
"unstructured": "Spinato G, Fabbris C, Costantini G, Conte F, Scotton PG, Cinetto F, et al. The effect of isotonic saline nasal lavages in improving symptoms in SARS-CoV-2 infection: a case-control study. Front Neurol. 2021;12:794471.",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.1038/s41598-018-37703-3",
"author": "S Ramalingam",
"doi-asserted-by": "publisher",
"first-page": "1015",
"issue": "1",
"journal-title": "Sci Rep",
"key": "749_CR24",
"unstructured": "Ramalingam S, Graham C, Dove J, Morrice L, Sheikh A. A pilot, open labeled, randomized controlled trial of hypertonic saline nasal irrigation and gargling for the common cold. Sci Rep. 2019;9:1015.",
"volume": "9",
"year": "2019"
},
{
"DOI": "10.1016/S2666-5247(20)30172-5",
"author": "M Cevik",
"doi-asserted-by": "publisher",
"first-page": "e13",
"issue": "1",
"journal-title": "Lancet Microbe",
"key": "749_CR25",
"unstructured": "Cevik M, Tate M, Lloyd O, Maraolo AE, Schafers J, Ho A. SARS-CoV-2, SARS-CoV, and MERS-CoV viral load dynamics, duration of viral shedding, and infectiousness: a systematic review and meta-analysis. Lancet Microbe. 2021;2:e13-22.",
"volume": "2",
"year": "2021"
}
],
"reference-count": 25,
"references-count": 25,
"relation": {},
"resource": {
"primary": {
"URL": "https://link.springer.com/10.1007/s12519-023-00749-z"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Pediatrics, Perinatology and Child Health"
],
"subtitle": [],
"title": "Efficacy of physiological seawater nasal irrigation for the treatment of children with SARS-CoV-2 Omicron BA.2 variant infection: a randomized controlled trial",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1007/springer_crossmark_policy"
}