Elimination of olfactory sensory neurons by zinc sulfate inoculation prevents SARS-CoV-2 infection of the brain in K18-hACE2 transgenic mice
et al., Scientific Reports, doi:10.1038/s41598-024-78538-5, Nov 2024
Zinc for COVID-19
2nd treatment shown to reduce risk in
July 2020, now with p = 0.00000028 from 47 studies, recognized in 23 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
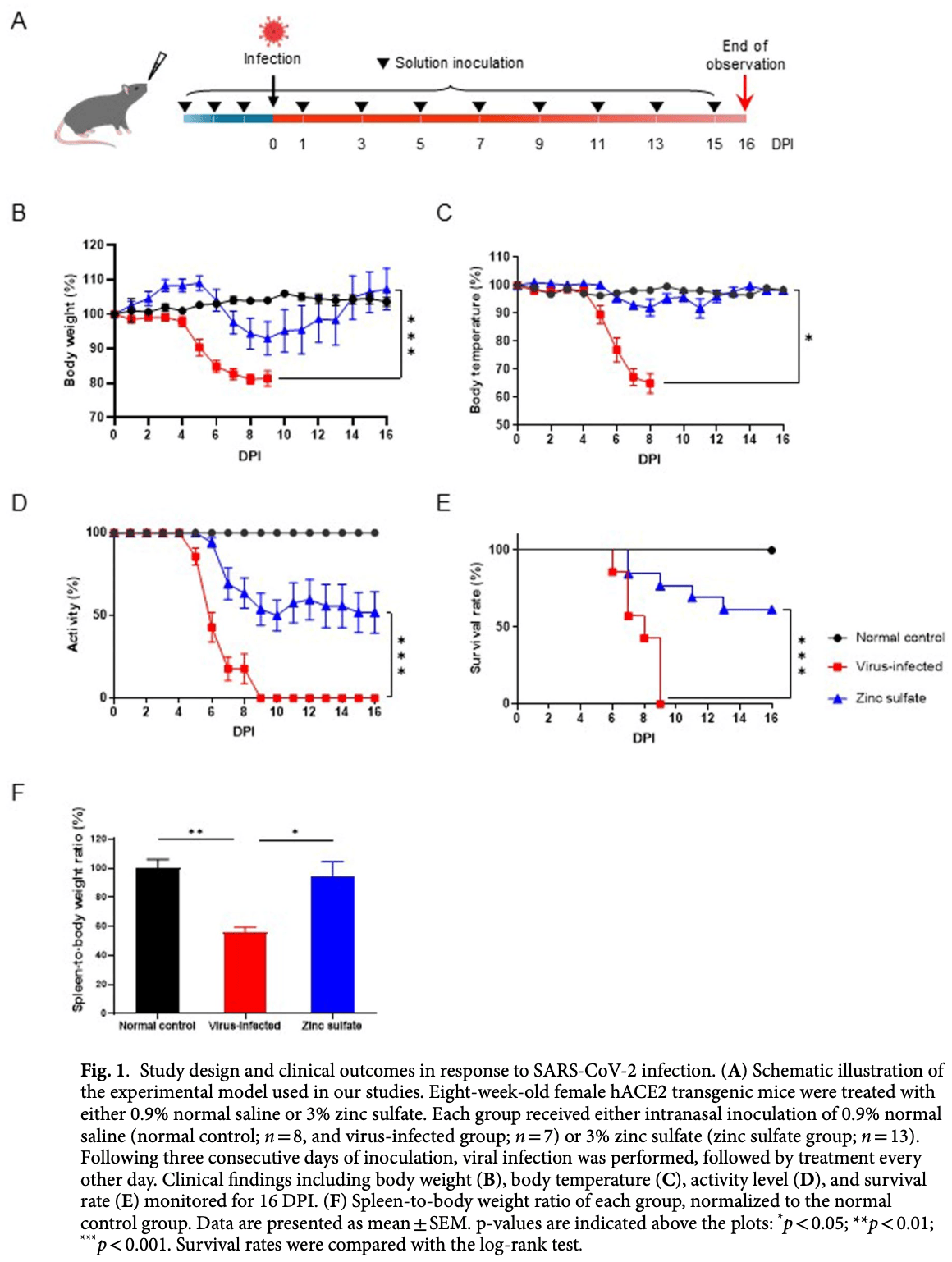
Mouse study showing that zinc sulfate protects K18-hACE2 transgenic mice from lethal SARS-CoV-2 infection by preventing viral transmission to the brain via the olfactory nerve pathway. Authors found that mice lacking olfactory sensory neurons exhibited reduced viral transmission to the brain and significantly improved survival compared to untreated infected mice. The virus persisted longer in the olfactory epithelium of untreated mice, and this correlated with greater brain infection. The results suggest that early inhibition of the olfactory nerve pathway may effectively prevent SARS-CoV-2 neuroinvasion.
12 preclinical studies support the efficacy of zinc for COVID-19:
1.
Agamah et al., Network-based multi-omics-disease-drug associations reveal drug repurposing candidates for COVID-19 disease phases, ScienceOpen, doi:10.58647/DRUGARXIV.PR000010.v1.
2.
Lockwood, T., Coordination chemistry suggests that independently observed benefits of metformin and Zn2+ against COVID-19 are not independent, BioMetals, doi:10.1007/s10534-024-00590-5.
3.
El-Megharbel et al., Chemical and spectroscopic characterization of (Artemisinin/Quercetin/ Zinc) novel mixed ligand complex with assessment of its potent high antiviral activity against SARS-CoV-2 and antioxidant capacity against toxicity induced by acrylamide in male rats, PeerJ, doi:10.7717/peerj.15638.
4.
Bess et al., Identification of oral therapeutics using an AI platform against the virus responsible for COVID-19, SARS-CoV-2, Frontiers in Pharmacology, doi:10.3389/fphar.2023.1297924.
5.
Pormohammad et al., Zinc and SARS-CoV-2: A molecular modeling study of Zn interactions with RNA-dependent RNA-polymerase and 3C-like proteinase enzymes, International Journal of Molecular Medicine, doi:10.3892/ijmm.2020.4790.
6.
Pelucelli et al., Zn2+ and Cu2+ Interaction with the Recognition Interface of ACE2 for SARS-CoV-2 Spike Protein, International Journal of Molecular Sciences, doi:10.3390/ijms24119202.
7.
Hajdrik et al., In Vitro Determination of Inhibitory Effects of Humic Substances Complexing Zn and Se on SARS-CoV-2 Virus Replication, Foods, doi:10.3390/foods11050694.
8.
Panchariya et al., Zinc2+ ion inhibits SARS-CoV-2 main protease and viral replication in vitro, Chemical Communications, doi:10.1039/D1CC03563K.
Lee et al., 13 Nov 2024, peer-reviewed, 16 authors.
Contact: snumouse@snu.ac.kr, yangkyuc@konkuk.ac.kr.
Elimination of olfactory sensory neurons by zinc sulfate inoculation prevents SARS-CoV-2 infection of the brain in K18-hACE2 transgenic mice
Scientific Reports, doi:10.1038/s41598-024-78538-5
Coronavirus disease-2019 (COVID-19), attributed to the severe acute respiratory syndrome-related coronavirus-2 (SARS-CoV-2), has posed global health challenges since it first emerged in 2019, and its impact continues to persist. The neurotropic nature of SARS-CoV-2 remains undisclosed, though researchers are proposing hypotheses on how the virus is transmitted to the central nervous system. One of the prevailing hypotheses is that SARS-CoV-2 travels through the olfactory nerve system via the olfactory epithelium (OE). Using a K18-human angiotensin converting-enzyme 2 (hACE2) transgenic mouse model with impaired olfactory sensory neurons (OSNs) induced by zinc sulfate, we examined the role of the olfactory nerve in the brain invasion by SARS-CoV-2. Mice lacking OSNs exhibited reduced levels of viral transmission to the brain, leading to significantly improved outcomes following SARS-CoV-2 infection. Moreover, a positive correlation was observed between viral persistence in the OE and brain infection. These results indicate that early inhibition of the olfactory nerve pathway effectively prevents viral invasion of the brain in K18-hACE2 mice. Our study underscores the significance of the olfactory nerve pathway in the transmission of SARS-CoV-2 to the brain.
Author contributions
Declarations
Competing interests The authors declare no competing interests.
Additional information
Supplementary Information The online version contains supplementary material available at h t t p s : / / d o i . o r g / 1 0 . 1 0 3 8 / s 4 1 5 9 8 -0 2 4 -7 8 5 3 8 -5 . Correspondence and requests for materials should be addressed to J.K.S. or Y.-K.C. Reprints and permissions information is available at www.nature.com/reprints.
Publisher's note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations. Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission..
References
Almutairi, Sivandzade, Albekairi, Alqahtani, Cucullo, Neuroinflammation and its impact on the Pathogenesis of COVID-19, Front. Med, doi:10.3389/fmed.2021.745789
Baig, Khaleeq, Ali, Syeda, Evidence of the COVID-19 virus targeting the CNS: tissue distribution, host-virus interaction, and proposed neurotropic mechanisms, ACS Chem. Neurosci, doi:10.1021/acschemneuro.0c00122
Barrantes, Central nervous system targets and routes for SARS-CoV-2: current views and new hypotheses, ACS Chem. Neurosci, doi:10.1021/acschemneuro.0c00434
Bryche, Baly, Meunier, Modulation of olfactory signal detection in the olfactory epithelium: focus on the internal and external environment, and the emerging role of the immune system, Cell. Tissue Res, doi:10.1007/s00441-021-03467-y
Butowt, Bilinska, Von Bartheld, Olfactory dysfunction in COVID-19: new insights into the underlying mechanisms, Trends Neurosci, doi:10.1016/j.tins.2022.11.003
Butowt, Von Bartheld, The route of SARS-CoV-2 to brain infection: have we been barking up the wrong tree?, Mol. Neurodegener, doi:10.1186/s13024-022-00529-9
Chen, Kachramanoglou, Li, Andrews, Choi, Anatomy and cellular constituents of the human olfactory mucosa: a review, J. Neurol. Surg. B Skull Base, doi:10.1055/s-0033-1361837
Chu, Chan, Yuen, Animal models in SARS-CoV-2 research, Nat. Methods, doi:10.1038/s41592-022-01447-w
Cui, Li, Shi, Origin and evolution of pathogenic coronaviruses, Nat. Rev. Microbiol, doi:10.1038/s41579-018-0118-9
De Melo, COVID-19-related anosmia is associated with viral persistence and inflammation in human olfactory epithelium and brain infection in hamsters, Sci. Transl Med, doi:10.1126/scitranslmed.abf8396
Dooley, Mashukova, Toetter, Hatt, Neuhaus, Purinergic receptor antagonists inhibit odorant-mediated CREB phosphorylation in sustentacular cells of mouse olfactory epithelium, BMC Neurosci, doi:10.1186/1471-2202-12-86
Fenrich, SARS-CoV-2 dissemination through peripheral nerves explains multiple organ injury, Front. Cell. Neurosci, doi:10.3389/fncel.2020.00229
Fodoulian, SARS-CoV-2 receptors and entry genes are expressed in the human olfactory neuroepithelium and brain, iScience, doi:10.1016/j.isci.2020.101839
Gheware, ACE2 protein expression in lung tissues of severe COVID-19 infection, Sci. Rep, doi:10.1038/s41598-022-07918-6
Hamming, Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis, J. Pathol, doi:10.1002/path.1570
Harkema, Sinus, pharynx, and Larynx
Helms, Neurologic features in severe SARS-CoV-2 infection, N Engl. J. Med, doi:10.1056/NEJMc2008597
Hernández-Parra, Alteration of the blood-brain barrier by COVID-19 and its implication in the permeation of drugs into the brain, Front. Cell. Neurosci, doi:10.3389/fncel.2023.1125109
Kuruppuarachchi, Jang, Seo, Comparison of the pathogenicity of SARS-CoV-2 delta and omicron variants by analyzing the expression patterns of immune response genes in K18-hACE2 transgenic mice, Front. Biosci, doi:10.31083/j.fbl2711316
Lopes-Pacheco, Pathogenesis of multiple organ injury in COVID-19 and potential therapeutic strategies, Front. Physiol, doi:10.3389/fphys.2021.593223
Matthews, Weiss, Paterson, Murine Hepatitis virus-a model for virus-induced CNS demyelination, J. Neurovirol, doi:10.1080/13550280290049534
Meinhardt, Olfactory transmucosal SARS-CoV-2 invasion as a port of central nervous system entry in individuals with COVID-19, Nat. Neurosci, doi:10.1038/s41593-020-00758-5
Mora-Díaz, Piñeyro, Houston, Zimmerman, Giménez-Lirola, Porcine hemagglutinating encephalomyelitis virus: a review, Front. Vet. Sci, doi:10.3389/fvets.2019.00053
Ni, Role of angiotensin-converting enzyme 2 (ACE2) in COVID-19, Crit. Care, doi:10.1186/s13054-020-03120-0
Prelic, Functional interaction between Drosophila olfactory sensory neurons and their support cells, Front. Cell. Neurosci, doi:10.3389/fncel.2021.789086
Rabaan, SARS-CoV-2 infection and multi-organ system damage: a review, Biomol. Biomed, doi:10.17305/bjbms.2022.7762
Salamanna, Maglio, Landini, Fini, Body localization of ACE-2: on the trail of the keyhole of SARS-CoV-2, Front. Med, doi:10.3389/fmed.2020.594495
Seo, Development of transgenic models susceptible and resistant to SARS-CoV-2 infection in FVB background mice, PloS One, doi:10.1371/journal.pone.0272019
Shao, Olfactory sensory axons target specific protoglomeruli in the olfactory bulb of zebrafish, Neural Dev, doi:10.1186/s13064-017-0095-0
Singh, Neurological infection and complications of SARS-CoV-2: a review, Medicine, doi:10.1097/MD.0000000000030284
Song, Neuroinvasion of SARS-CoV-2 in human and mouse brain, J. Exp. Med, doi:10.1084/jem.20202135
Soung, COVID-19 induces CNS cytokine expression and loss of hippocampal neurogenesis, Brain, doi:10.1093/brain/awac270
Taga, Lauria, COVID-19 and the peripheral nervous system. A 2-year review from the pandemic to the vaccine era, J. Peripher Nerv. Syst, doi:10.1111/jns.12482
Tsukahara, Brann, Datta, Mechanisms of SARS-CoV-2-associated anosmia, Physiol. Rev, doi:10.1152/physrev.00012.2023
Van Riel, Verdijk, Kuiken, The olfactory nerve: a shortcut for influenza and other viral diseases into the central nervous system, J. Pathol, doi:10.1002/path.4461
Verma, Zheng, Meyerholz, Perlman, SARS-CoV-2 infection of sustentacular cells disrupts olfactory signaling pathways, JCI Insight, doi:10.1172/jci.insight.160277
Verstrepen, Baisier, De Cauwer, Neurological manifestations of COVID-19, SARS and MERS, Acta Neurol. Belg, doi:10.1007/s13760-020-01412-4
Vogalis, Hegg, Lucero, Electrical coupling in sustentacular cells of the mouse olfactory epithelium, J. Neurophysiol, doi:10.1152/jn.01299.2004
Walls, Structure, function, and antigenicity of the SARS-CoV-2 spike glycoprotein, Cell, doi:10.1016/j.cell.2020.11.032
Wang, Horby, Hayden, Gao, A novel coronavirus outbreak of global health concern, Lancet, doi:10.1016/S0140-6736(20)30185-9
Wellford, Moseman, Olfactory immune response to SARS-CoV-2, Cell. Mol. Immunol, doi:10.1038/s41423-023-01119-5
Yao, Wang, Liu, Expression of ACE2 in airways: implication for COVID-19 risk and disease management in patients with chronic inflammatory respiratory diseases, Clin. Exp. Allergy, doi:10.1038/s41598-022-07918-6
Ye, SARS-CoV-2 infection in the mouse olfactory system, Cell. Discov, doi:10.1038/s41421-021-00290-1
Yu, Wu, Regeneration and rewiring of rodent olfactory sensory neurons, Exp. Neurol, doi:10.1016/j.expneurol.2016.06.001
Zhang, SARS-CoV-2 crosses the blood-brain barrier accompanied with basement membrane disruption without tight junctions alteration, Signal. Transduct. Target. Ther, doi:10.1038/s41392-021-00719-9
Zhang, Severe acute respiratory syndrome coronavirus 2 infects and damages the mature and immature olfactory sensory neurons of hamsters, Clin. Infect. Dis, doi:10.1093/cid/ciaa995
Zhou, Kang, Li, Zhao, Understanding the neurotropic characteristics of SARS-CoV-2: from neurological manifestations of COVID-19 to potential neurotropic mechanisms, J. Neurol, doi:10.1007/s00415-020-09929-7
Zhu, A novel coronavirus from patients with pneumonia in China, N Engl. J. Med, doi:10.1056/NEJMoa2001017
DOI record:
{
"DOI": "10.1038/s41598-024-78538-5",
"ISSN": [
"2045-2322"
],
"URL": "http://dx.doi.org/10.1038/s41598-024-78538-5",
"alternative-id": [
"78538"
],
"article-number": "27863",
"assertion": [
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Received",
"name": "received",
"order": 1,
"value": "31 May 2024"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Accepted",
"name": "accepted",
"order": 2,
"value": "31 October 2024"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "First Online",
"name": "first_online",
"order": 3,
"value": "13 November 2024"
},
{
"group": {
"label": "Declarations",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 1
},
{
"group": {
"label": "Competing interests",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 2,
"value": "The authors declare no competing interests."
}
],
"author": [
{
"affiliation": [],
"family": "Lee",
"given": "Ji-Hun",
"sequence": "first"
},
{
"affiliation": [],
"family": "Yoo",
"given": "Eun-Seon",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Kim",
"given": "Na-Won",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Shim",
"given": "Won-Yong",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Jeong",
"given": "Han-Bi",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Kim",
"given": "Dong-Hyun",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Park",
"given": "Young-Jun",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Seo",
"given": "Sun-Min",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Yun",
"given": "Jun-Won",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Park",
"given": "Jun Won",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Choi",
"given": "Kang-Seuk",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Lee",
"given": "Ho-Young",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Seo",
"given": "Jun-Young",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Nam",
"given": "Ki Taek",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Seong",
"given": "Je Kyung",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Choi",
"given": "Yang-Kyu",
"sequence": "additional"
}
],
"container-title": "Scientific Reports",
"container-title-short": "Sci Rep",
"content-domain": {
"crossmark-restriction": false,
"domain": [
"link.springer.com"
]
},
"created": {
"date-parts": [
[
2024,
11,
13
]
],
"date-time": "2024-11-13T23:14:54Z",
"timestamp": 1731539694000
},
"deposited": {
"date-parts": [
[
2024,
11,
14
]
],
"date-time": "2024-11-14T00:07:26Z",
"timestamp": 1731542846000
},
"funder": [
{
"award": [
"2021M3H9A1030260",
"2021M3H9A1097269"
],
"name": "Bio & Medical Technology Development Program of the National Research Foundation (NRF), funded by the Korean government"
}
],
"indexed": {
"date-parts": [
[
2024,
11,
14
]
],
"date-time": "2024-11-14T00:40:24Z",
"timestamp": 1731544824530,
"version": "3.28.0"
},
"is-referenced-by-count": 0,
"issue": "1",
"issued": {
"date-parts": [
[
2024,
11,
13
]
]
},
"journal-issue": {
"issue": "1",
"published-online": {
"date-parts": [
[
2024,
12
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by-nc-nd/4.0",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2024,
11,
13
]
],
"date-time": "2024-11-13T00:00:00Z",
"timestamp": 1731456000000
}
},
{
"URL": "https://creativecommons.org/licenses/by-nc-nd/4.0",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2024,
11,
13
]
],
"date-time": "2024-11-13T00:00:00Z",
"timestamp": 1731456000000
}
}
],
"link": [
{
"URL": "https://www.nature.com/articles/s41598-024-78538-5.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://www.nature.com/articles/s41598-024-78538-5",
"content-type": "text/html",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://www.nature.com/articles/s41598-024-78538-5.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "297",
"original-title": [],
"prefix": "10.1038",
"published": {
"date-parts": [
[
2024,
11,
13
]
]
},
"published-online": {
"date-parts": [
[
2024,
11,
13
]
]
},
"publisher": "Springer Science and Business Media LLC",
"reference": [
{
"DOI": "10.1056/NEJMoa2001017",
"author": "N Zhu",
"doi-asserted-by": "publisher",
"first-page": "727",
"journal-title": "N Engl. J. Med.",
"key": "78538_CR1",
"unstructured": "Zhu, N. et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl. J. Med. 382, 727–733. https://doi.org/10.1056/NEJMoa2001017 (2020).",
"volume": "382",
"year": "2020"
},
{
"DOI": "10.1038/s41579-018-0118-9",
"author": "J Cui",
"doi-asserted-by": "publisher",
"first-page": "181",
"journal-title": "Nat. Rev. Microbiol.",
"key": "78538_CR2",
"unstructured": "Cui, J., Li, F. & Shi, Z. L. Origin and evolution of pathogenic coronaviruses. Nat. Rev. Microbiol. 17, 181–192. https://doi.org/10.1038/s41579-018-0118-9 (2019).",
"volume": "17",
"year": "2019"
},
{
"DOI": "10.1016/S0140-6736(20)30185-9",
"author": "C Wang",
"doi-asserted-by": "publisher",
"first-page": "470",
"journal-title": "Lancet",
"key": "78538_CR3",
"unstructured": "Wang, C., Horby, P. W., Hayden, F. G. & Gao, G. F. A novel coronavirus outbreak of global health concern. Lancet. 395, 470–473. https://doi.org/10.1016/S0140-6736(20)30185-9 (2020).",
"volume": "395",
"year": "2020"
},
{
"key": "78538_CR4",
"unstructured": "World Health Organization, WHO Coronavirus (COVID-19) dashboard 2024. : (2024). https://data.who.int/dashboards/covid19/cases"
},
{
"DOI": "10.1016/j.cell.2020.11.032",
"author": "AC Walls",
"doi-asserted-by": "publisher",
"first-page": "1735",
"journal-title": "Cell",
"key": "78538_CR5",
"unstructured": "Walls, A. C. et al. Structure, function, and antigenicity of the SARS-CoV-2 spike glycoprotein. Cell. 183, 1735. https://doi.org/10.1016/j.cell.2020.11.032 (2020).",
"volume": "183",
"year": "2020"
},
{
"DOI": "10.3389/fmed.2020.594495",
"author": "F Salamanna",
"doi-asserted-by": "publisher",
"first-page": "594495",
"journal-title": "Front. Med.",
"key": "78538_CR6",
"unstructured": "Salamanna, F., Maglio, M., Landini, M. P. & Fini, M. Body localization of ACE-2: on the trail of the keyhole of SARS-CoV-2. Front. Med. 7, 594495. https://doi.org/10.3389/fmed.2020.594495 (2020).",
"volume": "7",
"year": "2020"
},
{
"DOI": "10.1002/path.1570",
"author": "I Hamming",
"doi-asserted-by": "publisher",
"first-page": "631",
"journal-title": "J. Pathol.",
"key": "78538_CR7",
"unstructured": "Hamming, I. et al. Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis. J. Pathol. 203, 631–637. https://doi.org/10.1002/path.1570 (2004).",
"volume": "203",
"year": "2004"
},
{
"DOI": "10.1186/s13054-020-03120-0",
"author": "W Ni",
"doi-asserted-by": "publisher",
"first-page": "422",
"journal-title": "Crit. Care",
"key": "78538_CR8",
"unstructured": "Ni, W. et al. Role of angiotensin-converting enzyme 2 (ACE2) in COVID-19. Crit. Care. 24, 422. https://doi.org/10.1186/s13054-020-03120-0 (2020).",
"volume": "24",
"year": "2020"
},
{
"DOI": "10.1111/cea.13746",
"author": "Y Yao",
"doi-asserted-by": "publisher",
"first-page": "1313",
"journal-title": "Clin. Exp. Allergy",
"key": "78538_CR9",
"unstructured": "Yao, Y., Wang, H. & Liu, Z. Expression of ACE2 in airways: implication for COVID-19 risk and disease management in patients with chronic inflammatory respiratory diseases. Clin. Exp. Allergy. 50, 1313–1324. https://doi.org/10.1111/cea.13746 (2020).",
"volume": "50",
"year": "2020"
},
{
"DOI": "10.1038/s41598-022-07918-6",
"author": "A Gheware",
"doi-asserted-by": "publisher",
"first-page": "4058",
"journal-title": "Sci. Rep.",
"key": "78538_CR10",
"unstructured": "Gheware, A. et al. ACE2 protein expression in lung tissues of severe COVID-19 infection. Sci. Rep. 12, 4058. https://doi.org/10.1038/s41598-022-07918-6 (2022).",
"volume": "12",
"year": "2022"
},
{
"DOI": "10.3389/fphys.2021.593223",
"author": "M Lopes-Pacheco",
"doi-asserted-by": "publisher",
"first-page": "593223",
"journal-title": "Front. Physiol.",
"key": "78538_CR11",
"unstructured": "Lopes-Pacheco, M. et al. Pathogenesis of multiple organ injury in COVID-19 and potential therapeutic strategies. Front. Physiol. 12, 593223. https://doi.org/10.3389/fphys.2021.593223 (2021).",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.17305/bjbms.2022.7762",
"author": "AA Rabaan",
"doi-asserted-by": "publisher",
"first-page": "37",
"journal-title": "Biomol. Biomed.",
"key": "78538_CR12",
"unstructured": "Rabaan, A. A. et al. SARS-CoV-2 infection and multi-organ system damage: a review. Biomol. Biomed. 23, 37–52. https://doi.org/10.17305/bjbms.2022.7762 (2023).",
"volume": "23",
"year": "2023"
},
{
"DOI": "10.1097/MD.0000000000030284",
"author": "S Singh",
"doi-asserted-by": "publisher",
"first-page": "e30284",
"journal-title": "Medicine",
"key": "78538_CR13",
"unstructured": "Singh, S. et al. Neurological infection and complications of SARS-CoV-2: a review. Medicine. 102, e30284. https://doi.org/10.1097/MD.0000000000030284 (2023).",
"volume": "102",
"year": "2023"
},
{
"DOI": "10.1056/NEJMc2008597",
"author": "J Helms",
"doi-asserted-by": "publisher",
"first-page": "2268",
"journal-title": "N Engl. J. Med.",
"key": "78538_CR14",
"unstructured": "Helms, J. et al. Neurologic features in severe SARS-CoV-2 infection. N Engl. J. Med. 382, 2268–2270. https://doi.org/10.1056/NEJMc2008597 (2020).",
"volume": "382",
"year": "2020"
},
{
"DOI": "10.1152/physrev.00012.2023",
"author": "T Tsukahara",
"doi-asserted-by": "publisher",
"first-page": "2759",
"issue": "4",
"journal-title": "Physiol. Rev.",
"key": "78538_CR15",
"unstructured": "Tsukahara, T., Brann, D. H. & Datta, S. R. Mechanisms of SARS-CoV-2-associated anosmia. Physiol. Rev. 103 (4), 2759–2766. https://doi.org/10.1152/physrev.00012.2023 (2023).",
"volume": "103",
"year": "2023"
},
{
"DOI": "10.1007/s00415-020-09929-7",
"author": "Z Zhou",
"doi-asserted-by": "publisher",
"first-page": "2179",
"journal-title": "J. Neurol.",
"key": "78538_CR16",
"unstructured": "Zhou, Z., Kang, H., Li, S. & Zhao, X. Understanding the neurotropic characteristics of SARS-CoV-2: from neurological manifestations of COVID-19 to potential neurotropic mechanisms. J. Neurol. 267, 2179–2184. https://doi.org/10.1007/s00415-020-09929-7 (2020).",
"volume": "267",
"year": "2020"
},
{
"DOI": "10.1021/acschemneuro.0c00122",
"author": "AM Baig",
"doi-asserted-by": "publisher",
"first-page": "995",
"journal-title": "ACS Chem. Neurosci.",
"key": "78538_CR17",
"unstructured": "Baig, A. M., Khaleeq, A., Ali, U. & Syeda, H. Evidence of the COVID-19 virus targeting the CNS: tissue distribution, host–virus interaction, and proposed neurotropic mechanisms. ACS Chem. Neurosci. 11, 995–998. https://doi.org/10.1021/acschemneuro.0c00122 (2020).",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.3389/fncel.2023.1125109",
"author": "H Hernández-Parra",
"doi-asserted-by": "publisher",
"first-page": "1125109",
"journal-title": "Front. Cell. Neurosci.",
"key": "78538_CR18",
"unstructured": "Hernández-Parra, H. et al. Alteration of the blood-brain barrier by COVID-19 and its implication in the permeation of drugs into the brain. Front. Cell. Neurosci. 17, 1125109. https://doi.org/10.3389/fncel.2023.1125109 (2023).",
"volume": "17",
"year": "2023"
},
{
"DOI": "10.1038/s41392-021-00719-9",
"author": "L Zhang",
"doi-asserted-by": "publisher",
"first-page": "337",
"journal-title": "Signal. Transduct. Target. Ther.",
"key": "78538_CR19",
"unstructured": "Zhang, L. et al. SARS-CoV-2 crosses the blood–brain barrier accompanied with basement membrane disruption without tight junctions alteration. Signal. Transduct. Target. Ther. 6, 337. https://doi.org/10.1038/s41392-021-00719-9 (2021).",
"volume": "6",
"year": "2021"
},
{
"DOI": "10.3389/fncel.2020.00229",
"author": "M Fenrich",
"doi-asserted-by": "publisher",
"first-page": "229",
"journal-title": "Front. Cell. Neurosci.",
"key": "78538_CR20",
"unstructured": "Fenrich, M. et al. SARS-CoV-2 dissemination through peripheral nerves explains multiple organ injury. Front. Cell. Neurosci. 14, 229. https://doi.org/10.3389/fncel.2020.00229 (2020).",
"volume": "14",
"year": "2020"
},
{
"DOI": "10.1111/jns.12482",
"author": "A Taga",
"doi-asserted-by": "publisher",
"first-page": "4",
"journal-title": "J. Peripher Nerv. Syst.",
"key": "78538_CR21",
"unstructured": "Taga, A. & Lauria, G. COVID-19 and the peripheral nervous system. A 2‐year review from the pandemic to the vaccine era. J. Peripher Nerv. Syst. 27, 4–30. https://doi.org/10.1111/jns.12482 (2022).",
"volume": "27",
"year": "2022"
},
{
"DOI": "10.1093/brain/awac270",
"author": "AL Soung",
"doi-asserted-by": "publisher",
"first-page": "4193",
"journal-title": "Brain",
"key": "78538_CR22",
"unstructured": "Soung, A. L. et al. COVID-19 induces CNS cytokine expression and loss of hippocampal neurogenesis. Brain. 145, 4193–4201. https://doi.org/10.1093/brain/awac270 (2022).",
"volume": "145",
"year": "2022"
},
{
"DOI": "10.3389/fmed.2021.745789",
"author": "MM Almutairi",
"doi-asserted-by": "publisher",
"first-page": "745789",
"journal-title": "Front. Med.",
"key": "78538_CR23",
"unstructured": "Almutairi, M. M., Sivandzade, F., Albekairi, T. H., Alqahtani, F. & Cucullo, L. Neuroinflammation and its impact on the Pathogenesis of COVID-19. Front. Med. 8, 745789. https://doi.org/10.3389/fmed.2021.745789 (2021).",
"volume": "8",
"year": "2021"
},
{
"DOI": "10.1038/s41423-023-01119-5",
"author": "SA Wellford",
"doi-asserted-by": "publisher",
"first-page": "134",
"journal-title": "Cell. Mol. Immunol.",
"key": "78538_CR24",
"unstructured": "Wellford, S. A. & Moseman, E. A. Olfactory immune response to SARS-CoV-2. Cell. Mol. Immunol. 21, 134–143. https://doi.org/10.1038/s41423-023-01119-5 (2023).",
"volume": "21",
"year": "2023"
},
{
"DOI": "10.1016/j.tins.2022.11.003",
"author": "R Butowt",
"doi-asserted-by": "publisher",
"first-page": "75",
"journal-title": "Trends Neurosci.",
"key": "78538_CR25",
"unstructured": "Butowt, R., Bilinska, K. & von Bartheld, C. S. Olfactory dysfunction in COVID-19: new insights into the underlying mechanisms. Trends Neurosci. 46, 75–90. https://doi.org/10.1016/j.tins.2022.11.003 (2023).",
"volume": "46",
"year": "2023"
},
{
"DOI": "10.1038/s41592-022-01447-w",
"author": "H Chu",
"doi-asserted-by": "publisher",
"first-page": "392",
"issue": "4",
"journal-title": "Nat. Methods",
"key": "78538_CR26",
"unstructured": "Chu, H., Chan, J. F. & Yuen, K. Y. Animal models in SARS-CoV-2 research. Nat. Methods. 19 (4), 392–394. https://doi.org/10.1038/s41592-022-01447-w (2022).",
"volume": "19",
"year": "2022"
},
{
"DOI": "10.1371/journal.pone.0272019",
"author": "SM Seo",
"doi-asserted-by": "publisher",
"first-page": "e0272019",
"journal-title": "PloS One",
"key": "78538_CR27",
"unstructured": "Seo, S. M. et al. Development of transgenic models susceptible and resistant to SARS-CoV-2 infection in FVB background mice. PloS One. 17, e0272019. https://doi.org/10.1371/journal.pone.0272019 (2022).",
"volume": "17",
"year": "2022"
},
{
"DOI": "10.1016/j.expneurol.2016.06.001",
"author": "CR Yu",
"doi-asserted-by": "publisher",
"first-page": "395",
"journal-title": "Exp. Neurol.",
"key": "78538_CR28",
"unstructured": "Yu, C. R. & Wu, Y. Regeneration and rewiring of rodent olfactory sensory neurons. Exp. Neurol. 287, 395–408. https://doi.org/10.1016/j.expneurol.2016.06.001 (2017).",
"volume": "287",
"year": "2017"
},
{
"DOI": "10.1186/s13024-022-00529-9",
"author": "R Butowt",
"doi-asserted-by": "publisher",
"first-page": "20",
"journal-title": "Mol. Neurodegener",
"key": "78538_CR29",
"unstructured": "Butowt, R. & von Bartheld, C. S. The route of SARS-CoV-2 to brain infection: have we been barking up the wrong tree? Mol. Neurodegener. 17, 20. https://doi.org/10.1186/s13024-022-00529-9 (2022).",
"volume": "17",
"year": "2022"
},
{
"DOI": "10.1021/acschemneuro.0c00434",
"author": "FJ Barrantes",
"doi-asserted-by": "publisher",
"first-page": "2793",
"journal-title": "ACS Chem. Neurosci.",
"key": "78538_CR30",
"unstructured": "Barrantes, F. J. Central nervous system targets and routes for SARS-CoV-2: current views and new hypotheses. ACS Chem. Neurosci. 11, 2793–2803. https://doi.org/10.1021/acschemneuro.0c00434 (2020).",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.31083/j.fbl2711316",
"author": "KAPP Kuruppuarachchi",
"doi-asserted-by": "publisher",
"first-page": "316",
"issue": "11",
"journal-title": "Front. Biosci.",
"key": "78538_CR31",
"unstructured": "Kuruppuarachchi, K. A. P. P., Jang, Y. & Seo, S. H. Comparison of the pathogenicity of SARS-CoV-2 delta and omicron variants by analyzing the expression patterns of immune response genes in K18-hACE2 transgenic mice. Front. Biosci. 27 (11), 316. https://doi.org/10.31083/j.fbl2711316 (2022).",
"volume": "27",
"year": "2022"
},
{
"DOI": "10.1055/s-0033-1361837",
"author": "CR Chen",
"doi-asserted-by": "publisher",
"first-page": "293",
"journal-title": "J. Neurol. Surg. B Skull Base",
"key": "78538_CR32",
"unstructured": "Chen, C. R., Kachramanoglou, C., Li, D., Andrews, P. & Choi, D. Anatomy and cellular constituents of the human olfactory mucosa: a review. J. Neurol. Surg. B Skull Base. 75, 293–300. https://doi.org/10.1055/s-0033-1361837 (2014).",
"volume": "75",
"year": "2014"
},
{
"DOI": "10.1186/1471-2202-12-86",
"author": "R Dooley",
"doi-asserted-by": "publisher",
"first-page": "86",
"journal-title": "BMC Neurosci.",
"key": "78538_CR33",
"unstructured": "Dooley, R., Mashukova, A., Toetter, B., Hatt, H. & Neuhaus, E. M. Purinergic receptor antagonists inhibit odorant-mediated CREB phosphorylation in sustentacular cells of mouse olfactory epithelium. BMC Neurosci. 12, 86. https://doi.org/10.1186/1471-2202-12-86 (2011).",
"volume": "12",
"year": "2011"
},
{
"DOI": "10.1007/s00441-021-03467-y",
"author": "B Bryche",
"doi-asserted-by": "publisher",
"first-page": "589",
"journal-title": "Cell. Tissue Res.",
"key": "78538_CR34",
"unstructured": "Bryche, B., Baly, C. & Meunier, N. Modulation of olfactory signal detection in the olfactory epithelium: focus on the internal and external environment, and the emerging role of the immune system. Cell. Tissue Res. 84, 589–605. https://doi.org/10.1007/s00441-021-03467-y (2021).",
"volume": "84",
"year": "2021"
},
{
"DOI": "10.1016/B978-0-12-381361-9.00006-8",
"doi-asserted-by": "crossref",
"key": "78538_CR35",
"unstructured": "Harkema, J. R. et al. Sinus, pharynx, and Larynx. in Comp. Anat. Histol. 71–94 (Elsevier, 2012)."
},
{
"DOI": "10.1186/s13064-017-0095-0",
"author": "X Shao",
"doi-asserted-by": "publisher",
"first-page": "18",
"journal-title": "Neural Dev.",
"key": "78538_CR36",
"unstructured": "Shao, X. et al. Olfactory sensory axons target specific protoglomeruli in the olfactory bulb of zebrafish. Neural Dev. 12, 18. https://doi.org/10.1186/s13064-017-0095-0 (2017).",
"volume": "12",
"year": "2017"
},
{
"DOI": "10.1080/13550280290049534",
"author": "A Matthews",
"doi-asserted-by": "publisher",
"first-page": "76",
"journal-title": "J. Neurovirol",
"key": "78538_CR37",
"unstructured": "Matthews, A., Weiss, S. & Paterson, Y. Murine Hepatitis virus–a model for virus-induced CNS demyelination. J. Neurovirol. 8, 76–85. https://doi.org/10.1080/13550280290049534 (2002).",
"volume": "8",
"year": "2002"
},
{
"DOI": "10.3389/fvets.2019.00053",
"author": "JC Mora-Díaz",
"doi-asserted-by": "publisher",
"first-page": "53",
"journal-title": "Front. Vet. Sci.",
"key": "78538_CR38",
"unstructured": "Mora-Díaz, J. C., Piñeyro, P. E., Houston, E., Zimmerman, J. & Giménez-Lirola, L. G. Porcine hemagglutinating encephalomyelitis virus: a review. Front. Vet. Sci. 6, 53. https://doi.org/10.3389/fvets.2019.00053 (2019).",
"volume": "6",
"year": "2019"
},
{
"DOI": "10.1007/s13760-020-01412-4",
"author": "K Verstrepen",
"doi-asserted-by": "publisher",
"first-page": "1051",
"journal-title": "Acta Neurol. Belg.",
"key": "78538_CR39",
"unstructured": "Verstrepen, K., Baisier, L. & De Cauwer, H. Neurological manifestations of COVID-19, SARS and MERS. Acta Neurol. Belg. 120, 1051–1060. https://doi.org/10.1007/s13760-020-01412-4 (2020).",
"volume": "120",
"year": "2020"
},
{
"DOI": "10.1002/path.4461",
"author": "D van Riel",
"doi-asserted-by": "publisher",
"first-page": "277",
"journal-title": "J. Pathol.",
"key": "78538_CR40",
"unstructured": "van Riel, D., Verdijk, R. & Kuiken, T. The olfactory nerve: a shortcut for influenza and other viral diseases into the central nervous system. J. Pathol. 235, 277–287. https://doi.org/10.1002/path.4461 (2015).",
"volume": "235",
"year": "2015"
},
{
"DOI": "10.1093/cid/ciaa995",
"author": "AJ Zhang",
"doi-asserted-by": "publisher",
"first-page": "e503",
"journal-title": "Clin. Infect. Dis.",
"key": "78538_CR41",
"unstructured": "Zhang, A. J. et al. Severe acute respiratory syndrome coronavirus 2 infects and damages the mature and immature olfactory sensory neurons of hamsters. Clin. Infect. Dis. 73, e503–e512. https://doi.org/10.1093/cid/ciaa995 (2021).",
"volume": "73",
"year": "2021"
},
{
"DOI": "10.1038/s41593-020-00758-5",
"author": "J Meinhardt",
"doi-asserted-by": "publisher",
"first-page": "168",
"journal-title": "Nat. Neurosci.",
"key": "78538_CR42",
"unstructured": "Meinhardt, J. et al. Olfactory transmucosal SARS-CoV-2 invasion as a port of central nervous system entry in individuals with COVID-19. Nat. Neurosci. 24, 168–175. https://doi.org/10.1038/s41593-020-00758-5 (2021).",
"volume": "24",
"year": "2021"
},
{
"DOI": "10.1172/jci.insight.160277",
"author": "AK Verma",
"doi-asserted-by": "publisher",
"first-page": "e160277",
"journal-title": "JCI Insight",
"key": "78538_CR43",
"unstructured": "Verma, A. K., Zheng, J., Meyerholz, D. K. & Perlman, S. SARS-CoV-2 infection of sustentacular cells disrupts olfactory signaling pathways. JCI Insight. 7, e160277. https://doi.org/10.1172/jci.insight.160277 (2022).",
"volume": "7",
"year": "2022"
},
{
"DOI": "10.1038/s41421-021-00290-1",
"author": "Q Ye",
"doi-asserted-by": "publisher",
"first-page": "49",
"journal-title": "Cell. Discov",
"key": "78538_CR44",
"unstructured": "Ye, Q. et al. SARS-CoV-2 infection in the mouse olfactory system. Cell. Discov. 7, 49. https://doi.org/10.1038/s41421-021-00290-1 (2021).",
"volume": "7",
"year": "2021"
},
{
"DOI": "10.1016/j.isci.2020.101839",
"author": "L Fodoulian",
"doi-asserted-by": "publisher",
"first-page": "101839",
"journal-title": "iScience",
"key": "78538_CR45",
"unstructured": "Fodoulian, L. et al. SARS-CoV-2 receptors and entry genes are expressed in the human olfactory neuroepithelium and brain. iScience. 23, 101839. https://doi.org/10.1016/j.isci.2020.101839 (2020).",
"volume": "23",
"year": "2020"
},
{
"DOI": "10.1126/scitranslmed.abf8396",
"author": "GD De Melo",
"doi-asserted-by": "publisher",
"first-page": "eabf8396",
"journal-title": "Sci. Transl Med.",
"key": "78538_CR46",
"unstructured": "De Melo, G. D. et al. COVID-19–related anosmia is associated with viral persistence and inflammation in human olfactory epithelium and brain infection in hamsters. Sci. Transl Med. 13, eabf8396. https://doi.org/10.1126/scitranslmed.abf8396 (2021).",
"volume": "13",
"year": "2021"
},
{
"DOI": "10.1084/jem.20202135",
"author": "E Song",
"doi-asserted-by": "publisher",
"first-page": "e20202135",
"journal-title": "J. Exp. Med.",
"key": "78538_CR47",
"unstructured": "Song, E. et al. Neuroinvasion of SARS-CoV-2 in human and mouse brain. J. Exp. Med. 218, e20202135. https://doi.org/10.1084/jem.20202135 (2021).",
"volume": "218",
"year": "2021"
},
{
"DOI": "10.3389/fncel.2021.789086",
"author": "S Prelic",
"doi-asserted-by": "publisher",
"first-page": "789086",
"journal-title": "Front. Cell. Neurosci.",
"key": "78538_CR48",
"unstructured": "Prelic, S. et al. Functional interaction between Drosophila olfactory sensory neurons and their support cells. Front. Cell. Neurosci. 15, 789086. https://doi.org/10.3389/fncel.2021.789086 (2022).",
"volume": "15",
"year": "2022"
},
{
"DOI": "10.1152/jn.01299.2004",
"author": "F Vogalis",
"doi-asserted-by": "publisher",
"first-page": "1001",
"journal-title": "J. Neurophysiol.",
"key": "78538_CR49",
"unstructured": "Vogalis, F., Hegg, C. C. & Lucero, M. T. Electrical coupling in sustentacular cells of the mouse olfactory epithelium. J. Neurophysiol. 94, 1001–1012. https://doi.org/10.1152/jn.01299.2004 (2005).",
"volume": "94",
"year": "2005"
}
],
"reference-count": 49,
"references-count": 49,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.nature.com/articles/s41598-024-78538-5"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"title": "Elimination of olfactory sensory neurons by zinc sulfate inoculation prevents SARS-CoV-2 infection of the brain in K18-hACE2 transgenic mice",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1007/springer_crossmark_policy",
"volume": "14"
}
