Clinical Outcome and Prognosis of a Nosocomial Outbreak of COVID-19
et al., Journal of Clinical Medicine, doi:10.3390/jcm12062279, Mar 2023
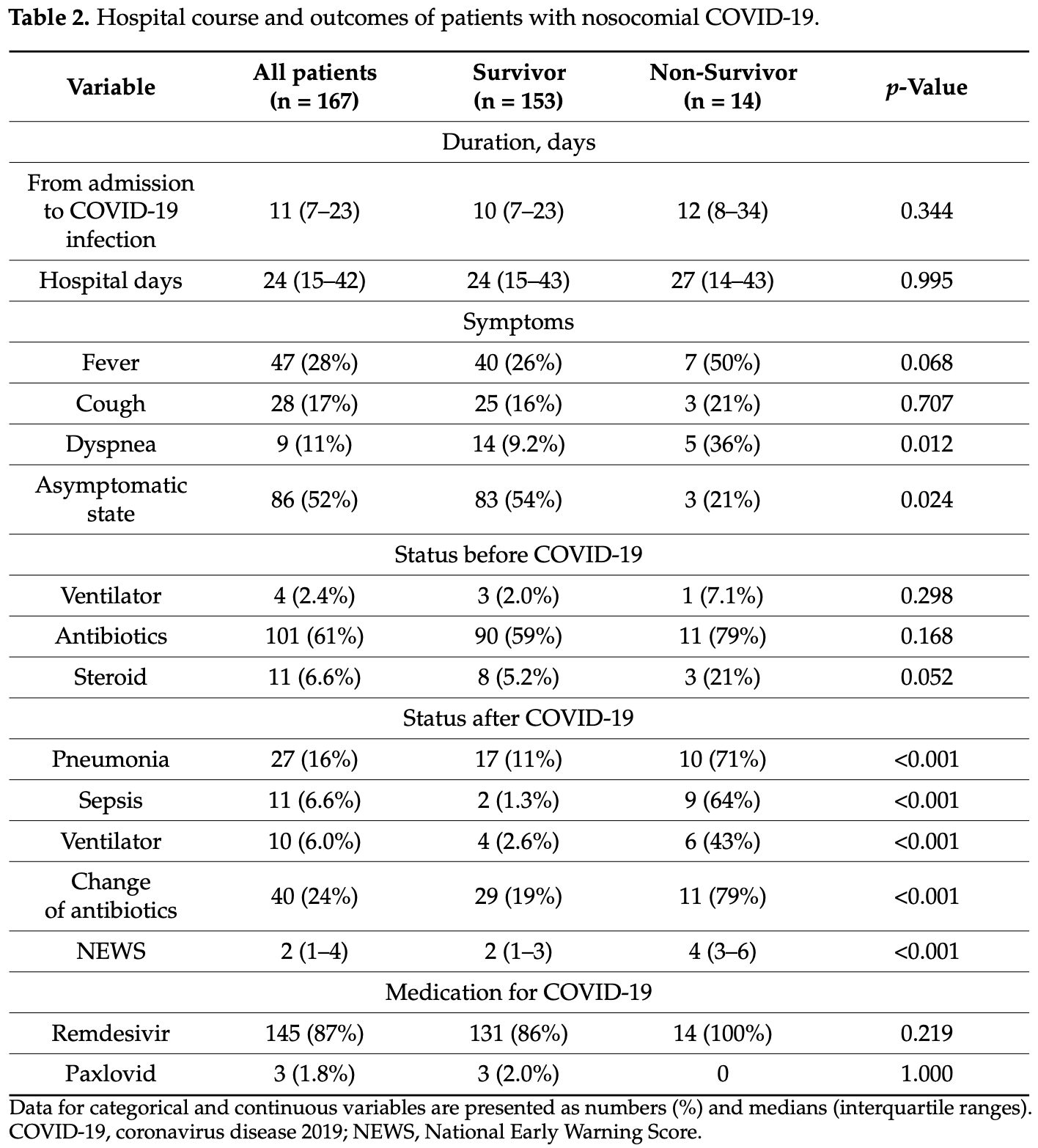
Retrospective 167 nosocomial COVID-19 patients in South Korea, showing higher mortality with remdesivir treatment, without statistical significance.
Gérard, Zhou, Wu, Kamo, Choi, Kim show increased risk of acute kidney injury, Leo, Briciu, Muntean, Petrov show increased risk of liver injury, and Negru, Cheng, Mohammed, Kwok show increased risk of cardiac disorders with remdesivir.
|
risk of death, 1612.4% higher, RR 17.12, p = 0.22, treatment 14 of 145 (9.7%), control 0 of 22 (0.0%), continuity correction due to zero event (with reciprocal of the contrasting arm).
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
1.
Gérard et al., Remdesivir and Acute Renal Failure: A Potential Safety Signal From Disproportionality Analysis of the WHO Safety Database, Clinical Pharmacology & Therapeutics, doi:10.1002/cpt.2145.
2.
Zhou et al., Acute Kidney Injury and Drugs Prescribed for COVID-19 in Diabetes Patients: A Real-World Disproportionality Analysis, Frontiers in Pharmacology, doi:10.3389/fphar.2022.833679.
3.
Wu et al., Acute Kidney Injury Associated With Remdesivir: A Comprehensive Pharmacovigilance Analysis of COVID-19 Reports in FAERS, Frontiers in Pharmacology, doi:10.3389/fphar.2022.692828.
4.
Kamo et al., Association of Antiviral Drugs for the Treatment of COVID-19 With Acute Renal Failure, In Vivo, doi:10.21873/invivo.13637.
5.
Choi et al., Comparative effectiveness of combination therapy with nirmatrelvir–ritonavir and remdesivir versus monotherapy with remdesivir or nirmatrelvir–ritonavir in patients hospitalised with COVID-19: a target trial emulation study, The Lancet Infectious Diseases, doi:10.1016/S1473-3099(24)00353-0.
6.
Kim et al., Investigating the Safety Profile of Fast‐Track COVID‐19 Drugs Using the FDA Adverse Event Reporting System Database: A Comparative Observational Study, Pharmacoepidemiology and Drug Safety, doi:10.1002/pds.70043.
7.
Leo et al., Hepatocellular liver injury in hospitalized patients affected by COVID-19: Presence of different risk factors at different time points, Digestive and Liver Disease, doi:10.1016/j.dld.2021.12.014.
8.
Briciu et al., Evolving Clinical Manifestations and Outcomes in COVID-19 Patients: A Comparative Analysis of SARS-CoV-2 Variant Waves in a Romanian Hospital Setting, Pathogens, doi:10.3390/pathogens12121453.
9.
Muntean et al., Effects of COVID-19 on the Liver and Mortality in Patients with SARS-CoV-2 Pneumonia Caused by Delta and Non-Delta Variants: An Analysis in a Single Centre, Pharmaceuticals, doi:10.3390/ph17010003.
10.
Petrov et al., The Effect of Potentially Hepatotoxic Medicinal Products on Alanine Transaminase Levels in COVID-19 Patients: A Case–Control Study, Safety and Risk of Pharmacotherapy, doi:10.30895/2312-7821-2025-458.
11.
Negru et al., Comparative Pharmacovigilance Analysis of Approved and Repurposed Antivirals for COVID-19: Insights from EudraVigilance Data, Biomedicines, doi:10.3390/biomedicines13061387.
12.
Cheng et al., Cardiovascular Safety of COVID-19 Treatments: A Disproportionality Analysis of Adverse Event Reports from the WHO VigiBase, Infectious Diseases and Therapy, doi:10.1007/s40121-025-01225-z.
Kim et al., 15 Mar 2023, retrospective, South Korea, peer-reviewed, 5 authors, study period 1 November, 2021 - 30 April, 2022.
Contact: sysliver@naver.com (corresponding author).
Clinical Outcome and Prognosis of a Nosocomial Outbreak of COVID-19
Journal of Clinical Medicine, doi:10.3390/jcm12062279
Nosocomial coronavirus disease 2019 (COVID-19) outbreaks have been reported despite widespread quarantine methods to prevent COVID-19 in society and hospitals. Our study was performed to investigate the clinical outcome and prognosis of a nosocomial outbreak of COVID-19. We retrospectively analyzed the medical records of patients diagnosed with nosocomial COVID-19 of severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) at a university teaching hospital between 1 November 2021 and 31 April 2022. Nosocomial COVID-19 was defined as a positive SARS-CoV-2 polymerase chain reaction (PCR) test result 4 or more days after admission in asymptomatic patients who had a negative SARS-CoV-2 PCR test on admission. In this study, 167 patients were diagnosed with nosocomial COVID-19 (1.14%) among a total of 14,667 patients admitted to hospital during the study period. A total of 153 patients (91.6%) survived, but 14 patients (8.4%) died. The median time between admission and COVID-19 diagnosis was 11 days, and the median duration of hospital stay was 24 days. After adjusting for other factors, no vaccination (adjusted HR = 5.944, 95% CI = 1.626-21.733, p = 0.007) and chronic kidney disease (adjusted HR = 6.963, 95% CI = 1.182-41.014, p = 0.032) were found to increase mortality risk. Despite strict quarantine, a significant number of nosocomial COVID-19 cases with a relatively high mortality rate were reported. As unvaccinated status or chronic kidney disease were associated with poor outcomes of nosocomial COVID-19, more active preventive strategies and treatments for patients with these risk factors are needed.
Informed Consent Statement: Informed consent was waived due to the retrospective nature of the study.
Conflicts of Interest: The authors declare no conflict of interest.
References
Baden, El Sahly, Essink, Kotloff, Frey et al., Efficacy and Safety of the mRNA-1273 SARS-CoV-2 Vaccine, N. Engl. J. Med, doi:10.1056/NEJMoa2035389
Biernat, Zi Ńczuk, Biernat, Bogucka-Fedorczuk, Kwiatkowski et al., Nosocomial outbreak of SARS-CoV-2 infection in a haematological unit-High mortality rate in infected patients with haematologic malignancies, J. Clin. Virol, doi:10.1016/j.jcv.2020.104574
Blackstone, Stirrup, Mapp, Panca, Copas et al., Protocol for the COG-UK hospital-onset COVID-19 infection (HOCI) multicentre interventional clinical study: Evaluating the efficacy of rapid genome sequencing of SARS-CoV-2 in limiting the spread of COVID-19 in UK NHS hospitals, BMJ Open
Borges, Isidro, Macedo, Neves, Silva et al., Nosocomial Outbreak of SARS-CoV-2 in a "Non-COVID-19" Hospital Ward: Virus Genome Sequencing as a Key Tool to Understand Cryptic Transmission, Viruses, doi:10.3390/v13040604
Boshier, Venturini, Stirrup, Guerra-Assunção, Alcolea-Medina et al., The Alpha variant was not associated with excess nosocomial SARS-CoV-2 infection in a multi-centre UK hospital study, J. Infect, doi:10.1016/j.jinf.2021.09.022
Carter, Collins, Barlow-Pay, Rickard, Bruce et al., Nosocomial COVID-19 infection: Examining the risk of mortality. The COPE-Nosocomial Study (COVID in Older PEople), J. Hosp. Infect, doi:10.1016/j.jhin.2020.07.013
Choi, COVID-19 in South Korea, Postgrad Med. J, doi:10.1136/postgradmedj-2020-137738
Eckart, Hauser, Kutz, Haubitz, Hausfater et al., Combination of the National Early Warning Score (NEWS) and inflammatory biomarkers for early risk stratification in emergency department patients: Results of a multinational, observational study, BMJ Open, doi:10.1136/bmjopen-2018-024636
Guan, Ni, Hu, Liang, Qu et al., Clinical Characteristics of coronavirus disease 2019 in China, N. Engl. J. Med, doi:10.1056/NEJMoa2002032
Hawkins, Pallett, Mazzella, Anton-Vazquez, Rosas et al., Transmission dynamics and associated mortality of nosocomial COVID-19 throughout 2021: A retrospective study at a large teaching hospital in London, J. Hosp. Infect, doi:10.1016/j.jhin.2022.12.014
Itoh, Akazawa, Ishikane, Kawabata, Kawamura et al., Lessons learned from an outbreak of COVID-19 in the head and neck surgery ward of a Japanese cancer center during the sixth wave by Omicron, J. Infect. Chemother, doi:10.1016/j.jiac.2022.08.010
Jang, Kim, Kim, Song, Moon et al., Are the Current Guidelines Sufficient to Establish Infection Control Strategies for COVID-19 Related Issues in Hospitals?, J. Korean Med. Sci, doi:10.3346/jkms.2021.36.e343
Jang, Kim, Moon, Kim, Lee, Correlation Between Third Dose of COVID-19 Vaccines and Regional Case Fatality Rates During the Omicron Wave in Korea, J. Korean Med. Sci, doi:10.3346/jkms.2022.37.e347
Jia, Gong, Will Mutations in the Spike Protein of SARS-CoV-2 Lead to the Failure of COVID-19 Vaccines?, J. Korean Med. Sci, doi:10.3346/jkms.2021.36.e124
Jia, Li, Li, Hou, Ma et al., Impact of Healthcare-Associated Infections on Length of Stay: A Study in 68 Hospitals in China, BioMed. Res. Int, doi:10.1155/2019/2590563
Jung, Lee, Park, Lim, Kim et al., Nosocomial Outbreak by Delta Variant from a Fully Vaccinated Patient, J. Korean Med. Sci, doi:10.3346/jkms.2022.37.e133
Kim, Choi, Jin, Choi, Lee et al., Predicting severe outcomes using national early warning score (NEWS) in patients identified by a rapid response system: A retrospective cohort study, Sci. Rep, doi:10.1038/s41598-021-97121-w
Kim, Kang, Lim, Lee, Kang et al., Comprehensive risk assessment for hospital-acquired pneumonia: Sociodemographic, clinical, and hospital environmental factors associated with the incidence of hospital-acquired pneumonia, BMC Pulm. Med, doi:10.1186/s12890-021-01816-9
Klompas, Pandolfi, Nisar, Baker, Rhee, Association of Omicron vs Wild-type SARS-CoV-2 Variants with Hospital-Onset SARS-CoV-2 Infections in a US Regional Hospital System, JAMA, doi:10.1001/jama.2022.9609
Kumar, Thambiraja, Karuppanan, Subramaniam, Omicron and Delta variant of SARS-CoV-2: A comparative computational study of spike protein, J. Med. Virol, doi:10.1002/jmv.27526
Kwon, Oh, COVID-19 vaccination program in South Korea: A long journey toward a new normal, Health Policy Technol, doi:10.1016/j.hlpt.2022.100601
Leducq, Couturier, Granger, Jolivet, Morand-Joubert et al., Investigation of healthcare-associated COVID-19 in a large French hospital group by whole-genome sequencing, Microbiol. Res, doi:10.1016/j.micres.2022.127133
Lee, Lee, Park, Choe, Song et al., Breakthrough COVID-19 Infection during the Delta Variant Dominant Period: Individualized Care Based on Vaccination Status Is Needed, J. Korean Med. Sci, doi:10.3346/jkms.2022.37.e252
Li, Peng, Li, Wang, Ping et al., Clinical and Transmission Characteristics of COVID-19-A Retrospective Study of 25 Cases from a Single Thoracic Surgery Department, Curr. Med. Sci
Luong-Nguyen, Hermand, Abdalla, Cabrit, Hobeika et al., Nosocomial infection with SARS-CoV-2 within Departments of Digestive Surgery, J. Visc. Surg, doi:10.1016/j.jviscsurg.2020.04.016
Meister, Pisarev, Kolde, Kalda, Suija et al., Clinical characteristics and risk factors for COVID-19 infection and disease severity: A nationwide observational study in Estonia, PLoS ONE, doi:10.1371/journal.pone.0270192
Nomura, Eguchi, Yoneoka, Kawashima, Tanoue et al., Reasons for being unsure or unwilling regarding intention to take COVID-19 vaccine among Japanese people: A large cross-sectional national survey, Lancet Reg. Health West. Pac, doi:10.1016/j.lanwpc.2021.100223
Nyberg, Ferguson, Nash, Webster, Flaxman et al., Comparative analysis of the risks of hospitalisation and death associated with SARS-CoV-2 omicron, Lancet, doi:10.1016/S0140-6736(22)00462-7
Paltansing, Sikkema, De Man, Koopmans, Munnink et al., Transmission of SARS-CoV-2 among healthcare workers and patients in a teaching hospital in The Netherlands confirmed by whole-genome sequencing, J. Hosp. Infect, doi:10.1016/j.jhin.2021.02.005
Ponsford, Jefferies, Davies, Farewell, Humphreys et al., Burden of nosocomial COVID-19 in Wales: Results from a multicentre retrospective observational study of 2508 hospitalised adults, Thorax, doi:10.1136/thoraxjnl-2021-216964
Rockett, Arnott, Lam, Sadsad, Timms et al., Revealing COVID-19 transmission in Australia by SARS-CoV-2 genome sequencing and agent-based modeling, Nat. Med, doi:10.1038/s41591-020-1000-7
Shi, Lee, Kang, Choi, Eom, Importance of Wearing Facial Masks to Prevent Nosocomial Transmissions of COVID-19, Korean J. Health Infect. Control. Prev, doi:10.14192/kjicp.2021.26.2.101
Sohn, Shin, Oh, Kim, Kim et al., Clinical Characteristics of Patients Who Contracted the SARS-CoV-2 Omicron Variant from an Outbreak in a Single Hospital, Yonsei Med. J, doi:10.3349/ymj.2022.63.8.790
Syed-Ahmed, Narayanan, Immune Dysfunction and Risk of Infection in Chronic Kidney Disease, Adv. Chronic Kidney Dis, doi:10.1053/j.ackd.2019.01.004
Thomas, Suresh, Assessment of COVID-19 prevention and protection measures in hospitals, Clean. Eng. Technol, doi:10.1016/j.clet.2022.100440
Wong, Chan, Yuen, Auyeung, Leung et al., Infection of healthcare workers despite a high vaccination rate during the fifth wave of COVID-19 due to Omicron variant in Hong Kong, Infect. Prev. Pr, doi:10.1016/j.infpip.2022.100261
Zhang, Xiao, Deng, Zhang, Zhuang et al., Transmission Dynamics of an Outbreak of the COVID-19 Delta Variant B.1.617.2-Guangdong Province, China, China CDC Wkly, doi:10.46234/ccdcw2021.148
Zhou, Gao, Wang, Liu, Du et al., Nosocomial infections among patients with COVID-19, SARS and MERS: A rapid review and meta-analysis, Ann. Transl. Med, doi:10.21037/atm-20-3324
DOI record:
{
"DOI": "10.3390/jcm12062279",
"ISSN": [
"2077-0383"
],
"URL": "http://dx.doi.org/10.3390/jcm12062279",
"abstract": "<jats:p>Nosocomial coronavirus disease 2019 (COVID-19) outbreaks have been reported despite widespread quarantine methods to prevent COVID-19 in society and hospitals. Our study was performed to investigate the clinical outcome and prognosis of a nosocomial outbreak of COVID-19. We retrospectively analyzed the medical records of patients diagnosed with nosocomial COVID-19 of severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) at a university teaching hospital between 1 November 2021 and 31 April 2022. Nosocomial COVID-19 was defined as a positive SARS-CoV-2 polymerase chain reaction (PCR) test result 4 or more days after admission in asymptomatic patients who had a negative SARS-CoV-2 PCR test on admission. In this study, 167 patients were diagnosed with nosocomial COVID-19 (1.14%) among a total of 14,667 patients admitted to hospital during the study period. A total of 153 patients (91.6%) survived, but 14 patients (8.4%) died. The median time between admission and COVID-19 diagnosis was 11 days, and the median duration of hospital stay was 24 days. After adjusting for other factors, no vaccination (adjusted HR = 5.944, 95% CI = 1.626–21.733, p = 0.007) and chronic kidney disease (adjusted HR = 6.963, 95% CI = 1.182–41.014, p = 0.032) were found to increase mortality risk. Despite strict quarantine, a significant number of nosocomial COVID-19 cases with a relatively high mortality rate were reported. As unvaccinated status or chronic kidney disease were associated with poor outcomes of nosocomial COVID-19, more active preventive strategies and treatments for patients with these risk factors are needed.</jats:p>",
"alternative-id": [
"jcm12062279"
],
"author": [
{
"ORCID": "http://orcid.org/0000-0002-0410-8524",
"affiliation": [
{
"name": "Division of Pulmonary, Allergy, and Critical Care Medicine, Department of Internal Medicine, Hallym University Kangnam Sacred Heart Hospital, Seoul 07441, Republic of Korea"
},
{
"name": "Lung Research Institute, Hallym University College of Medicine, Chuncheon 24252, Republic of Korea"
}
],
"authenticated-orcid": false,
"family": "Kim",
"given": "Sang Hyuk",
"sequence": "first"
},
{
"affiliation": [
{
"name": "Division of Pulmonary, Allergy, and Critical Care Medicine, Department of Internal Medicine, Hallym University Kangnam Sacred Heart Hospital, Seoul 07441, Republic of Korea"
},
{
"name": "Lung Research Institute, Hallym University College of Medicine, Chuncheon 24252, Republic of Korea"
}
],
"family": "Kim",
"given": "Taehee",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-4812-0653",
"affiliation": [
{
"name": "Division of Pulmonary, Allergy, and Critical Care Medicine, Department of Internal Medicine, Hallym University Kangnam Sacred Heart Hospital, Seoul 07441, Republic of Korea"
},
{
"name": "Lung Research Institute, Hallym University College of Medicine, Chuncheon 24252, Republic of Korea"
}
],
"authenticated-orcid": false,
"family": "Choi",
"given": "Hayoung",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Division of Pulmonary, Allergy, and Critical Care Medicine, Department of Internal Medicine, Hallym University Kangnam Sacred Heart Hospital, Seoul 07441, Republic of Korea"
},
{
"name": "Lung Research Institute, Hallym University College of Medicine, Chuncheon 24252, Republic of Korea"
}
],
"family": "Shin",
"given": "Tae Rim",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-3746-4947",
"affiliation": [
{
"name": "Division of Pulmonary, Allergy, and Critical Care Medicine, Department of Internal Medicine, Hallym University Kangnam Sacred Heart Hospital, Seoul 07441, Republic of Korea"
},
{
"name": "Lung Research Institute, Hallym University College of Medicine, Chuncheon 24252, Republic of Korea"
}
],
"authenticated-orcid": false,
"family": "Sim",
"given": "Yun Su",
"sequence": "additional"
}
],
"container-title": "Journal of Clinical Medicine",
"container-title-short": "JCM",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2023,
3,
15
]
],
"date-time": "2023-03-15T09:22:59Z",
"timestamp": 1678872179000
},
"deposited": {
"date-parts": [
[
2023,
3,
15
]
],
"date-time": "2023-03-15T12:18:08Z",
"timestamp": 1678882688000
},
"indexed": {
"date-parts": [
[
2023,
3,
16
]
],
"date-time": "2023-03-16T04:47:59Z",
"timestamp": 1678942079600
},
"is-referenced-by-count": 0,
"issue": "6",
"issued": {
"date-parts": [
[
2023,
3,
15
]
]
},
"journal-issue": {
"issue": "6",
"published-online": {
"date-parts": [
[
2023,
3
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
3,
15
]
],
"date-time": "2023-03-15T00:00:00Z",
"timestamp": 1678838400000
}
}
],
"link": [
{
"URL": "https://www.mdpi.com/2077-0383/12/6/2279/pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1968",
"original-title": [],
"page": "2279",
"prefix": "10.3390",
"published": {
"date-parts": [
[
2023,
3,
15
]
]
},
"published-online": {
"date-parts": [
[
2023,
3,
15
]
]
},
"publisher": "MDPI AG",
"reference": [
{
"DOI": "10.1056/NEJMoa2002032",
"article-title": "Clinical Characteristics of coronavirus disease 2019 in China",
"author": "Guan",
"doi-asserted-by": "crossref",
"first-page": "1708",
"journal-title": "N. Engl. J. Med.",
"key": "ref_1",
"volume": "382",
"year": "2020"
},
{
"DOI": "10.1016/j.clet.2022.100440",
"article-title": "Assessment of COVID-19 prevention and protection measures in hospitals",
"author": "Thomas",
"doi-asserted-by": "crossref",
"first-page": "100440",
"journal-title": "Clean. Eng. Technol.",
"key": "ref_2",
"volume": "7",
"year": "2022"
},
{
"DOI": "10.3346/jkms.2021.36.e343",
"article-title": "Are the Current Guidelines Sufficient to Establish Infection Control Strategies for COVID-19 Related Issues in Hospitals?",
"author": "Jang",
"doi-asserted-by": "crossref",
"first-page": "e343",
"journal-title": "J. Korean Med. Sci.",
"key": "ref_3",
"volume": "36",
"year": "2021"
},
{
"DOI": "10.14192/kjicp.2021.26.2.101",
"article-title": "Importance of Wearing Facial Masks to Prevent Nosocomial Transmissions of COVID-19",
"author": "Shi",
"doi-asserted-by": "crossref",
"first-page": "101",
"journal-title": "Korean J. Health Infect. Control. Prev.",
"key": "ref_4",
"volume": "26",
"year": "2021"
},
{
"DOI": "10.1016/j.jcv.2020.104574",
"article-title": "Nosocomial outbreak of SARS-CoV-2 infection in a haematological unit—High mortality rate in infected patients with haematologic malignancies",
"author": "Biernat",
"doi-asserted-by": "crossref",
"first-page": "104574",
"journal-title": "J. Clin. Virol.",
"key": "ref_5",
"volume": "130",
"year": "2020"
},
{
"DOI": "10.1016/j.jhin.2020.07.013",
"article-title": "Nosocomial COVID-19 infection: Examining the risk of mortality. The COPE-Nosocomial Study (COVID in Older PEople)",
"author": "Carter",
"doi-asserted-by": "crossref",
"first-page": "376",
"journal-title": "J. Hosp. Infect.",
"key": "ref_6",
"volume": "106",
"year": "2020"
},
{
"DOI": "10.1016/j.jviscsurg.2020.04.016",
"article-title": "Nosocomial infection with SARS-CoV-2 within Departments of Digestive Surgery",
"author": "Hermand",
"doi-asserted-by": "crossref",
"first-page": "S13",
"journal-title": "J. Visc. Surg.",
"key": "ref_7",
"volume": "157",
"year": "2020"
},
{
"DOI": "10.21037/atm-20-3324",
"article-title": "Nosocomial infections among patients with COVID-19, SARS and MERS: A rapid review and meta-analysis",
"author": "Zhou",
"doi-asserted-by": "crossref",
"first-page": "629",
"journal-title": "Ann. Transl. Med.",
"key": "ref_8",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1101/2021.02.20.20248421",
"doi-asserted-by": "crossref",
"key": "ref_9",
"unstructured": "Borges, V., Isidro, J., Macedo, F., Neves, J., Silva, L., Paiva, M., Barata, J., Catarino, J., Ciobanu, L., and Duarte, S. (2021). Nosocomial Outbreak of SARS-CoV-2 in a “Non-COVID-19” Hospital Ward: Virus Genome Sequencing as a Key Tool to Understand Cryptic Transmission. Viruses, 13."
},
{
"DOI": "10.1016/j.jinf.2021.09.022",
"article-title": "The Alpha variant was not associated with excess nosocomial SARS-CoV-2 infection in a multi-centre UK hospital study",
"author": "Boshier",
"doi-asserted-by": "crossref",
"first-page": "693",
"journal-title": "J. Infect.",
"key": "ref_10",
"volume": "83",
"year": "2021"
},
{
"DOI": "10.1016/j.jhin.2021.02.005",
"article-title": "Transmission of SARS-CoV-2 among healthcare workers and patients in a teaching hospital in The Netherlands confirmed by whole-genome sequencing",
"author": "Paltansing",
"doi-asserted-by": "crossref",
"first-page": "178",
"journal-title": "J. Hosp. Infect.",
"key": "ref_11",
"volume": "110",
"year": "2021"
},
{
"DOI": "10.1136/thoraxjnl-2021-216964",
"article-title": "Burden of nosocomial COVID-19 in Wales: Results from a multicentre retrospective observational study of 2508 hospitalised adults",
"author": "Ponsford",
"doi-asserted-by": "crossref",
"first-page": "1246",
"journal-title": "Thorax",
"key": "ref_12",
"volume": "76",
"year": "2021"
},
{
"DOI": "10.46234/ccdcw2021.148",
"article-title": "Transmission Dynamics of an Outbreak of the COVID-19 Delta Variant B.1.617.2—Guangdong Province, China, May–June 2021",
"author": "Zhang",
"doi-asserted-by": "crossref",
"first-page": "584",
"journal-title": "China CDC Wkly.",
"key": "ref_13",
"volume": "3",
"year": "2021"
},
{
"DOI": "10.1016/j.jiac.2022.08.010",
"article-title": "Lessons learned from an outbreak of COVID-19 in the head and neck surgery ward of a Japanese cancer center during the sixth wave by Omicron",
"author": "Itoh",
"doi-asserted-by": "crossref",
"first-page": "1610",
"journal-title": "J. Infect. Chemother.",
"key": "ref_14",
"volume": "28",
"year": "2022"
},
{
"DOI": "10.3346/jkms.2022.37.e133",
"article-title": "Nosocomial Outbreak by Delta Variant from a Fully Vaccinated Patient",
"author": "Jung",
"doi-asserted-by": "crossref",
"first-page": "e133",
"journal-title": "J. Korean Med. Sci.",
"key": "ref_15",
"volume": "37",
"year": "2022"
},
{
"DOI": "10.3349/ymj.2022.63.8.790",
"article-title": "Clinical Characteristics of Patients Who Contracted the SARS-CoV-2 Omicron Variant from an Outbreak in a Single Hospital",
"author": "Sohn",
"doi-asserted-by": "crossref",
"first-page": "790",
"journal-title": "Yonsei Med. J.",
"key": "ref_16",
"volume": "63",
"year": "2022"
},
{
"DOI": "10.1016/j.jhin.2022.12.014",
"article-title": "Transmission dynamics and associated mortality of nosocomial COVID-19 throughout 2021: A retrospective study at a large teaching hospital in London",
"author": "Hawkins",
"doi-asserted-by": "crossref",
"first-page": "62",
"journal-title": "J. Hosp. Infect.",
"key": "ref_17",
"volume": "133",
"year": "2023"
},
{
"article-title": "Infection of healthcare workers despite a high vaccination rate during the fifth wave of COVID-19 due to Omicron variant in Hong Kong",
"author": "Wong",
"first-page": "e124",
"journal-title": "Infect. Prev. Pr.",
"key": "ref_18",
"volume": "5",
"year": "2023"
},
{
"DOI": "10.3346/jkms.2021.36.e124",
"article-title": "Will Mutations in the Spike Protein of SARS-CoV-2 Lead to the Failure of COVID-19 Vaccines?",
"author": "Jia",
"doi-asserted-by": "crossref",
"first-page": "e124",
"journal-title": "J. Korean Med. Sci.",
"key": "ref_19",
"volume": "36",
"year": "2021"
},
{
"DOI": "10.1002/jmv.27526",
"article-title": "Omicron and Delta variant of SARS-CoV-2: A comparative computational study of spike protein",
"author": "Kumar",
"doi-asserted-by": "crossref",
"first-page": "1641",
"journal-title": "J. Med. Virol.",
"key": "ref_20",
"volume": "94",
"year": "2022"
},
{
"DOI": "10.3346/jkms.2022.37.e347",
"article-title": "Correlation Between Third Dose of COVID-19 Vaccines and Regional Case Fatality Rates During the Omicron Wave in Korea",
"author": "Jang",
"doi-asserted-by": "crossref",
"first-page": "e347",
"journal-title": "J. Korean Med. Sci.",
"key": "ref_21",
"volume": "37",
"year": "2022"
},
{
"key": "ref_22",
"unstructured": "Statistics Korea (2022, December 01). COVID-19 Dashboard. Available online: http://kosis.kr/covid/covid_index.do."
},
{
"DOI": "10.1007/s11596-020-2176-2",
"article-title": "Clinical and Transmission Characteristics of COVID-19—A Retrospective Study of 25 Cases from a Single Thoracic Surgery Department",
"author": "Li",
"doi-asserted-by": "crossref",
"first-page": "295",
"journal-title": "Curr. Med. Sci.",
"key": "ref_23",
"volume": "40",
"year": "2020"
},
{
"DOI": "10.1016/j.micres.2022.127133",
"article-title": "Investigation of healthcare-associated COVID-19 in a large French hospital group by whole-genome sequencing",
"author": "Leducq",
"doi-asserted-by": "crossref",
"first-page": "127133",
"journal-title": "Microbiol. Res.",
"key": "ref_24",
"volume": "263",
"year": "2022"
},
{
"DOI": "10.1001/jama.2022.9609",
"article-title": "Association of Omicron vs Wild-type SARS-CoV-2 Variants with Hospital-Onset SARS-CoV-2 Infections in a US Regional Hospital System",
"author": "Klompas",
"doi-asserted-by": "crossref",
"first-page": "296",
"journal-title": "JAMA",
"key": "ref_25",
"volume": "328",
"year": "2022"
},
{
"DOI": "10.1136/bmjopen-2018-024636",
"article-title": "Combination of the National Early Warning Score (NEWS) and inflammatory biomarkers for early risk stratification in emergency department patients: Results of a multinational, observational study",
"author": "Eckart",
"doi-asserted-by": "crossref",
"first-page": "e024636",
"journal-title": "BMJ Open",
"key": "ref_26",
"volume": "9",
"year": "2019"
},
{
"DOI": "10.1136/postgradmedj-2020-137738",
"article-title": "COVID-19 in South Korea",
"author": "Choi",
"doi-asserted-by": "crossref",
"first-page": "399",
"journal-title": "Postgrad Med. J.",
"key": "ref_27",
"volume": "96",
"year": "2020"
},
{
"DOI": "10.1016/S0140-6736(22)00462-7",
"article-title": "Comparative analysis of the risks of hospitalisation and death associated with SARS-CoV-2 omicron (B.1.1.529) and delta (B.1.617.2) variants in England: A cohort study",
"author": "Nyberg",
"doi-asserted-by": "crossref",
"first-page": "1303",
"journal-title": "Lancet",
"key": "ref_28",
"volume": "399",
"year": "2022"
},
{
"DOI": "10.1186/s12890-021-01816-9",
"doi-asserted-by": "crossref",
"key": "ref_29",
"unstructured": "Kim, B.-G., Kang, M., Lim, J., Lee, J., Kang, D., Kim, M., Kim, J., Park, H., Min, K.H., and Cho, J. (2022). Comprehensive risk assessment for hospital-acquired pneumonia: Sociodemographic, clinical, and hospital environmental factors associated with the incidence of hospital-acquired pneumonia. BMC Pulm. Med., 22."
},
{
"article-title": "Predicting severe outcomes using national early warning score (NEWS) in patients identified by a rapid response system: A retrospective cohort study",
"author": "Kim",
"first-page": "1",
"journal-title": "Sci. Rep.",
"key": "ref_30",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.1155/2019/2590563",
"article-title": "Impact of Healthcare-Associated Infections on Length of Stay: A Study in 68 Hospitals in China",
"author": "Jia",
"doi-asserted-by": "crossref",
"first-page": "2590563",
"journal-title": "BioMed. Res. Int.",
"key": "ref_31",
"volume": "2019",
"year": "2019"
},
{
"DOI": "10.1016/j.hlpt.2022.100601",
"article-title": "COVID-19 vaccination program in South Korea: A long journey toward a new normal",
"author": "Kwon",
"doi-asserted-by": "crossref",
"first-page": "100601",
"journal-title": "Health Policy Technol.",
"key": "ref_32",
"volume": "11",
"year": "2022"
},
{
"DOI": "10.3346/jkms.2022.37.e252",
"doi-asserted-by": "crossref",
"key": "ref_33",
"unstructured": "Lee, C.M., Lee, E., Park, W.B., Choe, P.G., Song, K.-H., Kim, E.S., and Park, S.-W. (2022). Breakthrough COVID-19 Infection during the Delta Variant Dominant Period: Individualized Care Based on Vaccination Status Is Needed. J. Korean Med. Sci., 37."
},
{
"DOI": "10.1016/j.lanwpc.2021.100223",
"article-title": "Reasons for being unsure or unwilling regarding intention to take COVID-19 vaccine among Japanese people: A large cross-sectional national survey",
"author": "Nomura",
"doi-asserted-by": "crossref",
"first-page": "100223",
"journal-title": "Lancet Reg. Health West. Pac.",
"key": "ref_34",
"volume": "14",
"year": "2021"
},
{
"DOI": "10.1371/journal.pone.0270192",
"doi-asserted-by": "crossref",
"key": "ref_35",
"unstructured": "Meister, T., Pisarev, H., Kolde, R., Kalda, R., Suija, K., Milani, L., Karo-Astover, L., Piirsoo, M., and Uusküla, A. (2022). Clinical characteristics and risk factors for COVID-19 infection and disease severity: A nationwide observational study in Estonia. PLoS ONE, 17."
},
{
"DOI": "10.1056/NEJMoa2035389",
"article-title": "Efficacy and Safety of the mRNA-1273 SARS-CoV-2 Vaccine",
"author": "Baden",
"doi-asserted-by": "crossref",
"first-page": "403",
"journal-title": "N. Engl. J. Med.",
"key": "ref_36",
"volume": "384",
"year": "2021"
},
{
"DOI": "10.1053/j.ackd.2019.01.004",
"article-title": "Immune Dysfunction and Risk of Infection in Chronic Kidney Disease",
"author": "Narayanan",
"doi-asserted-by": "crossref",
"first-page": "8",
"journal-title": "Adv. Chronic Kidney Dis.",
"key": "ref_37",
"volume": "26",
"year": "2019"
},
{
"DOI": "10.1038/s41591-020-1000-7",
"article-title": "Revealing COVID-19 transmission in Australia by SARS-CoV-2 genome sequencing and agent-based modeling",
"author": "Rockett",
"doi-asserted-by": "crossref",
"first-page": "1398",
"journal-title": "Nat. Med.",
"key": "ref_38",
"volume": "26",
"year": "2020"
},
{
"DOI": "10.1136/bmjopen-2021-052514",
"article-title": "Protocol for the COG-UK hospital-onset COVID-19 infection (HOCI) multicentre interventional clinical study: Evaluating the efficacy of rapid genome sequencing of SARS-CoV-2 in limiting the spread of COVID-19 in UK NHS hospitals",
"author": "Blackstone",
"doi-asserted-by": "crossref",
"first-page": "e052514",
"journal-title": "BMJ Open",
"key": "ref_39",
"volume": "12",
"year": "2022"
}
],
"reference-count": 39,
"references-count": 39,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.mdpi.com/2077-0383/12/6/2279"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"General Medicine"
],
"subtitle": [],
"title": "Clinical Outcome and Prognosis of a Nosocomial Outbreak of COVID-19",
"type": "journal-article",
"volume": "12"
}