In-hospital adverse outcomes and risk factors among chronic kidney disease patients infected with the omicron variant of SARS-CoV-2: a single-center retrospective study
et al., BMC Infectious Diseases, doi:10.1186/s12879-023-08620-2, Oct 2023
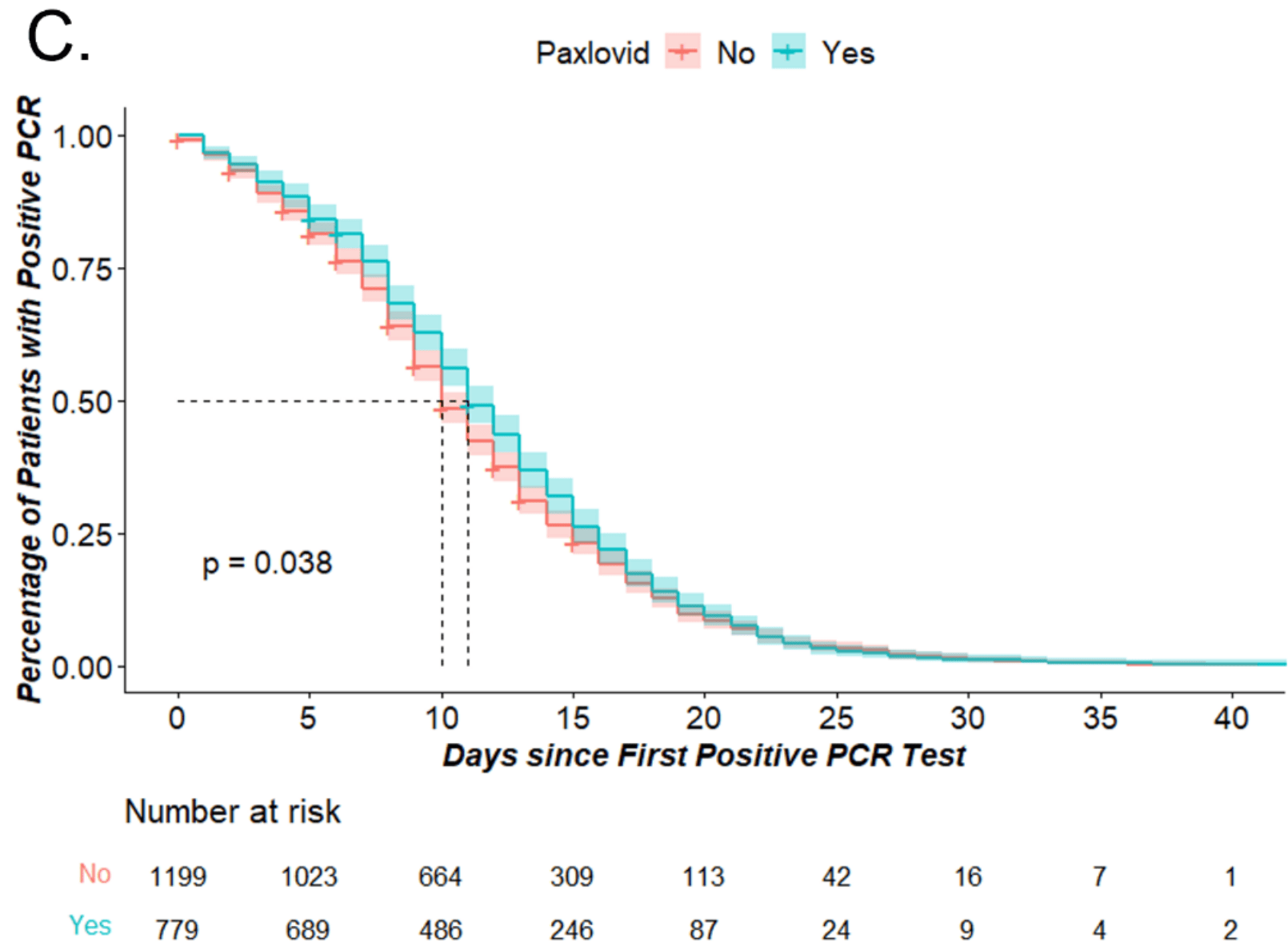
Retrospective 1,978 hospitalized patients in China, showing slower viral clearance with Paxlovid. Authors note improved results in the subgroup of non-severe patients with CKD.
Resistance. Variants may be resistant to paxlovid1-8. Use may promote the emergence of variants that weaken host immunity and potentially contribute to long COVID9. Confounding by contraindication. Hoertel et al. find that over 50% of patients that died had a contraindication for the use of Paxlovid10. Retrospective studies that do not exclude contraindicated patients may significantly overestimate efficacy. Black box warning. The FDA notes that severe, life-threatening, and/or fatal adverse reactions due to drug interactions have been reported in patients treated with paxlovid11. Kidney and liver injury. Studies show significantly increased risk of acute kidney injury12 and liver injury13,14. Viral rebound. Studies show significantly increased risk of replication-competent viral rebound15-17.
Standard of Care (SOC) for COVID-19 in the study country,
China, is average with moderate efficacy for approved treatments18.
|
time to viral-, 10.0% higher, relative time 1.10, p = 0.04, treatment 779, control 1,199, median time of positive-to-negative conversion.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
1.
Zhou et al., Nirmatrelvir-resistant SARS-CoV-2 variants with high fitness in an infectious cell culture system, Science Advances, doi:10.1126/sciadv.add7197.
2.
Moghadasi et al., Rapid resistance profiling of SARS-CoV-2 protease inhibitors, npj Antimicrobials and Resistance, doi:10.1038/s44259-023-00009-0.
3.
Jochmans et al., The Substitutions L50F, E166A, and L167F in SARS-CoV-2 3CLpro Are Selected by a Protease Inhibitor In Vitro and Confer Resistance To Nirmatrelvir, mBio, doi:10.1128/mbio.02815-22.
4.
Lopez et al., SARS-CoV-2 Resistance to Small Molecule Inhibitors, Current Clinical Microbiology Reports, doi:10.1007/s40588-024-00229-6.
5.
Zvornicanin et al., Molecular Mechanisms of Drug Resistance and Compensation in SARS-CoV-2 Main Protease: The Interplay Between E166 and L50, bioRxiv, doi:10.1101/2025.01.24.634813.
6.
Vukovikj et al., Impact of SARS-CoV-2 variant mutations on susceptibility to monoclonal antibodies and antiviral drugs: a non-systematic review, April 2022 to October 2024, Eurosurveillance, doi:10.2807/1560-7917.ES.2025.30.10.2400252.
7.
Deschenes et al., Functional and structural characterization of treatment-emergent nirmatrelvir resistance mutations at low frequencies in the main protease (Mpro) reveals a unique evolutionary route for SARS-CoV-2 to gain resistance, The Journal of Infectious Diseases, doi:10.1093/infdis/jiaf294.
8.
Zhou (B) et al., SARS-CoV-2 Mpro inhibitor ensitrelvir: asymmetrical cross-resistance with nirmatrelvir and emerging resistance hotspots, Emerging Microbes & Infections, doi:10.1080/22221751.2025.2552716.
9.
Thomas et al., Nirmatrelvir-Resistant Mutations in SARS-CoV-2 Mpro Enhance Host Immune Evasion via Cleavage of NF-κB Essential Modulator, bioRxiv, doi:10.1101/2024.10.18.619137.
10.
Hoertel et al., Prevalence of Contraindications to Nirmatrelvir-Ritonavir Among Hospitalized Patients With COVID-19 at Risk for Progression to Severe Disease, JAMA Network Open, doi:10.1001/jamanetworkopen.2022.42140.
11.
FDA, Fact sheet for healthcare providers: emergency use authorization for paxlovid, www.fda.gov/media/155050/download.
12.
Kamo et al., Association of Antiviral Drugs for the Treatment of COVID-19 With Acute Renal Failure, In Vivo, doi:10.21873/invivo.13637.
13.
Wang et al., Development and validation of a nomogram to assess the occurrence of liver dysfunction in patients with COVID-19 pneumonia in the ICU, BMC Infectious Diseases, doi:10.1186/s12879-025-10684-1.
14.
Siby et al., Temporal Trends in Serious Adverse Events Associated with Oral Antivirals During the COVID-19 Pandemic: Insights from the FAERS Database (2020–2023), Open Forum Infectious Diseases, doi:10.1093/ofid/ofaf695.1825.
15.
Edelstein et al., SARS-CoV-2 virologic rebound with nirmatrelvir-ritonavir therapy, medRxiv, doi:10.1101/2023.06.23.23288598.
16.
Shah et al., SARS-CoV-2 infectious shedding and rebound among adults with and without oral antiviral use: two case-ascertained prospective household studies, The Lancet Microbe, doi:10.1016/j.lanmic.2025.101227.
Guo et al., 18 Oct 2023, retrospective, China, peer-reviewed, median age 73.0, 18 authors, study period 29 March, 2022 - 17 May, 2022.
Contact: haoxiangzhu2015@163.com, richengmao@gmail.com, xuejun@fudan.edu.cn, jmzhang@fudan.edu.cn.
In-hospital adverse outcomes and risk factors among chronic kidney disease patients infected with the omicron variant of SARS-CoV-2: a single-center retrospective study
BMC Infectious Diseases, doi:10.1186/s12879-023-08620-2
Introduction The SARS-CoV-2 Omicron variant has decreased virulence and pathogenicity, yet the number of Omicron infections worldwide is unprecedentedly high, with rather high mortality and severe disease rate. Chronic kidney disease (CKD) patients are particularly vulnerable to the SARS-CoV-2 Omicron variant and have unique clinical outcomes.
Methods We retrospectively collected data from 2140 hospitalized patients with SARS-CoV-2 Omicron variant infection from March 29, 2022, to May 17, 2022. Demographic characteristics, ancillary examination results, and clinical treatments were described. Occurrence of critical COVID-19 or death and time of positive-to-negative conversion was defined as primary outcomes. The presence of COVID-19 pneumonia and the usage of respiratory or circulatory support was defined as secondary outcomes. Univariate or multivariate logistic regression analyses were performed to identify risk factors for primary outcomes. Results 15.74% of CKD patients infected with the SARS-CoV-2 Omicron variant ended up with critical COVID-19 or death. Pre-existing CKD was a risk factor for critical COVID-19 or death and prolonged time of positive-to-negative conversion of SARS-CoV-2. Nirmatrelvir-ritonavir facilitated viral clearance among COVID-19 patients with non-severe CKD.
Abbreviations
Supplementary Information The online version contains supplementary material available at https://doi. org/10.1186/s12879-023-08620-2.
Supplementary Material 1
Authors' contributions
Declarations Ethics approval and consent to participate Ethical approval was obtained from the Ethics Review Board of the Huashan Hospital, Fudan University (ethics approval registration number: KY2022-582). Informed consent forms were signed by each patient.All methods were carried out in accordance with relevant guidelines and regulations.
Consent for publication Not applicable.
Competing interests The authors declare no competing interests.
Publisher's Note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Amani, Amani, Efficacy and safety of nirmatrelvir/ritonavir (paxlovid) for COVID-19: a rapid review and meta-analysis, J Med Virol
Ao, Li, Wei, Wang, Tian et al., Clinical and virological characteristics of SARS-CoV-2 Omicron BA.2.2 variant outbreaks during April to May, 2022, Shanghai, China, J Infect
Broseta, Rodriguez-Espinosa, Cuadrado, Guillen-Olmos, Hermida et al., SARS-CoV-2 infection in a spanish cohort of CKD-5D patients: prevalence, clinical presentation, outcomes, and De-Isolation results, Blood Purif
Buetti, Trimboli, Mazzuchelli, Lo Priore, Balmelli et al., Diabetes mellitus is a risk factor for prolonged SARS-CoV-2 viral shedding in lower respiratory tract samples of critically ill patients, Endocrine
Cai, Yan, Liu, Li, Ding et al., Paxlovid for hospitalized COVID-19 patients with chronic kidney disease, Antiviral Res
Cai, Yan, Wang, Mou, Efficacy of Paxlovid in patients with acute kidney injury who developed COVID-19, J Infect
Caillard, Laugel, Benotmane, Kremer, Molecular evolution of the SARS-CoV-2 omicron BA.2 variant in kidney transplant recipients with prolonged viral shedding, J Infect
Chen, Wang, Ai, Shen, Lin et al., Identification of CKD, bedridden history and cancer as higher-risk comorbidities and their impact on prognosis of hospitalized Omicron patients: a multicentre cohort study, Emerg Microbes Infect
Chung, Palmer, Natale, Krishnan, Cooper et al., Incidence and outcomes of COVID-19 in people with CKD: a systematic review and Meta-analysis, Am J Kidney Dis
Danthu, Hantz, Dahlem, Duval, Ba et al., Humoral response after SARS-CoV-2 mRNA vaccination in a cohort of Hemodialysis patients and kidney transplant recipients, J Am Soc Nephrol
Devresse, Sebastien, Greef, Lemaitre, Boland et al., Safety, Efficacy, and relapse of nirmatrelvir-ritonavir in kidney transplant recipients infected with SARS-CoV-2, Kidney Int Rep
Flythe, Assimon, Tugman, Chang, Gupta et al., Characteristics and outcomes of individuals with pre-existing kidney disease and COVID-19 admitted to Intensive Care Units in the United States, Am J Kidney Dis
Gao, Zhu, Jin, Tong, Xiao et al., Proinflammatory cytokines are associated with prolonged viral RNA shedding in COVID-19 patients, Clin Immunol
Hao, Lian, Lu, Jia, Hu et al., Decreased B cells on Admission Associated with prolonged viral RNA shedding from the respiratory tract in Coronavirus Disease 2019: a case-control study, J Infect Dis
Kaso, Hareru, Kaso, Agero, Factors Associated with Poor Treatment Outcome among Hospitalized COVID-19 Patients in South Central, Ethiopia, Biomed Res Int
Kim, Lee, Choi, Um, Lee et al., Clinical characteristics of 40 patients infected with the SARS-CoV-2 Omicron variant in Korea, J Korean Med Sci
Lee, Tay, Sutjipto, Fong, Ong et al., Associations of viral ribonucleic acid (RNA) shedding patterns with clinical illness and immune responses in severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) infection, Clin Transl Immunology
Li, Liao, Zhou, Wang, Yang et al., Association between glucocorticoids treatment and viral clearance delay in patients with COVID-19: a systematic review and meta-analysis, BMC Infect Dis
Mahalingasivam, Su, Iwagami, Davids, Wetmore et al., COVID-19 and kidney disease: insights from epidemiology to inform clinical practice, Nat Rev Nephrol
Meiring, Tempia, Bhiman, Buys, Kleynhans et al., Prolonged shedding of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) at high viral loads among hospitalized immunocompromised persons living with Human Immunodeficiency Virus (HIV), South Africa, Clin Infect Dis
Nakajima, Ogai, Furukawa, Arai, Anan et al., Prolonged viral shedding of SARS-CoV-2 in an immunocompromised patient, J Infect Chemother
Pei, Chen, Zheng, Gong, Liu et al., Comorbidities prolonged viral shedding of patients infected with SARS-CoV-2 omicron variant in Shanghai: a multi-center, retrospective, observational study, J Infect Public Health
Planas, Saunders, Maes, Guivel-Benhassine, Planchais et al., Considerable escape of SARS-CoV-2 Omicron to antibody neutralization, Nature
Shaikh, Zeldis, Campbell, Chan, Prolonged SARS-CoV-2 viral RNA shedding and IgG antibody response to SARS-CoV-2 in patients on Hemodialysis, Clin J Am Soc Nephrol
Sun, Lin, Wang, Gao, Ye, Paxlovid in patients who are immunocompromised and hospitalised with SARS-CoV-2 infection, Lancet Infect Dis
Uraki, Kiso, Iida, Imai, Takashita et al., Characterization and antiviral susceptibility of SARS-CoV-2 Omicron BA.2, Nature
Wang, Zhao, Liu, Chen, Feng, Early administration of Paxlovid reduces the viral elimination time in patients infected with SARS-CoV-2 omicron variants, J Med Virol
Weng, Xie, Han, Yuan, Li et al., Safety and Efficacy of Paxlovid against Omicron Variants of Coronavirus Disease 2019 in Elderly Patients, Infect Dis Ther
Williamson, Walker, Bhaskaran, Bacon, Bates et al., Factors associated with COVID-19-related death using OpenSAFELY, Nature
Wolter, Jassat, Gottberg, Cohen, Da-Ga, Clinical severity of omicron lineage BA.2 infection compared with BA.1 infection in South Africa, Lancet
Wolter, Jassat, Walaza, Welch, Moultrie et al., Early assessment of the clinical severity of the SARS-CoV-2 omicron variant in South Africa: a data linkage study, Lancet
Yu, Guo, Zhang, Kong, Shen et al., Proportion of asymptomatic infection and nonsevere disease caused by SARS-CoV-2 Omicron variant: a systematic review and analysis, J Med Virol
Zhong, Jiang, Yang, Feng, Duan et al., The efficacy of paxlovid in elderly patients infected with SARS-CoV-2 omicron variants: results of a non-randomized clinical trial, Front Med
Zhou, Huang, Sun, Tian, Xue et al., Chronological changes of viral shedding in adult inpatients with Omicron infection in Shanghai, China, Front Immunol
Zhou, Yu, Du, Fan, Liu et al., Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study, Lancet
DOI record:
{
"DOI": "10.1186/s12879-023-08620-2",
"ISSN": [
"1471-2334"
],
"URL": "http://dx.doi.org/10.1186/s12879-023-08620-2",
"abstract": "<jats:title>Abstract</jats:title><jats:sec>\n <jats:title>Introduction</jats:title>\n <jats:p>The SARS-CoV-2 Omicron variant has decreased virulence and pathogenicity, yet the number of Omicron infections worldwide is unprecedentedly high, with rather high mortality and severe disease rate. Chronic kidney disease (CKD) patients are particularly vulnerable to the SARS-CoV-2 Omicron variant and have unique clinical outcomes.</jats:p>\n </jats:sec><jats:sec>\n <jats:title>Methods</jats:title>\n <jats:p>We retrospectively collected data from 2140 hospitalized patients with SARS-CoV-2 Omicron variant infection from March 29, 2022, to May 17, 2022. Demographic characteristics, ancillary examination results, and clinical treatments were described. Occurrence of critical COVID-19 or death and time of positive-to-negative conversion was defined as primary outcomes. The presence of COVID-19 pneumonia and the usage of respiratory or circulatory support was defined as secondary outcomes. Univariate or multivariate logistic regression analyses were performed to identify risk factors for primary outcomes.</jats:p>\n </jats:sec><jats:sec>\n <jats:title>Results</jats:title>\n <jats:p>15.74% of CKD patients infected with the SARS-CoV-2 Omicron variant ended up with critical COVID-19 or death. Pre-existing CKD was a risk factor for critical COVID-19 or death and prolonged time of positive-to-negative conversion of SARS-CoV-2. Nirmatrelvir-ritonavir facilitated viral clearance among COVID-19 patients with non-severe CKD.</jats:p>\n </jats:sec><jats:sec>\n <jats:title>Conclusion</jats:title>\n <jats:p>We found patients with CKD and COVID-19 due to Omicron experienced worse clinical outcomes and prolonged time of positive-to-negative conversion of SARS-CoV-2 compared to patients without CKD, which helps rationalize limited medical resources and offers guidance for appropriate clinical treatments.</jats:p>\n </jats:sec>",
"alternative-id": [
"8620"
],
"article-number": "698",
"assertion": [
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Received",
"name": "received",
"order": 1,
"value": "8 February 2023"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Accepted",
"name": "accepted",
"order": 2,
"value": "18 September 2023"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "First Online",
"name": "first_online",
"order": 3,
"value": "18 October 2023"
},
{
"group": {
"label": "Declarations",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 1
},
{
"group": {
"label": "Ethics approval and consent to participate",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 2,
"value": "Ethical approval was obtained from the Ethics Review Board of the Huashan Hospital, Fudan University (ethics approval registration number: KY2022-582).Informed consent forms were signed by each patient.All methods were carried out in accordance with relevant guidelines and regulations."
},
{
"group": {
"label": "Consent for publication",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 3,
"value": "Not applicable."
},
{
"group": {
"label": "Competing interests",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 4,
"value": "The authors declare no competing interests."
}
],
"author": [
{
"affiliation": [],
"family": "Guo",
"given": "Yue",
"sequence": "first"
},
{
"affiliation": [],
"family": "Guo",
"given": "Yifei",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ying",
"given": "Huajian",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Yu",
"given": "Weien",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Chen",
"given": "Shiqi",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Zhang",
"given": "Yao",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Zhang",
"given": "Shenyan",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Lin",
"given": "Yanxue",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Sun",
"given": "Feng",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Zhang",
"given": "Yongmei",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Yu",
"given": "Jie",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ma",
"given": "Ke",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Qin",
"given": "Lunxiu",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Long",
"given": "Feng",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Zhu",
"given": "Haoxiang",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Mao",
"given": "Richeng",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Xue",
"given": "Jun",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Zhang",
"given": "Jiming",
"sequence": "additional"
}
],
"container-title": "BMC Infectious Diseases",
"container-title-short": "BMC Infect Dis",
"content-domain": {
"crossmark-restriction": false,
"domain": [
"link.springer.com"
]
},
"created": {
"date-parts": [
[
2023,
10,
18
]
],
"date-time": "2023-10-18T15:03:44Z",
"timestamp": 1697641424000
},
"deposited": {
"date-parts": [
[
2023,
10,
19
]
],
"date-time": "2023-10-19T03:28:24Z",
"timestamp": 1697686104000
},
"funder": [
{
"name": "zhangjiming"
}
],
"indexed": {
"date-parts": [
[
2023,
10,
20
]
],
"date-time": "2023-10-20T05:21:17Z",
"timestamp": 1697779277923
},
"is-referenced-by-count": 0,
"issue": "1",
"issued": {
"date-parts": [
[
2023,
10,
18
]
]
},
"journal-issue": {
"issue": "1",
"published-online": {
"date-parts": [
[
2023,
12
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
10,
18
]
],
"date-time": "2023-10-18T00:00:00Z",
"timestamp": 1697587200000
}
},
{
"URL": "https://creativecommons.org/licenses/by/4.0",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
10,
18
]
],
"date-time": "2023-10-18T00:00:00Z",
"timestamp": 1697587200000
}
}
],
"link": [
{
"URL": "https://link.springer.com/content/pdf/10.1186/s12879-023-08620-2.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://link.springer.com/article/10.1186/s12879-023-08620-2/fulltext.html",
"content-type": "text/html",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://link.springer.com/content/pdf/10.1186/s12879-023-08620-2.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "297",
"original-title": [],
"prefix": "10.1186",
"published": {
"date-parts": [
[
2023,
10,
18
]
]
},
"published-online": {
"date-parts": [
[
2023,
10,
18
]
]
},
"publisher": "Springer Science and Business Media LLC",
"reference": [
{
"DOI": "10.1038/s41586-021-04389-z",
"author": "D Planas",
"doi-asserted-by": "publisher",
"first-page": "671",
"issue": "7898",
"journal-title": "Nature",
"key": "8620_CR1",
"unstructured": "Planas D, Saunders N, Maes P, Guivel-Benhassine F, Planchais C, Buchrieser J, Bolland WH, Porrot F, Staropoli I, Lemoine F, et al. Considerable escape of SARS-CoV-2 Omicron to antibody neutralization. Nature. 2022;602(7898):671–5.",
"volume": "602",
"year": "2022"
},
{
"DOI": "10.1002/jmv.28066",
"doi-asserted-by": "crossref",
"key": "8620_CR2",
"unstructured": "Yu W, Guo Y, Zhang S, Kong Y, Shen Z, Zhang J. Proportion of asymptomatic infection and nonsevere disease caused by SARS-CoV-2 Omicron variant: a systematic review and analysis. J Med Virol 2022."
},
{
"DOI": "10.3346/jkms.2022.37.e31",
"author": "MK Kim",
"doi-asserted-by": "publisher",
"first-page": "e31",
"issue": "3",
"journal-title": "J Korean Med Sci",
"key": "8620_CR3",
"unstructured": "Kim MK, Lee B, Choi YY, Um J, Lee KS, Sung HK, Kim Y, Park JS, Lee M, Jang HC, et al. Clinical characteristics of 40 patients infected with the SARS-CoV-2 Omicron variant in Korea. J Korean Med Sci. 2022;37(3):e31.",
"volume": "37",
"year": "2022"
},
{
"key": "8620_CR4",
"unstructured": "Weekly epidemiological update on COVID-19–19. January 2023 [https://www.who.int/publications/m/item/covid-19-weekly-epidemiological-update---21-december-2022]."
},
{
"DOI": "10.1155/2022/4551132",
"doi-asserted-by": "crossref",
"key": "8620_CR5",
"unstructured": "Kaso AW, Hareru HE, Kaso T, Agero G. Factors Associated with Poor Treatment Outcome among Hospitalized COVID-19 Patients in South Central, Ethiopia. Biomed Res Int 2022, 2022:4551132."
},
{
"DOI": "10.1016/S0140-6736(20)30045-3",
"author": "GBDCKD Collaboration",
"doi-asserted-by": "publisher",
"first-page": "709",
"issue": "10225",
"journal-title": "Lancet",
"key": "8620_CR6",
"unstructured": "Collaboration GBDCKD. Global, regional, and national burden of chronic kidney disease, 1990–2017: a systematic analysis for the global burden of Disease Study 2017. Lancet. 2020;395(10225):709–33.",
"volume": "395",
"year": "2020"
},
{
"DOI": "10.1038/s41581-022-00570-3",
"author": "V Mahalingasivam",
"doi-asserted-by": "publisher",
"first-page": "485",
"issue": "8",
"journal-title": "Nat Rev Nephrol",
"key": "8620_CR7",
"unstructured": "Mahalingasivam V, Su G, Iwagami M, Davids MR, Wetmore JB, Nitsch D. COVID-19 and kidney disease: insights from epidemiology to inform clinical practice. Nat Rev Nephrol. 2022;18(8):485–98.",
"volume": "18",
"year": "2022"
},
{
"DOI": "10.1053/j.ajkd.2021.07.003",
"author": "EYM Chung",
"doi-asserted-by": "publisher",
"first-page": "804",
"issue": "6",
"journal-title": "Am J Kidney Dis",
"key": "8620_CR8",
"unstructured": "Chung EYM, Palmer SC, Natale P, Krishnan A, Cooper TE, Saglimbene VM, Ruospo M, Au E, Jayanti S, Liang A, et al. Incidence and outcomes of COVID-19 in people with CKD: a systematic review and Meta-analysis. Am J Kidney Dis. 2021;78(6):804–15.",
"volume": "78",
"year": "2021"
},
{
"DOI": "10.1016/j.jinf.2022.07.027",
"author": "Y Ao",
"doi-asserted-by": "publisher",
"first-page": "573",
"issue": "5",
"journal-title": "J Infect",
"key": "8620_CR9",
"unstructured": "Ao Y, Li J, Wei Z, Wang Z, Tian H, Qiu Y, Fu X, Ma W, Li L, Zeng M, et al. Clinical and virological characteristics of SARS-CoV-2 Omicron BA.2.2 variant outbreaks during April to May, 2022, Shanghai, China. J Infect. 2022;85(5):573–607.",
"volume": "85",
"year": "2022"
},
{
"key": "8620_CR10",
"unstructured": "WHO: Available at. : https://www.who.int/publications/i/item/WHO-2019-nCoV-clinical-2022-1."
},
{
"DOI": "10.1038/s41586-022-04856-1",
"author": "R Uraki",
"doi-asserted-by": "publisher",
"first-page": "119",
"issue": "7917",
"journal-title": "Nature",
"key": "8620_CR11",
"unstructured": "Uraki R, Kiso M, Iida S, Imai M, Takashita E, Kuroda M, Halfmann PJ, Loeber S, Maemura T, Yamayoshi S, et al. Characterization and antiviral susceptibility of SARS-CoV-2 Omicron BA.2. Nature. 2022;607(7917):119–27.",
"volume": "607",
"year": "2022"
},
{
"DOI": "10.1016/S0140-6736(22)00017-4",
"author": "N Wolter",
"doi-asserted-by": "publisher",
"first-page": "437",
"issue": "10323",
"journal-title": "Lancet",
"key": "8620_CR12",
"unstructured": "Wolter N, Jassat W, Walaza S, Welch R, Moultrie H, Groome M, Amoako DG, Everatt J, Bhiman JN, Scheepers C, et al. Early assessment of the clinical severity of the SARS-CoV-2 omicron variant in South Africa: a data linkage study. Lancet. 2022;399(10323):437–46.",
"volume": "399",
"year": "2022"
},
{
"DOI": "10.1016/S0140-6736(22)00981-3",
"author": "N Wolter",
"doi-asserted-by": "publisher",
"first-page": "93",
"issue": "10346",
"journal-title": "Lancet",
"key": "8620_CR13",
"unstructured": "Wolter N, Jassat W, von Gottberg A, Cohen C, group DA-Ga. Clinical severity of omicron lineage BA.2 infection compared with BA.1 infection in South Africa. Lancet. 2022;400(10346):93–6.",
"volume": "400",
"year": "2022"
},
{
"DOI": "10.1038/s41586-020-2521-4",
"author": "EJ Williamson",
"doi-asserted-by": "publisher",
"first-page": "430",
"issue": "7821",
"journal-title": "Nature",
"key": "8620_CR14",
"unstructured": "Williamson EJ, Walker AJ, Bhaskaran K, Bacon S, Bates C, Morton CE, Curtis HJ, Mehrkar A, Evans D, Inglesby P, et al. Factors associated with COVID-19-related death using OpenSAFELY. Nature. 2020;584(7821):430–6.",
"volume": "584",
"year": "2020"
},
{
"DOI": "10.1053/j.ajkd.2020.09.003",
"author": "JE Flythe",
"doi-asserted-by": "publisher",
"first-page": "190",
"issue": "2",
"journal-title": "Am J Kidney Dis",
"key": "8620_CR15",
"unstructured": "Flythe JE, Assimon MM, Tugman MJ, Chang EH, Gupta S, Shah J, Sosa MA, Renaghan AD, Melamed ML, Wilson FP, et al. Characteristics and outcomes of individuals with pre-existing kidney disease and COVID-19 admitted to Intensive Care Units in the United States. Am J Kidney Dis. 2021;77(2):190–203. e191.",
"volume": "77",
"year": "2021"
},
{
"DOI": "10.1080/22221751.2022.2122581",
"author": "X Chen",
"doi-asserted-by": "publisher",
"first-page": "2501",
"issue": "1",
"journal-title": "Emerg Microbes Infect",
"key": "8620_CR16",
"unstructured": "Chen X, Wang H, Ai J, Shen L, Lin K, Yuan G, Sheng X, Jin X, Deng Z, Xu J, et al. Identification of CKD, bedridden history and cancer as higher-risk comorbidities and their impact on prognosis of hospitalized Omicron patients: a multi-centre cohort study. Emerg Microbes Infect. 2022;11(1):2501–9.",
"volume": "11",
"year": "2022"
},
{
"DOI": "10.1016/S0140-6736(20)30566-3",
"author": "F Zhou",
"doi-asserted-by": "publisher",
"first-page": "1054",
"issue": "10229",
"journal-title": "Lancet",
"key": "8620_CR17",
"unstructured": "Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, Xiang J, Wang Y, Song B, Gu X, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–62.",
"volume": "395",
"year": "2020"
},
{
"DOI": "10.3389/fimmu.2023.1090498",
"author": "X Zhou",
"doi-asserted-by": "publisher",
"first-page": "1090498",
"journal-title": "Front Immunol",
"key": "8620_CR18",
"unstructured": "Zhou X, Huang X, Sun T, Jin X, Tian Z, Xue M, Kang J, Gao B, Xu A, Chen Y, et al. Chronological changes of viral shedding in adult inpatients with Omicron infection in Shanghai, China. Front Immunol. 2023;14:1090498.",
"volume": "14",
"year": "2023"
},
{
"DOI": "10.1016/j.jiph.2022.12.003",
"author": "L Pei",
"doi-asserted-by": "publisher",
"first-page": "182",
"issue": "2",
"journal-title": "J Infect Public Health",
"key": "8620_CR19",
"unstructured": "Pei L, Chen Y, Zheng X, Gong F, Liu W, Lin J, Zheng R, Yang Z, Bi Y, Chen E. Comorbidities prolonged viral shedding of patients infected with SARS-CoV-2 omicron variant in Shanghai: a multi-center, retrospective, observational study. J Infect Public Health. 2023;16(2):182–9.",
"volume": "16",
"year": "2023"
},
{
"DOI": "10.1093/cid/ciac077",
"author": "S Meiring",
"doi-asserted-by": "publisher",
"first-page": "e144",
"issue": "1",
"journal-title": "Clin Infect Dis",
"key": "8620_CR20",
"unstructured": "Meiring S, Tempia S, Bhiman JN, Buys A, Kleynhans J, Makhasi M, McMorrow M, Moyes J, Quan V, Walaza S, et al. Prolonged shedding of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) at high viral loads among hospitalized immunocompromised persons living with Human Immunodeficiency Virus (HIV), South Africa. Clin Infect Dis. 2022;75(1):e144–56.",
"volume": "75",
"year": "2022"
},
{
"DOI": "10.2215/CJN.11120720",
"author": "A Shaikh",
"doi-asserted-by": "publisher",
"first-page": "290",
"issue": "2",
"journal-title": "Clin J Am Soc Nephrol",
"key": "8620_CR21",
"unstructured": "Shaikh A, Zeldis E, Campbell KN, Chan L. Prolonged SARS-CoV-2 viral RNA shedding and IgG antibody response to SARS-CoV-2 in patients on Hemodialysis. Clin J Am Soc Nephrol. 2021;16(2):290–2.",
"volume": "16",
"year": "2021"
},
{
"DOI": "10.1007/s12020-020-02465-4",
"author": "N Buetti",
"doi-asserted-by": "publisher",
"first-page": "454",
"issue": "3",
"journal-title": "Endocrine",
"key": "8620_CR22",
"unstructured": "Buetti N, Trimboli P, Mazzuchelli T, Lo Priore E, Balmelli C, Trkola A, Conti M, Martinetti G, Elzi L, Ceschi A, et al. Diabetes mellitus is a risk factor for prolonged SARS-CoV-2 viral shedding in lower respiratory tract samples of critically ill patients. Endocrine. 2020;70(3):454–60.",
"volume": "70",
"year": "2020"
},
{
"DOI": "10.1016/j.jinf.2023.02.001",
"author": "S Caillard",
"doi-asserted-by": "publisher",
"first-page": "513",
"issue": "5",
"journal-title": "J Infect",
"key": "8620_CR23",
"unstructured": "Caillard S, Laugel E, Benotmane I, Fafi Kremer S. Molecular evolution of the SARS-CoV-2 omicron BA.2 variant in kidney transplant recipients with prolonged viral shedding. J Infect. 2023;86(5):513–5.",
"volume": "86",
"year": "2023"
},
{
"DOI": "10.1016/j.jiac.2020.12.001",
"author": "Y Nakajima",
"doi-asserted-by": "publisher",
"first-page": "387",
"issue": "2",
"journal-title": "J Infect Chemother",
"key": "8620_CR24",
"unstructured": "Nakajima Y, Ogai A, Furukawa K, Arai R, Anan R, Nakano Y, Kurihara Y, Shimizu H, Misaki T, Okabe N. Prolonged viral shedding of SARS-CoV-2 in an immunocompromised patient. J Infect Chemother. 2021;27(2):387–9.",
"volume": "27",
"year": "2021"
},
{
"DOI": "10.1159/000510557",
"author": "JJ Broseta",
"doi-asserted-by": "publisher",
"first-page": "531",
"issue": "4–5",
"journal-title": "Blood Purif",
"key": "8620_CR25",
"unstructured": "Broseta JJ, Rodriguez-Espinosa D, Cuadrado E, Guillen-Olmos E, Hermida E, Montagud-Marrahi E, Rodas L, Vera M, Fontsere N, Arias M, et al. SARS-CoV-2 infection in a spanish cohort of CKD-5D patients: prevalence, clinical presentation, outcomes, and De-Isolation results. Blood Purif. 2021;50(4–5):531–8.",
"volume": "50",
"year": "2021"
},
{
"DOI": "10.1681/ASN.2021040490",
"author": "C Danthu",
"doi-asserted-by": "publisher",
"first-page": "2153",
"issue": "9",
"journal-title": "J Am Soc Nephrol",
"key": "8620_CR26",
"unstructured": "Danthu C, Hantz S, Dahlem A, Duval M, Ba B, Guibbert M, El Ouafi Z, Ponsard S, Berrahal I, Achard JM, et al. Humoral response after SARS-CoV-2 mRNA vaccination in a cohort of Hemodialysis patients and kidney transplant recipients. J Am Soc Nephrol. 2021;32(9):2153–8.",
"volume": "32",
"year": "2021"
},
{
"DOI": "10.1002/cti2.1160",
"author": "PH Lee",
"doi-asserted-by": "publisher",
"first-page": "e1160",
"issue": "7",
"journal-title": "Clin Transl Immunology",
"key": "8620_CR27",
"unstructured": "Lee PH, Tay WC, Sutjipto S, Fong SW, Ong SWX, Wei WE, Chan YH, Ling LM, Young BE, Toh MPH, et al. Associations of viral ribonucleic acid (RNA) shedding patterns with clinical illness and immune responses in severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) infection. Clin Transl Immunology. 2020;9(7):e1160.",
"volume": "9",
"year": "2020"
},
{
"DOI": "10.1093/infdis/jiaa311",
"author": "S Hao",
"doi-asserted-by": "publisher",
"first-page": "367",
"issue": "3",
"journal-title": "J Infect Dis",
"key": "8620_CR28",
"unstructured": "Hao S, Lian J, Lu Y, Jia H, Hu J, Yu G, Wang X, Xu K, Ni Q, Li Y, et al. Decreased B cells on Admission Associated with prolonged viral RNA shedding from the respiratory tract in Coronavirus Disease 2019: a case-control study. J Infect Dis. 2020;222(3):367–71.",
"volume": "222",
"year": "2020"
},
{
"DOI": "10.1016/j.clim.2020.108611",
"author": "C Gao",
"doi-asserted-by": "publisher",
"first-page": "108611",
"journal-title": "Clin Immunol",
"key": "8620_CR29",
"unstructured": "Gao C, Zhu L, Jin CC, Tong YX, Xiao AT, Zhang S. Proinflammatory cytokines are associated with prolonged viral RNA shedding in COVID-19 patients. Clin Immunol. 2020;221:108611.",
"volume": "221",
"year": "2020"
},
{
"DOI": "10.1186/s12879-021-06548-z",
"author": "J Li",
"doi-asserted-by": "publisher",
"first-page": "1063",
"issue": "1",
"journal-title": "BMC Infect Dis",
"key": "8620_CR30",
"unstructured": "Li J, Liao X, Zhou Y, Wang L, Yang H, Zhang W, Zhang Z, Kang Y. Association between glucocorticoids treatment and viral clearance delay in patients with COVID-19: a systematic review and meta-analysis. BMC Infect Dis. 2021;21(1):1063.",
"volume": "21",
"year": "2021"
},
{
"DOI": "10.1002/jmv.28441",
"author": "B Amani",
"doi-asserted-by": "publisher",
"first-page": "e28441",
"issue": "2",
"journal-title": "J Med Virol",
"key": "8620_CR31",
"unstructured": "Amani B, Amani B. Efficacy and safety of nirmatrelvir/ritonavir (paxlovid) for COVID-19: a rapid review and meta-analysis. J Med Virol. 2023;95(2):e28441.",
"volume": "95",
"year": "2023"
},
{
"DOI": "10.1002/jmv.28443",
"author": "Y Wang",
"doi-asserted-by": "publisher",
"first-page": "e28443",
"issue": "1",
"journal-title": "J Med Virol",
"key": "8620_CR32",
"unstructured": "Wang Y, Zhao D, Liu X, Chen X, Xiao W, Feng L. Early administration of Paxlovid reduces the viral elimination time in patients infected with SARS-CoV-2 omicron variants. J Med Virol. 2023;95(1):e28443.",
"volume": "95",
"year": "2023"
},
{
"DOI": "10.3389/fmed.2022.980002",
"author": "W Zhong",
"doi-asserted-by": "publisher",
"first-page": "980002",
"journal-title": "Front Med (Lausanne)",
"key": "8620_CR33",
"unstructured": "Zhong W, Jiang X, Yang X, Feng T, Duan Z, Wang W, Sun Z, Chen L, Nie X, Zhu C, et al. The efficacy of paxlovid in elderly patients infected with SARS-CoV-2 omicron variants: results of a non-randomized clinical trial. Front Med (Lausanne). 2022;9:980002.",
"volume": "9",
"year": "2022"
},
{
"DOI": "10.1007/s40121-023-00760-x",
"author": "C Weng",
"doi-asserted-by": "publisher",
"first-page": "649",
"issue": "2",
"journal-title": "Infect Dis Ther",
"key": "8620_CR34",
"unstructured": "Weng C, Xie R, Han G, Yuan Y, Li S, Wang C, Wang X, Jiang W, Jiang L. Safety and Efficacy of Paxlovid against Omicron Variants of Coronavirus Disease 2019 in Elderly Patients. Infect Dis Ther. 2023;12(2):649–62.",
"volume": "12",
"year": "2023"
},
{
"DOI": "10.1016/S1473-3099(22)00430-3",
"author": "F Sun",
"doi-asserted-by": "publisher",
"first-page": "1279",
"issue": "9",
"journal-title": "Lancet Infect Dis",
"key": "8620_CR35",
"unstructured": "Sun F, Lin Y, Wang X, Gao Y, Ye S. Paxlovid in patients who are immunocompromised and hospitalised with SARS-CoV-2 infection. Lancet Infect Dis. 2022;22(9):1279.",
"volume": "22",
"year": "2022"
},
{
"DOI": "10.1016/j.ekir.2022.08.026",
"author": "A Devresse",
"doi-asserted-by": "publisher",
"first-page": "2356",
"issue": "11",
"journal-title": "Kidney Int Rep",
"key": "8620_CR36",
"unstructured": "Devresse A, Sebastien B, De Greef J, Lemaitre F, Boland L, Haufroid V, Scohy A, Kabamba B, Yombi JC, Belkhir L, et al. Safety, Efficacy, and relapse of nirmatrelvir-ritonavir in kidney transplant recipients infected with SARS-CoV-2. Kidney Int Rep. 2022;7(11):2356–63.",
"volume": "7",
"year": "2022"
},
{
"DOI": "10.1016/j.jinf.2022.10.002",
"author": "H Cai",
"doi-asserted-by": "publisher",
"first-page": "702",
"issue": "6",
"journal-title": "J Infect",
"key": "8620_CR37",
"unstructured": "Cai H, Yan J, Wang J, Che X, Mou S. Efficacy of Paxlovid in patients with acute kidney injury who developed COVID-19. J Infect. 2022;85(6):702–69.",
"volume": "85",
"year": "2022"
},
{
"DOI": "10.1016/j.antiviral.2023.105659",
"author": "H Cai",
"doi-asserted-by": "publisher",
"first-page": "105659",
"journal-title": "Antiviral Res",
"key": "8620_CR38",
"unstructured": "Cai H, Yan J, Liu S, Li P, Ding L, Zhan Y, Lu J, Li Z, Sun Y, Zhu M, et al. Paxlovid for hospitalized COVID-19 patients with chronic kidney disease. Antiviral Res. 2023;216:105659.",
"volume": "216",
"year": "2023"
}
],
"reference-count": 38,
"references-count": 38,
"relation": {},
"resource": {
"primary": {
"URL": "https://bmcinfectdis.biomedcentral.com/articles/10.1186/s12879-023-08620-2"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Infectious Diseases"
],
"subtitle": [],
"title": "In-hospital adverse outcomes and risk factors among chronic kidney disease patients infected with the omicron variant of SARS-CoV-2: a single-center retrospective study",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1007/springer_crossmark_policy",
"volume": "23"
}