Comparative host-coronavirus protein interaction networks reveal pan-viral disease mechanisms
et al., Science, doi:10.1126/science.abe9403, Dec 2020
Analysis of interactions between viral and human proteins for SARS-CoV-2, SARS-CoV-1, and MERS-CoV and genetic screening to identify host factors that enhance or inhibit viral infection.
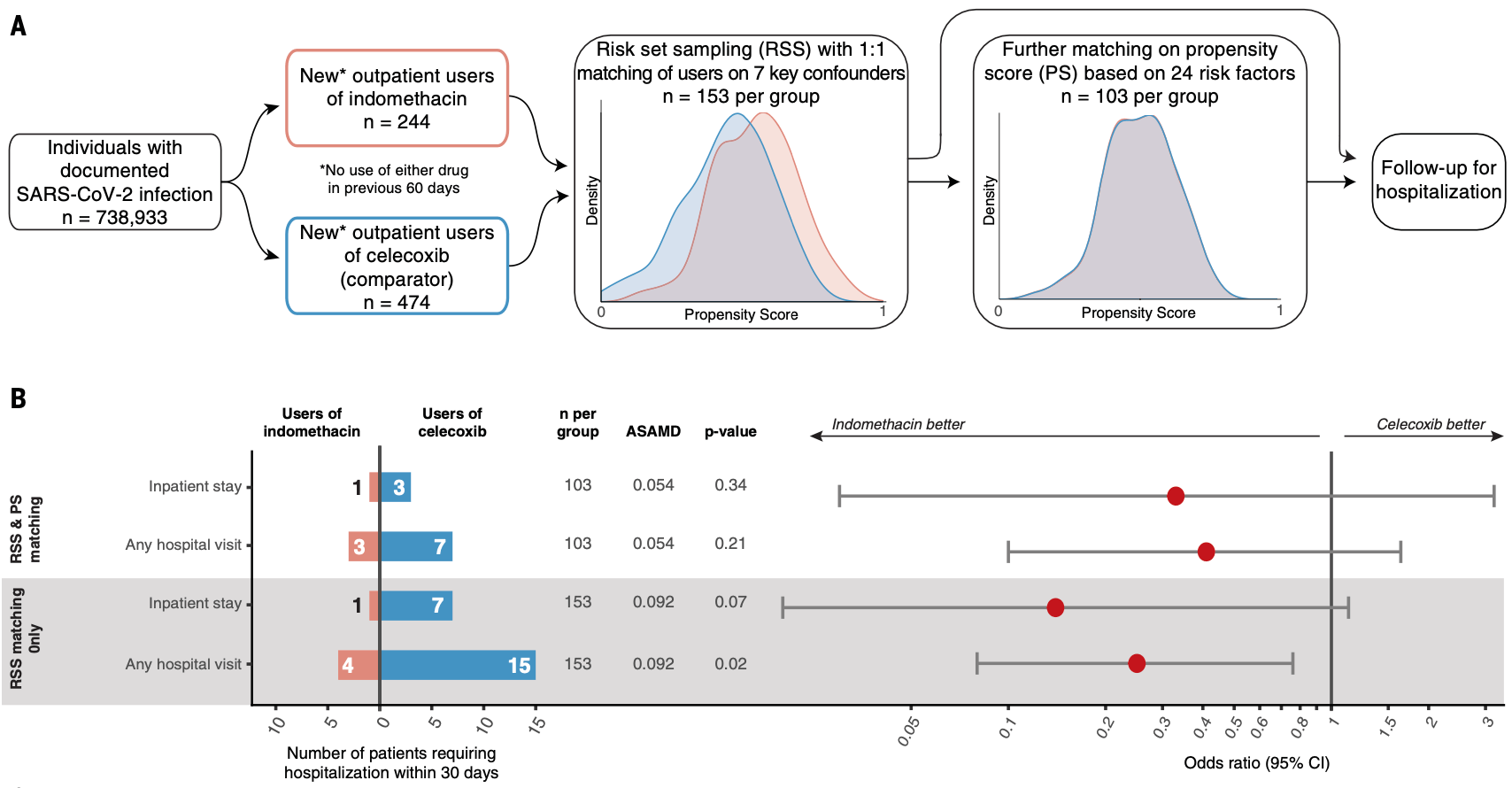
Authors predict indomethacin will have antiviral activity for SARS-CoV-2 and perform a retrospective study of patients in the USA that started treatment within 21 days after COVID-19 infection - 103 with indomethacin, and 103 using a celecoxib, a clinically similar drug without predicted antiviral activity. There were fewer hospital visits and hospitalizations with indomethacin, without statistical significance.
Standard of Care (SOC) for COVID-19 in the study country,
the USA, is very poor with very low average efficacy for approved treatments1.
Only expensive, high-profit treatments were approved for early treatment. Low-cost treatments were excluded, reducing the probability of early treatment due to access and cost barriers, and eliminating complementary and synergistic benefits seen with many low-cost treatments.
|
risk of hospitalization, 66.7% lower, RR 0.33, p = 0.34, treatment 1 of 103 (1.0%), control 3 of 103 (2.9%), NNT 51, RSS and PSM, propensity score matching.
|
|
risk of progression, 57.1% lower, RR 0.43, p = 0.21, treatment 3 of 103 (2.9%), control 7 of 103 (6.8%), NNT 26, RSS and PSM, propensity score matching.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Gordon et al., 4 Dec 2020, retrospective, USA, peer-reviewed, 200 authors, this trial compares with another treatment - results may be better when compared to placebo.
Contact: pbeltrao@ebi.ac.uk, marco.vignuzzi@pasteur.fr, cbasler@gsu.edu, verba@msg.ucsf, oren.rosenberg@ucsf.edu, a.peden@sheffield.ac.uk, robert.grosse@pharmakol.uni-freiburg.de, jeremy.rassen@aetion.com, garcia-sastre@mssm.edu, nevan.krogan@ucsf.edu, verba@msg.ucsf.edu, rosenberg@ucsf.edu, adolfo.garcia-sastre@mssm.edu.
Comparative host-coronavirus protein interaction networks reveal pan-viral disease mechanisms
Science, doi:10.1126/science.abe9403
The emergence of three lethal coronaviruses in <20 years and the urgency of the COVID-19 pandemic have prompted efforts to develop new therapeutic strategies, including by repurposing existing agents. After performing a comparative analysis of the three pathogenic human coronaviruses severe acute respiratory syndrome coronavirus 1 (SARS-CoV-1), SARS-CoV-2, and Middle East respiratory syndrome coronavirus (MERS-CoV), we identified shared biology and host-directed drug targets to prioritize therapeutics with potential for rapid deployment against current and future coronavirus outbreaks. RATIONALE: Expanding on our recent SARS-CoV-2 interactome, we mapped the virus-host protein-protein interactions for SARS-CoV-1 and MERS-CoV and assessed the cellular localization of each viral protein across the three strains. We conducted two genetic screens of SARS-CoV-2 interactors to prioritize functionally-relevant host factors and structurally characterized one virus-host interaction. We then tested the clinical relevance of three more host factors by assessing risk in genetic cohorts or observing effectiveness of host factor-targeting drugs in realworld evidence. RESULTS: Quantitative comparison of the 389 interactors of SARS-CoV-2, 366 of SARS-CoV-1, and 296 of MERS-CoV highlighted interactions with host processes that are conserved across all three viruses, including where nonorthologous proteins from different virus strains seem to fill similar roles. We also localized each individually-expressed viral protein by microscopy and then raised and validated antisera against 14 SARS-CoV-2 proteins to determine their localization during infection. On the basis of two independent genetic perturbation screens, we identified 73 host factors that, when depleted, caused significant changes in SARS-CoV-2 replication. From this list of potential drug targets, we validated the biological and clinical relevance of Tom70, IL17RA, PGES-2, and SigmaR1. A 3-Å cryo-electron microscopy structure of Tom70, a mitochondrial import receptor, in complex with SARS-CoV-2 ORF9b, provides insight into how ORF9b may modulate the host immune response. Using curated genome-wide association study data, we found that individuals with genotypes corresponding to higher soluble IL17RA levels in plasma are at decreased risk of COVID-19 hospitalization. To demonstrate the value of our data for drug repurposing, we identified SARS-CoV-2 patients who were prescribed drugs against prioritized targets and asked how they fared compared with carefully matched patients treated with clinically similar drugs that do not inhibit SARS-CoV-2. Both indomethacin, an inhibitor of host factor PGES-2, and typical antipsychotics, selected for their interaction with sigma receptors, showed effectiveness against COVID-19 compared with celecoxib and atypical antipsychotics, respectively. CONCLUSION: By employing an integrative and collaborative approach, we identified conserved mechanisms across three..
resources and reagents should be directed to and will be fulfilled by N.J.K. (nevan.krogan@ucsf.edu). The MS proteomics data have been deposited to the ProteomeXchange Consortium via the PRIDE partner repository with the dataset identifier PXD021588 (100) . An interactive version of PPI data can be found at https://kroganlab. ucsf.edu/network-maps. Atomic coordinates and the cryo-EM map of the reported Tom70-ORF9b structure have been deposited in the Protein Data Bank under accession code 7KDT and in the Electron Microscopy Data Bank under accession code EMD-22829. Expression vectors used in this study are readily available from the authors for biomedical researchers and educators in the nonprofit sector. The Aetion Evidence Platform used for the clinical analysis is available under license from Aetion, New York, NY. To protect patient privacy, data used in real-world analyses are available for inspection by qualified researchers under confidentiality and third-party agreements with Aetion and/or HealthVerity. This work is licensed under a Creative Commons Attribution 4.0 International (CC BY 4.0) license, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. To view a copy of this license, visit https://creativecommons.org/licenses/by/4.0/. This license does not apply to figures/photos/artwork or other content included in the article that is credited to a third party; obtain authorization from the rights..
References
-R, Wang, Automated structure refinement of macromolecular assemblies from cryo-EM maps using Rosetta, eLife, doi:10.7554/eLife.17219
Abate, Mosier, Berardi, Glennon, A structure-affinity and comparative molecular field analysis of sigma-2 (s2) receptor ligands, Cent. Nerv. Syst. Agents Med. Chem, doi:10.2174/1871524910909030246
Afonine, New tools for the analysis and validation of cryo-EM maps and atomic models, Acta Cryst, doi:10.1107/S2059798318009324
Akdel, Durairaj, De Ridder, Van Dijk, Caretta -A multiple protein structure alignment and feature extraction suite, Comput. Struct. Biotechnol. J, doi:10.1016/j.csbj.2020.03.011
Almagro Armenteros, Detecting sequence signals in targeting peptides using deep learning, Life Sci. Alliance, doi:10.26508/lsa.201900429
Almagro Armenteros, Sønderby, Sønderby, Nielsen, Winther, DeepLoc: Prediction of protein subcellular localization using deep learning, Bioinformatics, doi:10.1093/bioinformatics/btx431
Altschul, Gapped BLAST and PSI-BLAST: A new generation of protein database search programs, Nucleic Acids Res, doi:10.1093/nar/25.17.3389
Amici, Indomethacin has a potent antiviral activity against SARS coronavirus, Antivir. Ther
Armstrong, Hickey, Diekhans, Deran, Fang et al., Progressive alignment with Cactus: A multiple-genome aligner for the thousand-genome era, bioRxiv
Austin, Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples, Stat. Med, doi:10.1002/sim.3697
Backes, Tom70 enhances mitochondrial preprotein import efficiency by binding to internal targeting sequences, J. Cell Biol, doi:10.1083/jcb.201708044
Baker, Frazier, Gulbis, Ryan, Mitochondrial protein-import machinery: Correlating structure with function, Trends Cell Biol, doi:10.1016/j.tcb.2007.07.010
Be, Br, Du, Ba, Lo et al., The QCRG Structural Biology Consortium has received support from: Quantitative Biosciences Institute
Becerra-Flores, Cardozo, SARS-CoV-2 viral spike G614 mutation exhibits higher case fatality rate, Int. J. Clin. Pract, doi:10.1111/ijcp.13525
Beigel, Remdesivir for the treatment of Covid-19-Final report, N. Engl. J. Med, doi:10.1056/NEJMoa2007764
Bouhaddou, The Global Phosphorylation Landscape of SARS-CoV-2 Infection, Cell, doi:10.1016/j.cell.2020.06.034
Brix, Dietmeier, Pfanner, Differential recognition of preproteins by the purified cytosolic domains of the mitochondrial import receptors Tom20, Tom22, and Tom70, J. Biol. Chem, doi:10.1074/jbc.272.33.20730
Brix, The mitochondrial import receptor Tom70: Identification of a 25 kDa core domain with a specific binding site for preproteins, J. Mol. Biol, doi:10.1006/jmbi.2000.4120
Chen, Clinical and immunological features of severe and moderate coronavirus disease 2019, J. Clin. Invest, doi:10.1172/JCI137244
Chiva, QCloud: A cloud-based quality control system for mass spectrometry-based proteomics laboratories, PLOS ONE, doi:10.1371/journal.pone.0189209
Chu, Molecular Diagnosis of a Novel Coronavirus (2019-nCoV) Causing an Outbreak of Pneumonia, Clin. Chem, doi:10.1093/clinchem/hvaa029
Cox, Mann, MaxQuant enables high peptide identification rates, individualized p.p.b.-range mass accuracies and proteome-wide protein quantification, Nat. Biotechnol, doi:10.1038/nbt.1511
Croll, ISOLDE: A physically realistic environment for model building into low-resolution electron-density maps, Acta Cryst, doi:10.1107/S2059798318002425
Dold, Samara, Li, Tardy, Leucht, Haloperidol versus first-generation antipsychotics for the treatment of schizophrenia and other psychotic disorders, Cochrane Database Syst. Rev, doi:10.1002/14651858.CD009831.pub2
Dong, Fan, Schneidman-Duhovny, Webb, Sali, Optimized atomic statistical potentials: Assessment of protein interfaces and loops, Bioinformatics, doi:10.1093/bioinformatics/btt560
Drozdetskiy, Cole, Procter, Barton, JPred4: A protein secondary structure prediction server, Nucleic Acids Res, doi:10.1093/nar/gkv332
Durairaj, Akdel, De Ridder, Van Dijk, Geometricus Represents Protein Structures as Shape-mers Derived from Moment Invariants, bioRxiv
Edmonson, Mayfield, Vervoort, Dupont, Argyropoulos, Characterization of a human import component of the mitochondrial outer membrane, TOMM70A, Cell Commun. Adhes, doi:10.1080/15419060212186
Emsley, Cowtan, Coot: Model-building tools for molecular graphics, Acta Cryst, doi:10.1107/S0907444904019158
Fan, Bhangoo, Young, Hsp90 functions in the targeting and outer membrane translocation steps of Tom70-mediated mitochondrial import, J. Biol. Chem, doi:10.1074/jbc.M605250200
Fukasawa, MitoFates: Improved prediction of mitochondrial targeting sequences and their cleavage sites, Mol. Cell. Proteomics, doi:10.1074/mcp.M114.043083
Giurgiu, CORUM: The comprehensive resource of mammalian protein complexes-2019, Nucleic Acids Res, doi:10.1093/nar/gky973
Glennon, Sigma receptor ligands and the use thereof, U.S. Patent
Goddard, UCSF ChimeraX: Meeting modern challenges in visualization and analysis, Protein Sci, doi:10.1002/pro.3235
Gordon, A SARS-CoV-2 protein interaction map reveals targets for drug repurposing, Nature, doi:10.1038/s41586-020-2286-9
Gregori-Puigjané, Identifying mechanism-of-action targets for drugs and probes, Proc. Natl. Acad. Sci. U.S.A, doi:10.1073/pnas.1204524109
Honko, Storm, Bean, Vasquez, Downs et al., Rapid Quantification and Neutralization Assays for Novel Coronavirus SARS-CoV-2
Hsiau, Conant, Rossi, Maures, Waite et al., Inference of CRISPR Edits from Sanger Trace Data, bioRxiv, doi:10.1101/251082
Huang, Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China, Lancet, doi:10.1016/S0140-6736(20)30183-5
Hubisz, Pollard, Siepel, PHAST and RPHAST: Phylogenetic analysis with space/time models, Brief. Bioinform, doi:10.1093/bib/bbq072
Hubler, Accumulation of 8,9-unsaturated sterols drives oligodendrocyte formation and remyelination, Nature, doi:10.1038/s41586-018-0360-3
Huttlin, The BioPlex Network: A Systematic Exploration of the Human Interactome, Cell, doi:10.1016/j.cell.2015.06.043
Jiang, SARS-CoV-2 Orf9b suppresses type I interferon responses by targeting TOM70, Cell. Mol. Immunol, doi:10.1038/s41423-020-0514-8
Jureka, Silvas, Basler, Propagation, Inactivation, and Safety Testing of SARS-CoV-2, Viruses, doi:10.3390/v12060622
Jäger, Global landscape of HIV-human protein complexes, Nature, doi:10.1038/nature10719
Kidmose, Namdinator -automatic molecular dynamics flexible fitting of structural models into cryo-EM and crystallography experimental maps, IUCrJ, doi:10.1107/S2052252519007619
Kozakov, The ClusPro web server for protein-protein docking, Nat. Protoc, doi:10.1038/nprot.2016.169
Krissinel, Henrick, Inference of macromolecular assemblies from crystalline state, J. Mol. Biol, doi:10.1016/j.jmb.2007.05.022
Li, Qian, Hu, Sha, Molecular chaperone Hsp70/ Hsp90 prepares the mitochondrial outer membrane translocon receptor Tom71 for preprotein loading, J. Biol. Chem, doi:10.1074/jbc.M109.023986
Lin, Paz, Hiscott, Tom70 imports antiviral immunity to the mitochondria, Cell Res, doi:10.1038/cr.2010.113
Liu, A comparative overview of COVID-19, MERS and SARS: Review article, Int. J. Surg, doi:10.1016/j.ijsu.2020.07.032
Liu, Elevated plasma levels of selective cytokines in COVID-19 patients reflect viral load and lung injury, Natl. Sci. Rev, doi:10.1093/nsr/nwaa037
Liu, Wei, Shi, Shan, Wang, Tom70 mediates activation of interferon regulatory factor 3 on mitochondria, Cell Res, doi:10.1038/cr.2010.103
Livak, Schmittgen, Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) Method, Methods, doi:10.1006/meth.2001.1262
Lokau, Garbers, Biological functions and therapeutic opportunities of soluble cytokine receptors, Cytokine Growth Factor Rev, doi:10.1016/j.cytogfr.2020.04.003
Mastronarde, Automated electron microscope tomography using robust prediction of specimen movements, J. Struct. Biol, doi:10.1016/j.jsb.2005.07.007
Matsumoto, Pouw, Correlation between neuroleptic binding to s 1 and s 2 receptors and acute dystonic reactions, Eur. J. Pharmacol, doi:10.1016/S0014-2999(00)00430-1
Mills, Domain organization of the monomeric form of the Tom70 mitochondrial import receptor, J. Mol. Biol, doi:10.1016/j.jmb.2009.03.070
Moebius, Pharmacological analysis of sterol delta8-delta7 isomerase proteins with [3H]ifenprodil, Mol. Pharmacol, doi:10.1124/mol.54.3.591
Moebius, Reiter, Hanner, Glossmann, High affinity of sigma 1-binding sites for sterol isomerization inhibitors: Evidence for a pharmacological relationship with the yeast sterol C8-C7 isomerase, Br. J. Pharmacol, doi:10.1038/sj.bjp.0701079
Nigms, -S. ; R, CRIP (Center for Research for Influenza Pathogenesis), a NIAID supported Center of Excellence for Influenza Research and Surveillance (CEIRS, contract no
Paten, Cactus: Algorithms for genome multiple sequence alignment, Genome Res, doi:10.1101/gr.123356.111
Perez-Riverol, The PRIDE database and related tools and resources in 2019: Improving support for quantification data, doi:10.1093/nar/gky1106
Pierce, ZDOCK server: Interactive docking prediction of protein-protein complexes and symmetric multimers, Bioinformatics, doi:10.1093/bioinformatics/btu097
Pillich, Chen, Rynkov, Welker, Pratt, NDEx: A Community Resource for Sharing and Publishing of Biological Networks, Methods Mol. Biol, doi:10.1007/978-1-4939-6783-4_13
Pollard, Hubisz, Rosenbloom, Siepel, Detection of nonneutral substitution rates on mammalian phylogenies, Genome Res, doi:10.1101/gr.097857.109
Pond, Frost, Muse, HyPhy: Hypothesis testing using phylogenies, Bioinformatics, doi:10.1093/bioinformatics/bti079
Qin, Dysregulation of Immune Response in Patients With Coronavirus 2019 (COVID-19) in Wuhan, China, Clin. Infect. Dis, doi:10.1093/cid/ciaa248
Quan, Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data, Med. Care, doi:10.1097/01.mlr.0000182534.19832.83
Ramani, Krumholz, Huang, Siepel, PhastWeb: A web interface for evolutionary conservation scoring of multiple sequence alignments using phastCons and phyloP, Bioinformatics, doi:10.1093/bioinformatics/bty966
Ray, Evaluating medication effects outside of clinical trials: New-user designs, Am. J. Epidemiol, doi:10.1093/aje/kwg231
Remmert, Biegert, Hauser, Söding, HHblits: Lightning-fast iterative protein sequence searching by HMM-HMM alignment, Nat. Methods, doi:10.1038/nmeth.1818
Rosenbaum, Rubin, The central role of the propensity score in observational studies for causal effects, Biometrika, doi:10.1093/biomet/70.1.41
Sammel, Differences in Shedding of the Interleukin-11 Receptor by the Proteases ADAM9, ADAM10, ADAM17, Meprin a, Meprin b and MT1-MMP, Int. J. Mol. Sci, doi:10.3390/ijms20153677
Schneeweiss, A basic study design for expedited safety signal evaluation based on electronic healthcare data, Pharmacoepidemiol. Drug Saf, doi:10.1002/pds.1926
Schneidman-Duhovny, Inbar, Nussinov, Wolfson, PatchDock and SymmDock: Servers for rigid and symmetric docking, Nucleic Acids Res, doi:10.1093/nar/gki481
Shannon, Cytoscape: A software environment for integrated models of biomolecular interaction networks
Smith, Less is more: An adaptive branch-site random effects model for efficient detection of episodic diversifying selection, Mol. Biol. Evol, doi:10.1093/molbev/msv022
Sohda, Identification of a soluble isoform of human IL-17RA generated by alternative splicing, Cytokine, doi:10.1016/j.cyto.2013.09.012
Stoner, Maures, Conant, Methods and systems for guide RNA design and use, U.S. Patent
Sun, Genomic atlas of the human plasma proteome, Nature, doi:10.1038/s41586-018-0175-2
Teo, SAINTexpress: Improvements and additional features in Significance Analysis of INTeractome software, J. Proteomics, doi:10.1016/j.jprot.2013.10.023
Torchala, Moal, Chaleil, Fernandez-Recio, Bates, SwarmDock: A server for flexible protein-protein docking, Bioinformatics, doi:10.1093/bioinformatics/btt038
Tovchigrechko, Vakser, GRAMM-X public web server for protein-protein docking, Nucleic Acids Res, doi:10.1093/nar/gkl206
Was, supported by the National Science Foundation
Waterhouse, SWISS-MODEL: Homology modelling of protein structures and complexes, Nucleic Acids Res, doi:10.1093/nar/gky427
Weeks, De Graef, Munawar, Orf9b from SARS-CoV-2, doi:10.2210/pdb6z4u/pdb
Wei, Tom70 mediates Sendai virus-induced apoptosis on mitochondria, J. Virol, doi:10.1128/JVI.02959-14
Yamada, Komoto, Watanabe, Ohmiya, Takusagawa, Crystal structure and possible catalytic mechanism of microsomal prostaglandin E synthase type 2 (mPGES-2)
Yan, Tao, He, Huang, The HDOCK server for integrated protein-protein docking, Nat. Protoc, doi:10.1038/s41596-020-0312-x
Yang, Improved protein structure prediction using predicted interresidue orientations, Proc. Natl. Acad. Sci. U.S.A, doi:10.1073/pnas.1914677117
Yin, Structural basis for inhibition of the RNAdependent RNA polymerase from SARS-CoV-2 by remdesivir, Science, doi:10.1126/science.abc1560
Young, Effects of a major deletion in the SARS-CoV-2 genome on the severity of infection and the inflammatory response: An observational cohort study, Lancet, doi:10.1016/S0140-6736(20)31757-8
Young, Hoogenraad, Hartl, Molecular chaperones Hsp90 and Hsp70 deliver preproteins to the mitochondrial import receptor Tom70, Cell, doi:10.1016/S0092-8674(02)01250-3
Yu, Wang, Han, He, clusterProfiler: An R package for comparing biological themes among gene clusters, OMICS, doi:10.1089/omi.2011.0118
Zaretsky, Etzyoni, Kaye, Sklair-Tavron, Aharoni, Directed Evolution of a Soluble Human IL-17A Receptor for the Inhibition of Psoriasis Plaque Formation in a Mouse Model, Chem. Biol, doi:10.1016/j.chembiol.2012.11.012
Zhai, Insights into SARS-CoV transcription and replication from the structure of the nsp7-nsp8 hexadecamer, Nat. Struct. Mol. Biol, doi:10.1038/nsmb999
Zheng, MotionCor2: Anisotropic correction of beam-induced motion for improved cryo-electron microscopy, Nat. Methods, doi:10.1038/nmeth.4193
Zhu, Causal associations between risk factors and common diseases inferred from GWAS summary data, Nat. Commun, doi:10.1038/s41467-017-02317-2
Šali, Blundell, Comparative protein modelling by satisfaction of spatial restraints, J. Mol. Biol, doi:10.1006/jmbi.1993.1626
DOI record:
{
"DOI": "10.1126/science.abe9403",
"ISSN": [
"0036-8075",
"1095-9203"
],
"URL": "http://dx.doi.org/10.1126/science.abe9403",
"abstract": "<jats:title>How lethal coronaviruses engage hosts</jats:title>\n <jats:p>\n Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is closely related to the deadly coronaviruses SARS-CoV-1 and Middle East respiratory syndrome coronavirus (MERS-CoV). Considerable efforts are focused on developing treatments, and therapies that work across coronaviruses would be particularly valuable. Shedding light on the host factors hijacked by the viruses, Gordon\n <jats:italic>et al.</jats:italic>\n mapped the interactions between viral and human proteins for SARS-CoV-2, SARS-CoV-1, and MERS-CoV; analyzed the localization of viral proteins in human cells; and used genetic screening to identify host factors that either enhance or inhibit viral infection. For a subset of the interactions essential for the virus life cycle, the authors determined the cryo–electron microscopy structures and mined patient data to understand how targeting host factors may be relevant to clinical outcomes.\n </jats:p>\n <jats:p>\n <jats:italic>Science</jats:italic>\n , this issue p.\n <jats:related-article xmlns:xlink=\"http://www.w3.org/1999/xlink\" ext-link-type=\"doi\" related-article-type=\"in-this-issue\" xlink:href=\"10.1126/science.abe9403\">eabe9403</jats:related-article>\n </jats:p>",
"alternative-id": [
"10.1126/science.abe9403"
],
"author": [
{
"ORCID": "http://orcid.org/0000-0001-7954-0306",
"affiliation": [
{
"name": "Quantitative Biosciences Institute (QBI) COVID-19 Research Group (QCRG), San Francisco, CA 94158, USA."
},
{
"name": "QBI, University of California, San Francisco, CA 94158, USA."
},
{
"name": "Department of Cellular and Molecular Pharmacology, University of California, San Francisco, CA 94158, USA."
},
{
"name": "J. David Gladstone Institutes, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Gordon",
"given": "David E.",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0002-8015-9614",
"affiliation": [
{
"name": "Quantitative Biosciences Institute (QBI) COVID-19 Research Group (QCRG), San Francisco, CA 94158, USA."
},
{
"name": "J. David Gladstone Institutes, San Francisco, CA 94158, USA."
},
{
"name": "Medical Scientist Training Program, University of California, San Francisco, CA 94143, USA."
},
{
"name": "Department of Microbiology and Immunology, University of California, San Francisco, CA 94143, USA."
},
{
"name": "Biomedical Sciences Graduate Program, University of California, San Francisco, CA 94143, USA."
}
],
"authenticated-orcid": true,
"family": "Hiatt",
"given": "Joseph",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-9526-1427",
"affiliation": [
{
"name": "Quantitative Biosciences Institute (QBI) COVID-19 Research Group (QCRG), San Francisco, CA 94158, USA."
},
{
"name": "QBI, University of California, San Francisco, CA 94158, USA."
},
{
"name": "Department of Cellular and Molecular Pharmacology, University of California, San Francisco, CA 94158, USA."
},
{
"name": "J. David Gladstone Institutes, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Bouhaddou",
"given": "Mehdi",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-1571-8325",
"affiliation": [
{
"name": "Viral Populations and Pathogenesis Unit, CNRS UMR 3569, Institut Pasteur, 75724, Paris, cedex 15, France."
}
],
"authenticated-orcid": true,
"family": "Rezelj",
"given": "Veronica V.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-6605-8163",
"affiliation": [
{
"name": "Institute for Clinical and Experimental Pharmacology and Toxicology I, University of Freiburg, 79104 Freiburg, Germany."
}
],
"authenticated-orcid": true,
"family": "Ulferts",
"given": "Svenja",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-7070-2257",
"affiliation": [
{
"name": "Quantitative Biosciences Institute (QBI) COVID-19 Research Group (QCRG), San Francisco, CA 94158, USA."
},
{
"name": "QBI, University of California, San Francisco, CA 94158, USA."
},
{
"name": "Department of Cellular and Molecular Pharmacology, University of California, San Francisco, CA 94158, USA."
},
{
"name": "J. David Gladstone Institutes, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Braberg",
"given": "Hannes",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-6839-1835",
"affiliation": [
{
"name": "Center for Microbial Pathogenesis, Institute for Biomedical Sciences, Georgia State University, Atlanta, GA 30303, USA."
}
],
"authenticated-orcid": true,
"family": "Jureka",
"given": "Alexander S.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-4025-1299",
"affiliation": [
{
"name": "Quantitative Biosciences Institute (QBI) COVID-19 Research Group (QCRG), San Francisco, CA 94158, USA."
},
{
"name": "QBI, University of California, San Francisco, CA 94158, USA."
},
{
"name": "Department of Cellular and Molecular Pharmacology, University of California, San Francisco, CA 94158, USA."
},
{
"name": "J. David Gladstone Institutes, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Obernier",
"given": "Kirsten",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-2857-9870",
"affiliation": [
{
"name": "Quantitative Biosciences Institute (QBI) COVID-19 Research Group (QCRG), San Francisco, CA 94158, USA."
},
{
"name": "QBI, University of California, San Francisco, CA 94158, USA."
},
{
"name": "Department of Cellular and Molecular Pharmacology, University of California, San Francisco, CA 94158, USA."
},
{
"name": "J. David Gladstone Institutes, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Guo",
"given": "Jeffrey Z.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-2335-0607",
"affiliation": [
{
"name": "Quantitative Biosciences Institute (QBI) COVID-19 Research Group (QCRG), San Francisco, CA 94158, USA."
},
{
"name": "QBI, University of California, San Francisco, CA 94158, USA."
},
{
"name": "Department of Cellular and Molecular Pharmacology, University of California, San Francisco, CA 94158, USA."
},
{
"name": "J. David Gladstone Institutes, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Batra",
"given": "Jyoti",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-8341-3067",
"affiliation": [
{
"name": "Quantitative Biosciences Institute (QBI) COVID-19 Research Group (QCRG), San Francisco, CA 94158, USA."
},
{
"name": "QBI, University of California, San Francisco, CA 94158, USA."
},
{
"name": "Department of Cellular and Molecular Pharmacology, University of California, San Francisco, CA 94158, USA."
},
{
"name": "J. David Gladstone Institutes, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Kaake",
"given": "Robyn M.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-6227-6796",
"affiliation": [
{
"name": "Aetion, Inc., New York, NY 10001, USA."
}
],
"authenticated-orcid": true,
"family": "Weckstein",
"given": "Andrew R.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-7423-4879",
"affiliation": [
{
"name": "QBI Coronavirus Research Group Structural Biology Consortium, University of California, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Owens",
"given": "Tristan W.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-7432-3211",
"affiliation": [
{
"name": "QBI Coronavirus Research Group Structural Biology Consortium, University of California, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Gupta",
"given": "Meghna",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-7537-6016",
"affiliation": [
{
"name": "QBI Coronavirus Research Group Structural Biology Consortium, University of California, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Pourmal",
"given": "Sergei",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-6868-9121",
"affiliation": [
{
"name": "QBI Coronavirus Research Group Structural Biology Consortium, University of California, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Titus",
"given": "Erron W.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-1803-5693",
"affiliation": [
{
"name": "Quantitative Biosciences Institute (QBI) COVID-19 Research Group (QCRG), San Francisco, CA 94158, USA."
},
{
"name": "QBI, University of California, San Francisco, CA 94158, USA."
},
{
"name": "Department of Cellular and Molecular Pharmacology, University of California, San Francisco, CA 94158, USA."
},
{
"name": "J. David Gladstone Institutes, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Cakir",
"given": "Merve",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-0370-6653",
"affiliation": [
{
"name": "Quantitative Biosciences Institute (QBI) COVID-19 Research Group (QCRG), San Francisco, CA 94158, USA."
},
{
"name": "QBI, University of California, San Francisco, CA 94158, USA."
},
{
"name": "Department of Cellular and Molecular Pharmacology, University of California, San Francisco, CA 94158, USA."
},
{
"name": "J. David Gladstone Institutes, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Soucheray",
"given": "Margaret",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-5281-5736",
"affiliation": [
{
"name": "Quantitative Biosciences Institute (QBI) COVID-19 Research Group (QCRG), San Francisco, CA 94158, USA."
},
{
"name": "QBI, University of California, San Francisco, CA 94158, USA."
},
{
"name": "Department of Cellular and Molecular Pharmacology, University of California, San Francisco, CA 94158, USA."
},
{
"name": "J. David Gladstone Institutes, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "McGregor",
"given": "Michael",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Quantitative Biosciences Institute (QBI) COVID-19 Research Group (QCRG), San Francisco, CA 94158, USA."
},
{
"name": "QBI, University of California, San Francisco, CA 94158, USA."
},
{
"name": "Department of Cellular and Molecular Pharmacology, University of California, San Francisco, CA 94158, USA."
},
{
"name": "J. David Gladstone Institutes, San Francisco, CA 94158, USA."
}
],
"family": "Cakir",
"given": "Zeynep",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-7806-9874",
"affiliation": [
{
"name": "Quantitative Biosciences Institute (QBI) COVID-19 Research Group (QCRG), San Francisco, CA 94158, USA."
},
{
"name": "QBI, University of California, San Francisco, CA 94158, USA."
},
{
"name": "Department of Cellular and Molecular Pharmacology, University of California, San Francisco, CA 94158, USA."
},
{
"name": "J. David Gladstone Institutes, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Jang",
"given": "Gwendolyn",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-3128-5331",
"affiliation": [
{
"name": "Department of Computational Medicine and Bioinformatics, University of Michigan, Ann Arbor, MI 48109, USA."
}
],
"authenticated-orcid": true,
"family": "O’Meara",
"given": "Matthew J.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-9155-820X",
"affiliation": [
{
"name": "Quantitative Biosciences Institute (QBI) COVID-19 Research Group (QCRG), San Francisco, CA 94158, USA."
},
{
"name": "QBI, University of California, San Francisco, CA 94158, USA."
},
{
"name": "Department of Pharmaceutical Chemistry, University of California, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Tummino",
"given": "Tia A.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-0541-7211",
"affiliation": [
{
"name": "Quantitative Biosciences Institute (QBI) COVID-19 Research Group (QCRG), San Francisco, CA 94158, USA."
},
{
"name": "QBI, University of California, San Francisco, CA 94158, USA."
},
{
"name": "Department of Cellular and Molecular Pharmacology, University of California, San Francisco, CA 94158, USA."
},
{
"name": "Howard Hughes Medical Institute, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Zhang",
"given": "Ziyang",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-5063-113X",
"affiliation": [
{
"name": "Quantitative Biosciences Institute (QBI) COVID-19 Research Group (QCRG), San Francisco, CA 94158, USA."
},
{
"name": "QBI, University of California, San Francisco, CA 94158, USA."
},
{
"name": "Department of Cellular and Molecular Pharmacology, University of California, San Francisco, CA 94158, USA."
},
{
"name": "J. David Gladstone Institutes, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Foussard",
"given": "Helene",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-6183-7109",
"affiliation": [
{
"name": "Quantitative Biosciences Institute (QBI) COVID-19 Research Group (QCRG), San Francisco, CA 94158, USA."
},
{
"name": "QBI, University of California, San Francisco, CA 94158, USA."
},
{
"name": "Department of Cellular and Molecular Pharmacology, University of California, San Francisco, CA 94158, USA."
},
{
"name": "J. David Gladstone Institutes, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Rojc",
"given": "Ajda",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-1393-5476",
"affiliation": [
{
"name": "Quantitative Biosciences Institute (QBI) COVID-19 Research Group (QCRG), San Francisco, CA 94158, USA."
},
{
"name": "QBI, University of California, San Francisco, CA 94158, USA."
},
{
"name": "Department of Cellular and Molecular Pharmacology, University of California, San Francisco, CA 94158, USA."
},
{
"name": "J. David Gladstone Institutes, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Zhou",
"given": "Yuan",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Quantitative Biosciences Institute (QBI) COVID-19 Research Group (QCRG), San Francisco, CA 94158, USA."
},
{
"name": "QBI, University of California, San Francisco, CA 94158, USA."
},
{
"name": "Department of Cellular and Molecular Pharmacology, University of California, San Francisco, CA 94158, USA."
},
{
"name": "J. David Gladstone Institutes, San Francisco, CA 94158, USA."
}
],
"family": "Kuchenov",
"given": "Dmitry",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-0896-5910",
"affiliation": [
{
"name": "Quantitative Biosciences Institute (QBI) COVID-19 Research Group (QCRG), San Francisco, CA 94158, USA."
},
{
"name": "QBI, University of California, San Francisco, CA 94158, USA."
},
{
"name": "Department of Cellular and Molecular Pharmacology, University of California, San Francisco, CA 94158, USA."
},
{
"name": "J. David Gladstone Institutes, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Hüttenhain",
"given": "Ruth",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-8647-4172",
"affiliation": [
{
"name": "Quantitative Biosciences Institute (QBI) COVID-19 Research Group (QCRG), San Francisco, CA 94158, USA."
},
{
"name": "QBI, University of California, San Francisco, CA 94158, USA."
},
{
"name": "Department of Cellular and Molecular Pharmacology, University of California, San Francisco, CA 94158, USA."
},
{
"name": "J. David Gladstone Institutes, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Xu",
"given": "Jiewei",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-8143-6129",
"affiliation": [
{
"name": "Quantitative Biosciences Institute (QBI) COVID-19 Research Group (QCRG), San Francisco, CA 94158, USA."
},
{
"name": "QBI, University of California, San Francisco, CA 94158, USA."
},
{
"name": "Department of Cellular and Molecular Pharmacology, University of California, San Francisco, CA 94158, USA."
},
{
"name": "J. David Gladstone Institutes, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Eckhardt",
"given": "Manon",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-6119-6084",
"affiliation": [
{
"name": "Quantitative Biosciences Institute (QBI) COVID-19 Research Group (QCRG), San Francisco, CA 94158, USA."
},
{
"name": "QBI, University of California, San Francisco, CA 94158, USA."
},
{
"name": "Department of Cellular and Molecular Pharmacology, University of California, San Francisco, CA 94158, USA."
},
{
"name": "J. David Gladstone Institutes, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Swaney",
"given": "Danielle L.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Quantitative Biosciences Institute (QBI) COVID-19 Research Group (QCRG), San Francisco, CA 94158, USA."
},
{
"name": "QBI, University of California, San Francisco, CA 94158, USA."
}
],
"family": "Fabius",
"given": "Jacqueline M.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Quantitative Biosciences Institute (QBI) COVID-19 Research Group (QCRG), San Francisco, CA 94158, USA."
},
{
"name": "QBI, University of California, San Francisco, CA 94158, USA."
},
{
"name": "Department of Cellular and Molecular Pharmacology, University of California, San Francisco, CA 94158, USA."
},
{
"name": "J. David Gladstone Institutes, San Francisco, CA 94158, USA."
}
],
"family": "Ummadi",
"given": "Manisha",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-5458-2988",
"affiliation": [
{
"name": "Quantitative Biosciences Institute (QBI) COVID-19 Research Group (QCRG), San Francisco, CA 94158, USA."
},
{
"name": "QBI, University of California, San Francisco, CA 94158, USA."
},
{
"name": "Department of Cellular and Molecular Pharmacology, University of California, San Francisco, CA 94158, USA."
},
{
"name": "J. David Gladstone Institutes, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Tutuncuoglu",
"given": "Beril",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-0329-7431",
"affiliation": [
{
"name": "Quantitative Biosciences Institute (QBI) COVID-19 Research Group (QCRG), San Francisco, CA 94158, USA."
},
{
"name": "QBI, University of California, San Francisco, CA 94158, USA."
},
{
"name": "Department of Cellular and Molecular Pharmacology, University of California, San Francisco, CA 94158, USA."
},
{
"name": "J. David Gladstone Institutes, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Rathore",
"given": "Ujjwal",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-0670-6683",
"affiliation": [
{
"name": "Quantitative Biosciences Institute (QBI) COVID-19 Research Group (QCRG), San Francisco, CA 94158, USA."
},
{
"name": "QBI, University of California, San Francisco, CA 94158, USA."
},
{
"name": "Department of Cellular and Molecular Pharmacology, University of California, San Francisco, CA 94158, USA."
},
{
"name": "J. David Gladstone Institutes, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Modak",
"given": "Maya",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-8303-457X",
"affiliation": [
{
"name": "Quantitative Biosciences Institute (QBI) COVID-19 Research Group (QCRG), San Francisco, CA 94158, USA."
},
{
"name": "QBI, University of California, San Francisco, CA 94158, USA."
},
{
"name": "Department of Cellular and Molecular Pharmacology, University of California, San Francisco, CA 94158, USA."
},
{
"name": "J. David Gladstone Institutes, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Haas",
"given": "Paige",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-1463-6726",
"affiliation": [
{
"name": "Quantitative Biosciences Institute (QBI) COVID-19 Research Group (QCRG), San Francisco, CA 94158, USA."
},
{
"name": "QBI, University of California, San Francisco, CA 94158, USA."
},
{
"name": "Department of Cellular and Molecular Pharmacology, University of California, San Francisco, CA 94158, USA."
},
{
"name": "J. David Gladstone Institutes, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Haas",
"given": "Kelsey M.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-6320-5084",
"affiliation": [
{
"name": "Quantitative Biosciences Institute (QBI) COVID-19 Research Group (QCRG), San Francisco, CA 94158, USA."
},
{
"name": "QBI, University of California, San Francisco, CA 94158, USA."
},
{
"name": "Department of Cellular and Molecular Pharmacology, University of California, San Francisco, CA 94158, USA."
},
{
"name": "J. David Gladstone Institutes, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Naing",
"given": "Zun Zar Chi",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-3616-9743",
"affiliation": [
{
"name": "Quantitative Biosciences Institute (QBI) COVID-19 Research Group (QCRG), San Francisco, CA 94158, USA."
},
{
"name": "QBI, University of California, San Francisco, CA 94158, USA."
},
{
"name": "Department of Cellular and Molecular Pharmacology, University of California, San Francisco, CA 94158, USA."
},
{
"name": "J. David Gladstone Institutes, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Pulido",
"given": "Ernst H.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Quantitative Biosciences Institute (QBI) COVID-19 Research Group (QCRG), San Francisco, CA 94158, USA."
},
{
"name": "QBI, University of California, San Francisco, CA 94158, USA."
},
{
"name": "Department of Cellular and Molecular Pharmacology, University of California, San Francisco, CA 94158, USA."
},
{
"name": "Howard Hughes Medical Institute, San Francisco, CA 94158, USA."
}
],
"family": "Shi",
"given": "Ying",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-5686-0451",
"affiliation": [
{
"name": "European Molecular Biology Laboratory, European Bioinformatics Institute (EMBL-EBI), Wellcome Genome Campus, Hinxton, Cambridgeshire CB10 1SD, UK."
}
],
"authenticated-orcid": true,
"family": "Barrio-Hernandez",
"given": "Inigo",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "European Molecular Biology Laboratory, European Bioinformatics Institute (EMBL-EBI), Wellcome Genome Campus, Hinxton, Cambridgeshire CB10 1SD, UK."
}
],
"family": "Memon",
"given": "Danish",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-7514-4362",
"affiliation": [
{
"name": "European Molecular Biology Laboratory, European Bioinformatics Institute (EMBL-EBI), Wellcome Genome Campus, Hinxton, Cambridgeshire CB10 1SD, UK."
}
],
"authenticated-orcid": true,
"family": "Petsalaki",
"given": "Eirini",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-9076-3025",
"affiliation": [
{
"name": "European Molecular Biology Laboratory, European Bioinformatics Institute (EMBL-EBI), Wellcome Genome Campus, Hinxton, Cambridgeshire CB10 1SD, UK."
}
],
"authenticated-orcid": true,
"family": "Dunham",
"given": "Alistair",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-3840-3273",
"affiliation": [
{
"name": "European Molecular Biology Laboratory, European Bioinformatics Institute (EMBL-EBI), Wellcome Genome Campus, Hinxton, Cambridgeshire CB10 1SD, UK."
}
],
"authenticated-orcid": true,
"family": "Marrero",
"given": "Miguel Correa",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-8830-3951",
"affiliation": [
{
"name": "European Molecular Biology Laboratory, European Bioinformatics Institute (EMBL-EBI), Wellcome Genome Campus, Hinxton, Cambridgeshire CB10 1SD, UK."
}
],
"authenticated-orcid": true,
"family": "Burke",
"given": "David",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-2466-6731",
"affiliation": [
{
"name": "Viral Populations and Pathogenesis Unit, CNRS UMR 3569, Institut Pasteur, 75724, Paris, cedex 15, France."
}
],
"authenticated-orcid": true,
"family": "Koh",
"given": "Cassandra",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-7775-7448",
"affiliation": [
{
"name": "Viral Populations and Pathogenesis Unit, CNRS UMR 3569, Institut Pasteur, 75724, Paris, cedex 15, France."
}
],
"authenticated-orcid": true,
"family": "Vallet",
"given": "Thomas",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-1200-803X",
"affiliation": [
{
"name": "Center for Microbial Pathogenesis, Institute for Biomedical Sciences, Georgia State University, Atlanta, GA 30303, USA."
}
],
"authenticated-orcid": true,
"family": "Silvas",
"given": "Jesus A.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-3484-9921",
"affiliation": [
{
"name": "QBI Coronavirus Research Group Structural Biology Consortium, University of California, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Azumaya",
"given": "Caleigh M.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-8084-1552",
"affiliation": [
{
"name": "QBI Coronavirus Research Group Structural Biology Consortium, University of California, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Billesbølle",
"given": "Christian",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-8548-4224",
"affiliation": [
{
"name": "QBI Coronavirus Research Group Structural Biology Consortium, University of California, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Brilot",
"given": "Axel F.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-1909-5751",
"affiliation": [
{
"name": "QBI Coronavirus Research Group Structural Biology Consortium, University of California, San Francisco, CA 94158, USA."
},
{
"name": "Division of Basic Sciences, Fred Hutchinson Cancer Research Center, Seattle, WA 98109, USA."
}
],
"authenticated-orcid": true,
"family": "Campbell",
"given": "Melody G.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-9843-2255",
"affiliation": [
{
"name": "QBI Coronavirus Research Group Structural Biology Consortium, University of California, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Diallo",
"given": "Amy",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-8016-1570",
"affiliation": [
{
"name": "QBI Coronavirus Research Group Structural Biology Consortium, University of California, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Dickinson",
"given": "Miles Sasha",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-4285-435X",
"affiliation": [
{
"name": "QBI Coronavirus Research Group Structural Biology Consortium, University of California, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Diwanji",
"given": "Devan",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "QBI Coronavirus Research Group Structural Biology Consortium, University of California, San Francisco, CA 94158, USA."
}
],
"family": "Herrera",
"given": "Nadia",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-0265-5337",
"affiliation": [
{
"name": "QBI Coronavirus Research Group Structural Biology Consortium, University of California, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Hoppe",
"given": "Nick",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-8039-6823",
"affiliation": [
{
"name": "QBI Coronavirus Research Group Structural Biology Consortium, University of California, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Kratochvil",
"given": "Huong T.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-2253-3698",
"affiliation": [
{
"name": "QBI Coronavirus Research Group Structural Biology Consortium, University of California, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Liu",
"given": "Yanxin",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-0842-4935",
"affiliation": [
{
"name": "QBI Coronavirus Research Group Structural Biology Consortium, University of California, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Merz",
"given": "Gregory E.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-3811-5623",
"affiliation": [
{
"name": "QBI Coronavirus Research Group Structural Biology Consortium, University of California, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Moritz",
"given": "Michelle",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-6142-8807",
"affiliation": [
{
"name": "QBI Coronavirus Research Group Structural Biology Consortium, University of California, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Nguyen",
"given": "Henry C.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-1260-0279",
"affiliation": [
{
"name": "QBI Coronavirus Research Group Structural Biology Consortium, University of California, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Nowotny",
"given": "Carlos",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-3240-4176",
"affiliation": [
{
"name": "QBI Coronavirus Research Group Structural Biology Consortium, University of California, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Puchades",
"given": "Cristina",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-4813-6348",
"affiliation": [
{
"name": "QBI Coronavirus Research Group Structural Biology Consortium, University of California, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Rizo",
"given": "Alexandrea N.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-3919-4474",
"affiliation": [
{
"name": "QBI Coronavirus Research Group Structural Biology Consortium, University of California, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Schulze-Gahmen",
"given": "Ursula",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-0669-1589",
"affiliation": [
{
"name": "QBI Coronavirus Research Group Structural Biology Consortium, University of California, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Smith",
"given": "Amber M.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-4413-2502",
"affiliation": [
{
"name": "QBI Coronavirus Research Group Structural Biology Consortium, University of California, San Francisco, CA 94158, USA."
},
{
"name": "Beam Therapeutics, Cambridge, MA 02139, USA."
}
],
"authenticated-orcid": true,
"family": "Sun",
"given": "Ming",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-4713-9504",
"affiliation": [
{
"name": "QBI Coronavirus Research Group Structural Biology Consortium, University of California, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Young",
"given": "Iris D.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-4997-766X",
"affiliation": [
{
"name": "QBI Coronavirus Research Group Structural Biology Consortium, University of California, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Zhao",
"given": "Jianhua",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "QBI Coronavirus Research Group Structural Biology Consortium, University of California, San Francisco, CA 94158, USA."
}
],
"family": "Asarnow",
"given": "Daniel",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-0935-8362",
"affiliation": [
{
"name": "QBI Coronavirus Research Group Structural Biology Consortium, University of California, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Biel",
"given": "Justin",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-8518-6697",
"affiliation": [
{
"name": "QBI Coronavirus Research Group Structural Biology Consortium, University of California, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Bowen",
"given": "Alisa",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-1170-5140",
"affiliation": [
{
"name": "QBI Coronavirus Research Group Structural Biology Consortium, University of California, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Braxton",
"given": "Julian R.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "QBI Coronavirus Research Group Structural Biology Consortium, University of California, San Francisco, CA 94158, USA."
}
],
"family": "Chen",
"given": "Jen",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-8381-1957",
"affiliation": [
{
"name": "QBI Coronavirus Research Group Structural Biology Consortium, University of California, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Chio",
"given": "Cynthia M.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-5295-2690",
"affiliation": [
{
"name": "QBI Coronavirus Research Group Structural Biology Consortium, University of California, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Chio",
"given": "Un Seng",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-8276-9635",
"affiliation": [
{
"name": "QBI Coronavirus Research Group Structural Biology Consortium, University of California, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Deshpande",
"given": "Ishan",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "QBI Coronavirus Research Group Structural Biology Consortium, University of California, San Francisco, CA 94158, USA."
}
],
"family": "Doan",
"given": "Loan",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-4126-6409",
"affiliation": [
{
"name": "QBI Coronavirus Research Group Structural Biology Consortium, University of California, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Faust",
"given": "Bryan",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-6812-3988",
"affiliation": [
{
"name": "QBI Coronavirus Research Group Structural Biology Consortium, University of California, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Flores",
"given": "Sebastian",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-4961-7143",
"affiliation": [
{
"name": "QBI Coronavirus Research Group Structural Biology Consortium, University of California, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Jin",
"given": "Mingliang",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-8821-6663",
"affiliation": [
{
"name": "QBI Coronavirus Research Group Structural Biology Consortium, University of California, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Kim",
"given": "Kate",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "QBI Coronavirus Research Group Structural Biology Consortium, University of California, San Francisco, CA 94158, USA."
}
],
"family": "Lam",
"given": "Victor L.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-0720-3129",
"affiliation": [
{
"name": "QBI Coronavirus Research Group Structural Biology Consortium, University of California, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Li",
"given": "Fei",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-7426-9596",
"affiliation": [
{
"name": "QBI Coronavirus Research Group Structural Biology Consortium, University of California, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Li",
"given": "Junrui",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-7095-3507",
"affiliation": [
{
"name": "QBI Coronavirus Research Group Structural Biology Consortium, University of California, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Li",
"given": "Yen-Li",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-0216-0350",
"affiliation": [
{
"name": "QBI Coronavirus Research Group Structural Biology Consortium, University of California, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Li",
"given": "Yang",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-9002-3553",
"affiliation": [
{
"name": "QBI Coronavirus Research Group Structural Biology Consortium, University of California, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Liu",
"given": "Xi",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-6387-8182",
"affiliation": [
{
"name": "QBI Coronavirus Research Group Structural Biology Consortium, University of California, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Lo",
"given": "Megan",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "QBI Coronavirus Research Group Structural Biology Consortium, University of California, San Francisco, CA 94158, USA."
}
],
"family": "Lopez",
"given": "Kyle E.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-9345-1462",
"affiliation": [
{
"name": "QBI Coronavirus Research Group Structural Biology Consortium, University of California, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Melo",
"given": "Arthur A.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-6149-6447",
"affiliation": [
{
"name": "QBI Coronavirus Research Group Structural Biology Consortium, University of California, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Moss",
"given": "Frank R.",
"sequence": "additional",
"suffix": "III"
},
{
"affiliation": [
{
"name": "QBI Coronavirus Research Group Structural Biology Consortium, University of California, San Francisco, CA 94158, USA."
}
],
"family": "Nguyen",
"given": "Phuong",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-8846-822X",
"affiliation": [
{
"name": "QBI Coronavirus Research Group Structural Biology Consortium, University of California, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Paulino",
"given": "Joana",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-1968-9851",
"affiliation": [
{
"name": "QBI Coronavirus Research Group Structural Biology Consortium, University of California, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Pawar",
"given": "Komal Ishwar",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-3541-7431",
"affiliation": [
{
"name": "QBI Coronavirus Research Group Structural Biology Consortium, University of California, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Peters",
"given": "Jessica K.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-3630-3794",
"affiliation": [
{
"name": "QBI Coronavirus Research Group Structural Biology Consortium, University of California, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Pospiech",
"given": "Thomas H.",
"sequence": "additional",
"suffix": "Jr."
},
{
"ORCID": "http://orcid.org/0000-0002-9511-6481",
"affiliation": [
{
"name": "QBI Coronavirus Research Group Structural Biology Consortium, University of California, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Safari",
"given": "Maliheh",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-3772-7142",
"affiliation": [
{
"name": "QBI Coronavirus Research Group Structural Biology Consortium, University of California, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Sangwan",
"given": "Smriti",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "QBI Coronavirus Research Group Structural Biology Consortium, University of California, San Francisco, CA 94158, USA."
}
],
"family": "Schaefer",
"given": "Kaitlin",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-6772-3997",
"affiliation": [
{
"name": "QBI Coronavirus Research Group Structural Biology Consortium, University of California, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Thomas",
"given": "Paul V.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-1423-8189",
"affiliation": [
{
"name": "QBI Coronavirus Research Group Structural Biology Consortium, University of California, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Thwin",
"given": "Aye C.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-1748-0517",
"affiliation": [
{
"name": "QBI Coronavirus Research Group Structural Biology Consortium, University of California, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Trenker",
"given": "Raphael",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-2082-9006",
"affiliation": [
{
"name": "QBI Coronavirus Research Group Structural Biology Consortium, University of California, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Tse",
"given": "Eric",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-5741-1941",
"affiliation": [
{
"name": "QBI Coronavirus Research Group Structural Biology Consortium, University of California, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Tsui",
"given": "Tsz Kin Martin",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-1233-2745",
"affiliation": [
{
"name": "QBI Coronavirus Research Group Structural Biology Consortium, University of California, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Wang",
"given": "Feng",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-9073-2093",
"affiliation": [
{
"name": "QBI Coronavirus Research Group Structural Biology Consortium, University of California, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Whitis",
"given": "Natalie",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-8381-8788",
"affiliation": [
{
"name": "QBI Coronavirus Research Group Structural Biology Consortium, University of California, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Yu",
"given": "Zanlin",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-3734-3624",
"affiliation": [
{
"name": "QBI Coronavirus Research Group Structural Biology Consortium, University of California, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Zhang",
"given": "Kaihua",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-7497-3206",
"affiliation": [
{
"name": "QBI Coronavirus Research Group Structural Biology Consortium, University of California, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Zhang",
"given": "Yang",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "QBI Coronavirus Research Group Structural Biology Consortium, University of California, San Francisco, CA 94158, USA."
}
],
"family": "Zhou",
"given": "Fengbo",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-8641-6194",
"affiliation": [
{
"name": "Quantitative Biosciences Institute (QBI) COVID-19 Research Group (QCRG), San Francisco, CA 94158, USA."
},
{
"name": "QBI, University of California, San Francisco, CA 94158, USA."
},
{
"name": "Department of Bioengineering and Therapeutic Sciences, University of California, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Saltzberg",
"given": "Daniel",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-5906-0794",
"affiliation": [
{
"name": "Department of Biomedical Science, Centre for Membrane Interactions and Dynamics, University of Sheffield, Firth Court, Sheffield S10 2TN, UK."
}
],
"authenticated-orcid": true,
"family": "Hodder",
"given": "Anthony J.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-6439-7893",
"affiliation": [
{
"name": "Department of Biomedical Science, Centre for Membrane Interactions and Dynamics, University of Sheffield, Firth Court, Sheffield S10 2TN, UK."
}
],
"authenticated-orcid": true,
"family": "Shun-Shion",
"given": "Amber S.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-8483-021X",
"affiliation": [
{
"name": "Department of Biomedical Science, Centre for Membrane Interactions and Dynamics, University of Sheffield, Firth Court, Sheffield S10 2TN, UK."
}
],
"authenticated-orcid": true,
"family": "Williams",
"given": "Daniel M.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-0889-0506",
"affiliation": [
{
"name": "Department of Microbiology, Icahn School of Medicine at Mount Sinai, New York, NY 10029, USA."
},
{
"name": "Global Health and Emerging Pathogens Institute, Icahn School of Medicine at Mount Sinai, New York, NY 10029, USA."
}
],
"authenticated-orcid": true,
"family": "White",
"given": "Kris M.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-5326-4753",
"affiliation": [
{
"name": "Department of Microbiology, Icahn School of Medicine at Mount Sinai, New York, NY 10029, USA."
},
{
"name": "Global Health and Emerging Pathogens Institute, Icahn School of Medicine at Mount Sinai, New York, NY 10029, USA."
}
],
"authenticated-orcid": true,
"family": "Rosales",
"given": "Romel",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-6433-0098",
"affiliation": [
{
"name": "Department of Microbiology, Icahn School of Medicine at Mount Sinai, New York, NY 10029, USA."
},
{
"name": "Global Health and Emerging Pathogens Institute, Icahn School of Medicine at Mount Sinai, New York, NY 10029, USA."
}
],
"authenticated-orcid": true,
"family": "Kehrer",
"given": "Thomas",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-0989-3178",
"affiliation": [
{
"name": "Department of Microbiology, Icahn School of Medicine at Mount Sinai, New York, NY 10029, USA."
},
{
"name": "Global Health and Emerging Pathogens Institute, Icahn School of Medicine at Mount Sinai, New York, NY 10029, USA."
}
],
"authenticated-orcid": true,
"family": "Miorin",
"given": "Lisa",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-2301-4558",
"affiliation": [
{
"name": "Department of Microbiology, Icahn School of Medicine at Mount Sinai, New York, NY 10029, USA."
},
{
"name": "Global Health and Emerging Pathogens Institute, Icahn School of Medicine at Mount Sinai, New York, NY 10029, USA."
}
],
"authenticated-orcid": true,
"family": "Moreno",
"given": "Elena",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-4600-2047",
"affiliation": [
{
"name": "MRC–University of Glasgow Centre for Virus Research, Glasgow G61 1QH, Scotland, UK."
}
],
"authenticated-orcid": true,
"family": "Patel",
"given": "Arvind H.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-9495-4056",
"affiliation": [
{
"name": "MRC–University of Glasgow Centre for Virus Research, Glasgow G61 1QH, Scotland, UK."
}
],
"authenticated-orcid": true,
"family": "Rihn",
"given": "Suzannah",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-1862-6795",
"affiliation": [
{
"name": "J. David Gladstone Institutes, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Khalid",
"given": "Mir M.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-4815-5039",
"affiliation": [
{
"name": "J. David Gladstone Institutes, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Vallejo-Gracia",
"given": "Albert",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-6710-1506",
"affiliation": [
{
"name": "J. David Gladstone Institutes, San Francisco, CA 94158, USA."
},
{
"name": "Medical Scientist Training Program, University of California, San Francisco, CA 94143, USA."
},
{
"name": "Biomedical Sciences Graduate Program, University of California, San Francisco, CA 94143, USA."
}
],
"authenticated-orcid": true,
"family": "Fozouni",
"given": "Parinaz",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-9222-8130",
"affiliation": [
{
"name": "J. David Gladstone Institutes, San Francisco, CA 94158, USA."
},
{
"name": "Biomedical Sciences Graduate Program, University of California, San Francisco, CA 94143, USA."
}
],
"authenticated-orcid": true,
"family": "Simoneau",
"given": "Camille R.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Medical Scientist Training Program, University of California, San Francisco, CA 94143, USA."
},
{
"name": "Department of Microbiology and Immunology, University of California, San Francisco, CA 94143, USA."
},
{
"name": "Biomedical Sciences Graduate Program, University of California, San Francisco, CA 94143, USA."
}
],
"family": "Roth",
"given": "Theodore L.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Medical Scientist Training Program, University of California, San Francisco, CA 94143, USA."
},
{
"name": "Biomedical Sciences Graduate Program, University of California, San Francisco, CA 94143, USA."
}
],
"family": "Wu",
"given": "David",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Wellcome Trust Sanger Institute, Wellcome Genome Campus, Hinxton, Cambridgeshire CB10 1SA, UK."
},
{
"name": "Open Targets, Wellcome Genome Campus, Hinxton, Cambridgeshire CB10 1SD, UK."
}
],
"family": "Karim",
"given": "Mohd Anisul",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-2415-2143",
"affiliation": [
{
"name": "Wellcome Trust Sanger Institute, Wellcome Genome Campus, Hinxton, Cambridgeshire CB10 1SA, UK."
},
{
"name": "Open Targets, Wellcome Genome Campus, Hinxton, Cambridgeshire CB10 1SD, UK."
}
],
"authenticated-orcid": true,
"family": "Ghoussaini",
"given": "Maya",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-2525-5598",
"affiliation": [
{
"name": "European Molecular Biology Laboratory, European Bioinformatics Institute (EMBL-EBI), Wellcome Genome Campus, Hinxton, Cambridgeshire CB10 1SD, UK."
},
{
"name": "Open Targets, Wellcome Genome Campus, Hinxton, Cambridgeshire CB10 1SD, UK."
}
],
"authenticated-orcid": true,
"family": "Dunham",
"given": "Ian",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Dipartimento di Farmacia-Scienze del Farmaco, Università degli Studi di Bari ‘ALDO MORO’, Via Orabona, 4 70125, Bari, Italy."
}
],
"family": "Berardi",
"given": "Francesco",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-8415-6920",
"affiliation": [
{
"name": "Institute of Virology, Medical Center–University of Freiburg, 79104 Freiburg, Germany."
}
],
"authenticated-orcid": true,
"family": "Weigang",
"given": "Sebastian",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-3144-5032",
"affiliation": [
{
"name": "Département de Virologie, CNRS UMR 3569, Institut Pasteur, Paris 75015, France."
}
],
"authenticated-orcid": true,
"family": "Chazal",
"given": "Maxime",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-3077-1979",
"affiliation": [
{
"name": "Department of Medicine, University of California, San Diego, CA 92093, USA."
}
],
"authenticated-orcid": true,
"family": "Park",
"given": "Jisoo",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-7410-9741",
"affiliation": [
{
"name": "Department of Microbiology and Immunology, University of Maryland School of Medicine, Baltimore, MD 21201, USA."
}
],
"authenticated-orcid": true,
"family": "Logue",
"given": "James",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-7451-4958",
"affiliation": [
{
"name": "Department of Microbiology and Immunology, University of Maryland School of Medicine, Baltimore, MD 21201, USA."
}
],
"authenticated-orcid": true,
"family": "McGrath",
"given": "Marisa",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-9840-2953",
"affiliation": [
{
"name": "Department of Microbiology and Immunology, University of Maryland School of Medicine, Baltimore, MD 21201, USA."
}
],
"authenticated-orcid": true,
"family": "Weston",
"given": "Stuart",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-8300-7184",
"affiliation": [
{
"name": "Department of Microbiology and Immunology, University of Maryland School of Medicine, Baltimore, MD 21201, USA."
}
],
"authenticated-orcid": true,
"family": "Haupt",
"given": "Robert",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-7164-4098",
"affiliation": [
{
"name": "MRC Protein Phosphorylation and Ubiquitylation Unit, College of Life Sciences, University of Dundee, Dundee DD1 5EH, UK."
}
],
"authenticated-orcid": true,
"family": "Hastie",
"given": "C. James",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-1223-3253",
"affiliation": [
{
"name": "MRC Protein Phosphorylation and Ubiquitylation Unit, College of Life Sciences, University of Dundee, Dundee DD1 5EH, UK."
}
],
"authenticated-orcid": true,
"family": "Elliott",
"given": "Matthew",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-5677-2945",
"affiliation": [
{
"name": "MRC Protein Phosphorylation and Ubiquitylation Unit, College of Life Sciences, University of Dundee, Dundee DD1 5EH, UK."
}
],
"authenticated-orcid": true,
"family": "Brown",
"given": "Fiona",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-8086-1078",
"affiliation": [
{
"name": "MRC Protein Phosphorylation and Ubiquitylation Unit, College of Life Sciences, University of Dundee, Dundee DD1 5EH, UK."
}
],
"authenticated-orcid": true,
"family": "Burness",
"given": "Kerry A.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-8095-7387",
"affiliation": [
{
"name": "MRC Protein Phosphorylation and Ubiquitylation Unit, College of Life Sciences, University of Dundee, Dundee DD1 5EH, UK."
}
],
"authenticated-orcid": true,
"family": "Reid",
"given": "Elaine",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-5765-0926",
"affiliation": [
{
"name": "MRC Protein Phosphorylation and Ubiquitylation Unit, College of Life Sciences, University of Dundee, Dundee DD1 5EH, UK."
}
],
"authenticated-orcid": true,
"family": "Dorward",
"given": "Mark",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "MRC Protein Phosphorylation and Ubiquitylation Unit, College of Life Sciences, University of Dundee, Dundee DD1 5EH, UK."
}
],
"family": "Johnson",
"given": "Clare",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-3839-1556",
"affiliation": [
{
"name": "MRC Protein Phosphorylation and Ubiquitylation Unit, College of Life Sciences, University of Dundee, Dundee DD1 5EH, UK."
}
],
"authenticated-orcid": true,
"family": "Wilkinson",
"given": "Stuart G.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-7539-7979",
"affiliation": [
{
"name": "MRC Protein Phosphorylation and Ubiquitylation Unit, College of Life Sciences, University of Dundee, Dundee DD1 5EH, UK."
}
],
"authenticated-orcid": true,
"family": "Geyer",
"given": "Anna",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-8971-2511",
"affiliation": [
{
"name": "MRC Protein Phosphorylation and Ubiquitylation Unit, College of Life Sciences, University of Dundee, Dundee DD1 5EH, UK."
}
],
"authenticated-orcid": true,
"family": "Giesel",
"given": "Daniel M.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "MRC Protein Phosphorylation and Ubiquitylation Unit, College of Life Sciences, University of Dundee, Dundee DD1 5EH, UK."
}
],
"family": "Baillie",
"given": "Carla",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-3904-9050",
"affiliation": [
{
"name": "MRC Protein Phosphorylation and Ubiquitylation Unit, College of Life Sciences, University of Dundee, Dundee DD1 5EH, UK."
}
],
"authenticated-orcid": true,
"family": "Raggett",
"given": "Samantha",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-2474-1471",
"affiliation": [
{
"name": "MRC Protein Phosphorylation and Ubiquitylation Unit, College of Life Sciences, University of Dundee, Dundee DD1 5EH, UK."
}
],
"authenticated-orcid": true,
"family": "Leech",
"given": "Hannah",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "MRC Protein Phosphorylation and Ubiquitylation Unit, College of Life Sciences, University of Dundee, Dundee DD1 5EH, UK."
}
],
"family": "Toth",
"given": "Rachel",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-1339-9869",
"affiliation": [
{
"name": "MRC Protein Phosphorylation and Ubiquitylation Unit, College of Life Sciences, University of Dundee, Dundee DD1 5EH, UK."
}
],
"authenticated-orcid": true,
"family": "Goodman",
"given": "Nicola",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-7481-0511",
"affiliation": [
{
"name": "J. David Gladstone Institutes, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Keough",
"given": "Kathleen C.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-9579-4178",
"affiliation": [
{
"name": "J. David Gladstone Institutes, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Lind",
"given": "Abigail L.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-2095-3661",
"affiliation": [
{
"name": "HealthVerity, Philadelphia, PA 19103, USA."
}
],
"authenticated-orcid": true,
"family": "Klesh",
"given": "Reyna J.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-9468-7082",
"affiliation": [
{
"name": "Department of Neurology, University of California, San Francisco, CA 94143, USA."
}
],
"authenticated-orcid": true,
"family": "Hemphill",
"given": "Kafi R.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-7824-0950",
"affiliation": [
{
"name": "Synthego Corporation, Redwood City, CA 94063, USA."
}
],
"authenticated-orcid": true,
"family": "Carlson-Stevermer",
"given": "Jared",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-0147-0269",
"affiliation": [
{
"name": "Synthego Corporation, Redwood City, CA 94063, USA."
}
],
"authenticated-orcid": true,
"family": "Oki",
"given": "Jennifer",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-3091-4124",
"affiliation": [
{
"name": "Synthego Corporation, Redwood City, CA 94063, USA."
}
],
"authenticated-orcid": true,
"family": "Holden",
"given": "Kevin",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Synthego Corporation, Redwood City, CA 94063, USA."
}
],
"family": "Maures",
"given": "Travis",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-9870-6196",
"affiliation": [
{
"name": "J. David Gladstone Institutes, San Francisco, CA 94158, USA."
},
{
"name": "Department of Epidemiology & Biostatistics, University of California, San Francisco, CA 94158, USA."
},
{
"name": "Chan-Zuckerberg Biohub, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Pollard",
"given": "Katherine S.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-0435-6197",
"affiliation": [
{
"name": "Quantitative Biosciences Institute (QBI) COVID-19 Research Group (QCRG), San Francisco, CA 94158, USA."
},
{
"name": "QBI, University of California, San Francisco, CA 94158, USA."
},
{
"name": "Department of Pharmaceutical Chemistry, University of California, San Francisco, CA 94158, USA."
},
{
"name": "Department of Bioengineering and Therapeutic Sciences, University of California, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Sali",
"given": "Andrej",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-3512-695X",
"affiliation": [
{
"name": "Quantitative Biosciences Institute (QBI) COVID-19 Research Group (QCRG), San Francisco, CA 94158, USA."
},
{
"name": "QBI, University of California, San Francisco, CA 94158, USA."
},
{
"name": "QBI Coronavirus Research Group Structural Biology Consortium, University of California, San Francisco, CA 94158, USA."
},
{
"name": "Department of Biochemistry and Biophysics, University of California, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Agard",
"given": "David A.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-9535-0369",
"affiliation": [
{
"name": "Quantitative Biosciences Institute (QBI) COVID-19 Research Group (QCRG), San Francisco, CA 94158, USA."
},
{
"name": "QBI, University of California, San Francisco, CA 94158, USA."
},
{
"name": "QBI Coronavirus Research Group Structural Biology Consortium, University of California, San Francisco, CA 94158, USA."
},
{
"name": "Howard Hughes Medical Institute, San Francisco, CA 94158, USA."
},
{
"name": "Department of Biochemistry and Biophysics, University of California, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Cheng",
"given": "Yifan",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-5080-2859",
"affiliation": [
{
"name": "Quantitative Biosciences Institute (QBI) COVID-19 Research Group (QCRG), San Francisco, CA 94158, USA."
},
{
"name": "QBI, University of California, San Francisco, CA 94158, USA."
},
{
"name": "QBI Coronavirus Research Group Structural Biology Consortium, University of California, San Francisco, CA 94158, USA."
},
{
"name": "Department of Bioengineering and Therapeutic Sciences, University of California, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Fraser",
"given": "James S.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-2231-2577",
"affiliation": [
{
"name": "Quantitative Biosciences Institute (QBI) COVID-19 Research Group (QCRG), San Francisco, CA 94158, USA."
},
{
"name": "QBI, University of California, San Francisco, CA 94158, USA."
},
{
"name": "QBI Coronavirus Research Group Structural Biology Consortium, University of California, San Francisco, CA 94158, USA."
},
{
"name": "Department of Biochemistry and Biophysics, University of California, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Frost",
"given": "Adam",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-5129-641X",
"affiliation": [
{
"name": "Quantitative Biosciences Institute (QBI) COVID-19 Research Group (QCRG), San Francisco, CA 94158, USA."
},
{
"name": "QBI, University of California, San Francisco, CA 94158, USA."
},
{
"name": "Department of Cellular and Molecular Pharmacology, University of California, San Francisco, CA 94158, USA."
},
{
"name": "QBI Coronavirus Research Group Structural Biology Consortium, University of California, San Francisco, CA 94158, USA."
},
{
"name": "Cardiovascular Research Institute, University of California, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Jura",
"given": "Natalia",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-8494-680X",
"affiliation": [
{
"name": "Quantitative Biosciences Institute (QBI) COVID-19 Research Group (QCRG), San Francisco, CA 94158, USA."
},
{
"name": "QBI, University of California, San Francisco, CA 94158, USA."
},
{
"name": "QBI Coronavirus Research Group Structural Biology Consortium, University of California, San Francisco, CA 94158, USA."
},
{
"name": "Department of Bioengineering and Therapeutic Sciences, University of California, San Francisco, CA 94158, USA."
},
{
"name": "The University of California, Berkeley–University of California, San Francisco Graduate Program in Bioengineering, University of California, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Kortemme",
"given": "Tanja",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-7173-3741",
"affiliation": [
{
"name": "Quantitative Biosciences Institute (QBI) COVID-19 Research Group (QCRG), San Francisco, CA 94158, USA."
},
{
"name": "QBI, University of California, San Francisco, CA 94158, USA."
},
{
"name": "QBI Coronavirus Research Group Structural Biology Consortium, University of California, San Francisco, CA 94158, USA."
},
{
"name": "Department of Pharmaceutical Chemistry, University of California, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Manglik",
"given": "Aashish",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Quantitative Biosciences Institute (QBI) COVID-19 Research Group (QCRG), San Francisco, CA 94158, USA."
},
{
"name": "QBI Coronavirus Research Group Structural Biology Consortium, University of California, San Francisco, CA 94158, USA."
},
{
"name": "Department of Biochemistry and Biophysics, University of California, San Francisco, CA 94158, USA."
}
],
"family": "Southworth",
"given": "Daniel R.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-2083-5665",
"affiliation": [
{
"name": "Quantitative Biosciences Institute (QBI) COVID-19 Research Group (QCRG), San Francisco, CA 94158, USA."
},
{
"name": "QBI, University of California, San Francisco, CA 94158, USA."
},
{
"name": "QBI Coronavirus Research Group Structural Biology Consortium, University of California, San Francisco, CA 94158, USA."
},
{
"name": "Department of Biochemistry and Biophysics, University of California, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Stroud",
"given": "Robert M.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-2140-9185",
"affiliation": [
{
"name": "MRC Protein Phosphorylation and Ubiquitylation Unit, College of Life Sciences, University of Dundee, Dundee DD1 5EH, UK."
}
],
"authenticated-orcid": true,
"family": "Alessi",
"given": "Dario R.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-8022-2719",
"affiliation": [
{
"name": "MRC Protein Phosphorylation and Ubiquitylation Unit, College of Life Sciences, University of Dundee, Dundee DD1 5EH, UK."
}
],
"authenticated-orcid": true,
"family": "Davies",
"given": "Paul",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-0107-0775",
"affiliation": [
{
"name": "Department of Microbiology and Immunology, University of Maryland School of Medicine, Baltimore, MD 21201, USA."
}
],
"authenticated-orcid": true,
"family": "Frieman",
"given": "Matthew B.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-1708-8454",
"affiliation": [
{
"name": "Department of Medicine, University of California, San Diego, CA 92093, USA."
},
{
"name": "Department to Bioengineering, University of California, San Diego, CA 92093, USA."
}
],
"authenticated-orcid": true,
"family": "Ideker",
"given": "Trey",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Dipartimento di Farmacia-Scienze del Farmaco, Università degli Studi di Bari ‘ALDO MORO’, Via Orabona, 4 70125, Bari, Italy."
}
],
"family": "Abate",
"given": "Carmen",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-6103-6048",
"affiliation": [
{
"name": "Institute of Virology, Medical Center–University of Freiburg, 79104 Freiburg, Germany."
},
{
"name": "Département de Virologie, CNRS UMR 3569, Institut Pasteur, Paris 75015, France."
}
],
"authenticated-orcid": true,
"family": "Jouvenet",
"given": "Nolwenn",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-0187-559X",
"affiliation": [
{
"name": "Institute of Virology, Medical Center–University of Freiburg, 79104 Freiburg, Germany."
}
],
"authenticated-orcid": true,
"family": "Kochs",
"given": "Georg",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-6098-7367",
"affiliation": [
{
"name": "Quantitative Biosciences Institute (QBI) COVID-19 Research Group (QCRG), San Francisco, CA 94158, USA."
},
{
"name": "QBI, University of California, San Francisco, CA 94158, USA."
},
{
"name": "Department of Pharmaceutical Chemistry, University of California, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Shoichet",
"given": "Brian",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-5697-1274",
"affiliation": [
{
"name": "J. David Gladstone Institutes, San Francisco, CA 94158, USA."
},
{
"name": "Department of Medicine, University of California, San Francisco, CA 94143, USA."
}
],
"authenticated-orcid": true,
"family": "Ott",
"given": "Melanie",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-7007-4070",
"affiliation": [
{
"name": "MRC–University of Glasgow Centre for Virus Research, Glasgow G61 1QH, Scotland, UK."
}
],
"authenticated-orcid": true,
"family": "Palmarini",
"given": "Massimo",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-8590-7741",
"affiliation": [
{
"name": "Quantitative Biosciences Institute (QBI) COVID-19 Research Group (QCRG), San Francisco, CA 94158, USA."
},
{
"name": "QBI, University of California, San Francisco, CA 94158, USA."
},
{
"name": "Department of Cellular and Molecular Pharmacology, University of California, San Francisco, CA 94158, USA."
},
{
"name": "Howard Hughes Medical Institute, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Shokat",
"given": "Kevan M.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-6551-1827",
"affiliation": [
{
"name": "Department of Microbiology, Icahn School of Medicine at Mount Sinai, New York, NY 10029, USA."
},
{
"name": "Global Health and Emerging Pathogens Institute, Icahn School of Medicine at Mount Sinai, New York, NY 10029, USA."
},
{
"name": "Department of Medicine, Division of Infectious Diseases, Icahn School of Medicine at Mount Sinai, New York, NY 10029, USA."
},
{
"name": "The Tisch Cancer Institute, Icahn School of Medicine at Mount Sinai, New York, NY 10029, USA."
}
],
"authenticated-orcid": true,
"family": "García-Sastre",
"given": "Adolfo",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-4369-7381",
"affiliation": [
{
"name": "Aetion, Inc., New York, NY 10001, USA."
}
],
"authenticated-orcid": true,
"family": "Rassen",
"given": "Jeremy A.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Institute for Clinical and Experimental Pharmacology and Toxicology I, University of Freiburg, 79104 Freiburg, Germany."
},
{
"name": "Centre for Integrative Biological Signaling Studies (CIBSS), University of Freiburg, 79104 Freiburg, Germany."
}
],
"family": "Grosse",
"given": "Robert",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-5736-4388",
"affiliation": [
{
"name": "Quantitative Biosciences Institute (QBI) COVID-19 Research Group (QCRG), San Francisco, CA 94158, USA."
},
{
"name": "QBI, University of California, San Francisco, CA 94158, USA."
},
{
"name": "QBI Coronavirus Research Group Structural Biology Consortium, University of California, San Francisco, CA 94158, USA."
},
{
"name": "Chan-Zuckerberg Biohub, San Francisco, CA 94158, USA."
},
{
"name": "Department of Biochemistry and Biophysics, University of California, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Rosenberg",
"given": "Oren S.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-2238-8590",
"affiliation": [
{
"name": "Quantitative Biosciences Institute (QBI) COVID-19 Research Group (QCRG), San Francisco, CA 94158, USA."
},
{
"name": "QBI, University of California, San Francisco, CA 94158, USA."
},
{
"name": "QBI Coronavirus Research Group Structural Biology Consortium, University of California, San Francisco, CA 94158, USA."
},
{
"name": "Department of Pharmaceutical Chemistry, University of California, San Francisco, CA 94158, USA."
}
],
"authenticated-orcid": true,
"family": "Verba",
"given": "Kliment A.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-4195-425X",
"affiliation": [
{
"name": "Center for Microbial Pathogenesis, Institute for Biomedical Sciences, Georgia State University, Atlanta, GA 30303, USA."
}
],
"authenticated-orcid": true,
"family": "Basler",
"given": "Christopher F.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-4400-771X",
"affiliation": [
{
"name": "Viral Populations and Pathogenesis Unit, CNRS UMR 3569, Institut Pasteur, 75724, Paris, cedex 15, France."
}
],
"authenticated-orcid": true,
"family": "Vignuzzi",
"given": "Marco",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-0144-7712",
"affiliation": [
{
"name": "Department of Biomedical Science, Centre for Membrane Interactions and Dynamics, University of Sheffield, Firth Court, Sheffield S10 2TN, UK."
}
],
"authenticated-orcid": true,
"family": "Peden",
"given": "Andrew A.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-2724-7703",
"affiliation": [
{
"name": "European Molecular Biology Laboratory, European Bioinformatics Institute (EMBL-EBI), Wellcome Genome Campus, Hinxton, Cambridgeshire CB10 1SD, UK."
}
],
"authenticated-orcid": true,
"family": "Beltrao",
"given": "Pedro",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-4902-337X",
"affiliation": [
{
"name": "Quantitative Biosciences Institute (QBI) COVID-19 Research Group (QCRG), San Francisco, CA 94158, USA."
},
{
"name": "QBI, University of California, San Francisco, CA 94158, USA."
},
{
"name": "Department of Cellular and Molecular Pharmacology, University of California, San Francisco, CA 94158, USA."
},
{
"name": "J. David Gladstone Institutes, San Francisco, CA 94158, USA."
},
{
"name": "Department of Microbiology, Icahn School of Medicine at Mount Sinai, New York, NY 10029, USA."
}
],
"authenticated-orcid": true,
"family": "Krogan",
"given": "Nevan J.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Owens",
"given": "Tristan W.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Gupta",
"given": "Meghna",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Pourmal",
"given": "Sergei",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Titus",
"given": "Erron W.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Azumaya",
"given": "Caleigh M.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Billesbølle",
"given": "Christian",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Brilot",
"given": "Axel F.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Campbell",
"given": "Melody G.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Diallo",
"given": "Amy",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Dickinson",
"given": "Miles Sasha",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Diwanji",
"given": "Devan",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Herrera",
"given": "Nadia",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Hoppe",
"given": "Nick",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Kratochvil",
"given": "Huong T.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Liu",
"given": "Yanxin",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Merz",
"given": "Gregory E.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Moritz",
"given": "Michelle",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Nguyen",
"given": "Henry C.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Nowotny",
"given": "Carlos",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Puchades",
"given": "Cristina",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Rizo",
"given": "Alexandrea N.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Schulze-Gahmen",
"given": "Ursula",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Smith",
"given": "Amber M.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Sun",
"given": "Ming",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Young",
"given": "Iris D.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Zhao",
"given": "Jianhua",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Asarnow",
"given": "Daniel",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Biel",
"given": "Justin",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Bowen",
"given": "Alisa",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Braxton",
"given": "Julian R.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Chen",
"given": "Jen",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Chio",
"given": "Cynthia M.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Chio",
"given": "Un Seng",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Deshpande",
"given": "Ishan",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Doan",
"given": "Loan",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Faust",
"given": "Bryan",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Flores",
"given": "Sebastian",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Jin",
"given": "Mingliang",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Kim",
"given": "Kate",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Lam",
"given": "Victor L.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Li",
"given": "Fei",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Li",
"given": "Junrui",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Li",
"given": "Yen-Li",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Li",
"given": "Yang",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Liu",
"given": "Xi",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Lo",
"given": "Megan",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Lopez",
"given": "Kyle E.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Melo",
"given": "Arthur A.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Moss",
"given": "Frank R.",
"sequence": "additional",
"suffix": "III"
},
{
"affiliation": [],
"family": "Nguyen",
"given": "Phuong",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Paulino",
"given": "Joana",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Pawar",
"given": "Komal Ishwar",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Peters",
"given": "Jessica K.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Pospiech",
"given": "Thomas H.",
"sequence": "additional",
"suffix": "Jr."
},
{
"affiliation": [],
"family": "Safari",
"given": "Maliheh",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Sangwan",
"given": "Smriti",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Schaefer",
"given": "Kaitlin",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Thomas",
"given": "Paul V.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Thwin",
"given": "Aye C.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Trenker",
"given": "Raphael",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Tse",
"given": "Eric",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Tsui",
"given": "Tsz Kin Martin",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Wang",
"given": "Feng",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Whitis",
"given": "Natalie",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Yu",
"given": "Zanlin",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Zhang",
"given": "Kaihua",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Zhang",
"given": "Yang",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Zhou",
"given": "Fengbo",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Trinidad",
"given": "Donovan",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Agard",
"given": "David A.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Cheng",
"given": "Yifan",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Fraser",
"given": "James S.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Frost",
"given": "Adam",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Jura",
"given": "Natalia",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Kortemme",
"given": "Tanja",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Manglik",
"given": "Aashish",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Southworth",
"given": "Daniel R.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Stroud",
"given": "Robert M.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Rosenberg",
"given": "Oren S.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Verba",
"given": "Kliment A.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Damas",
"given": "Joana",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Hughes",
"given": "Graham M.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Keough",
"given": "Kathleen C.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Painter",
"given": "Corrie A.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Persky",
"given": "Nicole S.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Corbo",
"given": "Marco",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Kirilenko",
"given": "Bodgan",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Hiller",
"given": "Michael",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Koepfli",
"given": "Klaus-Peter",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Kaplow",
"given": "Irene",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Wirthlin",
"given": "Morgan",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Pfenning",
"given": "Andreas R.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Zhao",
"given": "Huabin",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Genereux",
"given": "Diane P.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Swofford",
"given": "Ross",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Lind",
"given": "Abigail",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Pollard",
"given": "Katherine S.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ryderq",
"given": "Oliver A.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Nweeia",
"given": "Martin T.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Meadows",
"given": "Jennifer",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Dong",
"given": "Michael",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Wallerman",
"given": "Ola",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Marinescu",
"given": "Vikki",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Lindblad-Toh",
"given": "Kerstin",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ray",
"given": "David A.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Power",
"given": "Sarahjane",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Teeling",
"given": "Emma C.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Chauhan",
"given": "Gaurav",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Li",
"given": "Shirley Xue",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Karlsson",
"given": "Elinor K.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Lewin",
"given": "Harris A.",
"sequence": "additional"
},
{
"affiliation": [],
"name": "QCRG Structural Biology Consortium",
"sequence": "additional"
},
{
"affiliation": [],
"name": "Zoonomia Consortium",
"sequence": "additional"
}
],
"container-title": [
"Science"
],
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2020,
10,
15
]
],
"date-time": "2020-10-15T19:17:28Z",
"timestamp": 1602789448000
},
"deposited": {
"date-parts": [
[
2022,
1,
13
]
],
"date-time": "2022-01-13T16:47:24Z",
"timestamp": 1642092444000
},
"funder": [
{
"DOI": "10.13039/100000001",
"award": [
"1650113"
],
"doi-asserted-by": "publisher",
"name": "National Science Foundation"
},
{
"DOI": "10.13039/100000002",
"award": [
"P01AI063302, P50AI150476, R01AI120694, R01AI122747, R01AI143292, U19AI135972, U19AI135990"
],
"doi-asserted-by": "publisher",
"name": "National Institutes of Health"
},
{
"DOI": "10.13039/100000002",
"award": [
"P01AI120943, R01AI143292"
],
"doi-asserted-by": "publisher",
"name": "National Institutes of Health"
},
{
"DOI": "10.13039/100000002",
"award": [
"U19AI135990"
],
"doi-asserted-by": "publisher",
"name": "National Institutes of Health"
},
{
"DOI": "10.13039/100000002",
"award": [
"R35GM122481"
],
"doi-asserted-by": "publisher",
"name": "National Institutes of Health"
},
{
"DOI": "10.13039/100000002",
"award": [
"U19AI135972"
],
"doi-asserted-by": "publisher",
"name": "National Institutes of Health"
},
{
"DOI": "10.13039/100000060",
"award": [
"R01AI128214"
],
"doi-asserted-by": "publisher",
"name": "National Institute of Allergy and Infectious Diseases"
},
{
"DOI": "10.13039/100000051",
"award": [
"R01 HG009979"
],
"doi-asserted-by": "publisher",
"name": "National Human Genome Research Institute"
},
{
"DOI": "10.13039/100000002",
"award": [
"K99GM138753"
],
"doi-asserted-by": "publisher",
"name": "National Institutes of Health"
},
{
"DOI": "10.13039/100000011",
"award": [
"None"
],
"doi-asserted-by": "publisher",
"name": "Howard Hughes Medical Institute"
},
{
"DOI": "10.13039/100000002",
"award": [
"T32GM007618"
],
"doi-asserted-by": "publisher",
"name": "National Institutes of Health"
},
{
"DOI": "10.13039/100000052",
"award": [
"AI150476"
],
"doi-asserted-by": "publisher",
"name": "NIH Office of the Director"
},
{
"DOI": "10.13039/100000005",
"award": [
"W81XWH-20-1-0270"
],
"doi-asserted-by": "publisher",
"name": "U.S. Department of Defense"
},
{
"DOI": "10.13039/100000057",
"award": [
"F32GM137463"
],
"doi-asserted-by": "publisher",
"name": "National Institute of General Medical Sciences"
},
{
"DOI": "10.13039/100000002",
"award": [
"F32CA239333"
],
"doi-asserted-by": "publisher",
"name": "National Institutes of Health"
},
{
"DOI": "10.13039/100000002",
"award": [
"F32 CA239336"
],
"doi-asserted-by": "publisher",
"name": "National Institutes of Health"
},
{
"DOI": "10.13039/100000002",
"award": [
"T32GM007618"
],
"doi-asserted-by": "publisher",
"name": "National Institutes of Health"
},
{
"DOI": "10.13039/100000002",
"award": [
"F30AI143401"
],
"doi-asserted-by": "publisher",
"name": "National Institutes of Health"
},
{
"DOI": "10.13039/100014989",
"doi-asserted-by": "publisher",
"name": "Chan Zuckerberg Initiative"
},
{
"DOI": "10.13039/100013349",
"doi-asserted-by": "publisher",
"name": "LABoratoires d’EXcellence ARCANE"
},
{
"DOI": "10.13039/100012399",
"award": [
"ASPR-20-01495"
],
"doi-asserted-by": "publisher",
"name": "Biomedical Advanced Research and Development Authority"
},
{
"DOI": "10.13039/100000865",
"award": [
"INV-006099"
],
"doi-asserted-by": "publisher",
"name": "Bill and Melinda Gates Foundation"
},
{
"DOI": "10.13039/100000185",
"award": [
"HR0011-20-2-0040"
],
"doi-asserted-by": "publisher",
"name": "Defense Advanced Research Projects Agency"
},
{
"DOI": "10.13039/100006502",
"award": [
"HR0011-19-2-0020"
],
"doi-asserted-by": "publisher",
"name": "Defense Sciences Office, DARPA"
},
{
"DOI": "10.13039/100016127",
"award": [
"COVID19 grant"
],
"doi-asserted-by": "publisher",
"name": "Fast Grants"
},
{
"DOI": "10.13039/501100000265",
"award": [
"MC PC 19026"
],
"doi-asserted-by": "publisher",
"name": "Medical Research Council"
},
{
"DOI": "10.13039/100006502",
"award": [
"HR0011-19-2-0020"
],
"doi-asserted-by": "publisher",
"name": "Defense Sciences Office, DARPA"
},
{
"DOI": "10.13039/501100000265",
"award": [
"MC_UU_12016/2"
],
"doi-asserted-by": "publisher",
"name": "Medical Research Council"
},
{
"DOI": "10.13039/100006502",
"award": [
"HR0011-19-2-0020"
],
"doi-asserted-by": "publisher",
"name": "Defense Sciences Office, DARPA"
},
{
"DOI": "10.13039/100006502",
"award": [
"HR0011-19-2-0020"
],
"doi-asserted-by": "publisher",
"name": "Defense Sciences Office, DARPA"
},
{
"DOI": "10.13039/100007013",
"doi-asserted-by": "publisher",
"name": "Hoffman-La Roche"
},
{
"DOI": "10.13039/100016127",
"award": [
"COVID19 grant"
],
"doi-asserted-by": "publisher",
"name": "Fast Grants"
},
{
"DOI": "10.13039/100008072",
"doi-asserted-by": "publisher",
"name": "Gladstone Institutes"
},
{
"DOI": "10.13039/100009724",
"doi-asserted-by": "publisher",
"name": "Roddenberry Foundation"
},
{
"DOI": "10.13039/100006502",
"award": [
"HR0011-19-2-0020"
],
"doi-asserted-by": "publisher",
"name": "Defense Sciences Office, DARPA"
},
{
"DOI": "10.13039/100000065",
"award": [
"R01 NS089713"
],
"doi-asserted-by": "publisher",
"name": "National Institute of Neurological Disorders and Stroke"
},
{
"DOI": "10.13039/100014895",
"doi-asserted-by": "publisher",
"name": "Open Philanthropy Project"
},
{
"DOI": "10.13039/100007457",
"doi-asserted-by": "publisher",
"name": "JPB Foundation"
},
{
"DOI": "10.13039/100000060",
"award": [
"HHSN272201400008C"
],
"doi-asserted-by": "publisher",
"name": "National Institute of Allergy and Infectious Diseases"
},
{
"DOI": "10.13039/100006502",
"award": [
"HR0011-19-2-0020"
],
"doi-asserted-by": "publisher",
"name": "Defense Sciences Office, DARPA"
},
{
"DOI": "10.13039/100001021",
"award": [
"DRG-2402-20"
],
"doi-asserted-by": "publisher",
"name": "Damon Runyon Cancer Research Foundation"
},
{
"DOI": "10.13039/100000861",
"award": [
"1019894"
],
"doi-asserted-by": "publisher",
"name": "Burroughs Wellcome Fund"
},
{
"award": [
"Excellence in Research Award COVID19"
],
"name": "Laboratory for Genomics Research"
},
{
"name": "URGENCE COVID-19 Institut Pasteur fundraising campaign"
},
{
"award": [
"COVID19 grant"
],
"name": "FastGrants"
},
{
"name": "The Augusta University-Georgia State University Seed Grant"
},
{
"DOI": "10.13039/501100000265",
"award": [
"MC_UU_12016/2"
],
"doi-asserted-by": "publisher",
"name": "Medical Research Council"
},
{
"name": "Vir Biotechnology"
},
{
"name": "The Ron Conway Family"
},
{
"award": [
"Excellence in Research Award, 133122P"
],
"name": "The Laboratory for Genomics Research"
},
{
"award": [
"EXC-2189, project ID 390939984"
],
"name": "DFG under Germany’s Excellence Strategy"
},
{
"award": [
"None"
],
"name": "Chan Zuckerberg Biohub"
},
{
"DOI": "10.13039/100000057",
"award": [
"R01 GM24485"
],
"doi-asserted-by": "crossref",
"name": "NIGMS"
},
{
"award": [
"Excellence in Research Award"
],
"name": "Laboratory for Genomics Research"
},
{
"name": "URGENCE COVID-19 Institut Pasteur fundraising campaign"
},
{
"DOI": "10.13039/501100000268",
"award": [
"BB/S009566/1, BB/L002841/1"
],
"doi-asserted-by": "crossref",
"name": "BBSRC"
},
{
"DOI": "10.13039/501100000268",
"award": [
"BB/S009566/1, BB/L002841/1"
],
"doi-asserted-by": "crossref",
"name": "BBSRC"
},
{
"DOI": "10.13039/501100000268",
"award": [
"BB/J014443/1"
],
"doi-asserted-by": "publisher",
"name": "Biotechnology and Biological Sciences Research Council"
},
{
"award": [
"Excellence in Research Award, 133122P"
],
"name": "The Laboratory for Genomics Research"
}
],
"indexed": {
"date-parts": [
[
2022,
9,
15
]
],
"date-time": "2022-09-15T08:27:16Z",
"timestamp": 1663230436720
},
"is-referenced-by-count": 307,
"issn-type": [
{
"type": "print",
"value": "0036-8075"
},
{
"type": "electronic",
"value": "1095-9203"
}
],
"issue": "6521",
"issued": {
"date-parts": [
[
2020,
12,
4
]
]
},
"journal-issue": {
"issue": "6521",
"published-print": {
"date-parts": [
[
2020,
12,
4
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2020,
12,
4
]
],
"date-time": "2020-12-04T00:00:00Z",
"timestamp": 1607040000000
}
}
],
"link": [
{
"URL": "https://syndication.highwire.org/content/doi/10.1126/science.abe9403",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "syndication"
},
{
"URL": "https://syndication.highwire.org/content/doi/10.1126/science.abe9403",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "221",
"original-title": [],
"prefix": "10.1126",
"published": {
"date-parts": [
[
2020,
12,
4
]
]
},
"published-print": {
"date-parts": [
[
2020,
12,
4
]
]
},
"publisher": "American Association for the Advancement of Science (AAAS)",
"reference": [
{
"DOI": "10.1016/j.ijsu.2020.07.032",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_2_2"
},
{
"DOI": "10.1056/NEJMoa2007764",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_3_2"
},
{
"DOI": "10.1056/nejmoa2021436",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_4_2"
},
{
"DOI": "10.1111/ijcp.13525",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_5_2"
},
{
"DOI": "10.1038/s41586-020-2286-9",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_6_2"
},
{
"DOI": "10.1016/j.jprot.2013.10.023",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_7_2"
},
{
"DOI": "10.1038/nature10719",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_8_2"
},
{
"DOI": "10.1016/S0092-8674(02)01250-3",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_9_2"
},
{
"DOI": "10.1038/cr.2010.113",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_10_2"
},
{
"DOI": "10.1128/JVI.02959-14",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_11_2"
},
{
"DOI": "10.1080/15419060212186",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_12_2"
},
{
"DOI": "10.1016/j.tcb.2007.07.010",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_13_2"
},
{
"DOI": "10.1074/jbc.272.33.20730",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_14_2"
},
{
"DOI": "10.1006/jmbi.2000.4120",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_15_2"
},
{
"DOI": "10.1016/j.jmb.2009.03.070",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_16_2"
},
{
"DOI": "10.2210/pdb6z4u/pdb",
"doi-asserted-by": "crossref",
"key": "e_1_3_3_17_2",
"unstructured": "S. D. Weeks S. De Graef A. Munawar X-ray Crystallographic Structure of Orf9b from SARS-CoV-2 (2020); https://doi.org/10.2210/pdb6z4u/pdb.10.2210/pdb6z4u/pdb"
},
{
"DOI": "10.1016/j.cell.2020.06.034",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_18_2"
},
{
"DOI": "10.1074/jbc.M109.023986",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_19_2"
},
{
"DOI": "10.1038/cr.2010.103",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_20_2"
},
{
"DOI": "10.1093/nsr/nwaa037",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_21_2"
},
{
"DOI": "10.1016/S0140-6736(20)30183-5",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_22_2"
},
{
"DOI": "10.1093/cid/ciaa248",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_23_2"
},
{
"DOI": "10.1172/JCI137244",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_24_2"
},
{
"DOI": "10.1016/j.chembiol.2012.11.012",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_25_2"
},
{
"DOI": "10.1016/j.cyto.2013.09.012",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_26_2"
},
{
"DOI": "10.1016/j.cytogfr.2020.04.003",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_27_2"
},
{
"DOI": "10.3390/ijms20153677",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_28_2"
},
{
"DOI": "10.1038/s41586-018-0175-2",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_29_2"
},
{
"DOI": "10.1038/s41467-017-02317-2",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_30_2"
},
{
"DOI": "10.1038/s41431-020-0636-6",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_31_2"
},
{
"DOI": "10.1016/S0140-6736(20)31757-8",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_32_2"
},
{
"article-title": "Indomethacin has a potent antiviral activity against SARS coronavirus",
"author": "Amici C.",
"first-page": "1021",
"journal-title": "Antivir. Ther.",
"key": "e_1_3_3_33_2",
"unstructured": "C. Amici, A. Di Caro, A. Ciucci, L. Chiappa, C. Castilletti, V. Martella, N. Decaro, C. Buonavoglia, M. R. Capobianchi, M. G. Santoro, Indomethacin has a potent antiviral activity against SARS coronavirus. Antivir. Ther. 11, 1021–1030 (2006). 17302372",
"volume": "11",
"year": "2006"
},
{
"DOI": "10.1093/biomet/70.1.41",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_34_2"
},
{
"DOI": "10.2174/1871524910909030246",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_35_2"
},
{
"key": "e_1_3_3_36_2",
"unstructured": "R. A. Glennon Sigma receptor ligands and the use thereof U.S. Patent 6 057 371 (2000); https://patentimages.storage.googleapis.com/dc/36/68/73f4ccdac4c973/US6057371.pdf."
},
{
"DOI": "10.1016/S0014-2999(00)00430-1",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_37_2"
},
{
"DOI": "10.1002/14651858.CD009831.pub2",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_38_2"
},
{
"DOI": "10.1124/mol.54.3.591",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_39_2"
},
{
"DOI": "10.1073/pnas.1204524109",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_40_2"
},
{
"DOI": "10.1038/s41586-018-0360-3",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_41_2"
},
{
"DOI": "10.1038/sj.bjp.0701079",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_42_2"
},
{
"DOI": "10.1038/s41423-020-0514-8",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_43_2"
},
{
"DOI": "10.1093/bioinformatics/btx431",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_44_2"
},
{
"DOI": "10.1371/journal.pone.0189209",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_45_2"
},
{
"DOI": "10.1038/nbt.1511",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_46_2"
},
{
"DOI": "10.1093/nar/gky973",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_47_2"
},
{
"DOI": "10.1016/j.cell.2015.06.043",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_48_2"
},
{
"DOI": "10.1089/omi.2011.0118",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_49_2"
},
{
"DOI": "10.1038/nmeth.1818",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_50_2"
},
{
"DOI": "10.1073/pnas.1914677117",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_51_2"
},
{
"DOI": "10.1038/nsmb999",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_52_2"
},
{
"DOI": "10.1093/nar/gky427",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_53_2"
},
{
"DOI": "10.1101/2020.09.07.285569",
"doi-asserted-by": "crossref",
"key": "e_1_3_3_54_2",
"unstructured": "J. Durairaj M. Akdel D. de Ridder A. D. J. van Dijk Geometricus Represents Protein Structures as Shape-mers Derived from Moment Invariants. bioRxiv 2020.09.07.285569 [Preprint]. 8 September 2020. .10.1101/2020.09.07.285569"
},
{
"DOI": "10.1016/j.csbj.2020.03.011",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_55_2"
},
{
"DOI": "10.1101/gr.1239303",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_56_2"
},
{
"DOI": "10.1007/978-1-4939-6783-4_13",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_57_2"
},
{
"DOI": "10.1093/clinchem/hvaa029",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_58_2"
},
{
"DOI": "10.1006/meth.2001.1262",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_59_2"
},
{
"key": "e_1_3_3_60_2",
"unstructured": "R. Stoner T. Maures D. Conant Methods and systems for guide RNA design and use U.S. Patent 2019/0382797 A1 (2019); https://patentimages.storage.googleapis.com/95/c7/43/3d48387ce0f116/US20190382797A1.pdf."
},
{
"DOI": "10.1101/251082",
"doi-asserted-by": "crossref",
"key": "e_1_3_3_61_2",
"unstructured": "T. Hsiau D. Conant N. Rossi T. Maures K. Waite J. Yang S. Joshi R. Kelso K. Holden B. L. Enzmann R. Stoner Inference of CRISPR Edits from Sanger Trace Data. bioRxiv 251082 [Preprint]. 10 August 2018. .10.1101/251082"
},
{
"DOI": "10.3390/v12060622",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_62_2"
},
{
"DOI": "10.1074/jbc.M605250200",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_63_2"
},
{
"DOI": "10.1083/jcb.201708044",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_64_2"
},
{
"DOI": "10.26508/lsa.201900429",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_65_2"
},
{
"DOI": "10.1074/mcp.M114.043083",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_66_2"
},
{
"DOI": "10.1093/nar/gkv332",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_67_2"
},
{
"DOI": "10.1016/j.jsb.2005.07.007",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_68_2"
},
{
"DOI": "10.1038/nmeth.4193",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_69_2"
},
{
"DOI": "10.1093/nar/25.17.3389",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_70_2"
},
{
"DOI": "10.1107/S0907444904019158",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_71_2"
},
{
"DOI": "10.7554/eLife.17219",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_72_2"
},
{
"DOI": "10.1107/S2052252519007619",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_73_2"
},
{
"DOI": "10.1107/S2059798318002425",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_74_2"
},
{
"DOI": "10.1002/pro.3235",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_75_2"
},
{
"DOI": "10.1107/S2059798318009324",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_76_2"
},
{
"DOI": "10.1016/j.jmb.2007.05.022",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_77_2"
},
{
"DOI": "10.20944/preprints202005.0264.v1",
"doi-asserted-by": "crossref",
"key": "e_1_3_3_78_2",
"unstructured": "A. N. Honko N. Storm D. J. Bean J. H. Vasquez S. N. Downs A. Griffiths Rapid Quantification and Neutralization Assays for Novel Coronavirus SARS-CoV-2 Using Avicel RC-591 Semi-Solid Overlay. Preprints 2020050264 [Preprint]. 16 May 2020. www.preprints.org/manuscript/202005.0264/v1."
},
{
"DOI": "10.1006/jmbi.1993.1626",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_79_2"
},
{
"DOI": "10.1016/j.jmb.2005.03.035",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_80_2"
},
{
"DOI": "10.1126/science.abc1560",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_81_2"
},
{
"DOI": "10.1038/nprot.2016.169",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_82_2"
},
{
"DOI": "10.1093/bioinformatics/btu097",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_83_2"
},
{
"DOI": "10.1038/s41596-020-0312-x",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_84_2"
},
{
"DOI": "10.1093/nar/gkl206",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_85_2"
},
{
"DOI": "10.1093/bioinformatics/btt038",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_86_2"
},
{
"DOI": "10.1093/nar/gki481",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_87_2"
},
{
"DOI": "10.1093/bioinformatics/btt560",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_88_2"
},
{
"DOI": "10.1101/730531",
"doi-asserted-by": "crossref",
"key": "e_1_3_3_89_2",
"unstructured": "J. Armstrong G. Hickey M. Diekhans A. Deran Q. Fang D. Xie S. Feng J. Stiller D. Genereux J. Johnson V. D. Marinescu D. Haussler J. Alföldi K. Lindblad-Toh E. Karlsson E. D. Jarvis G. Zhang B. Paten Progressive alignment with Cactus: A multiple-genome aligner for the thousand-genome era. bioRxiv 730531 [Preprint]. 15 October 2019. https://doi.org/10.1101/730531.10.1101/730531"
},
{
"DOI": "10.1101/gr.123356.111",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_90_2"
},
{
"DOI": "10.1093/molbev/msv022",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_91_2"
},
{
"DOI": "10.1093/bioinformatics/bti079",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_92_2"
},
{
"DOI": "10.1101/gr.097857.109",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_93_2"
},
{
"DOI": "10.1093/bib/bbq072",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_94_2"
},
{
"DOI": "10.1093/bioinformatics/bty966",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_95_2"
},
{
"DOI": "10.1093/aje/kwg231",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_96_2"
},
{
"DOI": "10.1002/pds.1926",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_97_2"
},
{
"DOI": "10.1097/01.mlr.0000182534.19832.83",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_98_2"
},
{
"DOI": "10.1002/sim.3697",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_99_2"
},
{
"key": "e_1_3_3_100_2",
"unstructured": "World Health Organization (WHO) WHO R&D Blueprint novel Coronavirus: COVID-19 Therapeutic Trial Synopsis (WHO 2020); www.who.int/blueprint/priority-diseases/key-action/COVID-19_Treatment_Trial_Design_Master_Protocol_synopsis_Final_18022020.pdf."
},
{
"DOI": "10.1093/nar/gky1106",
"doi-asserted-by": "publisher",
"key": "e_1_3_3_101_2"
},
{
"DOI": "10.2210/pdb3fp2/pdb",
"doi-asserted-by": "crossref",
"key": "e_1_3_3_102_2",
"unstructured": "J. Li X. Qian J. Hu B. Sha Crystal structure of Tom71 complexed with Hsp82 C-terminal fragment (2009); https://doi.org/10.2210/pdb3fp2/pdb.10.2210/pdb3fp2/pdb"
}
],
"reference-count": 101,
"references-count": 101,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.science.org/doi/10.1126/science.abe9403"
}
},
"score": 1,
"short-container-title": [
"Science"
],
"short-title": [],
"source": "Crossref",
"subject": [
"Multidisciplinary"
],
"subtitle": [],
"title": [
"Comparative host-coronavirus protein interaction networks reveal pan-viral disease mechanisms"
],
"type": "journal-article",
"volume": "370"
}