Vitamin D Level in Laboratory Confirmed COVID-19 and Disease Progression
et al., The Eurasian Journal of Medicine, doi:10.5152/eurasianjmed.2022.21088, Aug 2022
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 136 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Analysis of 831 hospitalized patients in Iran, showing higher mortality with severe vitamin D deficiency, without statistical significance.
This is the 144th of 228 COVID-19 sufficiency studies for vitamin D, which collectively show higher levels reduce risk with p<0.0000000001.
|
risk of death, 33.1% lower, RR 0.67, p = 0.29, high D levels (≥10ng/mL) 49 of 376 (13.0%), low D levels (<10ng/mL) 8 of 46 (17.4%), NNT 23, adjusted per study, inverted to make RR<1 favor high D levels (≥10ng/mL), odds ratio converted to relative risk, sufficiency vs. severe deficiency, multivariable.
|
|
risk of death, 15.7% lower, RR 0.84, p = 0.44, high D levels (≥20ng/mL) 49 of 376 (13.0%), low D levels (<20ng/mL) 30 of 197 (15.2%), NNT 46, adjusted per study, inverted to make RR<1 favor high D levels (≥20ng/mL), odds ratio converted to relative risk, sufficiency vs. deficiency, multivariable.
|
|
risk of severe case, no change, RR 1.00, p = 1.00, high D levels (≥10ng/mL) 59 of 376 (15.7%), low D levels (<10ng/mL) 7 of 46 (15.2%), adjusted per study, inverted to make RR<1 favor high D levels (≥10ng/mL), odds ratio converted to relative risk, sufficiency vs. severe deficiency, multivariable.
|
|
risk of severe case, 11.6% lower, RR 0.88, p = 0.45, high D levels (≥20ng/mL) 59 of 376 (15.7%), low D levels (<20ng/mL) 35 of 197 (17.8%), NNT 48, adjusted per study, inverted to make RR<1 favor high D levels (≥20ng/mL), odds ratio converted to relative risk, sufficiency vs. deficiency, multivariable.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Dana et al., 11 Aug 2022, retrospective, Iran, peer-reviewed, 16 authors, study period March 2020 - November 2020.
Contact: sh_haghjoo@med.mui.ac.ir.
Vitamin D Level in Laboratory Confirmed COVID-19 and Disease Progression
The Eurasian Journal of Medicine, doi:10.5152/eurasianjmed.2022.21088
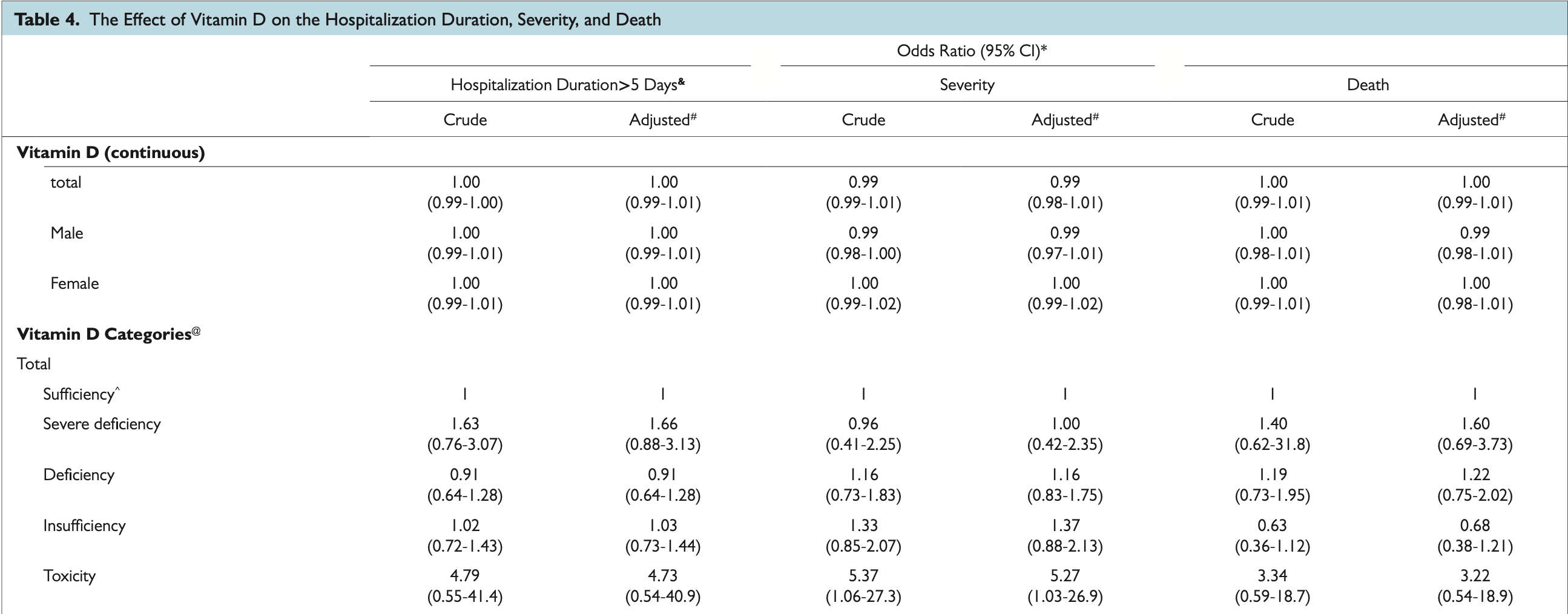
Objective: There is no conclusive evidence to suggest vitamin D level can prevent or treat infection with the new coronavirus disease 2019. This study aimed to investigate the effects of serum level of vitamin D in patients with coronavirus disease 2019 on death, severity, and hospitalization duration. Materials and Methods: Baseline characteristic of patients was extracted from the Isfahan coronavirus disease 2019 registry database (I-CORE). Blood samples were taken from all patients to measure the level of vitamin D (25-hydroxyvitamin D) and categorized. The effect of 25(OH) D on death, severity, and hospitalization duration was analyzed by logistic regression. Results: Among our study patients, 5.5% had a severe deficiency of vitamin D, 23.7% deficiency, and 24.8% insufficiency. Of the 107 patients who died, 7.5% were severely deficient in vitamin D. We found that vitamin D deficiency had no significant effect on death, disease severity, and hospitalization (P > .05). However, having at least one comorbidity increased the odds of death five times after adjusting age > 60 years and gender (P < .0001). The results showed that among all comorbidities, diabetes has the greatest impact on the outcomes as it raised the odds of death, disease severity, and length of hospital stay by 2.23,1.72, and 1.48, respectively, after controlling the age > 60 and gender (P = .0002, P = .08, P = .012).
Conclusions: The mortality, disease severity, and hospitalization of coronavirus disease 2019 patients seem to be not affected by the low levels of 25(OH)D. However, the synergy between vitamin D levels and comorbidities, age, and gender could affect the outcome of coronavirus disease 2019 patients.
@ Severe deficiency (0-10), Deficiency (1-20), Insufficiency (20-30), Sufficiency (30-100), Toxicity (upper than 100). ^Sufficiency category with the highest case number was considered as reference group. & Days between admission to discharge (just for alive patients; n = 724). # Adjusted for have at least one underlying disease. *Estimated crude or adjusted odds ratio using binary logistic regression was significant if P value <.05.
References
Abrishami, Dalili, Torbati, Possible association of vitamin D status with lung involvement and outcome in patients with COVID-19: a retrospective study, Eur J Nutr, doi:10.1007/s00394-020-02411-0
Ali, Role of vitamin D in preventing of COVID-19 infection, progression and severity, J Infect Public Health, doi:10.1016/j.jiph.2020.06.021
Angelidi, Belanger, Lorinsky, Vitamin D status is associated With in-hospital mortality and mechanical ventilation: a cohort of COVID-19 hospitalized patients, Mayo Clin Proc, doi:10.1016/j.mayocp.2021.01.001
Biesalski, Vitamin D deficiency and co-morbidities in COVID-19 patients -A fatal relationship?, NFS J, doi:10.3390/nu12092757
Carpagnano, Lecce, Quaranta, Vitamin D deficiency as a predictor of poor prognosis in patients with acute respiratory failure due to COVID-19, J Endocrinol Invest, doi:10.1007/s40618-020-01370-x
Cereda, Bogliolo, Klersy, Vitamin D 25OH deficiency in COVID-19 patients admitted to a tertiary referral hospital, Clin Nutr, doi:10.1016/j.clnu.2020.10.055
Cheng, Wang, Wang, Organ-protective effect of angiotensin-converting enzyme 2 and its effect on the prognosis of COVID-19, J Med Virol, doi:10.1002/jmv.25785
Daneshkhah, Agrawal, Eshein, Subramanian, Roy et al., Evidence for possible association of vitamin D status with cytokine storm and unregulated inflammation in COVID-19 patients, Aging Clin Exp Res, doi:10.1007/s40520-020-01677-y
Ebadi, Montano-Loza, Perspective: improving vitamin D status in the management of COVID-19, Eur J Clin Nutr, doi:10.1038/s41430-020-0661-0
Gatera, Abdulah, Musfiroh, Judistiani, Setiabudiawan, Updates on the status of vitamin D as a risk factor for respiratory distress syndrome, Adv Pharmacol Sci, doi:10.1155/2018/8494816
Gaudio, Murabito, Agodi, Montineri, Castellino et al., Vitamin D levels are reduced at the time of hospital admission in Sicilian SARS-CoV-2-Positive patients, Int J Environ Res Public Health
Gois, Ferreira, Olenski, Seguro, Vitamin D and infectious diseases: simple bystander or contributing factor?, Nutrients
Greiller, Martineau, Modulation of the immune response to respiratory viruses by vitamin D, Nutrients
Ha, Gu, Hou, Incidence, clinical characteristics and prognostic factor of patients with COVID-19: a systematic review and meta-analysis, medRxiv, doi:10.3389/fendo.2020.567824
Hastie, Pell, Sattar, Vitamin D and COVID-19 infection and mortality in UK Biobank, Eur J Nutr
Holick, Binkley, Bischoff-Ferrari, Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline, J Clin Endocrinol Metab, doi:10.1210/jc.2011-0385
Im, Je, Baek, Chung, Kwon et al., Nutritional status of patients with COVID-19, Int J Infect Dis, doi:10.1016/j.ijid.2020.08.018
Javanmard, Nasirian, Ataei, Vaseghi, Vaezi et al., Isfahan COvid-19 REgistry (I-CORE): design and methodology, J Res Med Sci, doi:10.4103/jrms.JRMS_271_20
Katz, Yue, Xue, Increased risk for COVID-19 in patients with vitamin D deficiency, Nutrition, doi:10.1016/j.nut.2020.111106
Khan, Nasir, Nasir, Maha, Rehman, Vitamin D and COVID-19: is there a role? J Diabetes, Metab Disord, doi:10.1007/s40200-021-00775-6
Lim, Pranata, Huang, Yonas, Soeroto et al., Multiorgan failure With emphasis on acute kidney injury and severity of COVID-19: systematic review and meta-analysis, Can J Kidney Health Dis, doi:10.1177/2054358120938573
Luo, Liao, Shen, Li, Cheng, chinese people (corrected)
Lélu, Laffont, Delpy, Estrogen receptor α signaling in T lymphocytes is required for estradiol-mediated inhibition of Th1 and Th17 cell differentiation and protection against experimental autoimmune encephalomyelitis, J Immunol
Martineau, Forouhi, Vitamin D for COVID-19: a case to answer?, Lancet Diabetes Endocrinol, doi:10.1016/S2213-8587(20)30268-0
Murai, Fernandes, Sales, Effect of a single high dose of vitamin D 3 on hospital length of stay in patients With moderate to severe COVID-19, JAMA, doi:10.1001/jama.2020.26848
Pagano, Peruzzu, Ruggieri, Ortona, Gagliardi, Vitamin D and sex differences in COVID-19, Front Endocrinol
Radujkovic, Hippchen, Tiwari-Heckler, Dreher, Boxberger, Vitamin D deficiency and outcome of COVID-19 patients, Nutrients
Rehan, Torday, Peleg, 1α,25-Dihydroxy-3-epi-vitamin D3, a natural metabolite of 1α,25-dihydroxy vitamin D3: production and biological activity studies in pulmonary alveolar type II cells, Mol Genet Metab, doi:10.1016/s1096-7192(02)00022-7
Sanghera, Sapkota, Aston, Vitamin D status, gender differences, and cardiometabolic health disparities, Ann Nutr Metab
Schwalfenberg, A review of the critical role of vitamin D in the functioning of the immune system and the clinical implications of vitamin D deficiency, Mol Nutr Food Res, doi:10.1002/mnfr.201000174
Smet, Smet, Herroelen, Gryspeerdt, Martens, Serum 25(OH)D level on hospital admission associated with COVID-19 stage and mortality, Am J Clin Pathol, doi:10.1093/ajcp/aqaa252
Tehrani, Khabiri, Moradi, Mosavat, Khabiri, Evaluation of vitamin D levels in COVID-19 patients referred to Labafinejad hospital in Tehran and its relationship with disease severity and mortality, Clin Nutr ESPEN, doi:10.1016/j.clnesp.2021.01.014
Vatandost, Jahani, Afshari, Amiri, Heidarimoghadam et al., Prevalence of vitamin D deficiency in Iran: a systematic review and meta-analysis, Nutr Health, doi:10.1177/0260106018802968
Wang, Zhang, Fang, Role of vitamin D in COVID-19 infections and deaths, J Evid Based Med, doi:10.1111/jebm.12421
Xu, Yang, Chen, Luo, Zhang et al., Vitamin D alleviates lipopolysaccharide-induced acute lung injury via regulation of the reninangiotensin system, Mol Med Rep, doi:10.3892/mmr.2017.7546
DOI record:
{
"DOI": "10.5152/eurasianjmed.2022.21088",
"ISSN": [
"1308-8742"
],
"URL": "http://dx.doi.org/10.5152/eurasianjmed.2022.21088",
"author": [
{
"affiliation": [],
"family": "Dana",
"given": "Nasim",
"sequence": "first"
},
{
"affiliation": [],
"name": "Applied Physiology Research Center, Cardiovascular Research Institute, Isfahan University of Medical Sciences, Isfahan, Iran",
"sequence": "first"
},
{
"affiliation": [],
"family": "Nasirian",
"given": "Maryam",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Vaseghi",
"given": "Golnaz",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Heshmat-Ghahdarijani",
"given": "Kiyan",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ataei",
"given": "Behrooz",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Mosayebi",
"given": "Azam",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Manteghinejad",
"given": "Amirreza",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Haghjooy Javanmard",
"given": "Shaghayegh",
"sequence": "additional"
},
{
"affiliation": [],
"name": "Infectious Diseases and Tropical Medicine Research Center; and Epidemiology and Biostatistics Department, Health School, Isfahan University of Medical Sciences, Isfahan, Iran",
"sequence": "additional"
},
{
"affiliation": [],
"name": "Isfahan Cardiovascular Research Center, Cardiovascular Research Institute, Isfahan University of Medical Sciences, Isfahan, Iran",
"sequence": "additional"
},
{
"affiliation": [],
"name": "Heart Failure Research Center,Cardiovascular Research Institute, Isfahan University of Medical Sciences, Isfahan, Iran",
"sequence": "additional"
},
{
"affiliation": [],
"name": "Infectious Diseases and Tropical Medicine Research Center, Isfahan University of Medical Sciences, Isfahan, Iran",
"sequence": "additional"
},
{
"affiliation": [],
"name": "Applied Physiology Research Center, Cardiovascular Research Institute, Isfahan University of Medical Sciences, Isfahan, Iran",
"sequence": "additional"
},
{
"affiliation": [],
"name": "Cancer Prevention Research Center, Isfahan University of Medical Sciences, Omid Hospital, Isfahan, Iran",
"sequence": "additional"
},
{
"affiliation": [],
"name": "Applied Physiology Research Center, Cardiovascular Research Institute, Isfahan University of Medical Sciences, Isfahan, Iran",
"sequence": "additional"
}
],
"container-title": "The Eurasian Journal of Medicine",
"container-title-short": "Eurasian J Med",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2022,
8,
11
]
],
"date-time": "2022-08-11T08:24:03Z",
"timestamp": 1660206243000
},
"deposited": {
"date-parts": [
[
2022,
8,
11
]
],
"date-time": "2022-08-11T08:24:15Z",
"timestamp": 1660206255000
},
"indexed": {
"date-parts": [
[
2022,
8,
11
]
],
"date-time": "2022-08-11T08:42:32Z",
"timestamp": 1660207352288
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2022,
8,
11
]
]
},
"member": "3111",
"original-title": [],
"prefix": "10.5152",
"published": {
"date-parts": [
[
2022,
8,
11
]
]
},
"published-online": {
"date-parts": [
[
2022,
8,
11
]
]
},
"publisher": "AVES Publishing Co.",
"reference-count": 0,
"references-count": 0,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.eajm.org/en/vitamin-d-level-in-laboratory-confirmed-covid-19-and-disease-progression-133414"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"General Medicine"
],
"subtitle": [],
"title": "Vitamin D Level in Laboratory Confirmed COVID-19 and Disease Progression",
"type": "journal-article"
}
