Efficacy and Safety of Ivermectin and Hydroxychloroquine in Patients with Severe COVID-19: A Randomized Controlled Trial
et al., Infectious Disease Reports, doi:10.3390/idr14020020, NCT04391127, Feb 2021 (preprint)
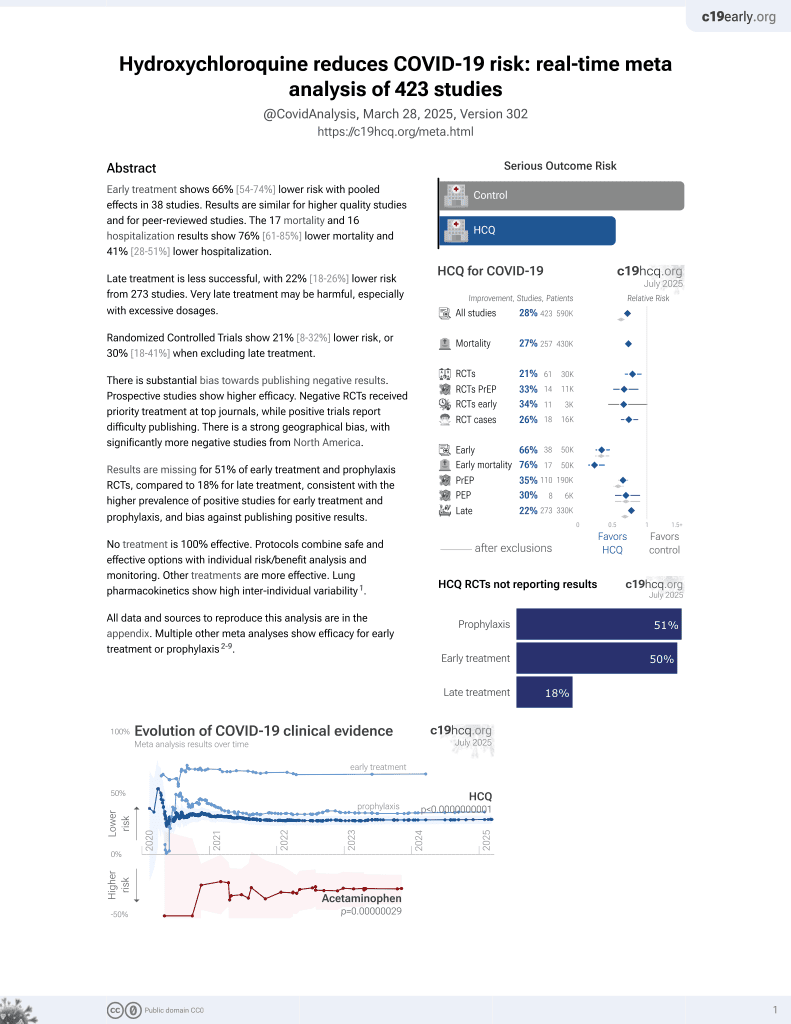
HCQ for COVID-19
1st treatment shown to reduce risk in
March 2020, now with p < 0.00000000001 from 423 studies, used in 59 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
RCT late stage severe condition (93% SOFA ≥ 2, 96% APACHE ≥ 8) high comorbidity hospitalized patients in Mexico with 33 HCQ and 37 control patients not finding significant differences. NCT04391127 (history).
Study covers HCQ and ivermectin.
|
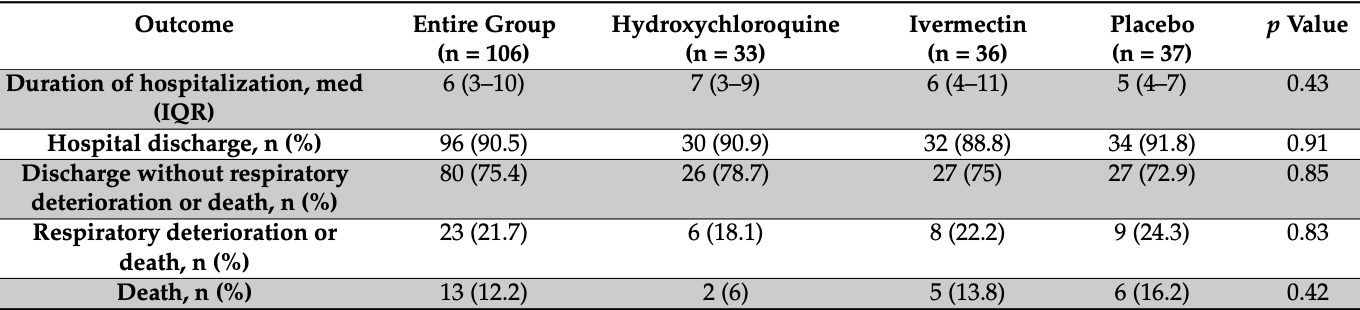
risk of death, 62.6% lower, RR 0.37, p = 0.27, treatment 2 of 33 (6.1%), control 6 of 37 (16.2%), NNT 9.8.
|
|
risk of respiratory deterioration or death, 25.3% lower, RR 0.75, p = 0.57, treatment 6 of 33 (18.2%), control 9 of 37 (24.3%), NNT 16.
|
|
risk of no hospital discharge, 12.1% higher, RR 1.12, p = 1.00, treatment 3 of 33 (9.1%), control 3 of 37 (8.1%).
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Beltran Gonzalez et al., 23 Feb 2021, Double Blind Randomized Controlled Trial, Mexico, peer-reviewed, mean age 53.8, 13 authors, study period 4 May, 2020 - 6 November, 2020, average treatment delay 7.0 days, trial NCT04391127 (history).
Efficacy and Safety of Ivermectin and Hydroxychloroquine in Patients with Severe COVID-19: A Randomized Controlled Trial
Infectious Disease Reports, doi:10.3390/idr14020020
During the first year of the COVID-19 pandemic, unauthorized drugs were widely used. Ivermectin and hydroxychloroquine are drugs that inhibit viral replication in vitro and that have been used in several medical centers. This clinical trial analyzes their efficacy in hospitalized patients with moderate COVID-19. Methods: This a controlled, clinical, randomized, double-blind trial that included hospitalized patients with COVID-19-induced pneumonia, without severe respiratory failure. Patients were randomized to one of three groups: Group 1-hydroxychloroquine, 400 mg every 12 h on the first day and, subsequently, 200 mg every 12 h for 4 days; Group 2-ivermectin, 12 mg or 18 mg, according to patient weight; and Group 3-placebo. At inclusion, blood samples for arterial blood gases and biochemical markers were obtained. The primary outcome was established as the length of stay due to patient improvement and the rate of respiratory deterioration or death. Results: During the month of August 2020, the admission of patients requiring hospitalization mostly encompassed cases with severe respiratory failure, so we ended the recruitment process and analyzed the data that was available at the time. One hundred and six (106) patients with an average age of 53 yrs (±16.9) were included, with a greater proportion of males (n = 66, 62.2%). Seventy-two percent (72%) (n = 76) had an associated comorbidity. Ninety percent (90%) of patients were discharged due to improvement (n = 96). The average duration of hospitalization was 6 days (IQR, (3) (4) (5) (6) (7) (8) (9) (10) . No difference in hospitalization duration was found between the treatment groups (Group1: 7 vs. Group 2: 6 vs. Group 3: 5, p = 0.43) nor in respiratory deterioration or death (Group 1: 18% vs. Group 2: 22.2% vs. Group 3: 24.3%, p = 0.83). Conclusions: In non-critical hospitalized patients with COVID-19 pneumonia, neither ivermectin nor hydroxychloroquine decreases the number of in-hospital days, respiratory deterioration, or deaths.
References
Boulware, Pullen, Bangdiwala, Pastick, Lofgren et al., A Randomized Trial of Hydroxychloroquine as Postexposure Prophylaxis for Covid-19, N. Engl. J. Med, doi:10.1056/NEJMoa2016638
Caly, Druce, Catton, Jans, Wagstaff, The FDA-approved drug ivermectin inhibits the replication of SARS-CoV-2 in vitro, Antiviral Res, doi:10.1016/j.antiviral.2020.104787
Cavalcanti, Zampieri, Rosa, Azevedo, Veiga et al., Hydroxychloroquine with or without Azithromycin in Mild-to-Moderate Covid-19, N. Engl. J. Med, doi:10.1056/NEJMoa2019014
De Smet, De Smet, Ryckaert, Laridon, Heremans et al., Diagnostic Performance of Chest CT for SARS-CoV-2 Infection in Individuals with or without COVID-19 Symptoms, Radiology, doi:10.1148/radiol.2020202708
Geleris, Sun, Platt, Zucker, Baldwin et al., Observational Study of Hydroxychloroquine in Hospitalized Patients with Covid-19, N. Engl. J. Med, doi:10.1056/NEJMoa2012410
Horby, Lim, Emberson, Mafham, Bell et al., Dexamethasone in Hospitalized Patients with Covid-19-Preliminary Report
Mega, Latin America's embrace of an unproven COVID treatment is hindering drug trials, Nature, doi:10.1038/d41586-020-02958-2
Momekov, Momekova, Ivermectin as a potential COVID-19 treatment from the pharmacokinetic point of view: Antiviral levels are not likely attainable with known dosing regimens, Biotechnol. Biotechnol. Equip, doi:10.1080/13102818.2020.1775118
Olson, Davis, Diagnosis and Treatment of Adults with Community-Acquired Pneumonia, JAMA, doi:10.1001/jama.2019.21118
Pan, Peto, Henao-Restrepo, Preziosi, Sathiyamoorthy et al., Repurposed Antiviral Drugs for Covid-19-Interim WHO Solidarity Trial Results, N. Engl. J. Med
Rajter, Sherman, Fatteh, Vogel, Sacks et al., Use of Ivermectin Is Associated with Lower Mortality in Hospitalized Patients with Coronavirus Disease 2019: The Ivermectin in COVID Nineteen Study, Chest, doi:10.1016/j.chest.2020.10.009
Roca, Caralt, Messika, Samper, Sztrymf et al., An Index Combining Respiratory Rate and Oxygenation to Predict Outcome of Nasal High-Flow Therapy, Am. J. Respir. Crit. Care Med, doi:10.1164/rccm.201803-0589OC
Ruiz, Jurado, Güeto, Yuste, García et al., Predictors of success of high-flow nasal cannula in the treatment of acute hypoxemic respiratory failure
Savarino, Boelaert, Cassone, Majori, Cauda, Effects of chloroquine on viral infections: An old drug against today's diseases, Lancet Infect. Dis, doi:10.1016/S1473-3099(03)00806-5
Schmith, Zhou, Lohmer, The Approved Dose of Ivermectin Alone is not the Ideal Dose for the Treatment of COVID-19, Clin. Pharmacol. Ther, doi:10.1002/cpt.1889
Zhai, Li, Chen, Gerotziafas, Zhang et al., Prevention and Treatment of Venous Thromboembolism Associated with Coronavirus Disease 2019 Infection: A Consensus Statement before Guidelines, Thromb Haemost, doi:10.1055/s-0040-1710019
DOI record:
{
"DOI": "10.3390/idr14020020",
"ISSN": [
"2036-7449"
],
"URL": "http://dx.doi.org/10.3390/idr14020020",
"abstract": "<jats:p>During the first year of the COVID-19 pandemic, unauthorized drugs were widely used. Ivermectin and hydroxychloroquine are drugs that inhibit viral replication in vitro and that have been used in several medical centers. This clinical trial analyzes their efficacy in hospitalized patients with moderate COVID-19. Methods: This a controlled, clinical, randomized, double-blind trial that included hospitalized patients with COVID-19-induced pneumonia, without severe respiratory failure. Patients were randomized to one of three groups: Group 1—hydroxychloroquine, 400 mg every 12 h on the first day and, subsequently, 200 mg every 12 h for 4 days; Group 2—ivermectin, 12 mg or 18 mg, according to patient weight; and Group 3—placebo. At inclusion, blood samples for arterial blood gases and biochemical markers were obtained. The primary outcome was established as the length of stay due to patient improvement and the rate of respiratory deterioration or death. Results: During the month of August 2020, the admission of patients requiring hospitalization mostly encompassed cases with severe respiratory failure, so we ended the recruitment process and analyzed the data that was available at the time. One hundred and six (106) patients with an average age of 53 yrs (±16.9) were included, with a greater proportion of males (n = 66, 62.2%). Seventy-two percent (72%) (n = 76) had an associated comorbidity. Ninety percent (90%) of patients were discharged due to improvement (n = 96). The average duration of hospitalization was 6 days (IQR, 3–10). No difference in hospitalization duration was found between the treatment groups (Group1: 7 vs. Group 2: 6 vs. Group 3: 5, p = 0.43) nor in respiratory deterioration or death (Group 1: 18% vs. Group 2: 22.2% vs. Group 3: 24.3%, p = 0.83). Conclusions: In non-critical hospitalized patients with COVID-19 pneumonia, neither ivermectin nor hydroxychloroquine decreases the number of in-hospital days, respiratory deterioration, or deaths.</jats:p>",
"alternative-id": [
"idr14020020"
],
"author": [
{
"affiliation": [],
"family": "Beltran Gonzalez",
"given": "Jose Lenin",
"sequence": "first"
},
{
"affiliation": [],
"family": "González Gámez",
"given": "Mario",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Mendoza Enciso",
"given": "Emanuel Antonio",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Esparza Maldonado",
"given": "Ramiro Josue",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Hernández Palacios",
"given": "Daniel",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Dueñas Campos",
"given": "Samuel",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Robles",
"given": "Itzel Ovalle",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Macías Guzmán",
"given": "Mariana Jocelyn",
"sequence": "additional"
},
{
"affiliation": [],
"family": "García Díaz",
"given": "Andrea Lucia",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Gutiérrez Peña",
"given": "César Mauricio",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Martinez Medina",
"given": "Lucila",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-1298-0566",
"affiliation": [],
"authenticated-orcid": false,
"family": "Monroy Colin",
"given": "Victor Antonio",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-7430-702X",
"affiliation": [],
"authenticated-orcid": false,
"family": "Arreola Guerra",
"given": "Jose Manuel",
"sequence": "additional"
}
],
"container-title": [
"Infectious Disease Reports"
],
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2022,
3,
3
]
],
"date-time": "2022-03-03T14:24:53Z",
"timestamp": 1646317493000
},
"deposited": {
"date-parts": [
[
2022,
3,
3
]
],
"date-time": "2022-03-03T15:14:02Z",
"timestamp": 1646320442000
},
"indexed": {
"date-parts": [
[
2022,
3,
3
]
],
"date-time": "2022-03-03T15:42:12Z",
"timestamp": 1646322132444
},
"is-referenced-by-count": 0,
"issn-type": [
{
"type": "electronic",
"value": "2036-7449"
}
],
"issue": "2",
"issued": {
"date-parts": [
[
2022,
3,
3
]
]
},
"journal-issue": {
"issue": "2",
"published-online": {
"date-parts": [
[
2022,
4
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
3,
3
]
],
"date-time": "2022-03-03T00:00:00Z",
"timestamp": 1646265600000
}
}
],
"link": [
{
"URL": "https://www.mdpi.com/2036-7449/14/2/20/pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1968",
"original-title": [],
"page": "160-168",
"prefix": "10.3390",
"published": {
"date-parts": [
[
2022,
3,
3
]
]
},
"published-online": {
"date-parts": [
[
2022,
3,
3
]
]
},
"publisher": "MDPI AG",
"reference": [
{
"key": "ref1",
"unstructured": "Statement on the Second Meeting of the Emergency Committee of the International Health Regulations (2005) on the Outbreak of the New Coronavirus (2019-nCoV)\n https://www.who.int/news/item/30-01-2020-statement-on-the-second-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-outbreak-of-novel-coronavirus-(2019-ncov)"
},
{
"DOI": "10.1016/S1473-3099(03)00806-5",
"doi-asserted-by": "publisher",
"key": "ref2"
},
{
"DOI": "10.1056/NEJMoa2012410",
"doi-asserted-by": "publisher",
"key": "ref3"
},
{
"DOI": "10.1056/NEJMoa2019014",
"doi-asserted-by": "publisher",
"key": "ref4"
},
{
"DOI": "10.1056/NEJMoa2016638",
"doi-asserted-by": "publisher",
"key": "ref5"
},
{
"key": "ref6",
"unstructured": "Coronavirus Disease (COVID-19)\n https://www.who.int/es"
},
{
"DOI": "10.1016/j.antiviral.2020.104787",
"doi-asserted-by": "publisher",
"key": "ref7"
},
{
"DOI": "10.1001/jama.2019.21118",
"doi-asserted-by": "publisher",
"key": "ref8"
},
{
"DOI": "10.1164/rccm.201803-0589OC",
"doi-asserted-by": "publisher",
"key": "ref9"
},
{
"DOI": "10.1080/13102818.2020.1775118",
"doi-asserted-by": "publisher",
"key": "ref10"
},
{
"DOI": "10.1148/radiol.2020202708",
"doi-asserted-by": "publisher",
"key": "ref11"
},
{
"key": "ref12",
"unstructured": "Recommendations for Thromboprophylaxis and Antithrombotic Treatment in COVID-19 Patients\n https://www.covid-19.seth.es/wp-content/uploads/2020/04/Recomendaciones-tromboprofilaxis-y-tratamiento-antitrombotico-pacientes-COVID-19_2020-04-29.pdf"
},
{
"DOI": "10.1055/s-0040-1710019",
"doi-asserted-by": "publisher",
"key": "ref13"
},
{
"DOI": "10.1056/NEJMoa2021436",
"doi-asserted-by": "publisher",
"key": "ref14"
},
{
"article-title": "Predictors of success of high-flow nasal cannula in the treatment of acute hypoxemic respiratory failure [published online ahead of print, 2019 Aug 24]",
"author": "Ruiz",
"first-page": "80",
"journal-title": "Med. Intensiv.",
"key": "ref15",
"volume": "45",
"year": "2019"
},
{
"DOI": "10.1056/NEJMoa2023184",
"article-title": "Repurposed Antiviral Drugs for Covid-19—Interim WHO Solidarity Trial Results",
"author": "Pan",
"doi-asserted-by": "crossref",
"first-page": "497",
"journal-title": "N. Engl. J. Med.",
"key": "ref16",
"volume": "384",
"year": "2021"
},
{
"key": "ref17",
"unstructured": "Ministerio de Salud, Republica del Peru. Resolucion Ministerial. Published Online May 8, 2020\n https://cdn.www.gob.pe/uploads/document/file/694719/RM_270-2020-MINSA.PDF"
},
{
"DOI": "10.1016/j.chest.2020.10.009",
"doi-asserted-by": "publisher",
"key": "ref18"
},
{
"DOI": "10.1002/cpt.1889",
"doi-asserted-by": "publisher",
"key": "ref19"
},
{
"DOI": "10.1038/d41586-020-02958-2",
"doi-asserted-by": "publisher",
"key": "ref20"
}
],
"reference-count": 20,
"references-count": 20,
"relation": {},
"score": 1,
"short-container-title": [
"Infectious Disease Reports"
],
"short-title": [],
"source": "Crossref",
"subject": [
"Infectious Diseases"
],
"subtitle": [],
"title": [
"Efficacy and Safety of Ivermectin and Hydroxychloroquine in Patients with Severe COVID-19: A Randomized Controlled Trial"
],
"type": "journal-article",
"volume": "14"
}
beltrangonzalez