Frequency of COVID-19 Infection as a Function of Vitamin D Levels
et al., Nutrients, doi:10.3390/nu15071581, Mar 2023
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 136 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 134 patients in Poland between ages 6-50, showing higher risk of COVID-19 cases with vitamin D levels <12 ng/mL.
This is the 168th of 228 COVID-19 sufficiency studies for vitamin D, which collectively show higher levels reduce risk with p<0.0000000001.
This study is excluded in the after exclusion results of meta-analysis:
unadjusted results with no group details.
|
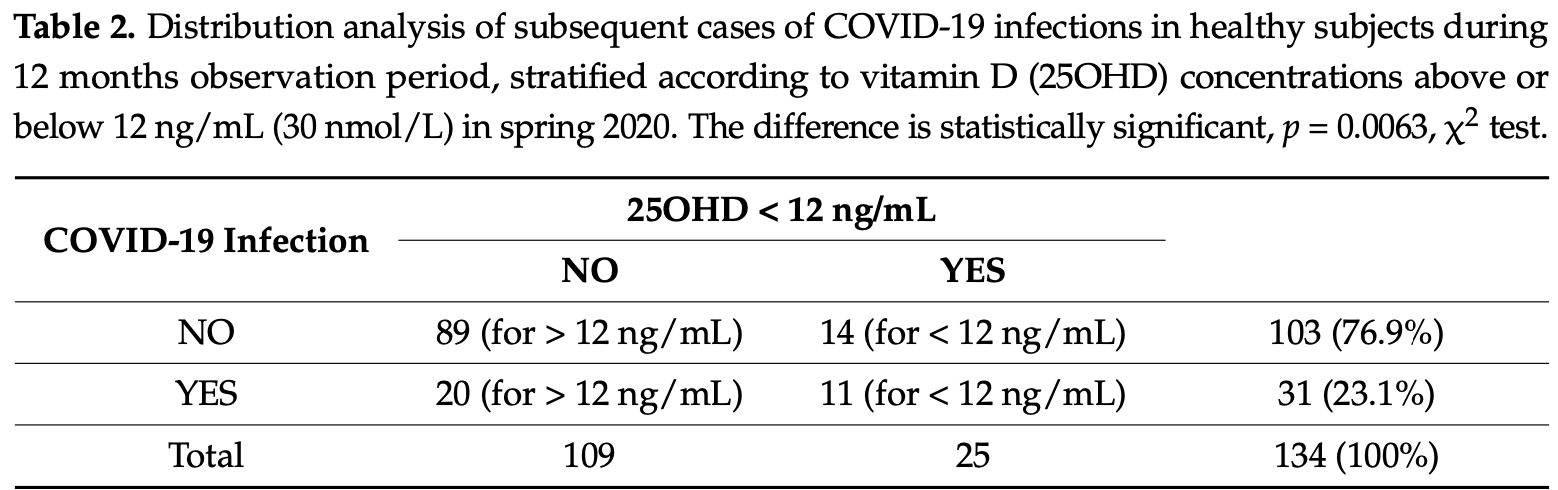
risk of case, 58.3% lower, RR 0.42, p = 0.02, high D levels (≥12ng/mL) 20 of 109 (18.3%), low D levels (<12ng/mL) 11 of 25 (44.0%), NNT 3.9.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Basińska-Lewandowska et al., 24 Mar 2023, retrospective, Poland, peer-reviewed, 5 authors.
Contact: elzbieta.skowronska-jozwiak@umed.lodz.pl (corresponding author), mblbas@poczta.onet.pl, krzysztof.lewandowski@umed.lodz.pl, andrzej.lewinski@umed.lodz.pl, wojciech.horzelski@wmii.uni.lodz.pl.
Frequency of COVID-19 Infection as a Function of Vitamin D Levels
Nutrients, doi:10.3390/nu15071581
Background: It has been speculated that higher concentrations of 25-hydroxy-vitamin D (25OHD) provide some protection against COVID-19. We assessed whether there is any relationship between 25OHD concentrations and the subsequent development of COVID-19 infection. Materials and Methods: Concentrations of 25OHD were measured in March-April 2020 in 134 healthy subjects (57 males), age range 6-50, from a single urban general practice in central Poland. Data on COVID-19 infection during the subsequent 12 months (prior to the vaccination program) were obtained from the national database of COVID-19 cases. None of the subjects received any 25OHD supplements. Results: The average 25OHD concentrations were 18.1 ± 7.39 ng/mL (37.3% had 25OHD above 20 ng/mL). Thirty-one (23.1%) patients developed COVID-19 infection, but an increased risk was only observed in individuals with 25OHD concentrations below 12 ng/mL (COVID-19 infection in 11 out of 25 patients (44%) with 25OHD < 12 ng/mL versus 20 out of 109 (18.3%) for those with 25OHD above 12 ng/mL, p = 0.0063). Such a relationship was no longer observed for subjects with 25OHD concentrations above 20 ng/mL (p = 0.2787). Conclusions: Although only a minority of healthy subjects had 25OHD concentrations above 20 ng/mL in spring, an increased risk of subsequent COVID-19 infection was only observed in those with severe 25OHD deficiency (<12 ng/mL).
Conflicts of Interest: The authors declare no conflict of interest.
References
Baktash, Hosack, Patel, Shah, Kanbdiah et al., Vitamin D status and outcomes for hospitalised older patients with COVID-19, Postgrad Med. J, doi:10.1136/postgradmedj-2020-138712
Basi Ńska-Lewandowska, Lewi Ński, Horzelski, Skowro Ńska-Jóźwiak, Effect of Summer Sunshine Exposure on Vitamin D Status in Young and Middle Age Poles: Is 30 ng/mL Vitamin D Cut-Off Really Suitable for the Polish Population?, Int. J. Environ. Res. Public Health, doi:10.3390/ijerph18158116
Binkley, Coursin, Krueger, Iglar, Heiner et al., Surgery alters parameters of vitamin D status and other laboratory results, Osteoporos Int, doi:10.1007/s00198-016-3819-9
Borsche, Glauner, Von Mendel, COVID-19 Mortality Risk Correlates Inversely with Vitamin D3 Status, and a Mortality Rate Close to Zero Could Theoretically Be Achieved at 50 ng/mL 25(OH)D3: Results of a Systematic Review and Meta-Analysis, Nutrients, doi:10.3390/nu13103596
Cummings, Rosen, VITAL Findings-A Decisive Verdict on Vitamin D Supplementation, N. Engl. J. Med, doi:10.1056/NEJMe2205993
Grant, Lahore, Mcdonnell, Baggerly, French et al., Evidence that Vitamin D Supplementation Could Reduce Risk of Influenza and COVID-19 Infections and Deaths, Nutrients, doi:10.3390/nu12040988
Hernandez, Nan, Fernandez-Ayala, Garcia-Unzueta, Hernandez-Hernandez et al., Vitamin D Status in Hospitalized Patients with SARS-CoV-2
Holick, Binkley, Bischoff-Ferrari, Gordon, Hanley et al., Evaluation, treatment, and prevention of vitamin D deficiency: An Endocrine Society clinical practice guideline, J. Clin. Endocrinol. Metab, doi:10.1210/jc.2011-0385
Hosseini, El Abd, Ducharme, Effects of Vitamin D Supplementation on COVID-19 Related Outcomes: A Systematic Review and Meta-Analysis, Nutrients, doi:10.3390/nu14102134
Jolliffe, Holt, Greenig, Talaei, Perdek et al., Effect of a test-and-treat approach to vitamin D supplementation on risk of all cause acute respiratory tract infection and covid-19: Phase 3 randomised controlled trial (CORONAVIT), BMJ, doi:10.1136/bmj-2022-071230
Leboff, Chou, Ratliff, Cook, Khurana et al., Supplemental Vitamin D and Incident Fractures in Midlife and Older Adults, N. Engl. J. Med, doi:10.1056/NEJMoa2202106
Lopez-Castro, Coronavirus disease-19 pandemic and vitamin D: So much for so little?, Rev. Investig. Clin, doi:10.24875/RIC.21000305
Mercola, Grant, Wagner, Evidence Regarding Vitamin D and Risk of COVID-19 and Its Severity, Nutrients, doi:10.3390/nu12113361
Nogues, Ovejero, Pineda-Moncusi, Bouillon, Arenas et al., Calcifediol treatment and COVID-19-related outcomes, J. Clin. Endocrinol. Metab, doi:10.1210/clinem/dgab405
Oristrell, Oliva, Casado, Subirana, Domínguez et al., Vitamin D supplementation and COVID-19 risk: A population-based, cohort study, J. Endocrinol. Investig, doi:10.1007/s40618-021-01639-9
Oscanoa, Ghashut, Carvajal, Romero-Ortuno, Association between low serum vitamin D and increased mortality and severity due to COVID-19: Reverse causality?, Disaster Emerg. Med. J, doi:10.5603/DEMJ.a2022.0016
Perna, Is vitamin D supplementation useful for weight-loss programs? A systematic review and meta-analysis of randomized controlled trials, Medicina, doi:10.3390/medicina55070368
Perna, The enigma of vitamin D supplementation in aging with obesity, Minerva. Gastroenterol, doi:10.23736/S2724-5985.21.02955-7
Płudowski, Kos-Kudła, Walczak, Fal, Zozuli Ńska-Ziółkiewicz et al., Guidelines for Preventing and Treating Vitamin D Deficiency: A 2023 Update in Poland, Nutrients, doi:10.3390/nu15030695
Rosen, Abrams, Aloia, Brannon, Clinton et al., IOM committee members respond to Endocrine Society vitamin D guideline, J. Clin. Endocrinol. Metab, doi:10.1210/jc.2011-2218
Rubin, Sorting out whether vitamin D deficiency raises COVID-19 risk, JAMA, doi:10.1001/jama.2020.24127
Sassi, Tamone, D'amelio, Vitamin, Nutrient, Hormone, and Immunomodulator, Nutrients, doi:10.3390/nu10111656
Silva, Furlanetto, Does serum 25-hydroxyvitamin D decrease during acute-phase response? A systematic review, Nutr. Res, doi:10.1016/j.nutres.2014.12.008
Stroehlein, Wallqvist, Iannizzi, Mikolajewsja, Metzendorf et al., Supplementation for the treatment of COVID-19: A living systematic review, Cochrane Database Syst. Rev, doi:10.1002/14651858.CD015043
Sulli, Gotelli, Casabella, Paolino, Pizzorni et al., Vitamin D and Lung Outcomes in Elderly COVID-19 Patients, Nutrients, doi:10.3390/nu13030717
Wang, Joshi, Leopold, Jackson, Christensen et al., Association of vitamin D deficiency with COVID-19 infection severity: Systematic review and meta-analysis, Clin. Endocrinol, doi:10.1111/cen.14540
Zygmunt, Lewi Ński, Niedobór witaminy D a cię żki przebieg COVID-19 czy istnieje zwi ązek? [Vitamin D deficiency and severe course of COVID-19-Is there a connection?
DOI record:
{
"DOI": "10.3390/nu15071581",
"ISSN": [
"2072-6643"
],
"URL": "http://dx.doi.org/10.3390/nu15071581",
"abstract": "<jats:p>Background: It has been speculated that higher concentrations of 25-hydroxy-vitamin D (25OHD) provide some protection against COVID-19. We assessed whether there is any relationship between 25OHD concentrations and the subsequent development of COVID-19 infection. Materials and Methods: Concentrations of 25OHD were measured in March–April 2020 in 134 healthy subjects (57 males), age range 6–50, from a single urban general practice in central Poland. Data on COVID-19 infection during the subsequent 12 months (prior to the vaccination program) were obtained from the national database of COVID-19 cases. None of the subjects received any 25OHD supplements. Results: The average 25OHD concentrations were 18.1 ± 7.39 ng/mL (37.3% had 25OHD above 20 ng/mL). Thirty-one (23.1%) patients developed COVID-19 infection, but an increased risk was only observed in individuals with 25OHD concentrations below 12 ng/mL (COVID-19 infection in 11 out of 25 patients (44%) with 25OHD < 12 ng/mL versus 20 out of 109 (18.3%) for those with 25OHD above 12 ng/mL, p = 0.0063). Such a relationship was no longer observed for subjects with 25OHD concentrations above 20 ng/mL (p = 0.2787). Conclusions: Although only a minority of healthy subjects had 25OHD concentrations above 20 ng/mL in spring, an increased risk of subsequent COVID-19 infection was only observed in those with severe 25OHD deficiency (<12 ng/mL).</jats:p>",
"alternative-id": [
"nu15071581"
],
"author": [
{
"affiliation": [
{
"name": "“Your Family Doctor”, General Practice Surgery, 93-324 Lodz, Poland"
}
],
"family": "Basińska-Lewandowska",
"given": "Magdalena",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0002-9113-2804",
"affiliation": [
{
"name": "Department of Endocrinology and Metabolic Diseases, Medical University of Lodz, 90-419 Lodz, Poland"
},
{
"name": "Department of Endocrinology and Metabolic Diseases, Polish Mother’s Memorial Hospital—Research Institute, 93-338 Lodz, Poland"
}
],
"authenticated-orcid": false,
"family": "Lewandowski",
"given": "Krzysztof",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-3690-5368",
"affiliation": [
{
"name": "Department of Mathematics and Computer Science, University of Lodz, 90-238 Lodz, Poland"
}
],
"authenticated-orcid": false,
"family": "Horzelski",
"given": "Wojciech",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-8748-3337",
"affiliation": [
{
"name": "Department of Endocrinology and Metabolic Diseases, Medical University of Lodz, 90-419 Lodz, Poland"
},
{
"name": "Department of Endocrinology and Metabolic Diseases, Polish Mother’s Memorial Hospital—Research Institute, 93-338 Lodz, Poland"
}
],
"authenticated-orcid": false,
"family": "Lewiński",
"given": "Andrzej",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-0019-4269",
"affiliation": [
{
"name": "Department of Endocrinology and Metabolic Diseases, Medical University of Lodz, 90-419 Lodz, Poland"
},
{
"name": "Department of Endocrinology and Metabolic Diseases, Polish Mother’s Memorial Hospital—Research Institute, 93-338 Lodz, Poland"
}
],
"authenticated-orcid": false,
"family": "Skowrońska-Jóźwiak",
"given": "Elżbieta",
"sequence": "additional"
}
],
"container-title": "Nutrients",
"container-title-short": "Nutrients",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2023,
3,
24
]
],
"date-time": "2023-03-24T12:43:03Z",
"timestamp": 1679661783000
},
"deposited": {
"date-parts": [
[
2023,
3,
24
]
],
"date-time": "2023-03-24T13:46:22Z",
"timestamp": 1679665582000
},
"funder": [
{
"award": [
"503/1-107-03/503-11-001-19-00"
],
"name": "Medical University of Lodz"
}
],
"indexed": {
"date-parts": [
[
2023,
3,
25
]
],
"date-time": "2023-03-25T04:46:42Z",
"timestamp": 1679719602776
},
"is-referenced-by-count": 0,
"issue": "7",
"issued": {
"date-parts": [
[
2023,
3,
24
]
]
},
"journal-issue": {
"issue": "7",
"published-online": {
"date-parts": [
[
2023,
4
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
3,
24
]
],
"date-time": "2023-03-24T00:00:00Z",
"timestamp": 1679616000000
}
}
],
"link": [
{
"URL": "https://www.mdpi.com/2072-6643/15/7/1581/pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1968",
"original-title": [],
"page": "1581",
"prefix": "10.3390",
"published": {
"date-parts": [
[
2023,
3,
24
]
]
},
"published-online": {
"date-parts": [
[
2023,
3,
24
]
]
},
"publisher": "MDPI AG",
"reference": [
{
"DOI": "10.3390/nu10111656",
"doi-asserted-by": "crossref",
"key": "ref_1",
"unstructured": "Sassi, F., Tamone, C., and D’Amelio, P. (2018). Vitamin D: Nutrient, Hormone, and Immunomodulator. Nutrients, 10."
},
{
"DOI": "10.3390/nu12113361",
"doi-asserted-by": "crossref",
"key": "ref_2",
"unstructured": "Mercola, J., Grant, W.B., and Wagner, C.L. (2020). Evidence Regarding Vitamin D and Risk of COVID-19 and Its Severity. Nutrients, 12."
},
{
"article-title": "Niedobór witaminy D a ciężki przebieg COVID-19 czy istnieje związek? [Vitamin D deficiency and severe course of COVID-19—Is there a connection?]",
"author": "Zygmunt",
"first-page": "69",
"journal-title": "Med. Prakt.",
"key": "ref_3",
"volume": "7–8",
"year": "2020"
},
{
"DOI": "10.1007/s40618-021-01639-9",
"article-title": "Vitamin D supplementation and COVID-19 risk: A population-based, cohort study",
"author": "Oristrell",
"doi-asserted-by": "crossref",
"first-page": "167",
"journal-title": "J. Endocrinol. Investig.",
"key": "ref_4",
"volume": "45",
"year": "2022"
},
{
"DOI": "10.20944/preprints202003.0235.v2",
"doi-asserted-by": "crossref",
"key": "ref_5",
"unstructured": "Grant, W.B., Lahore, H., McDonnell, S.L., Baggerly, C.A., French, C.B., Aliano, J.L., and Bhattoa, H.P. (2020). Evidence that Vitamin D Supplementation Could Reduce Risk of Influenza and COVID-19 Infections and Deaths. Nutrients, 12."
},
{
"DOI": "10.1101/2021.09.22.21263977",
"doi-asserted-by": "crossref",
"key": "ref_6",
"unstructured": "Borsche, L., Glauner, B., and von Mendel, J. (2021). COVID-19 Mortality Risk Correlates Inversely with Vitamin D3 Status, and a Mortality Rate Close to Zero Could Theoretically Be Achieved at 50 ng/mL 25(OH)D3: Results of a Systematic Review and Meta-Analysis. Nutrients, 13."
},
{
"article-title": "Supplementation for the treatment of COVID-19: A living systematic review",
"author": "Stroehlein",
"first-page": "CD015043",
"journal-title": "Cochrane Database Syst. Rev.",
"key": "ref_7",
"volume": "5",
"year": "2021"
},
{
"DOI": "10.3390/nu14102134",
"doi-asserted-by": "crossref",
"key": "ref_8",
"unstructured": "Hosseini, B., El Abd, A., and Ducharme, F.M. (2022). Effects of Vitamin D Supplementation on COVID-19 Related Outcomes: A Systematic Review and Meta-Analysis. Nutrients, 14."
},
{
"DOI": "10.1056/NEJMoa2202106",
"article-title": "Supplemental Vitamin D and Incident Fractures in Midlife and Older Adults",
"author": "LeBoff",
"doi-asserted-by": "crossref",
"first-page": "299",
"journal-title": "N. Engl. J. Med.",
"key": "ref_9",
"volume": "387",
"year": "2022"
},
{
"article-title": "Coronavirus disease-19 pandemic and vitamin D: So much for so little?",
"first-page": "408",
"journal-title": "Rev. Investig. Clin.",
"key": "ref_10",
"volume": "73",
"year": "2021"
},
{
"DOI": "10.1001/jama.2020.24127",
"article-title": "Sorting out whether vitamin D deficiency raises COVID-19 risk",
"author": "Rubin",
"doi-asserted-by": "crossref",
"first-page": "329",
"journal-title": "JAMA",
"key": "ref_11",
"volume": "325",
"year": "2021"
},
{
"DOI": "10.1210/jc.2011-2218",
"article-title": "IOM committee members respond to Endocrine Society vitamin D guideline",
"author": "Rosen",
"doi-asserted-by": "crossref",
"first-page": "1146",
"journal-title": "J. Clin. Endocrinol. Metab.",
"key": "ref_12",
"volume": "97",
"year": "2012"
},
{
"DOI": "10.1210/jc.2011-0385",
"article-title": "Evaluation, treatment, and prevention of vitamin D deficiency: An Endocrine Society clinical practice guideline",
"author": "Holick",
"doi-asserted-by": "crossref",
"first-page": "1911",
"journal-title": "J. Clin. Endocrinol. Metab.",
"key": "ref_13",
"volume": "96",
"year": "2011"
},
{
"DOI": "10.3390/nu15030695",
"doi-asserted-by": "crossref",
"key": "ref_14",
"unstructured": "Płudowski, P., Kos-Kudła, B., Walczak, M., Fal, A., Zozulińska-Ziółkiewicz, D., Sieroszewski, P., Peregud-Pogorzelski, J., Lauterbach, R., Targowski, T., and Lewiński, A. (2023). Guidelines for Preventing and Treating Vitamin D Deficiency: A 2023 Update in Poland. Nutrients, 15."
},
{
"DOI": "10.3390/ijerph18158116",
"doi-asserted-by": "crossref",
"key": "ref_15",
"unstructured": "Basińska-Lewandowska, M., Lewiński, A., Horzelski, W., and Skowrońska-Jóźwiak, E. (2021). Effect of Summer Sunshine Exposure on Vitamin D Status in Young and Middle Age Poles: Is 30 ng/mL Vitamin D Cut-Off Really Suitable for the Polish Population?. Int. J. Environ. Res. Public Health, 18."
},
{
"DOI": "10.1136/bmj-2022-071230",
"article-title": "Effect of a test-and-treat approach to vitamin D supplementation on risk of all cause acute respiratory tract infection and covid-19: Phase 3 randomised controlled trial (CORONAVIT)",
"author": "Jolliffe",
"doi-asserted-by": "crossref",
"first-page": "e071230",
"journal-title": "BMJ",
"key": "ref_16",
"volume": "378",
"year": "2022"
},
{
"DOI": "10.1111/cen.14540",
"article-title": "Association of vitamin D deficiency with COVID-19 infection severity: Systematic review and meta-analysis",
"author": "Wang",
"doi-asserted-by": "crossref",
"first-page": "281",
"journal-title": "Clin. Endocrinol.",
"key": "ref_17",
"volume": "96",
"year": "2022"
},
{
"DOI": "10.1210/clinem/dgaa733",
"article-title": "Vitamin D Status in Hospitalized Patients with SARS-CoV-2 Infection",
"author": "Hernandez",
"doi-asserted-by": "crossref",
"first-page": "e1343",
"journal-title": "J. Clin. Endocrinol. Metab.",
"key": "ref_18",
"volume": "106",
"year": "2021"
},
{
"DOI": "10.1136/postgradmedj-2020-138712",
"article-title": "Vitamin D status and outcomes for hospitalised older patients with COVID-19",
"author": "Baktash",
"doi-asserted-by": "crossref",
"first-page": "442",
"journal-title": "Postgrad Med. J.",
"key": "ref_19",
"volume": "97",
"year": "2021"
},
{
"DOI": "10.3390/nu13030717",
"doi-asserted-by": "crossref",
"key": "ref_20",
"unstructured": "Sulli, A., Gotelli, E., Casabella, A., Paolino, S., Pizzorni, C., Alessandri, E., Grosso, M., Ferone, D., Smith, V., and Cutolo, M. (2021). Vitamin D and Lung Outcomes in Elderly COVID-19 Patients. Nutrients, 13."
},
{
"DOI": "10.1210/clinem/dgab405",
"article-title": "Calcifediol treatment and COVID-19-related outcomes",
"author": "Nogues",
"doi-asserted-by": "crossref",
"first-page": "e4017",
"journal-title": "J. Clin. Endocrinol. Metab.",
"key": "ref_21",
"volume": "106",
"year": "2021"
},
{
"DOI": "10.1016/j.nutres.2014.12.008",
"article-title": "Does serum 25-hydroxyvitamin D decrease during acute-phase response? A systematic review",
"author": "Silva",
"doi-asserted-by": "crossref",
"first-page": "91",
"journal-title": "Nutr. Res.",
"key": "ref_22",
"volume": "35",
"year": "2015"
},
{
"DOI": "10.1007/s00198-016-3819-9",
"article-title": "Surgery alters parameters of vitamin D status and other laboratory results",
"author": "Binkley",
"doi-asserted-by": "crossref",
"first-page": "1013",
"journal-title": "Osteoporos Int.",
"key": "ref_23",
"volume": "28",
"year": "2017"
},
{
"DOI": "10.5603/DEMJ.a2022.0016",
"article-title": "Association between low serum vitamin D and increased mortality and severity due to COVID-19: Reverse causality?",
"author": "Oscanoa",
"doi-asserted-by": "crossref",
"first-page": "124",
"journal-title": "Disaster Emerg. Med. J.",
"key": "ref_24",
"volume": "7",
"year": "2022"
},
{
"DOI": "10.23736/S2724-5985.21.02955-7",
"article-title": "The enigma of vitamin D supplementation in aging with obesity",
"author": "Perna",
"doi-asserted-by": "crossref",
"first-page": "459",
"journal-title": "Minerva. Gastroenterol.",
"key": "ref_25",
"volume": "68",
"year": "2022"
},
{
"DOI": "10.3390/medicina55070368",
"doi-asserted-by": "crossref",
"key": "ref_26",
"unstructured": "Perna, S. (2019). Is vitamin D supplementation useful for weight-loss programs? A systematic review and meta-analysis of randomized controlled trials. Medicina, 55."
},
{
"DOI": "10.1056/NEJMe2205993",
"article-title": "VITAL Findings—A Decisive Verdict on Vitamin D Supplementation",
"author": "Cummings",
"doi-asserted-by": "crossref",
"first-page": "368",
"journal-title": "N. Engl. J. Med.",
"key": "ref_27",
"volume": "387",
"year": "2022"
}
],
"reference-count": 27,
"references-count": 27,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.mdpi.com/2072-6643/15/7/1581"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Food Science",
"Nutrition and Dietetics"
],
"subtitle": [],
"title": "Frequency of COVID-19 Infection as a Function of Vitamin D Levels",
"type": "journal-article",
"volume": "15"
}
