Vitamin D Levels as a Marker of Severe SARS-CoV-2 Infection
et al., Life, doi:10.3390/life14020210, Sep 2023 (preprint)
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 136 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 88 hospitalized COVID-19 patients and matched controls, showing significantly lower vitamin D levels for COVID-19 patients, and higher mortality for COVID-19 patients with deficiency of insufficiency in unadjusted results, without statistical significance.
This is the 188th of 228 COVID-19 sufficiency studies for vitamin D, which collectively show higher levels reduce risk with p<0.0000000001.
This study is excluded in the after exclusion results of meta-analysis:
unadjusted results with no group details.
|
risk of death, 47.9% lower, RR 0.52, p = 0.39, high D levels (≥10ng/mL) 5 of 64 (7.8%), low D levels (<10ng/mL) 3 of 20 (15.0%), NNT 14.
|
|
risk of death, 43.0% lower, RR 0.57, p = 0.70, high D levels (≥20ng/mL) 2 of 31 (6.5%), low D levels (<20ng/mL) 6 of 53 (11.3%), NNT 21.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Athanassiou et al., 15 Sep 2023, prospective, Greece, peer-reviewed, 9 authors.
Contact: ikostoglouathanassiou@yahoo.gr (corresponding author), lambros.ath@gmail.com, sofnikol@yahoo.gr, alexkonstantinou2@gmail.com, esiarkos@gmail.com, xarisamar@gmail.com, olmascha@gmail.com, pathanassiou@yahoo.gr, yehuda.shoenfeld@sheba.health.gov.il.
Vitamin D Levels as a Marker of Severe SARS-CoV-2 Infection
Life, doi:10.3390/life14020210
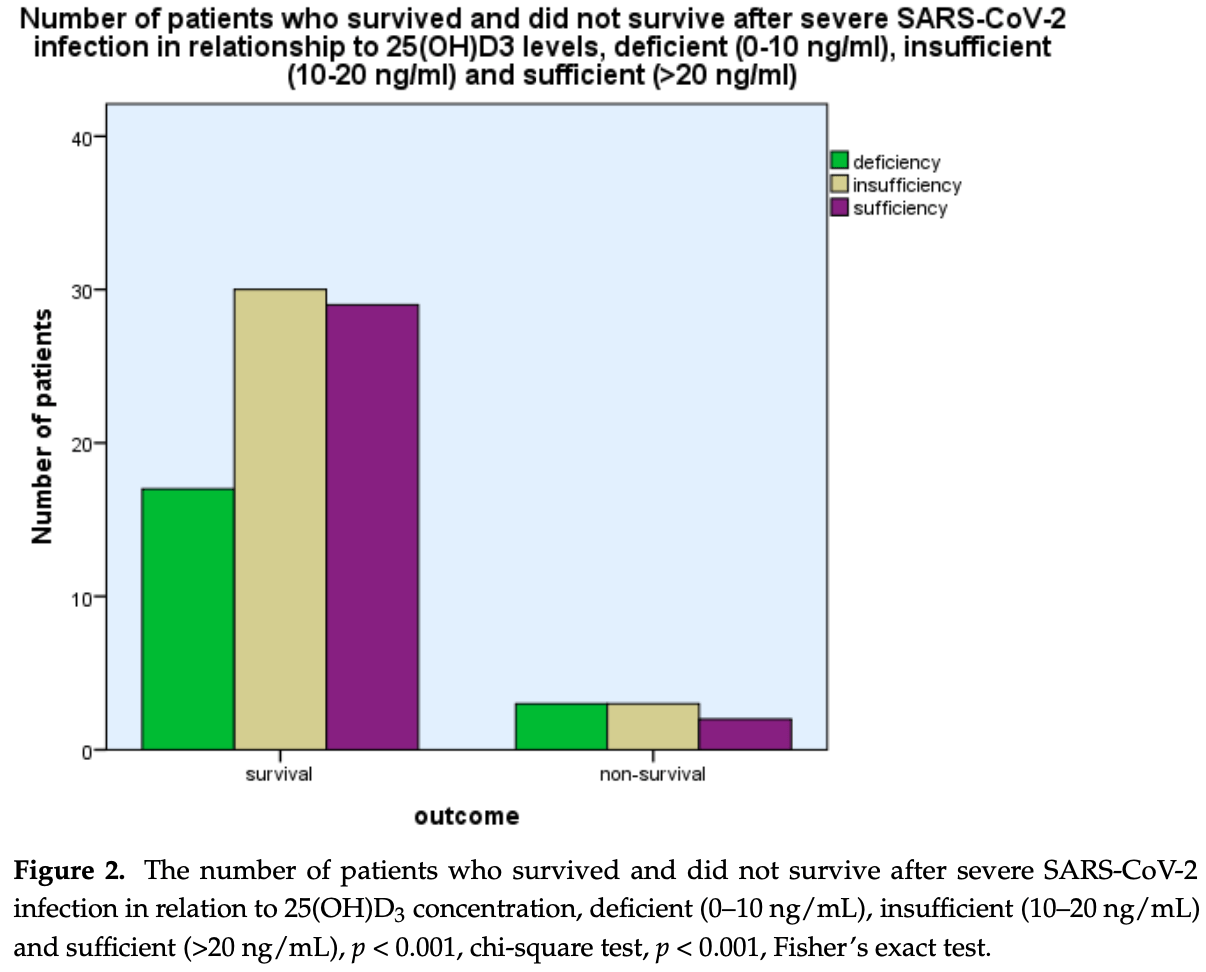
The SARS-CoV-2 virus may cause severe infection, which is associated with diverse clinical manifestations. Vitamin D has immunomodulating properties and may enhance the body's defense system against invading pathogenic organisms. The aim was to assess 25(OH)D 3 levels in patients hospitalized for severe infection from the SARS-CoV-2 virus and explore the relationship between 25(OH)D 3 and outcomes. In a group of 88 patients hospitalized for severe infection from the SARS-CoV-2 virus and a control group matched for age and sex, the levels of 25(OH)D 3 were analyzed. Levels of 25(OH)D 3 were 17.36 ± 8.80 ng/mL (mean ± SD) compared with 24.34 ± 10.34 ng/mL in patients with severe SARS-CoV-2 infection and the control group, respectively, p < 0.001 (Student's t-test). 25(OH)D 3 levels were significantly related to outcomes, i.e., survival as opposed to nonsurvival, as more patients with 25(OH)D 3 deficiency (0-10 ng/mL) and insufficiency (10-20 ng/mL) had a fatal outcome as compared with those with vitamin D sufficiency (p < 0.001, chi-square test, p < 0.001, Fisher's exact test). Levels of 25(OH)D3 were inversely related to C-reactive protein (CRP), ferritin, d-dimer, and fibrinogen levels (p < 0.001, linear regression analysis, beta coefficient of variation, -0.176, -0.160, -0.178, and -0.158, respectively). Vitamin D deficiency observed in severe SARS-CoV-2 infection was related to disease outcomes.
Funding: This research received no external funding.
Institutional Review Board Statement: The study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of Asclepeion Hospital, Voula, Athens, Greece, approval number 15335, 24 November 2020. Informed Consent Statement: Informed consent was obtained from all subjects involved in the study. Written informed consent has been obtained from the patients to publish this paper.
Conflicts of Interest: The authors declare no conflicts of interest.
References
Ackermann, Verleden, Kuehnel, Haverich, Welte et al., Pulmonary Vascular Endothelialitis, Thrombosis, and Angiogenesis in COVID-19, N. Engl. J. Med, doi:10.1056/NEJMoa2015432
Ahmed, A Network-Based Analysis Reveals the Mechanism Underlying Vitamin D in Suppressing Cytokine Storm and Virus in SARS-CoV-2 Infection, Front. Immunol, doi:10.3389/fimmu.2020.590459
Ali, Spinler, COVID-19 and thrombosis: From bench to bedside, Trends Cardiovasc. Med, doi:10.1016/j.tcm.2020.12.004
Alsafar, Grant, Hijazi, Uddin, Alkaabi et al., COVID-19 Disease Severity and Death in Relation to Vitamin D Status among SARS-CoV-2-Positive UAE Residents, Nutrients, doi:10.3390/nu13051714
Andreakos, Papadaki, Serhan, Dexamethasone, pro-resolving lipid mediators and resolution of inflammation in COVID-19, Allergy, doi:10.1111/all.14595
Annweiler, Beaudenon, Gautier, Gonsard, Boucher et al., High-dose versus standard-dose vitamin D supplementation in older adults with COVID-19 (COVIT-TRIAL): A multicenter, open-label, randomized controlled superiority trial, PLoS Med, doi:10.1371/journal.pmed.1003999
Annweiler, Beaudenon, Gautier, Simon, Dubée et al., COvid-19 and high-dose VITamin D supplementation TRIAL in high-risk older patients (COVIT-TRIAL): Study protocol for a randomized controlled trial, Trials, doi:10.1186/s13063-020-04928-5
Antonelli, Kushner, Epstein, The constellation of vitamin D, the acute-phase response, and inflammation, Cleve. Clin. J. Med, doi:10.3949/ccjm.90a.22048
Arosio, Levi, Ferritin, iron homeostasis, and oxidative damage, Free Radic. Biol. Med, doi:10.1016/S0891-5849(02)00842-0
Azzam, Ghozy, Azab, Vitamin D and its' role in Parkinson's disease patients with SARS-CoV-2 infection. A review article, Interdiscip. Neurosurg, doi:10.1016/j.inat.2021.101441
Bacchetta, Zaritsky, Sea, Chun, Lisse et al., Suppression of iron-regulatory hepcidin by vitamin D, J. Am. Soc. Nephrol, doi:10.1681/ASN.2013040355
Bae, Kim, Mini-Review on the Roles of Vitamin C, Vitamin D, and Selenium in the Immune System against COVID-19, Molecules, doi:10.3390/molecules25225346
Bassatne, Basbous, Chakhtoura, El Zein, Rahme et al., The link between COVID-19 and VItamin D (VIVID): A systematic review and meta-analysis, Metabolism, doi:10.1016/j.metabol.2021.154753
Bhatti, Bhatti, Khullar, Reddy, Reddy, Therapeutic Strategies in the Development of Anti-viral Drugs and Vaccines Against SARS-CoV-2 Infection, Mol. Neurobiol, doi:10.1007/s12035-020-02074-2
Bilezikian, Formenti, Adler, Binkley, Bouillon et al., Dosing, levels, form, and route of administration: Does one approach fit all?, Rev. Endocr. Metab. Disord, doi:10.1007/s11154-021-09693-7
Bobescu, Marceanu, Covaciu, Vladau, Thrombosis, an important piece in the COVID-19 puzzle: From pathophysiology to therapy, Anatol. J. Cardiol, doi:10.5152/AnatolJCardiol.2021.475
Boulkrane, Ilina, Melchakov, Fedotova, Drago et al., COVID-19 Disease and Vitamin D: A Mini-Review, Front. Pharmacol, doi:10.3389/fphar.2020.604579
Channappanavar, Perlman, Pathogenic human coronavirus infections: Causes and consequences of cytokine storm and immunopathology, Semin. Immunopathol, doi:10.1007/s00281-017-0629-x
Charoenngam, Holick, Immunologic Effects of Vitamin D on Human Health and Disease, Nutrients, doi:10.3390/nu12072097
Charoenngam, Shirvani, Holick, Vitamin D for skeletal and non-skeletal health: What we should know, J. Clin. Orthop. Trauma, doi:10.1016/j.jcot.2019.07.004
Cheng, Li, Li, Liu, Yan et al., Ferritin in the coronavirus disease 2019 (COVID-19): A systematic review and meta-analysis, J. Clin. Lab. Anal, doi:10.1002/jcla.23618
Chiodini, Gatti, Soranna, Merlotti, Mingiano et al., Vitamin D Status and SARS-CoV-2 Infection and COVID-19 Clinical Outcomes, Front. Public Health, doi:10.3389/fpubh.2021.736665
Cimmino, Conte, Morello, Pellegrino, Marra et al., Vitamin D Inhibits IL-6 Pro-Atherothrombotic Effects in Human Endothelial Cells: A Potential Mechanism for Protection against COVID-19 Infection?, J. Cardiovasc. Dev. Dis, doi:10.3390/jcdd9010027
Contreras-Bolívar, García-Fontana, García-Fontana, Muñoz-Torres, Vitamin D and COVID-19: Where are we now?, Postgrad. Med, doi:10.1080/00325481.2021.2017647
Cui, Zhang, Kang, Ren, Miao et al., High-Volume Hemofiltration in Critically Ill Patients With Secondary Hemophagocytic Lymphohistiocytosis/Macrophage Activation Syndrome: A Prospective Study in the PICU, Pediatr. Crit. Care Med, doi:10.1097/PCC.0000000000000896
D'ecclesiis, Gavioli, Martinoli, Raimondi, Chiocca et al., Vitamin D and SARS-CoV2 infection, severity and mortality: A systematic review and meta-analysis, PLoS ONE, doi:10.1371/journal.pone.0268396
Daneshkhah, Agrawal, Eshein, Subramanian, Roy et al., Evidence for possible association of vitamin D status with cytokine storm and unregulated inflammation in COVID-19 patients, Aging Clin. Exp. Res, doi:10.1007/s40520-020-01677-y
Decyk, Kobyli Ńska, Antosik, Kurowska, Vitamin D in SARS-CoV-2 infection, Rocz. Panstw. Zakl. Hig, doi:10.32394/rpzh.2022.0191
Dennison, De Oliveira, Fraga, Lima, Ferreira et al., Mycobacterium leprae-helminth co-infections and vitamin D deficiency as potential risk factors for leprosy: A case-control study in south-eastern Brazil, Int. J. Infect. Dis, doi:10.1016/j.ijid.2021.02.048
Farrag, Amer, Bhat, Hamed, Aziz et al., SARS-CoV-2: An Overview of Virus Genetics, Transmission, and Immunopathogenesis, Int. J. Environ. Res. Public Health, doi:10.3390/ijerph18126312
Farrell, Martin, Mcwhinney, Straub, Williams et al., State-of-the-art vitamin D assays: A comparison of automated immunoassays with liquid chromatography-tandem mass spectrometry methods, Clin. Chem, doi:10.1373/clinchem.2011.172155
Feentved Ødum, Kongsbak-Wismann, Vitamin D and SARS-CoV-2, Basic. Clin. Pharmacol. Toxicol, doi:10.1111/bcpt.13872
Ferrari, Locatelli, Briguglio, Lombardi, Is there a link between vitamin D status, SARS-CoV-2 infection risk and COVID-19 severity?, Cell Biochem. Funct, doi:10.1002/cbf.3597
Gao, Ding, Dong, Zhang, Kursat Azkur et al., Risk factors for severe and critically ill COVID-19 patients: A review, Allergy, doi:10.1111/all.14657
Golob, Lugogo, Lauring, Lok, SARS-CoV-2 vaccines: A triumph of science and collaboration, JCI Insight, doi:10.1172/jci.insight.149187
Grant, Lahore, Mcdonnell, Baggerly, French et al., Evidence that Vitamin D Supplementation Could Reduce Risk of Influenza and COVID-19 Infections and Deaths, Nutrients, doi:10.3390/nu12040988
Helms, Tacquard, Severac, Leonard-Lorant, Ohana et al., High risk of thrombosis in patients with severe SARS-CoV-2 infection: A multicenter prospective cohort study, Intensive Care Med, doi:10.1007/s00134-020-06062-x
Hsieh, Hsiao, Liao, Hou, Chang et al., The Role of Vitamin D in SARS-CoV-2 Infection and Acute Kidney Injury, Int. J. Mol. Sci, doi:10.3390/ijms23137368
Imai, Ito, Kiso, Yamayoshi, Uraki et al., Efficacy of Antiviral Agents against Omicron Subvariants BQ.1.1 and XBB, N. Engl. J. Med, doi:10.1056/NEJMc2214302
Karcioglu Batur, Hekim, The role of DBP gene polymorphisms in the prevalence of new coronavirus disease 2019 infection and mortality rate, J. Med. Virol, doi:10.1002/jmv.26409
Kim, Teles, Haile, Liu, Modlin, Vitamin D status contributes to the antimicrobial activity of macrophages against Mycobacterium leprae, PLoS Negl. Trop. Dis, doi:10.1371/journal.pntd.0006608
Klein, Arnaud, Gallagher, Deluca, Riggs, Intestinal calcium absorption in exogenous hypercortisonism. Role of 25-hydroxyvitamin D and corticosteroid dose, J. Clin. Investig, doi:10.1172/JCI108762
Kostoglou-Athanassiou, Athanassiou, Lyraki, Raftakis, Antoniadis, Vitamin D and rheumatoid arthritis, Ther. Adv. Endocrinol. Metab, doi:10.1177/2042018812471070
Kostoglou-Athanassiou, Pantazi, Kontogiannis, Kousouris, Mavropoulos et al., Vitamin D in acutely ill patients, J. Int. Med. Res, doi:10.1177/0300060518792783
Liu, Zheng, Lu, Lin, Shyu et al., Vitamin D and immune function in chronic kidney disease, Clin. Chim. Acta, doi:10.1016/j.cca.2015.08.011
Mahroum, Alghory, Kiyak, Alwani, Seida et al., Ferritin-from iron, through inflammation and autoimmunity, to COVID-19, J. Autoimmun, doi:10.1016/j.jaut.2021.102778
Mccullough, Bolisetty, Iron Homeostasis and Ferritin in Sepsis-Associated Kidney Injury, Nephron, doi:10.1159/000508857
Mcpadden, Warner, Young, Hurley, Pulk et al., Clinical characteristics and outcomes for 7,995 patients with SARS-CoV-2 infection, PLoS ONE, doi:10.1371/journal.pone.0243291
Mohammad, Mishra, Ashraf, Emerging Role of Vitamin D and its Associated Molecules in Pathways Related to Pathogenesis of Thrombosis, Biomolecules, doi:10.3390/biom9110649
Mohan, Cherian, Sharma, Exploring links between vitamin D deficiency and COVID-19, PLoS Pathog, doi:10.1371/journal.ppat.1008874
Nairz, Weiss, Iron in infection and immunity, Mol. Aspects Med, doi:10.1016/j.mam.2020.100864
Nappi, Nappi, Gambardella, Singh, Thromboembolic Disease and Cardiac Thrombotic Complication in COVID-19: A Systematic Review, Metabolites, doi:10.3390/metabo12100889
Nugroho, Wardhana, Maghfirah, Mulia, Rachmi et al., Relationship of D-dimer with severity and mortality in SARS-CoV-2 patients: A meta-analysis, Int. J. Lab. Hematol, doi:10.1111/ijlh.13336
Papagni, Pellegrino, Di Gennaro, Patti, Ricciardi et al., Impact of Vitamin D in Prophylaxis and Treatment in Tuberculosis Patients, Int. J. Mol. Sci, doi:10.3390/ijms23073860
Patel, Kaki, Potluri, Kahar, Khanna, A comprehensive review of SARS-CoV-2 vaccines: Pfizer, Moderna & Johnson & Johnson, Hum. Vaccin. Immunother, doi:10.1080/21645515.2021.2002083
Peng, Liu, Zheng, Lu, Hou et al., Immunological Aspects of SARS-CoV-2 Infection and the Putative Beneficial Role of Vitamin-D, Int. J. Mol. Sci, doi:10.3390/ijms22105251
Perkins, Joseph, Dittmer, Mackman, Cardiovascular Disease and Thrombosis in HIV Infection, Arterioscler. Thromb. Vasc. Biol, doi:10.1161/ATVBAHA.122.318232
Perricone, Bartoloni, Bursi, Cafaro, Guidelli et al., COVID-19 as part of the hyperferritinemic syndromes: The role of iron depletion therapy, Immunol. Res, doi:10.1007/s12026-020-09145-5
Pinheiro, Fabbri, Infante, Cytokine storm modulation in COVID-19: A proposed role for vitamin D and DPP-4 inhibitor combination therapy (VIDPP-4i), Immunotherapy, doi:10.2217/imt-2020-0349
Porta-Etessam, Yus, González García, Valcarcel, Barrado-Cuchillo et al., Brain inflammatory thrombogenic vasculopathy related with SARS-CoV-2 infection (Vasculopatía trombogénica inflamatoria del cerebro relacionada con la infección del SARS-CoV-2), Neurologia, doi:10.1016/j.nrl.2020.07.012
Pran, Baijoo, Slim, Viral infection-induced thrombosis, novel coronavirus, J. Vasc. Surg, doi:10.1016/j.jvs.2020.05.001
Qeadan, Tingey, Gu, Packard, Erdei et al., Prognostic Values of Serum Ferritin and D-Dimer Trajectory in Patients with COVID-19, Viruses, doi:10.3390/v13030419
Radujkovic, Hippchen, Tiwari-Heckler, Dreher, Boxberger et al., Vitamin D Deficiency and Outcome of COVID-19 Patients, Nutrients, doi:10.3390/nu12092757
Raisi-Estabragh, Martineau, Curtis, Moon, Darling et al., Vitamin D and coronavirus disease 2019 (COVID-19): Rapid evidence review, Aging Clin. Exp. Res, doi:10.1007/s40520-021-01894-z
Rastogi, Bhansali, Khare, Suri, Yaddanapudi et al., Short term, high-dose vitamin D supplementation for COVID-19 disease: A randomised, placebo-controlled, study (SHADE study), Postgrad. Med. J, doi:10.1136/postgradmedj-2020-139065
Rawat, Roy, Maitra, Shankar, Khanna et al., Vitamin D supplementation and COVID-19 treatment: A systematic review and meta-analysis, Diabetes Metab. Syndr, doi:10.1016/j.dsx.2021.102189
Rostami, Mansouritorghabeh, D-dimer level in COVID-19 infection: A systematic review, Expert. Rev. Hematol, doi:10.1080/17474086.2020.1831383
Ruscitti, Berardicurti, Di Benedetto, Cipriani, Iagnocco et al., Severe COVID-19, Another Piece in the Puzzle of the Hyperferritinemic Syndrome. An Immunomodulatory Perspective to Alleviate the Storm, Front. Immunol, doi:10.3389/fimmu.2020.01130
Sassi, Tamone, D'amelio, Vitamin, Nutrient, Hormone, and Immunomodulator, Nutrients, doi:10.3390/nu10111656
Savla, Prabhavalkar, Bhatt, Cytokine storm associated coagulation complications in COVID-19 patients: Pathogenesis and Management, Expert. Rev. Anti Infect. Ther, doi:10.1080/14787210.2021.1915129
Shapira, Agmon-Levin, Shoenfeld, Mycobacterium tuberculosis, autoimmunity, and vitamin D, Clin. Rev. Allergy Immunol, doi:10.1007/s12016-009-8150-1
Shivalkar, Pingali, Verma, Singh, Singh et al., Outbreak of COVID-19: A Detailed Overview and Its Consequences, Adv. Exp. Med. Biol, doi:10.1007/978-3-030-85113-2_2
Speeckaert, Delanghe, Commentary: Vitamin D Status in Relation to the Clinical Outcome of Hospitalized COVID-19 Patients, Front. Med, doi:10.3389/fmed.2022.922820
Stang, Mitchell, Fibrinogen, None, Methods Mol. Biol, doi:10.1007/978-1-62703-339-8_14
Takashita, Kinoshita, Yamayoshi, Sakai-Tagawa, Fujisaki et al., Efficacy of Antiviral Agents against the SARS-CoV-2 Omicron Subvariant BA.2, N. Engl. J. Med, doi:10.1056/NEJMc2201933
Tao, Tzou, Nouhin, Bonilla, Jagannathan et al., SARS-CoV-2 Antiviral Therapy, Clin. Microbiol. Rev, doi:10.1128/CMR.00109-21
Terpos, Ntanasis-Stathopoulos, Elalamy, Kastritis, Sergentanis et al., Hematological findings and complications of COVID-19, Am. J. Hematol, doi:10.1002/ajh.25829
Tiwari, Phatak, Sharma, Agarwal, COVID-19 and thrombotic microangiopathies, Thromb. Res, doi:10.1016/j.thromres.2021.04.012
Tomazini, Maia, Cavalcanti, Berwanger, Rosa et al., Effect of Dexamethasone on Days Alive and Ventilator-Free in Patients With Moderate or Severe Acute Respiratory Distress Syndrome and COVID-19: The CoDEX Randomized Clinical Trial, JAMA, doi:10.1001/jama.2020.17021
Torres, Casado, Vigón, Rodríguez-Mora, Mateos et al., Changes in the immune response against SARS-CoV-2 in individuals with severe COVID-19 treated with high dose of vitamin D, Biomed. Pharmacother, doi:10.1016/j.biopha.2022.112965
Tsai, Lai, Lin, Luo, Lin et al., Clinical manifestation and disease progression in COVID-19 infection, J. Chin. Med. Assoc, doi:10.1097/JCMA.0000000000000463
Volfovitch, Tsur, Gurevitch, Novick, Rabinowitz et al., The intercorrelations between blood levels of ferritin, sCD163, and IL-18 in COVID-19 patients and their association to prognosis, Immunol. Res, doi:10.1007/s12026-022-09312-w
Waldron, Ashby, Cornes, Bechervaise, Razavi et al., A negative acute phase reactant, J. Clin. Pathol, doi:10.1136/jclinpath-2012-201301
Wu, He, Low Vitamin D Levels Are Associated With the Development of Deep Venous Thromboembolic Events in Patients With Ischemic Stroke, Clin. Appl. Thromb. Hemost, doi:10.1177/1076029618786574
Xu, Baylink, Chen, Reeves, Xiao et al., The importance of vitamin d metabolism as a potential prophylactic, immunoregulatory and neuroprotective treatment for COVID-19, J. Transl. Med, doi:10.1186/s12967-020-02488-5
Xu, Yang, Chen, Luo, Zhang et al., Vitamin D alleviates lipopolysaccharide-induced acute lung injury via regulation of the renin-angiotensin system, Mol. Med. Rep, doi:10.3892/mmr.2017.7546
Yang, Gui, Gao, Ke, Xiong, Clinical progression and changes of chest CT findings among asymptomatic and pre-symptomatic patients with SARS-CoV-2 infection in Wuhan, China, Expert. Rev. Respir. Med, doi:10.1080/17476348.2021.1840358
Zhu, Kuznia, Boakye, Schöttker, Brenner, Vitamin D-Binding Protein, Bioavailable, and Free 25(OH)D, and Mortality: A Systematic Review and Meta-Analysis, Nutrients, doi:10.3390/nu14193894
DOI record:
{
"DOI": "10.3390/life14020210",
"ISSN": [
"2075-1729"
],
"URL": "http://dx.doi.org/10.3390/life14020210",
"abstract": "<jats:p>The SARS-CoV-2 virus may cause severe infection, which is associated with diverse clinical manifestations. Vitamin D has immunomodulating properties and may enhance the body’s defense system against invading pathogenic organisms. The aim was to assess 25(OH)D3 levels in patients hospitalized for severe infection from the SARS-CoV-2 virus and explore the relationship between 25(OH)D3 and outcomes. In a group of 88 patients hospitalized for severe infection from the SARS-CoV-2 virus and a control group matched for age and sex, the levels of 25(OH)D3 were analyzed. Levels of 25(OH)D3 were 17.36 ± 8.80 ng/mL (mean ± SD) compared with 24.34 ± 10.34 ng/mL in patients with severe SARS-CoV-2 infection and the control group, respectively, p < 0.001 (Student’s t-test). 25(OH)D3 levels were significantly related to outcomes, i.e., survival as opposed to non-survival, as more patients with 25(OH)D3 deficiency (0–10 ng/mL) and insufficiency (10–20 ng/mL) had a fatal outcome as compared with those with vitamin D sufficiency (p < 0.001, chi-square test, p < 0.001, Fisher’s exact test). Levels of 25(OH)D3 were inversely related to C-reactive protein (CRP), ferritin, d-dimer, and fibrinogen levels (p < 0.001, linear regression analysis, beta coefficient of variation, −0.176, −0.160, −0.178, and −0.158, respectively). Vitamin D deficiency observed in severe SARS-CoV-2 infection was related to disease outcomes.</jats:p>",
"alternative-id": [
"life14020210"
],
"author": [
{
"affiliation": [
{
"name": "COVID-19 Department, Asclepeion Hospital, Voula, GR16673 Athens, Greece"
}
],
"family": "Athanassiou",
"given": "Lambros",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0002-2029-8372",
"affiliation": [
{
"name": "Department of Endocrinology, Asclepeion Hospital, Voula, GR16673 Athens, Greece"
}
],
"authenticated-orcid": false,
"family": "Kostoglou-Athanassiou",
"given": "Ifigenia",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "COVID-19 Department, Asclepeion Hospital, Voula, GR16673 Athens, Greece"
}
],
"family": "Nikolakopoulou",
"given": "Sofia",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "COVID-19 Department, Asclepeion Hospital, Voula, GR16673 Athens, Greece"
}
],
"family": "Konstantinou",
"given": "Alexandra",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Biochemistry, Asclepeion Hospital, Voula, GR16673 Athens, Greece"
}
],
"family": "Mascha",
"given": "Olga",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "COVID-19 Department, Asclepeion Hospital, Voula, GR16673 Athens, Greece"
}
],
"family": "Siarkos",
"given": "Evangelos",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "COVID-19 Department, Asclepeion Hospital, Voula, GR16673 Athens, Greece"
}
],
"family": "Samaras",
"given": "Charilaos",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-4370-7394",
"affiliation": [
{
"name": "Department of Rheumatology, St. Paul’s Hospital, GR55134 Thessaloniki, Greece"
}
],
"authenticated-orcid": false,
"family": "Athanassiou",
"given": "Panagiotis",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Zabludowicz Center for Autoimmune Diseases, Sheba Medical Center, Reichman University, Herzelya 4610101, Israel"
}
],
"family": "Shoenfeld",
"given": "Yehuda",
"sequence": "additional"
}
],
"container-title": "Life",
"container-title-short": "Life",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2024,
1,
31
]
],
"date-time": "2024-01-31T13:44:06Z",
"timestamp": 1706708646000
},
"deposited": {
"date-parts": [
[
2024,
1,
31
]
],
"date-time": "2024-01-31T15:04:42Z",
"timestamp": 1706713482000
},
"indexed": {
"date-parts": [
[
2024,
2,
1
]
],
"date-time": "2024-02-01T00:37:45Z",
"timestamp": 1706747865025
},
"is-referenced-by-count": 0,
"issue": "2",
"issued": {
"date-parts": [
[
2024,
1,
31
]
]
},
"journal-issue": {
"issue": "2",
"published-online": {
"date-parts": [
[
2024,
2
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2024,
1,
31
]
],
"date-time": "2024-01-31T00:00:00Z",
"timestamp": 1706659200000
}
}
],
"link": [
{
"URL": "https://www.mdpi.com/2075-1729/14/2/210/pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1968",
"original-title": [],
"page": "210",
"prefix": "10.3390",
"published": {
"date-parts": [
[
2024,
1,
31
]
]
},
"published-online": {
"date-parts": [
[
2024,
1,
31
]
]
},
"publisher": "MDPI AG",
"reference": [
{
"DOI": "10.3390/ijerph18126312",
"doi-asserted-by": "crossref",
"key": "ref_1",
"unstructured": "Farrag, M.A., Amer, H.M., Bhat, R., Hamed, M.E., Aziz, I.M., Mubarak, A., Dawoud, T.M., Almalki, S.G., Alghofaili, F., and Alnemare, A.K. (2021). SARS-CoV-2: An Overview of Virus Genetics, Transmission, and Immunopathogenesis. Int. J. Environ. Res. Public Health, 18."
},
{
"DOI": "10.1007/978-3-030-85113-2_2",
"article-title": "Outbreak of COVID-19: A Detailed Overview and Its Consequences",
"author": "Shivalkar",
"doi-asserted-by": "crossref",
"first-page": "23",
"journal-title": "Adv. Exp. Med. Biol.",
"key": "ref_2",
"volume": "1353",
"year": "2021"
},
{
"DOI": "10.1007/s12035-020-02074-2",
"article-title": "Therapeutic Strategies in the Development of Anti-viral Drugs and Vaccines Against SARS-CoV-2 Infection",
"author": "Bhatti",
"doi-asserted-by": "crossref",
"first-page": "4856",
"journal-title": "Mol. Neurobiol.",
"key": "ref_3",
"volume": "57",
"year": "2020"
},
{
"DOI": "10.3389/fpubh.2021.736665",
"article-title": "Vitamin D Status and SARS-CoV-2 Infection and COVID-19 Clinical Outcomes",
"author": "Chiodini",
"doi-asserted-by": "crossref",
"first-page": "736665",
"journal-title": "Front. Public Health",
"key": "ref_4",
"volume": "9",
"year": "2021"
},
{
"DOI": "10.1111/bcpt.13872",
"article-title": "Vitamin D and SARS-CoV-2",
"doi-asserted-by": "crossref",
"first-page": "6",
"journal-title": "Basic. Clin. Pharmacol. Toxicol.",
"key": "ref_5",
"volume": "133",
"year": "2023"
},
{
"DOI": "10.1371/journal.pone.0268396",
"doi-asserted-by": "crossref",
"key": "ref_6",
"unstructured": "D’Ecclesiis, O., Gavioli, C., Martinoli, C., Raimondi, S., Chiocca, S., Miccolo, C., Bossi, P., Cortinovis, D., Chiaradonna, F., and Palorini, R. (2022). Vitamin D and SARS-CoV2 infection, severity and mortality: A systematic review and meta-analysis. PLoS ONE, 17."
},
{
"DOI": "10.3389/fphar.2020.604579",
"article-title": "COVID-19 Disease and Vitamin D: A Mini-Review",
"author": "Boulkrane",
"doi-asserted-by": "crossref",
"first-page": "604579",
"journal-title": "Front. Pharmacol.",
"key": "ref_7",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.3390/nu12072097",
"doi-asserted-by": "crossref",
"key": "ref_8",
"unstructured": "Charoenngam, N., and Holick, M.F. (2020). Immunologic Effects of Vitamin D on Human Health and Disease. Nutrients, 12."
},
{
"DOI": "10.1016/j.jcot.2019.07.004",
"article-title": "Vitamin D for skeletal and non-skeletal health: What we should know",
"author": "Charoenngam",
"doi-asserted-by": "crossref",
"first-page": "1082",
"journal-title": "J. Clin. Orthop. Trauma",
"key": "ref_9",
"volume": "10",
"year": "2019"
},
{
"DOI": "10.1007/s12016-009-8150-1",
"article-title": "Mycobacterium tuberculosis, autoimmunity, and vitamin D",
"author": "Shapira",
"doi-asserted-by": "crossref",
"first-page": "169",
"journal-title": "Clin. Rev. Allergy Immunol.",
"key": "ref_10",
"volume": "38",
"year": "2010"
},
{
"DOI": "10.1371/journal.pntd.0006608",
"doi-asserted-by": "crossref",
"key": "ref_11",
"unstructured": "Kim, E.W., Teles, R.M.B., Haile, S., Liu, P.T., and Modlin, R.L. (2018). Vitamin D status contributes to the antimicrobial activity of macrophages against Mycobacterium leprae. PLoS Negl. Trop. Dis., 12."
},
{
"DOI": "10.20944/preprints202003.0235.v2",
"doi-asserted-by": "crossref",
"key": "ref_12",
"unstructured": "Grant, W.B., Lahore, H., McDonnell, S.L., Baggerly, C.A., French, C.B., Aliano, J.L., and Bhattoa, H.P. (2020). Evidence that Vitamin D Supplementation Could Reduce Risk of Influenza and COVID-19 Infections and Deaths. Nutrients, 12."
},
{
"DOI": "10.1007/s40520-020-01677-y",
"article-title": "Evidence for possible association of vitamin D status with cytokine storm and unregulated inflammation in COVID-19 patients",
"author": "Daneshkhah",
"doi-asserted-by": "crossref",
"first-page": "2141",
"journal-title": "Aging Clin. Exp. Res.",
"key": "ref_13",
"volume": "32",
"year": "2020"
},
{
"DOI": "10.2217/imt-2020-0349",
"article-title": "Cytokine storm modulation in COVID-19: A proposed role for vitamin D and DPP-4 inhibitor combination therapy (VIDPP-4i)",
"author": "Pinheiro",
"doi-asserted-by": "crossref",
"first-page": "753",
"journal-title": "Immunotherapy",
"key": "ref_14",
"volume": "13",
"year": "2021"
},
{
"DOI": "10.3390/nu10111656",
"doi-asserted-by": "crossref",
"key": "ref_15",
"unstructured": "Sassi, F., Tamone, C., and D’Amelio, P. (2018). Vitamin D: Nutrient, Hormone, and Immunomodulator. Nutrients, 10."
},
{
"DOI": "10.3389/fimmu.2020.590459",
"article-title": "A Network-Based Analysis Reveals the Mechanism Underlying Vitamin D in Suppressing Cytokine Storm and Virus in SARS-CoV-2 Infection",
"author": "Ahmed",
"doi-asserted-by": "crossref",
"first-page": "590459",
"journal-title": "Front. Immunol.",
"key": "ref_16",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.1016/j.biopha.2022.112965",
"doi-asserted-by": "crossref",
"key": "ref_17",
"unstructured": "Torres, M., Casado, G., Vigón, L., Rodríguez-Mora, S., Mateos, E., Ramos-Martín, F., López-Wolf, D., Sanz-Moreno, J., Ryan-Murua, P., and Taboada-Martínez, M.L. (2022). Changes in the immune response against SARS-CoV-2 in individuals with severe COVID-19 treated with high dose of vitamin D. Biomed. Pharmacother., 150."
},
{
"DOI": "10.1016/j.dsx.2021.102189",
"article-title": "Vitamin D supplementation and COVID-19 treatment: A systematic review and meta-analysis",
"author": "Rawat",
"doi-asserted-by": "crossref",
"first-page": "102189",
"journal-title": "Diabetes Metab. Syndr.",
"key": "ref_18",
"volume": "15",
"year": "2021"
},
{
"DOI": "10.3390/molecules25225346",
"doi-asserted-by": "crossref",
"key": "ref_19",
"unstructured": "Bae, M., and Kim, H. (2020). Mini-Review on the Roles of Vitamin C, Vitamin D, and Selenium in the Immune System against COVID-19. Molecules, 25."
},
{
"DOI": "10.1001/jama.2020.17021",
"article-title": "Effect of Dexamethasone on Days Alive and Ventilator-Free in Patients With Moderate or Severe Acute Respiratory Distress Syndrome and COVID-19: The CoDEX Randomized Clinical Trial",
"author": "Tomazini",
"doi-asserted-by": "crossref",
"first-page": "1307",
"journal-title": "JAMA",
"key": "ref_20",
"volume": "324",
"year": "2020"
},
{
"DOI": "10.1111/all.14595",
"article-title": "Dexamethasone, pro-resolving lipid mediators and resolution of inflammation in COVID-19",
"author": "Andreakos",
"doi-asserted-by": "crossref",
"first-page": "626",
"journal-title": "Allergy",
"key": "ref_21",
"volume": "76",
"year": "2021"
},
{
"DOI": "10.1111/all.14657",
"article-title": "Risk factors for severe and critically ill COVID-19 patients: A review",
"author": "Gao",
"doi-asserted-by": "crossref",
"first-page": "428",
"journal-title": "Allergy",
"key": "ref_22",
"volume": "76",
"year": "2021"
},
{
"DOI": "10.1371/journal.pone.0243291",
"doi-asserted-by": "crossref",
"key": "ref_23",
"unstructured": "McPadden, J., Warner, F., Young, H.P., Hurley, N.C., Pulk, R.A., Singh, A., Durant, T.J.S., Gong, G., Desai, N., and Haimovich, A. (2021). Clinical characteristics and outcomes for 7,995 patients with SARS-CoV-2 infection. PLoS ONE, 16."
},
{
"DOI": "10.1016/j.jvs.2020.05.001",
"article-title": "Viral infection-induced thrombosis, novel coronavirus",
"author": "Pran",
"doi-asserted-by": "crossref",
"first-page": "764",
"journal-title": "J. Vasc. Surg.",
"key": "ref_24",
"volume": "72",
"year": "2020"
},
{
"DOI": "10.1007/s00134-020-06062-x",
"article-title": "High risk of thrombosis in patients with severe SARS-CoV-2 infection: A multicenter prospective cohort study",
"author": "Helms",
"doi-asserted-by": "crossref",
"first-page": "1089",
"journal-title": "Intensive Care Med.",
"key": "ref_25",
"volume": "46",
"year": "2020"
},
{
"DOI": "10.1016/j.thromres.2021.04.012",
"article-title": "COVID-19 and thrombotic microangiopathies",
"author": "Tiwari",
"doi-asserted-by": "crossref",
"first-page": "191",
"journal-title": "Thromb. Res.",
"key": "ref_26",
"volume": "202",
"year": "2021"
},
{
"DOI": "10.5152/AnatolJCardiol.2021.475",
"article-title": "Thrombosis, an important piece in the COVID-19 puzzle: From pathophysiology to therapy",
"author": "Bobescu",
"doi-asserted-by": "crossref",
"first-page": "601",
"journal-title": "Anatol. J. Cardiol.",
"key": "ref_27",
"volume": "25",
"year": "2021"
},
{
"DOI": "10.1016/j.nrl.2020.07.012",
"article-title": "Brain inflammatory thrombogenic vasculopathy related with SARS-CoV-2 infection (Vasculopatía trombogénica inflamatoria del cerebro relacionada con la infección del SARS-CoV-2)",
"author": "Yus",
"doi-asserted-by": "crossref",
"first-page": "701",
"journal-title": "Neurologia",
"key": "ref_28",
"volume": "35",
"year": "2020"
},
{
"DOI": "10.3390/metabo12100889",
"doi-asserted-by": "crossref",
"key": "ref_29",
"unstructured": "Nappi, F., Nappi, P., Gambardella, I., and Avtaar Singh, S.S. (2022). Thromboembolic Disease and Cardiac Thrombotic Complication in COVID-19: A Systematic Review. Metabolites, 12."
},
{
"DOI": "10.1056/NEJMoa2015432",
"article-title": "Pulmonary Vascular Endothelialitis, Thrombosis, and Angiogenesis in COVID-19",
"author": "Ackermann",
"doi-asserted-by": "crossref",
"first-page": "120",
"journal-title": "N. Engl. J. Med.",
"key": "ref_30",
"volume": "383",
"year": "2020"
},
{
"DOI": "10.1002/ajh.25829",
"article-title": "Hematological findings and complications of COVID-19",
"author": "Terpos",
"doi-asserted-by": "crossref",
"first-page": "834",
"journal-title": "Am. J. Hematol.",
"key": "ref_31",
"volume": "95",
"year": "2020"
},
{
"DOI": "10.3390/v13030419",
"doi-asserted-by": "crossref",
"key": "ref_32",
"unstructured": "Qeadan, F., Tingey, B., Gu, L.Y., Packard, A.H., Erdei, E., and Saeed, A.I. (2021). Prognostic Values of Serum Ferritin and D-Dimer Trajectory in Patients with COVID-19. Viruses, 13."
},
{
"DOI": "10.1177/1076029618786574",
"article-title": "Low Vitamin D Levels Are Associated With the Development of Deep Venous Thromboembolic Events in Patients With Ischemic Stroke",
"author": "Wu",
"doi-asserted-by": "crossref",
"first-page": "69s",
"journal-title": "Clin. Appl. Thromb. Hemost.",
"key": "ref_33",
"volume": "24",
"year": "2018"
},
{
"DOI": "10.3390/biom9110649",
"doi-asserted-by": "crossref",
"key": "ref_34",
"unstructured": "Mohammad, S., Mishra, A., and Ashraf, M.Z. (2019). Emerging Role of Vitamin D and its Associated Molecules in Pathways Related to Pathogenesis of Thrombosis. Biomolecules, 9."
},
{
"DOI": "10.1016/S0891-5849(02)00842-0",
"article-title": "Ferritin, iron homeostasis, and oxidative damage",
"author": "Arosio",
"doi-asserted-by": "crossref",
"first-page": "457",
"journal-title": "Free Radic. Biol. Med.",
"key": "ref_35",
"volume": "33",
"year": "2002"
},
{
"DOI": "10.1159/000508857",
"article-title": "Iron Homeostasis and Ferritin in Sepsis-Associated Kidney Injury",
"author": "McCullough",
"doi-asserted-by": "crossref",
"first-page": "616",
"journal-title": "Nephron",
"key": "ref_36",
"volume": "144",
"year": "2020"
},
{
"DOI": "10.1016/j.mam.2020.100864",
"article-title": "Iron in infection and immunity",
"author": "Nairz",
"doi-asserted-by": "crossref",
"first-page": "100864",
"journal-title": "Mol. Aspects Med.",
"key": "ref_37",
"volume": "75",
"year": "2020"
},
{
"DOI": "10.1681/ASN.2013040355",
"article-title": "Suppression of iron-regulatory hepcidin by vitamin D",
"author": "Bacchetta",
"doi-asserted-by": "crossref",
"first-page": "564",
"journal-title": "J. Am. Soc. Nephrol.",
"key": "ref_38",
"volume": "25",
"year": "2014"
},
{
"DOI": "10.1002/jcla.23618",
"article-title": "Ferritin in the coronavirus disease 2019 (COVID-19): A systematic review and meta-analysis",
"author": "Cheng",
"doi-asserted-by": "crossref",
"first-page": "e23618",
"journal-title": "J. Clin. Lab. Anal.",
"key": "ref_39",
"volume": "34",
"year": "2020"
},
{
"DOI": "10.1016/j.jaut.2021.102778",
"article-title": "Ferritin-from iron, through inflammation and autoimmunity, to COVID-19",
"author": "Mahroum",
"doi-asserted-by": "crossref",
"first-page": "102778",
"journal-title": "J. Autoimmun.",
"key": "ref_40",
"volume": "126",
"year": "2022"
},
{
"DOI": "10.1373/clinchem.2011.172155",
"article-title": "State-of-the-art vitamin D assays: A comparison of automated immunoassays with liquid chromatography-tandem mass spectrometry methods",
"author": "Farrell",
"doi-asserted-by": "crossref",
"first-page": "531",
"journal-title": "Clin. Chem.",
"key": "ref_41",
"volume": "58",
"year": "2012"
},
{
"DOI": "10.1007/978-1-62703-339-8_14",
"article-title": "Fibrinogen",
"author": "Stang",
"doi-asserted-by": "crossref",
"first-page": "181",
"journal-title": "Methods Mol. Biol.",
"key": "ref_42",
"volume": "992",
"year": "2013"
},
{
"DOI": "10.1097/JCMA.0000000000000463",
"article-title": "Clinical manifestation and disease progression in COVID-19 infection",
"author": "Tsai",
"doi-asserted-by": "crossref",
"first-page": "3",
"journal-title": "J. Chin. Med. Assoc.",
"key": "ref_43",
"volume": "84",
"year": "2021"
},
{
"DOI": "10.1080/17476348.2021.1840358",
"article-title": "Clinical progression and changes of chest CT findings among asymptomatic and pre-symptomatic patients with SARS-CoV-2 infection in Wuhan, China",
"author": "Yang",
"doi-asserted-by": "crossref",
"first-page": "411",
"journal-title": "Expert. Rev. Respir. Med.",
"key": "ref_44",
"volume": "15",
"year": "2021"
},
{
"DOI": "10.1172/jci.insight.149187",
"article-title": "SARS-CoV-2 vaccines: A triumph of science and collaboration",
"author": "Golob",
"doi-asserted-by": "crossref",
"first-page": "e149187",
"journal-title": "JCI Insight",
"key": "ref_45",
"volume": "6",
"year": "2021"
},
{
"DOI": "10.1080/21645515.2021.2002083",
"article-title": "A comprehensive review of SARS-CoV-2 vaccines: Pfizer, Moderna & Johnson & Johnson",
"author": "Patel",
"doi-asserted-by": "crossref",
"first-page": "2002083",
"journal-title": "Hum. Vaccin. Immunother.",
"key": "ref_46",
"volume": "18",
"year": "2022"
},
{
"DOI": "10.1128/CMR.00109-21",
"doi-asserted-by": "crossref",
"key": "ref_47",
"unstructured": "Tao, K., Tzou, P.L., Nouhin, J., Bonilla, H., Jagannathan, P., and Shafer, R.W. (2021). SARS-CoV-2 Antiviral Therapy. Clin. Microbiol. Rev., 34."
},
{
"DOI": "10.1056/NEJMc2214302",
"article-title": "Efficacy of Antiviral Agents against Omicron Subvariants BQ.1.1 and XBB",
"author": "Imai",
"doi-asserted-by": "crossref",
"first-page": "89",
"journal-title": "N. Engl. J. Med.",
"key": "ref_48",
"volume": "388",
"year": "2023"
},
{
"DOI": "10.1056/NEJMc2201933",
"article-title": "Efficacy of Antiviral Agents against the SARS-CoV-2 Omicron Subvariant BA.2",
"author": "Takashita",
"doi-asserted-by": "crossref",
"first-page": "1475",
"journal-title": "N. Engl. J. Med.",
"key": "ref_49",
"volume": "386",
"year": "2022"
},
{
"DOI": "10.1371/journal.ppat.1008874",
"doi-asserted-by": "crossref",
"key": "ref_50",
"unstructured": "Mohan, M., Cherian, J.J., and Sharma, A. (2020). Exploring links between vitamin D deficiency and COVID-19. PLoS Pathog., 16."
},
{
"DOI": "10.1016/j.metabol.2021.154753",
"article-title": "The link between COVID-19 and VItamin D (VIVID): A systematic review and meta-analysis",
"author": "Bassatne",
"doi-asserted-by": "crossref",
"first-page": "154753",
"journal-title": "Metabolism",
"key": "ref_51",
"volume": "119",
"year": "2021"
},
{
"DOI": "10.3390/ijms23137368",
"doi-asserted-by": "crossref",
"key": "ref_52",
"unstructured": "Hsieh, M.C., Hsiao, P.J., Liao, M.T., Hou, Y.C., Chang, Y.C., Chiang, W.F., Wu, K.L., Chan, J.S., and Lu, K.C. (2022). The Role of Vitamin D in SARS-CoV-2 Infection and Acute Kidney Injury. Int. J. Mol. Sci., 23."
},
{
"DOI": "10.1016/j.inat.2021.101441",
"article-title": "Vitamin D and its’ role in Parkinson’s disease patients with SARS-CoV-2 infection. A review article",
"author": "Azzam",
"doi-asserted-by": "crossref",
"first-page": "101441",
"journal-title": "Interdiscip. Neurosurg.",
"key": "ref_53",
"volume": "27",
"year": "2022"
},
{
"DOI": "10.3390/nu12092757",
"doi-asserted-by": "crossref",
"key": "ref_54",
"unstructured": "Radujkovic, A., Hippchen, T., Tiwari-Heckler, S., Dreher, S., Boxberger, M., and Merle, U. (2020). Vitamin D Deficiency and Outcome of COVID-19 Patients. Nutrients, 12."
},
{
"DOI": "10.3390/nu13051714",
"doi-asserted-by": "crossref",
"key": "ref_55",
"unstructured": "AlSafar, H., Grant, W.B., Hijazi, R., Uddin, M., Alkaabi, N., Tay, G., Mahboub, B., and Al Anouti, F. (2021). COVID-19 Disease Severity and Death in Relation to Vitamin D Status among SARS-CoV-2-Positive UAE Residents. Nutrients, 13."
},
{
"DOI": "10.32394/rpzh.2022.0191",
"article-title": "Vitamin D in SARS-CoV-2 infection",
"author": "Decyk",
"doi-asserted-by": "crossref",
"first-page": "5",
"journal-title": "Rocz. Panstw. Zakl. Hig.",
"key": "ref_56",
"volume": "73",
"year": "2022"
},
{
"DOI": "10.1002/cbf.3597",
"article-title": "Is there a link between vitamin D status, SARS-CoV-2 infection risk and COVID-19 severity?",
"author": "Ferrari",
"doi-asserted-by": "crossref",
"first-page": "35",
"journal-title": "Cell Biochem. Funct.",
"key": "ref_57",
"volume": "39",
"year": "2021"
},
{
"DOI": "10.1080/00325481.2021.2017647",
"article-title": "Vitamin D and COVID-19: Where are we now?",
"doi-asserted-by": "crossref",
"first-page": "195",
"journal-title": "Postgrad. Med.",
"key": "ref_58",
"volume": "135",
"year": "2023"
},
{
"DOI": "10.3390/ijms22105251",
"doi-asserted-by": "crossref",
"key": "ref_59",
"unstructured": "Peng, M.Y., Liu, W.C., Zheng, J.Q., Lu, C.L., Hou, Y.C., Zheng, C.M., Song, J.Y., Lu, K.C., and Chao, Y.C. (2021). Immunological Aspects of SARS-CoV-2 Infection and the Putative Beneficial Role of Vitamin-D. Int. J. Mol. Sci., 22."
},
{
"DOI": "10.1016/j.ijid.2021.02.048",
"article-title": "Mycobacterium leprae-helminth co-infections and vitamin D deficiency as potential risk factors for leprosy: A case-control study in south-eastern Brazil",
"author": "Dennison",
"doi-asserted-by": "crossref",
"first-page": "261",
"journal-title": "Int. J. Infect. Dis.",
"key": "ref_60",
"volume": "105",
"year": "2021"
},
{
"DOI": "10.3390/ijms23073860",
"doi-asserted-by": "crossref",
"key": "ref_61",
"unstructured": "Papagni, R., Pellegrino, C., Di Gennaro, F., Patti, G., Ricciardi, A., Novara, R., Cotugno, S., Musso, M., Guido, G., and Ronga, L. (2022). Impact of Vitamin D in Prophylaxis and Treatment in Tuberculosis Patients. Int. J. Mol. Sci., 23."
},
{
"DOI": "10.1016/j.cca.2015.08.011",
"article-title": "Vitamin D and immune function in chronic kidney disease",
"author": "Liu",
"doi-asserted-by": "crossref",
"first-page": "135",
"journal-title": "Clin. Chim. Acta",
"key": "ref_62",
"volume": "450",
"year": "2015"
},
{
"DOI": "10.1007/s00281-017-0629-x",
"article-title": "Pathogenic human coronavirus infections: Causes and consequences of cytokine storm and immunopathology",
"author": "Channappanavar",
"doi-asserted-by": "crossref",
"first-page": "529",
"journal-title": "Semin. Immunopathol.",
"key": "ref_63",
"volume": "39",
"year": "2017"
},
{
"DOI": "10.3892/mmr.2017.7546",
"article-title": "Vitamin D alleviates lipopolysaccharide-induced acute lung injury via regulation of the renin-angiotensin system",
"author": "Xu",
"doi-asserted-by": "crossref",
"first-page": "7432",
"journal-title": "Mol. Med. Rep.",
"key": "ref_64",
"volume": "16",
"year": "2017"
},
{
"DOI": "10.1186/s12967-020-02488-5",
"article-title": "The importance of vitamin d metabolism as a potential prophylactic, immunoregulatory and neuroprotective treatment for COVID-19",
"author": "Xu",
"doi-asserted-by": "crossref",
"first-page": "322",
"journal-title": "J. Transl. Med.",
"key": "ref_65",
"volume": "18",
"year": "2020"
},
{
"DOI": "10.1007/s40520-021-01894-z",
"article-title": "Vitamin D and coronavirus disease 2019 (COVID-19): Rapid evidence review",
"author": "Martineau",
"doi-asserted-by": "crossref",
"first-page": "2031",
"journal-title": "Aging Clin. Exp. Res.",
"key": "ref_66",
"volume": "33",
"year": "2021"
},
{
"DOI": "10.1136/jclinpath-2012-201301",
"article-title": "Vitamin D: A negative acute phase reactant",
"author": "Waldron",
"doi-asserted-by": "crossref",
"first-page": "620",
"journal-title": "J. Clin. Pathol.",
"key": "ref_67",
"volume": "66",
"year": "2013"
},
{
"DOI": "10.1172/JCI108762",
"article-title": "Intestinal calcium absorption in exogenous hypercortisonism. Role of 25-hydroxyvitamin D and corticosteroid dose",
"author": "Klein",
"doi-asserted-by": "crossref",
"first-page": "253",
"journal-title": "J. Clin. Investig.",
"key": "ref_68",
"volume": "60",
"year": "1977"
},
{
"DOI": "10.3390/nu14193894",
"doi-asserted-by": "crossref",
"key": "ref_69",
"unstructured": "Zhu, A., Kuznia, S., Boakye, D., Schöttker, B., and Brenner, H. (2022). Vitamin D-Binding Protein, Bioavailable, and Free 25(OH)D, and Mortality: A Systematic Review and Meta-Analysis. Nutrients, 14."
},
{
"DOI": "10.3389/fmed.2022.922820",
"article-title": "Commentary: Vitamin D Status in Relation to the Clinical Outcome of Hospitalized COVID-19 Patients",
"author": "Speeckaert",
"doi-asserted-by": "crossref",
"first-page": "922820",
"journal-title": "Front. Med.",
"key": "ref_70",
"volume": "9",
"year": "2022"
},
{
"DOI": "10.1002/jmv.26409",
"article-title": "The role of DBP gene polymorphisms in the prevalence of new coronavirus disease 2019 infection and mortality rate",
"author": "Hekim",
"doi-asserted-by": "crossref",
"first-page": "1409",
"journal-title": "J. Med. Virol.",
"key": "ref_71",
"volume": "93",
"year": "2021"
},
{
"DOI": "10.1186/s13063-020-04928-5",
"article-title": "COvid-19 and high-dose VITamin D supplementation TRIAL in high-risk older patients (COVIT-TRIAL): Study protocol for a randomized controlled trial",
"author": "Annweiler",
"doi-asserted-by": "crossref",
"first-page": "1031",
"journal-title": "Trials",
"key": "ref_72",
"volume": "21",
"year": "2020"
},
{
"DOI": "10.1371/journal.pmed.1003999",
"doi-asserted-by": "crossref",
"key": "ref_73",
"unstructured": "Annweiler, C., Beaudenon, M., Gautier, J., Gonsard, J., Boucher, S., Chapelet, G., Darsonval, A., Fougère, B., Guérin, O., and Houvet, M. (2022). High-dose versus standard-dose vitamin D supplementation in older adults with COVID-19 (COVIT-TRIAL): A multicenter, open-label, randomized controlled superiority trial. PLoS Med., 19."
},
{
"DOI": "10.1007/s11154-021-09693-7",
"article-title": "Vitamin D: Dosing, levels, form, and route of administration: Does one approach fit all?",
"author": "Bilezikian",
"doi-asserted-by": "crossref",
"first-page": "1201",
"journal-title": "Rev. Endocr. Metab. Disord.",
"key": "ref_74",
"volume": "22",
"year": "2021"
},
{
"DOI": "10.1177/0300060518792783",
"article-title": "Vitamin D in acutely ill patients",
"author": "Pantazi",
"doi-asserted-by": "crossref",
"first-page": "4246",
"journal-title": "J. Int. Med. Res.",
"key": "ref_75",
"volume": "46",
"year": "2018"
},
{
"DOI": "10.1177/2042018812471070",
"article-title": "Vitamin D and rheumatoid arthritis",
"author": "Athanassiou",
"doi-asserted-by": "crossref",
"first-page": "181",
"journal-title": "Ther. Adv. Endocrinol. Metab.",
"key": "ref_76",
"volume": "3",
"year": "2012"
},
{
"DOI": "10.3949/ccjm.90a.22048",
"article-title": "The constellation of vitamin D, the acute-phase response, and inflammation",
"author": "Antonelli",
"doi-asserted-by": "crossref",
"first-page": "85",
"journal-title": "Cleve. Clin. J. Med.",
"key": "ref_77",
"volume": "90",
"year": "2023"
},
{
"DOI": "10.1007/s12026-020-09145-5",
"article-title": "COVID-19 as part of the hyperferritinemic syndromes: The role of iron depletion therapy",
"author": "Perricone",
"doi-asserted-by": "crossref",
"first-page": "213",
"journal-title": "Immunol. Res.",
"key": "ref_78",
"volume": "68",
"year": "2020"
},
{
"DOI": "10.3389/fimmu.2020.01130",
"article-title": "Severe COVID-19, Another Piece in the Puzzle of the Hyperferritinemic Syndrome. An Immunomodulatory Perspective to Alleviate the Storm",
"author": "Ruscitti",
"doi-asserted-by": "crossref",
"first-page": "1130",
"journal-title": "Front. Immunol.",
"key": "ref_79",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.1097/PCC.0000000000000896",
"article-title": "High-Volume Hemofiltration in Critically Ill Patients With Secondary Hemophagocytic Lymphohistiocytosis/Macrophage Activation Syndrome: A Prospective Study in the PICU",
"author": "Cui",
"doi-asserted-by": "crossref",
"first-page": "e437",
"journal-title": "Pediatr. Crit. Care Med.",
"key": "ref_80",
"volume": "17",
"year": "2016"
},
{
"DOI": "10.1007/s12026-022-09312-w",
"article-title": "The intercorrelations between blood levels of ferritin, sCD163, and IL-18 in COVID-19 patients and their association to prognosis",
"author": "Volfovitch",
"doi-asserted-by": "crossref",
"first-page": "817",
"journal-title": "Immunol. Res.",
"key": "ref_81",
"volume": "70",
"year": "2022"
},
{
"DOI": "10.1161/ATVBAHA.122.318232",
"article-title": "Cardiovascular Disease and Thrombosis in HIV Infection",
"author": "Perkins",
"doi-asserted-by": "crossref",
"first-page": "175",
"journal-title": "Arterioscler. Thromb. Vasc. Biol.",
"key": "ref_82",
"volume": "43",
"year": "2023"
},
{
"DOI": "10.1016/j.tcm.2020.12.004",
"article-title": "COVID-19 and thrombosis: From bench to bedside",
"author": "Ali",
"doi-asserted-by": "crossref",
"first-page": "143",
"journal-title": "Trends Cardiovasc. Med.",
"key": "ref_83",
"volume": "31",
"year": "2021"
},
{
"DOI": "10.1080/14787210.2021.1915129",
"article-title": "Cytokine storm associated coagulation complications in COVID-19 patients: Pathogenesis and Management",
"author": "Savla",
"doi-asserted-by": "crossref",
"first-page": "1397",
"journal-title": "Expert. Rev. Anti Infect. Ther.",
"key": "ref_84",
"volume": "19",
"year": "2021"
},
{
"DOI": "10.1080/17474086.2020.1831383",
"article-title": "D-dimer level in COVID-19 infection: A systematic review",
"author": "Rostami",
"doi-asserted-by": "crossref",
"first-page": "1265",
"journal-title": "Expert. Rev. Hematol.",
"key": "ref_85",
"volume": "13",
"year": "2020"
},
{
"DOI": "10.1111/ijlh.13336",
"article-title": "Relationship of D-dimer with severity and mortality in SARS-CoV-2 patients: A meta-analysis",
"author": "Nugroho",
"doi-asserted-by": "crossref",
"first-page": "110",
"journal-title": "Int. J. Lab. Hematol.",
"key": "ref_86",
"volume": "43",
"year": "2021"
},
{
"DOI": "10.1136/postgradmedj-2020-139065",
"article-title": "Short term, high-dose vitamin D supplementation for COVID-19 disease: A randomised, placebo-controlled, study (SHADE study)",
"author": "Rastogi",
"doi-asserted-by": "crossref",
"first-page": "87",
"journal-title": "Postgrad. Med. J.",
"key": "ref_87",
"volume": "98",
"year": "2022"
},
{
"DOI": "10.3390/jcdd9010027",
"doi-asserted-by": "crossref",
"key": "ref_88",
"unstructured": "Cimmino, G., Conte, S., Morello, M., Pellegrino, G., Marra, L., Morello, A., Nicoletti, G., De Rosa, G., Golino, P., and Cirillo, P. (2022). Vitamin D Inhibits IL-6 Pro-Atherothrombotic Effects in Human Endothelial Cells: A Potential Mechanism for Protection against COVID-19 Infection?. J. Cardiovasc. Dev. Dis., 9."
}
],
"reference-count": 88,
"references-count": 88,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.mdpi.com/2075-1729/14/2/210"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Paleontology",
"Space and Planetary Science",
"General Biochemistry, Genetics and Molecular Biology",
"Ecology, Evolution, Behavior and Systematics"
],
"subtitle": [],
"title": "Vitamin D Levels as a Marker of Severe SARS-CoV-2 Infection",
"type": "journal-article",
"volume": "14"
}
