Profile of patients diagnosed with COVID-19 infection: a single-center retrospective study
et al., Health Problems of Civilization, doi:10.5114/hpc.2023.133494, Jan 2024
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 136 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 232 hospitalized COVID-19 patients in Poland showing vitamin D deficiency associated with longer hospitalization.
This is the 194th of 228 COVID-19 sufficiency studies for vitamin D, which collectively show higher levels reduce risk with p<0.0000000001.
|
hospitalization time, 33.3% lower, relative time 0.67, p < 0.001, high D levels (≥50nmol/L) 169, low D levels (<50nmol/L) 63.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Węgrzynek-Gallina et al., 31 Jan 2024, retrospective, Poland, peer-reviewed, mean age 66.5, 6 authors, study period November 2020 - June 2021.
Contact: ajarosinska@sum.edu.pl.
PROFILE OF PATIENTS DIAGNOSED WITH COVID-19 INFECTION: A SINGLE-CENTER RETROSPECTIVE STUDY
Health Problems of Civilization, doi:10.5114/hpc.2023.133494
Background. The purpose of this study was to examine the profile of COVID-19 patients hospitalized at the Department of Internal, Autoimmune and Metabolic Diseases of Central Clinical Hospital of the Medical University of Silesia in Katowice.
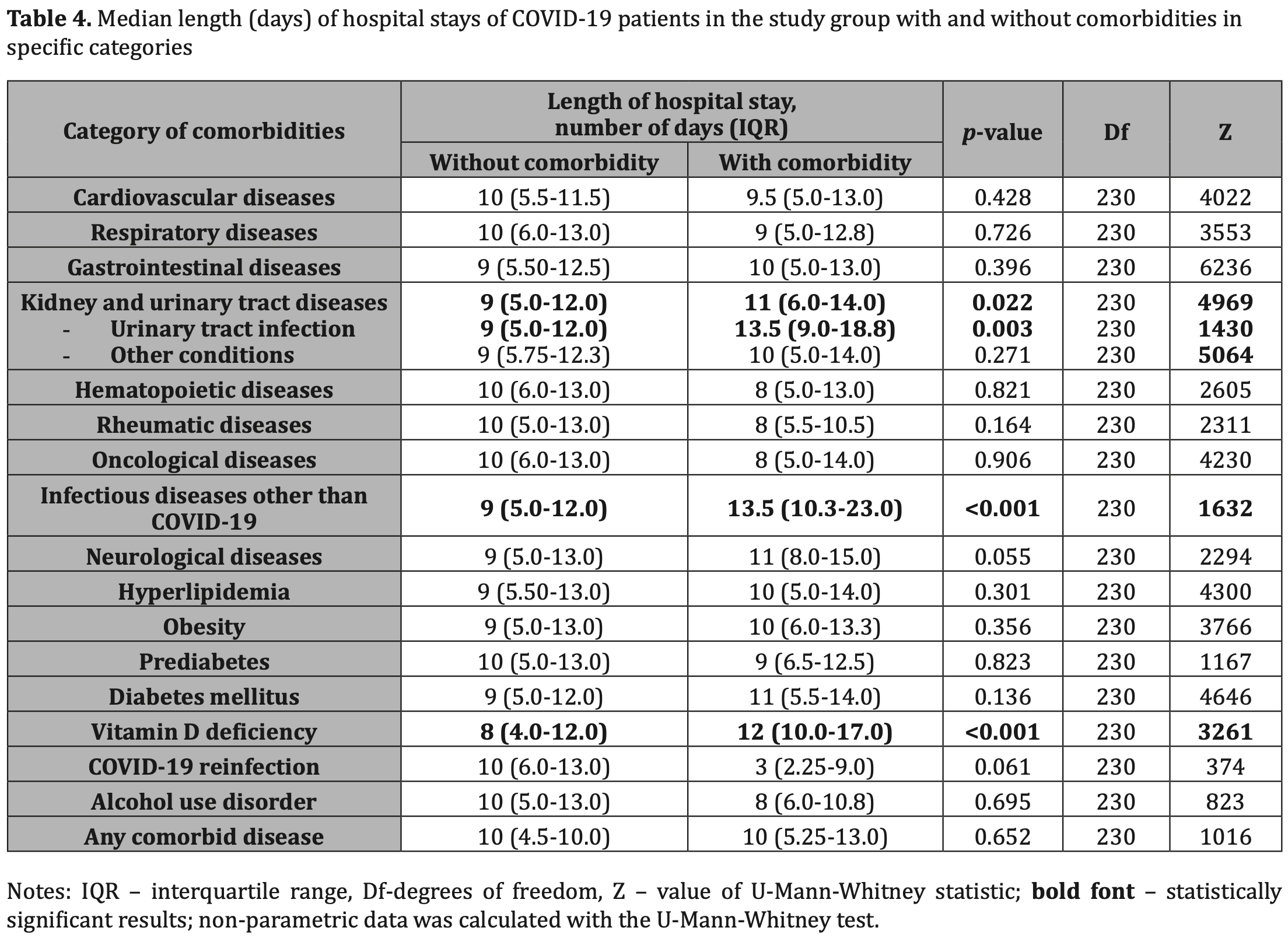
Material and methods. A retrospective analysis included all patients admitted to COVID-19 Internal Medicine Ward from November 2020 to June 2021. Collected data embraced: gender, age, date of admission, length of hospital stays, the mode of admission, main diagnoses and comorbidities, discharge mode from the hospital, and cause of death. Results. The study group comprised 232 patients (124 (53.4%) males) diagnosed with COVID-19, mean age of 66.5±14.7 (24-96) years old. The number of coexisting cardiovascular diseases, diagnosis of chronic heart failure, and ischemic heart disease were statistically significantly associated with mortality of patients. The average length of hospitalization was 9.96±6.35 (0-35) days. It was significantly longer among patients diagnosed with kidney and urinary tract diseases (11 (6.0-14.0) vs. 9 (5.0-15.0) days, p=0.022), especially with urinary tract infection (13.5 (9.0-18.8) vs. 9 (5.0-12.0) days, p=0.003). Coexisting infections other than COVID-19 (9 (5.0-12.0) vs. 5 (10.3-23.0) days, p<0.001) and vitamin D deficiency (8 (4.0-12.0) vs. 12 (10.0-17.0) days, p<0.001) were also significant factors in prolonging hospital stay. Conclusions. Among hospitalized COVID-19 patients, cardiovascular diseases are significant factors associated with mortality. Coexisting infections and vitamin D deficiency may prolong the hospitalization.
Disclosures and acknowledgements The authors declare no conflicts of interest with respect to the research, authorship, and/or publication of this article. This research received no specific grant from any funding agency in the public, commercial, or notfor-profit sectors. Artificial intelligence (AI) was not used in the creation of the manuscript. The data presented in the study can be accessed via contact with the corresponding author.
References
Al-Hazmi, Role of duration of catheterization and length of hospital stay on the rate of catheter-related hospital-acquired urinary tract infections, Res Rep Urol, doi:10.2147/RRU.S75419
Bassatne, Basbous, Chakhtoura, El Zein, Rahme et al., The link between COVID-19 and vitamin D (VIVID): a systematic review and meta-analysis, Metabolism, doi:10.1016/j.metabol.2021.154753
Gold, Sehayek, Gabrielli, Zhang, Mccusker et al., COVID-19 and comorbidities: a systematic review and meta-analysis, Postgrad Med, doi:10.1080/00325481.2020.1786964
Jalandra, Babu, Dutt, Chauhan, Bhatia et al., Co-infections in hospitalized COVID-19 patients -a prospective observational study, Cureus, doi:10.7759/cureus.30608
Kanecki, Nitsch-Osuch, Goryński, Wojtyniak, Juszczyk et al., Hospitalizations for COVID-19 in Poland: a study based on data from a national hospital register, Pol Arch Intern Med, doi:10.20452/pamw.15946ProfileofpatientsdiagnosedwithCOVID-19
Kaya, Pamukçu, Yakar, The role of vitamin D deficiency on COVID-19: a systematic review and meta-analysis of observational studies, Epidemiol Health, doi:10.4178/epih.e2021074
Kowalska, Barański, Brożek, Kaleta-Pilarska, Zejda, COVID-19-related risk of in-hospital death in Silesia, Poland, Pol Arch Intern Med, doi:10.20452/pamw.15893
Liu, Yang, Liao, Lin, Huang, Risk factors for COVID-19 progression and mortality in hospitalized patients without pre-existing comorbidities, J Infect Public Health, doi:10.1016/j.jiph.2021.11.012
Maslennikov, Ivashkin, Ufimtseva, Poluektova, Ulyanin, Clostridioides difficile co-infection in patients with COVID-19, Future Microbiol, doi:10.2217/fmb-2021-0145
Nowak, Szymański, Pańkowski, Szarowska, Życińska et al., Clinical characteristics and short-term outcomes of patients with coronavirus disease 2019: a retrospective single-center experience of a designated hospital in Poland, Pol Arch Intern Med, doi:10.20452/pamw.15361
Orsini, Sacha, Han, Wang, Duggal et al., Risk factors associated with development of coinfection in critically ill patients with COVID-19, Acute Crit Care, doi:10.4266/acc.2022.00136
Płudowski, Ducki, Konstantynowicz, Jaworski, Vitamin D status in Poland, Pol Arch Med Wewn, doi:10.20452/pamw.3479
Rey, Caro-Codón, Rosillo, Iniesta, Castrejón-Castrejón et al., Heart failure in COVID-19 patients: prevalence, incidence and prognostic implications, Eur J Heart Fail, doi:10.1002/ejhf.1990ProfileofpatientsdiagnosedwithCOVID-19
Rosiello, Pietrantonio, Berardino, Castelli, Ciamei et al., Is COVID-19 introducing a new model of internal medicine ward?, European Journal of Public Health, doi:10.1093/eurpub/ckab165.035
Schulze, Bayer, Changes in symptoms experienced by SARS-CoV-2-infected individuals-from the first wave to the omicron variant, Front. Virol, doi:10.3389/fviro.2022.880707
Szarpak, Pruc, Nadolny, Smereka, Ladny, Role of a field hospital in COVID-19 pandemic, Disaster Emerg Med J, doi:10.5603/DEMJ.a2020.0046
Tucker, COVID-19 hospitalization costs and outcomes in 2020 improved over time
Zhou, Yu, Du, Fan, Liu et al., Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study, Lancet, doi:10.1016/S0140-6736(20)30566-3
DOI record:
{
"DOI": "10.5114/hpc.2023.133494",
"ISSN": [
"2353-6942"
],
"URL": "http://dx.doi.org/10.5114/hpc.2023.133494",
"alternative-id": [
"133494"
],
"author": [
{
"affiliation": [],
"family": "Węgrzynek-Gallina",
"given": "Julia",
"sequence": "first"
},
{
"affiliation": [],
"family": "Pilśniak",
"given": "Joanna",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Pilśniak",
"given": "Aleksandra",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Jarosińska",
"given": "Agnieszka",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Pietrukaniec",
"given": "Marta",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Holecki",
"given": "Michał",
"sequence": "additional"
}
],
"container-title": "Health Problems of Civilization",
"container-title-short": "hpc",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2024,
1,
31
]
],
"date-time": "2024-01-31T08:12:01Z",
"timestamp": 1706688721000
},
"deposited": {
"date-parts": [
[
2024,
6,
11
]
],
"date-time": "2024-06-11T10:15:37Z",
"timestamp": 1718100937000
},
"indexed": {
"date-parts": [
[
2024,
6,
12
]
],
"date-time": "2024-06-12T00:24:05Z",
"timestamp": 1718151845168
},
"is-referenced-by-count": 0,
"issue": "2",
"issued": {
"date-parts": [
[
2024
]
]
},
"journal-issue": {
"issue": "2",
"published-print": {
"date-parts": [
[
2024
]
]
}
},
"link": [
{
"URL": "https://www.termedia.pl/doi_ft/10.5114/hpc.2023.133494",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "3061",
"original-title": [
"PROFIL PACJENTÓW Z INFEKCJĄ COVID-19: RETROSPEKTYWNE BADANIE JEDNOOŚRODKOWE"
],
"page": "180-193",
"prefix": "10.5114",
"published": {
"date-parts": [
[
2024
]
]
},
"published-print": {
"date-parts": [
[
2024
]
]
},
"publisher": "Termedia Sp. z.o.o.",
"reference-count": 0,
"references-count": 0,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.termedia.pl/doi/10.5114/hpc.2023.133494"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"title": "PROFILE OF PATIENTS DIAGNOSED WITH COVID-19 INFECTION: A SINGLE-CENTER RETROSPECTIVE STUDY",
"type": "journal-article",
"volume": "18"
}
