Clinical Progression and Outcome of Hospitalized Patients Infected with SARS-CoV-2 Omicron Variant in Shanghai, China
et al., Vaccines, doi:10.3390/vaccines10091409, Aug 2022
Retrospective 226 patients in China, showing faster viral clearance with paxlovid. Age range and severity differed between groups.
Resistance. Variants may be resistant to paxlovid1-8. Use may promote the emergence of variants that weaken host immunity and potentially contribute to long COVID9. Confounding by contraindication. Hoertel et al. find that over 50% of patients that died had a contraindication for the use of Paxlovid10. Retrospective studies that do not exclude contraindicated patients may significantly overestimate efficacy. Black box warning. The FDA notes that severe, life-threatening, and/or fatal adverse reactions due to drug interactions have been reported in patients treated with paxlovid11. Kidney and liver injury. Studies show significantly increased risk of acute kidney injury12 and liver injury13,14. Viral rebound. Studies show significantly increased risk of replication-competent viral rebound15-17.
Standard of Care (SOC) for COVID-19 in the study country,
China, is average with moderate efficacy for approved treatments18.
This study is excluded in the after exclusion results of meta-analysis:
significant unadjusted differences between groups.
|
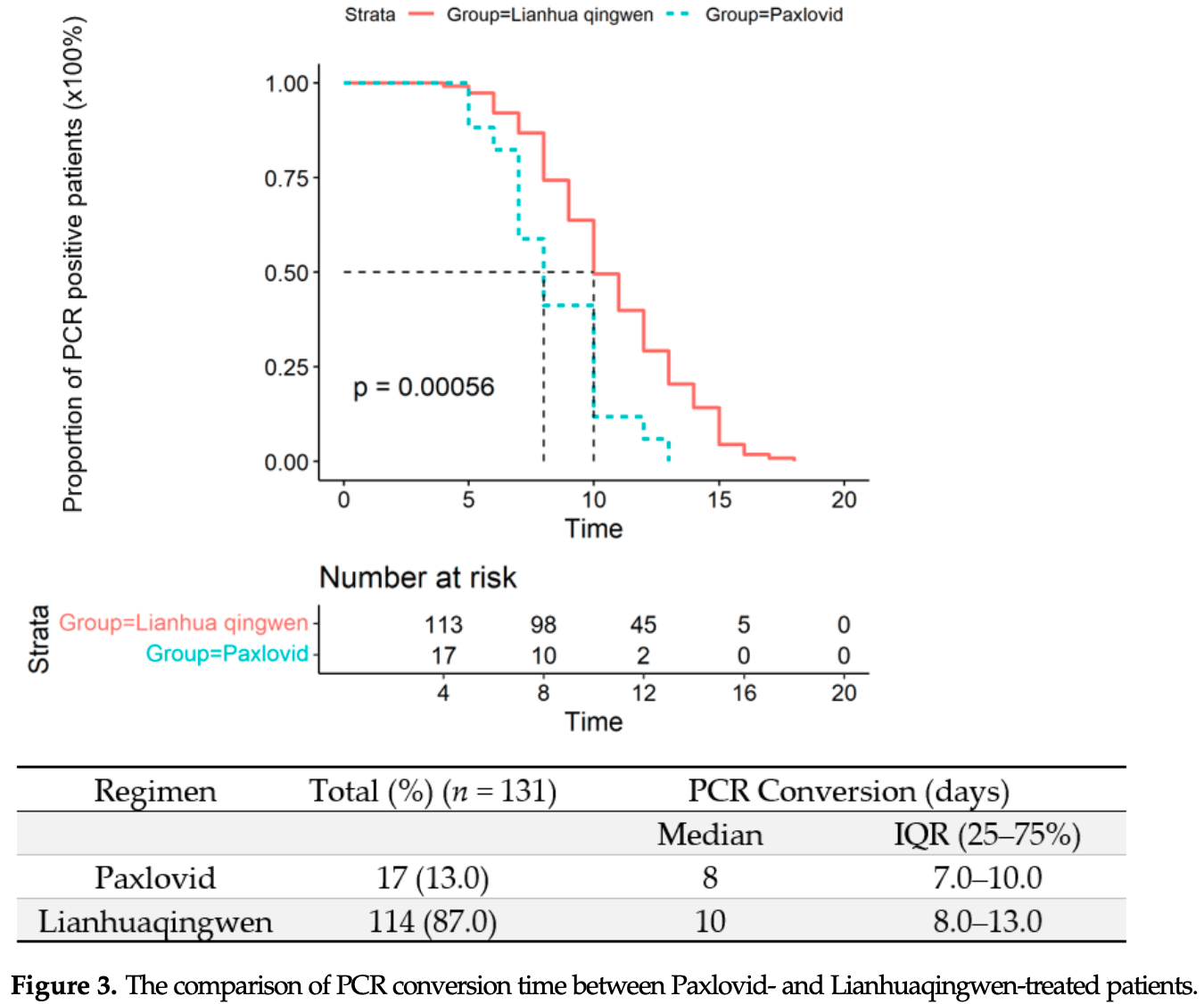
time to viral-, 20.0% lower, relative time 0.80, p < 0.001, treatment 17, control 114.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
1.
Zhou et al., Nirmatrelvir-resistant SARS-CoV-2 variants with high fitness in an infectious cell culture system, Science Advances, doi:10.1126/sciadv.add7197.
2.
Moghadasi et al., Rapid resistance profiling of SARS-CoV-2 protease inhibitors, npj Antimicrobials and Resistance, doi:10.1038/s44259-023-00009-0.
3.
Jochmans et al., The Substitutions L50F, E166A, and L167F in SARS-CoV-2 3CLpro Are Selected by a Protease Inhibitor In Vitro and Confer Resistance To Nirmatrelvir, mBio, doi:10.1128/mbio.02815-22.
4.
Lopez et al., SARS-CoV-2 Resistance to Small Molecule Inhibitors, Current Clinical Microbiology Reports, doi:10.1007/s40588-024-00229-6.
5.
Zvornicanin et al., Molecular Mechanisms of Drug Resistance and Compensation in SARS-CoV-2 Main Protease: The Interplay Between E166 and L50, bioRxiv, doi:10.1101/2025.01.24.634813.
6.
Vukovikj et al., Impact of SARS-CoV-2 variant mutations on susceptibility to monoclonal antibodies and antiviral drugs: a non-systematic review, April 2022 to October 2024, Eurosurveillance, doi:10.2807/1560-7917.ES.2025.30.10.2400252.
7.
Deschenes et al., Functional and structural characterization of treatment-emergent nirmatrelvir resistance mutations at low frequencies in the main protease (Mpro) reveals a unique evolutionary route for SARS-CoV-2 to gain resistance, The Journal of Infectious Diseases, doi:10.1093/infdis/jiaf294.
8.
Zhou (B) et al., SARS-CoV-2 Mpro inhibitor ensitrelvir: asymmetrical cross-resistance with nirmatrelvir and emerging resistance hotspots, Emerging Microbes & Infections, doi:10.1080/22221751.2025.2552716.
9.
Thomas et al., Nirmatrelvir-Resistant Mutations in SARS-CoV-2 Mpro Enhance Host Immune Evasion via Cleavage of NF-κB Essential Modulator, bioRxiv, doi:10.1101/2024.10.18.619137.
10.
Hoertel et al., Prevalence of Contraindications to Nirmatrelvir-Ritonavir Among Hospitalized Patients With COVID-19 at Risk for Progression to Severe Disease, JAMA Network Open, doi:10.1001/jamanetworkopen.2022.42140.
11.
FDA, Fact sheet for healthcare providers: emergency use authorization for paxlovid, www.fda.gov/media/155050/download.
12.
Kamo et al., Association of Antiviral Drugs for the Treatment of COVID-19 With Acute Renal Failure, In Vivo, doi:10.21873/invivo.13637.
13.
Wang et al., Development and validation of a nomogram to assess the occurrence of liver dysfunction in patients with COVID-19 pneumonia in the ICU, BMC Infectious Diseases, doi:10.1186/s12879-025-10684-1.
14.
Siby et al., Temporal Trends in Serious Adverse Events Associated with Oral Antivirals During the COVID-19 Pandemic: Insights from the FAERS Database (2020–2023), Open Forum Infectious Diseases, doi:10.1093/ofid/ofaf695.1825.
15.
Edelstein et al., SARS-CoV-2 virologic rebound with nirmatrelvir-ritonavir therapy, medRxiv, doi:10.1101/2023.06.23.23288598.
16.
Shah et al., SARS-CoV-2 infectious shedding and rebound among adults with and without oral antiviral use: two case-ascertained prospective household studies, The Lancet Microbe, doi:10.1016/j.lanmic.2025.101227.
Shao et al., 28 Aug 2022, retrospective, China, peer-reviewed, median age 52.0, 12 authors, study period 6 April, 2022 - 11 May, 2022, average treatment delay 3.0 days, this trial compares with another treatment - results may be better when compared to placebo.
Contact: huanggang@sumhs.edu.cn (corresponding author).
Clinical Progression and Outcome of Hospitalized Patients Infected with SARS-CoV-2 Omicron Variant in Shanghai, China
Vaccines, doi:10.3390/vaccines10091409
Background: Studies on the Omicron variant infection have generally been restricted to descriptions of its initial clinical and epidemiological characteristics. We investigated the timelinerelated progression and clinical outcome in hospitalized individuals with the Omicron variant. Methods: We conducted a retrospective, single-centered study including 226 laboratory-confirmed cases with the Omicron variant between 6 April and 11 May 2022 in Shanghai, China. The final date of follow-up was 30 May 2022. Results: Among 226 enrolled patients, the median age was 52 years, and 118 (52.2%) were female. The duration from onset of symptoms to hospitalization was 3 days (interquartile range (IQR): 2-4 days) for symptomatic patients. Cough occurred in 168 patients (74.3%). The median interval to negative reverse-transcriptase PCR tests of nasopharynx swab was 10 days ((IQR): 8-13 days). No radiographic progressions were found in 196 patients on the 7th day after onset of symptoms. The median duration of fever in all participants was 5 days (IQR: 4-6 days). The median PCR conversion time of Paxlovid-treated patients was 8 days (IQR: 7-10 days) compared with that of a traditional Chinese herb medicine lianhuaqingwen (10 days, IQR: 8-13 days) (p = 0.00056). Booster vaccination can significantly decrease the severity of Omicron infection when compared with unvaccinated patients (p = 0.009). In multivariate logistic analysis, erythrocyte sedimentation rate (ESR) (OR = 1.05) was independently related to the severity of the infection. Conclusions: The majority of clinical symptoms of Omicron infection were not severe. Early and aggressive administration of Paxlovid can significantly reduce the PCR conversion time. Booster vaccination should also be highly recommended in the population over 14 years old.
Factors Related to the Severity of the Infection To figure out factors that were associated with the severity of the disease, we compared clinical laboratory characters and vaccination status of asymptomatic (n = 4), mild (n = 180), and moderate (n = 41) patients. In univariate analysis, older age, comorbidity, lymphopenia, high levels of CRP, ESR, lactate, estimated glomerular filtration rate (e-GFR), low levels of albumin, and fewer vaccination doses are all associated with the severity of Omicron infection. In multivariate logistic analysis, ESR (OR = 1.05) was independently related to the severity of the infection (Table 3 ).
Discussion On 24 November 2021, the World Health Organization (WHO) announced a new variant of SARS-CoV-2 Omicron in South Africa, and 17 days later, the first case infected with Omicron in China was identified [15] . Recent investigations on the Omicron variant have described the epidemiologic characteristics, initial clinical, laboratory, and radiological findings [4, 6, 16] . To our knowledge, we are the first to describe the temporal clinical progression of Omicron variant infection to date. Our investigation has several distinguished features from current research. As one of the megacities and most important economic centers in China, the policy of "Dynamic zero" was implemented strictly in Shanghai. The whole city underwent completely lockdown during the pandemic outbreak since the end of March 2022 [17] . Under the policy of..
References
Abas, Marfuah, Idroes, Kusumawaty, Fatimawali, None
Anjos, Fiaccadori, Servian, Da Fonseca, Guilarde et al., SARS-CoV-2 loads in urine, sera and stool specimens in association with clinical features of COVID-19 patients, J. Clin. Virol. Plus, doi:10.1016/j.jcvp.2021.100059
Bennasrallah, Zemni, Dhouib, Sriha, Mezhoud et al., Factors associated with a prolonged negative conversion of viral RNA in patients with COVID-19, Int. J. Infect. Dis, doi:10.1016/j.ijid.2021.02.089
Butt, Dargham, Loka, Shaik, Chemaitelly et al., COVID-19 Disease Severity in Children Infected with the Omicron Variant, Clin. Infect. Dis, doi:10.1093/cid/ciac275
Cann, Fever: Could A Cardinal Sign of COVID-19 Infection Reduce Mortality?, Am. J. Med. Sci, doi:10.1016/j.amjms.2021.01.004
Chen, Qi, Liu, Ling, Qian et al., Clinical progression of patients with COVID-19 in Shanghai, China, J. Infect, doi:10.1016/j.jinf.2020.03.004
Graham, Daily briefing: Omicron struggles to infect the lungs, Nature, doi:10.1038/d41586-022-00039-0
Guan, Ni, Hu, Liang, Ou et al., Clinical Characteristics of Coronavirus Disease 2019 in China, N. Engl. J. Med, doi:10.1056/NEJMoa2002032
Gupta, SARS-CoV-2 Omicron spike mediated immune escape and tropism shift, Res. Sq, doi:10.21203/rs.3.rs-1191837/v1
He, Lau, Wu, Deng, Wang et al., Temporal dynamics in viral shedding and transmissibility of COVID-19, Nat. Med, doi:10.1038/s41591-020-0869-5
Huang, Zeng, Letter to the editor: Epidemiology of the SARS-CoV-2 variant Omicron BA.2-vigilance needed, Euro Surveill, doi:10.2807/1560-7917.ES.2022.27.13.2200254
Hui, Ho, Cheung, Ng, Ching et al., SARS-CoV-2 Omicron variant replication in human bronchus and lung ex vivo, Nature, doi:10.1038/s41586-022-04479-6
Kim, Lee, Choi, Um, Lee et al., Clinical Characteristics of 40 Patients Infected With the SARS-CoV-2 Omicron Variant in Korea, J. Korean Med. Sci, doi:10.3346/jkms.2022.37.e31
Kozlov, Omicron's feeble attack on the lungs could make it less dangerous, Nature, doi:10.1038/d41586-022-00007-8
Lee, Choe, Jeong, Kim, Kim et al., Importation and Transmission of SARS-CoV-2 B.1.1.529 (Omicron) Variant of Concern in Korea, J. Korean Med. Sci, doi:10.3346/jkms.2021.36.e346
Liang, Hui, Liu, Qiao, Li et al., Insights into forsythia honeysuckle (Lianhuaqingwen) capsules: A Chinese herbal medicine repurposed for COVID-19 pandemic, Phytomed. Plus, doi:10.1016/j.phyplu.2021.100027
Liu, Gao, Yuan, Yang, Shi et al., Efficacy and safety of herbal medicine (Lianhuaqingwen) for treating COVID-19: A systematic review and meta-analysis, Integr. Med. Res, doi:10.1016/j.imr.2020.100644
Martin, Dewitt, Russell, Sanchez-Pinto, Haendel et al., Acute Upper Airway Disease in Children With the Omicron (B.1.1.529) Variant of SARS-CoV-2-A Report from the US National COVID Cohort Collaborative, JAMA Pediatr, doi:10.1001/jamapediatrics.2022.1110
Maslo, Friedland, Toubkin, Laubscher, Akaloo et al., Characteristics and Outcomes of Hospitalized Patients in South Africa During the COVID-19 Omicron Wave Compared With Previous Waves, JAMA, doi:10.1001/jama.2021.24868
Mesfin, Chen, Bond, Lam, Cheung et al., Epidemiology of infections with SARS-CoV-2 Omicron BA.2 variant in Hong Kong, medRxiv, doi:10.1101/2022.04.07.22273595
Nhcotpsro, Notice on printing and distributing the COVID-19 Pneumonia Diagnosis and Treatment Plan (Ninth Trial Version
Park, Siyadatpanah, Alhumaydhi, Mahmud, Tallei, Can the SARS-CoV-2 Omicron Variant Confer Natural Immunity against COVID-19?, Molecules
Rossler, Riepler, Bante, Von Laer, Kimpel, SARS-CoV-2 Omicron Variant Neutralization in Serum from Vaccinated and Convalescent Persons, N. Engl. J. Med, doi:10.1056/NEJMc2119236
Runfeng, Yunlong, Jicheng, Weiqi, Qinhai et al., Lianhuaqingwen exerts anti-viral and anti-inflammatory activity against novel coronavirus (SARS-CoV-2), Pharmacol. Res, doi:10.1016/j.phrs.2020.104761
Shen, Li, Tu, Wu, Peng et al., Positive effects of Lianhuaqingwen granules in COVID-19 patients: A retrospective study of 248 cases, J. Ethnopharmacol, doi:10.1016/j.jep.2021.114220
Singhal, The Emergence of Omicron: Challenging Times Are Here Again!, Indian J. Pediatr, doi:10.1007/s12098-022-04077-4
Sun, Li, Huang, Shi, Xing et al., Case Report of China/Tianjin's First Novel Coronavirus Variant Omicron, Iran J. Immunol, doi:10.22034/IJI.2022.94050.2278
Team, -R, Omicron) Variant-United States, doi:10.15585/mmwr.mm7050e1
Thakur, Ratho, Omicron, A new SARS-CoV-2 variant of concern mounting worldwide fear, J. Med. Virol, doi:10.1002/jmv.27541
Torjesen, Covid-19: Peak of viral shedding is later with omicron variant, Japanese data suggest, BMJ, doi:10.1136/bmj.o89
Wang, Prather, Sznitman, Jimenez, Lakdawala et al., Airborne transmission of respiratory viruses, Science, doi:10.1126/science.abd9149
Wang, Yang, In the age of Omicron variant: Paxlovid raises new hopes of COVID-19 recovery, J. Med. Virol, doi:10.1002/jmv.27540
Widders, Broom, Broom, SARS-CoV-2: The viral shedding vs infectivity dilemma, Infect. Dis. Health
Wu, Guo, Tang, Hong, Zhou et al., Prolonged presence of SARS-CoV-2 viral RNA in faecal samples, Lancet Gastroenterol. Hepatol, doi:10.1016/S2468-1253(20)30083-2
Yan, Zhang, Chen, Jiang, Liu et al., Characteristics of Viral Shedding Time in SARS-CoV-2 Infections: A Systematic Review and Meta-Analysis, Front. Public Health
Yuan, Hou, Lin, Chen, Ren, How China responds to Omicron, J. Infect, doi:10.1016/j.jinf.2022.04.017
DOI record:
{
"DOI": "10.3390/vaccines10091409",
"ISSN": [
"2076-393X"
],
"URL": "http://dx.doi.org/10.3390/vaccines10091409",
"abstract": "<jats:p>Background: Studies on the Omicron variant infection have generally been restricted to descriptions of its initial clinical and epidemiological characteristics. We investigated the timeline-related progression and clinical outcome in hospitalized individuals with the Omicron variant. Methods: We conducted a retrospective, single-centered study including 226 laboratory-confirmed cases with the Omicron variant between 6 April and 11 May 2022 in Shanghai, China. The final date of follow-up was 30 May 2022. Results: Among 226 enrolled patients, the median age was 52 years, and 118 (52.2%) were female. The duration from onset of symptoms to hospitalization was 3 days (interquartile range (IQR): 2–4 days) for symptomatic patients. Cough occurred in 168 patients (74.3%). The median interval to negative reverse-transcriptase PCR tests of nasopharynx swab was 10 days ((IQR): 8–13 days). No radiographic progressions were found in 196 patients on the 7th day after onset of symptoms. The median duration of fever in all participants was 5 days (IQR: 4–6 days). The median PCR conversion time of Paxlovid-treated patients was 8 days (IQR: 7–10 days) compared with that of a traditional Chinese herb medicine lianhuaqingwen (10 days, IQR: 8–13 days) (p = 0.00056). Booster vaccination can significantly decrease the severity of Omicron infection when compared with unvaccinated patients (p = 0.009). In multivariate logistic analysis, erythrocyte sedimentation rate (ESR) (OR = 1.05) was independently related to the severity of the infection. Conclusions: The majority of clinical symptoms of Omicron infection were not severe. Early and aggressive administration of Paxlovid can significantly reduce the PCR conversion time. Booster vaccination should also be highly recommended in the population over 14 years old.</jats:p>",
"alternative-id": [
"vaccines10091409"
],
"author": [
{
"affiliation": [],
"family": "Shao",
"given": "Jiasheng",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0002-0814-0548",
"affiliation": [],
"authenticated-orcid": false,
"family": "Fan",
"given": "Rong",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Hu",
"given": "Jianrong",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Zhang",
"given": "Tiejun",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Lee",
"given": "Catherine",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Huang",
"given": "Xuyuan",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Wang",
"given": "Fei",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Liang",
"given": "Haiying",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Jin",
"given": "Ye",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Jiang",
"given": "Ying",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Gu",
"given": "Yanhua",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Huang",
"given": "Gang",
"sequence": "additional"
}
],
"container-title": "Vaccines",
"container-title-short": "Vaccines",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2022,
8,
31
]
],
"date-time": "2022-08-31T06:09:36Z",
"timestamp": 1661926176000
},
"deposited": {
"date-parts": [
[
2022,
8,
31
]
],
"date-time": "2022-08-31T07:10:13Z",
"timestamp": 1661929813000
},
"funder": [
{
"DOI": "10.13039/501100015377",
"award": [
"18DZ2260400"
],
"doi-asserted-by": "publisher",
"name": "Shanghai Key Laboratory of Molecular Imaging"
}
],
"indexed": {
"date-parts": [
[
2022,
8,
31
]
],
"date-time": "2022-08-31T07:41:17Z",
"timestamp": 1661931677965
},
"is-referenced-by-count": 0,
"issue": "9",
"issued": {
"date-parts": [
[
2022,
8,
28
]
]
},
"journal-issue": {
"issue": "9",
"published-online": {
"date-parts": [
[
2022,
9
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
8,
28
]
],
"date-time": "2022-08-28T00:00:00Z",
"timestamp": 1661644800000
}
}
],
"link": [
{
"URL": "https://www.mdpi.com/2076-393X/10/9/1409/pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1968",
"original-title": [],
"page": "1409",
"prefix": "10.3390",
"published": {
"date-parts": [
[
2022,
8,
28
]
]
},
"published-online": {
"date-parts": [
[
2022,
8,
28
]
]
},
"publisher": "MDPI AG",
"reference": [
{
"DOI": "10.2807/1560-7917.ES.2022.27.13.2200254",
"doi-asserted-by": "publisher",
"key": "ref1"
},
{
"DOI": "10.1002/jmv.27541",
"doi-asserted-by": "publisher",
"key": "ref2"
},
{
"DOI": "10.1007/s12098-022-04077-4",
"doi-asserted-by": "publisher",
"key": "ref3"
},
{
"DOI": "10.3346/jkms.2022.37.e31",
"doi-asserted-by": "publisher",
"key": "ref4"
},
{
"DOI": "10.3346/jkms.2021.36.e346",
"doi-asserted-by": "publisher",
"key": "ref5"
},
{
"DOI": "10.15585/mmwr.mm7050e1",
"doi-asserted-by": "publisher",
"key": "ref6"
},
{
"key": "ref7",
"unstructured": "COVID-19 Coronavirus Pandemic: Reported Cases and Deaths by Country or Territory\nhttps://www.worldometers.info/coronavirus/"
},
{
"article-title": "Shanghai Municipal Health Commission",
"key": "ref8",
"year": "2022"
},
{
"DOI": "10.1002/jmv.27540",
"doi-asserted-by": "publisher",
"key": "ref9"
},
{
"DOI": "10.1016/j.jep.2021.114220",
"doi-asserted-by": "publisher",
"key": "ref10"
},
{
"DOI": "10.1016/j.imr.2020.100644",
"doi-asserted-by": "publisher",
"key": "ref11"
},
{
"article-title": "Notice on printing and distributing the COVID-19 Pneumonia Diagnosis and Treatment Plan (Ninth Trial Version) 2022",
"author": "China NHCotPsRo",
"key": "ref12",
"year": "2022"
},
{
"DOI": "10.1056/NEJMoa2002032",
"doi-asserted-by": "publisher",
"key": "ref13"
},
{
"DOI": "10.1016/j.amjms.2021.01.004",
"doi-asserted-by": "publisher",
"key": "ref14"
},
{
"DOI": "10.22034/IJI.2022.94050.2278",
"doi-asserted-by": "publisher",
"key": "ref15"
},
{
"DOI": "10.1001/jama.2021.24868",
"doi-asserted-by": "publisher",
"key": "ref16"
},
{
"DOI": "10.1016/j.jinf.2022.04.017",
"doi-asserted-by": "publisher",
"key": "ref17"
},
{
"DOI": "10.1038/s41586-022-04479-6",
"doi-asserted-by": "publisher",
"key": "ref18"
},
{
"DOI": "10.21203/rs.3.rs-1191837/v1",
"doi-asserted-by": "publisher",
"key": "ref19"
},
{
"DOI": "10.1126/science.abd9149",
"doi-asserted-by": "publisher",
"key": "ref20"
},
{
"DOI": "10.1016/j.ijid.2021.02.089",
"doi-asserted-by": "publisher",
"key": "ref21"
},
{
"DOI": "10.1016/j.idh.2020.05.002",
"doi-asserted-by": "publisher",
"key": "ref22"
},
{
"DOI": "10.1038/s41591-020-0869-5",
"doi-asserted-by": "publisher",
"key": "ref23"
},
{
"DOI": "10.1136/bmj.o89",
"doi-asserted-by": "publisher",
"key": "ref24"
},
{
"DOI": "10.1016/j.jinf.2020.03.004",
"doi-asserted-by": "publisher",
"key": "ref25"
},
{
"DOI": "10.1038/d41586-022-00039-0",
"doi-asserted-by": "publisher",
"key": "ref26"
},
{
"DOI": "10.1038/d41586-022-00007-8",
"doi-asserted-by": "publisher",
"key": "ref27"
},
{
"DOI": "10.1016/j.phrs.2020.104761",
"doi-asserted-by": "publisher",
"key": "ref28"
},
{
"DOI": "10.1016/j.phyplu.2021.100027",
"doi-asserted-by": "publisher",
"key": "ref29"
},
{
"DOI": "10.1101/2022.04.07.22273595",
"doi-asserted-by": "publisher",
"key": "ref30"
},
{
"DOI": "10.1056/NEJMc2119236",
"doi-asserted-by": "publisher",
"key": "ref31"
},
{
"DOI": "10.3390/molecules27072221",
"doi-asserted-by": "publisher",
"key": "ref32"
},
{
"DOI": "10.1093/cid/ciac275",
"doi-asserted-by": "publisher",
"key": "ref33"
},
{
"DOI": "10.1001/jamapediatrics.2022.1110",
"doi-asserted-by": "publisher",
"key": "ref34"
},
{
"DOI": "10.3389/fpubh.2021.652842",
"doi-asserted-by": "publisher",
"key": "ref35"
},
{
"DOI": "10.1016/j.jcvp.2021.100059",
"doi-asserted-by": "publisher",
"key": "ref36"
},
{
"DOI": "10.1016/S2468-1253(20)30083-2",
"doi-asserted-by": "publisher",
"key": "ref37"
}
],
"reference-count": 37,
"references-count": 37,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.mdpi.com/2076-393X/10/9/1409"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Pharmacology (medical)",
"Infectious Diseases",
"Drug Discovery",
"Pharmacology",
"Immunology"
],
"subtitle": [],
"title": "Clinical Progression and Outcome of Hospitalized Patients Infected with SARS-CoV-2 Omicron Variant in Shanghai, China",
"type": "journal-article",
"volume": "10"
}