The association of mortality with vaccination and underlying disease among COVID-19 patients in long term care hospitals at Daegu and Gyeonsangbuk-do in Korea
et al., Research Square, doi:10.21203/rs.3.rs-3003449/v1, Jun 2023
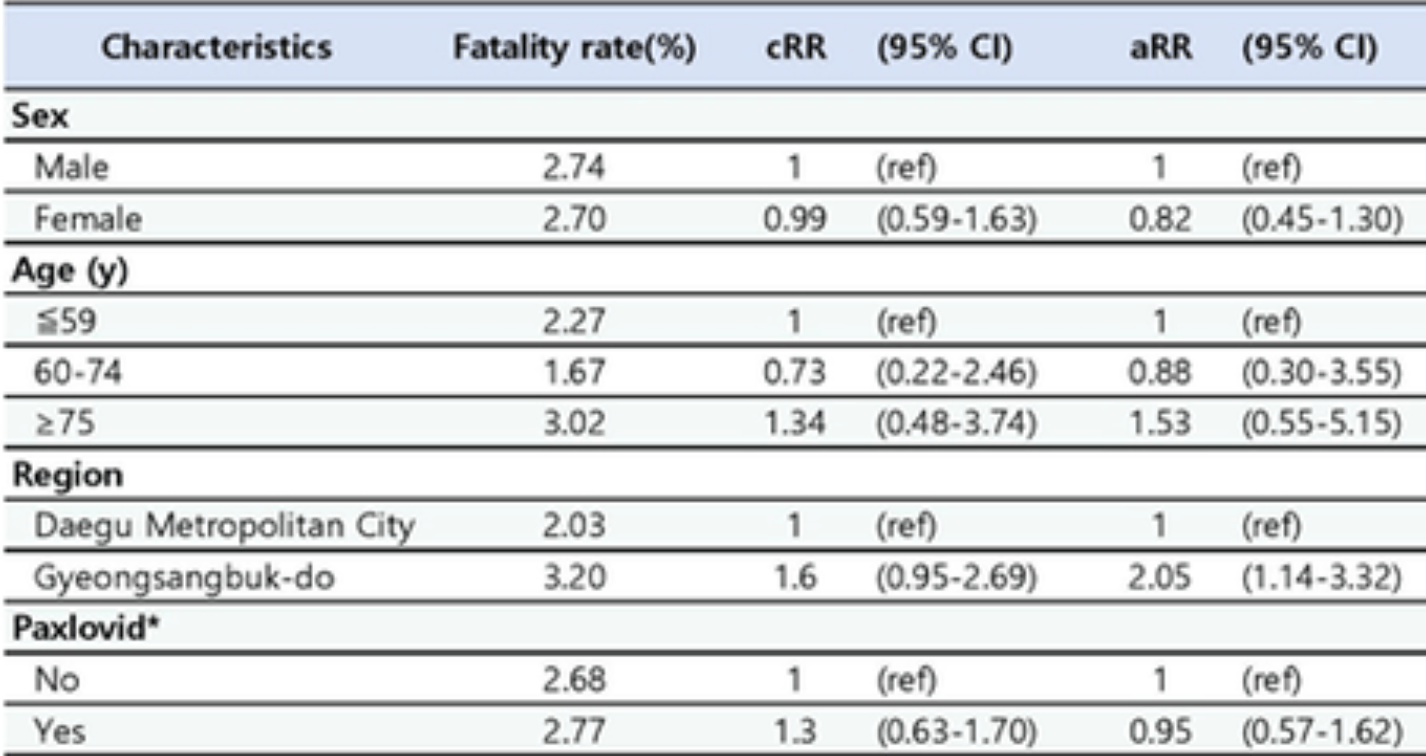
Retrospective 2,507 COVID-19 patients at 18 long term care hospitals with COVID-19 outbreaks in Korea, showing no significant difference in mortality with paxlovid treatment. Note that this study is less affected by the typical confounding in paxlovid population studies since the standard of care and treatment propensity for additional treatments is likely to be more similar for this population. Treatment delay is unknown and authors note that treatment may have been delayed.
In most population studies patients receiving paxlovid may have more contact with the medical system, be more likely to follow other recommendations, be more likely to receive additional care, and be more likely to take additional treatments that are not tracked in the data (e.g., nasal/oral hygiene1,2, vitamin D3, etc.).
Resistance. Variants may be resistant to paxlovid4-11. Use may promote the emergence of variants that weaken host immunity and potentially contribute to long COVID12. Confounding by contraindication. Hoertel et al. find that over 50% of patients that died had a contraindication for the use of Paxlovid13. Retrospective studies that do not exclude contraindicated patients may significantly overestimate efficacy. Black box warning. The FDA notes that severe, life-threatening, and/or fatal adverse reactions due to drug interactions have been reported in patients treated with paxlovid14. Kidney and liver injury. Studies show significantly increased risk of acute kidney injury15 and liver injury16,17. Viral rebound. Studies show significantly increased risk of replication-competent viral rebound18-20.
|
risk of death, 5.0% lower, RR 0.95, p = 0.86, treatment 940, control 1,567, adjusted per study, multivariable.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
4.
Zhou et al., Nirmatrelvir-resistant SARS-CoV-2 variants with high fitness in an infectious cell culture system, Science Advances, doi:10.1126/sciadv.add7197.
5.
Moghadasi et al., Rapid resistance profiling of SARS-CoV-2 protease inhibitors, npj Antimicrobials and Resistance, doi:10.1038/s44259-023-00009-0.
6.
Jochmans et al., The Substitutions L50F, E166A, and L167F in SARS-CoV-2 3CLpro Are Selected by a Protease Inhibitor In Vitro and Confer Resistance To Nirmatrelvir, mBio, doi:10.1128/mbio.02815-22.
7.
Lopez et al., SARS-CoV-2 Resistance to Small Molecule Inhibitors, Current Clinical Microbiology Reports, doi:10.1007/s40588-024-00229-6.
8.
Zvornicanin et al., Molecular Mechanisms of Drug Resistance and Compensation in SARS-CoV-2 Main Protease: The Interplay Between E166 and L50, bioRxiv, doi:10.1101/2025.01.24.634813.
9.
Vukovikj et al., Impact of SARS-CoV-2 variant mutations on susceptibility to monoclonal antibodies and antiviral drugs: a non-systematic review, April 2022 to October 2024, Eurosurveillance, doi:10.2807/1560-7917.ES.2025.30.10.2400252.
10.
Deschenes et al., Functional and structural characterization of treatment-emergent nirmatrelvir resistance mutations at low frequencies in the main protease (Mpro) reveals a unique evolutionary route for SARS-CoV-2 to gain resistance, The Journal of Infectious Diseases, doi:10.1093/infdis/jiaf294.
11.
Zhou (B) et al., SARS-CoV-2 Mpro inhibitor ensitrelvir: asymmetrical cross-resistance with nirmatrelvir and emerging resistance hotspots, Emerging Microbes & Infections, doi:10.1080/22221751.2025.2552716.
12.
Thomas et al., Nirmatrelvir-Resistant Mutations in SARS-CoV-2 Mpro Enhance Host Immune Evasion via Cleavage of NF-κB Essential Modulator, bioRxiv, doi:10.1101/2024.10.18.619137.
13.
Hoertel et al., Prevalence of Contraindications to Nirmatrelvir-Ritonavir Among Hospitalized Patients With COVID-19 at Risk for Progression to Severe Disease, JAMA Network Open, doi:10.1001/jamanetworkopen.2022.42140.
14.
FDA, Fact sheet for healthcare providers: emergency use authorization for paxlovid, www.fda.gov/media/155050/download.
15.
Kamo et al., Association of Antiviral Drugs for the Treatment of COVID-19 With Acute Renal Failure, In Vivo, doi:10.21873/invivo.13637.
16.
Wang et al., Development and validation of a nomogram to assess the occurrence of liver dysfunction in patients with COVID-19 pneumonia in the ICU, BMC Infectious Diseases, doi:10.1186/s12879-025-10684-1.
17.
Siby et al., Temporal Trends in Serious Adverse Events Associated with Oral Antivirals During the COVID-19 Pandemic: Insights from the FAERS Database (2020–2023), Open Forum Infectious Diseases, doi:10.1093/ofid/ofaf695.1825.
18.
Edelstein et al., SARS-CoV-2 virologic rebound with nirmatrelvir-ritonavir therapy, medRxiv, doi:10.1101/2023.06.23.23288598.
Park et al., 16 Jun 2023, retrospective, South Korea, peer-reviewed, 11 authors, study period January 2022 - August 2022.
The association of mortality with vaccination and underlying disease among COVID-19 patients in long term care hospitals at Daegu and Gyeonsangbuk-do in Korea
doi:10.21203/rs.3.rs-3003449/v1
Background This study aimed to estimate the effects of vaccine on reducing the mortality rate and the relationship between underlying diseases and death among long term care hospital residents during the Omicron epidemic.
Methods This study included 2,507 inpatients at 18 long term care hospitals that experienced COVID-19 outbreaks more than twice in Daegu Metropolitan City and Gyeongsangbuk-do in Korea, from January 2022 to August 2022. Descriptive statistics were used to analyze participants' demographic characteristics and mortality, which were expressed as percentages (%). Logistic regression analysis was performed to compare mortality, and the crude risk ratio (cRR) and adjusted risk risk (aRR) were estimated. The analysis model was adjusted for sex, age, region, history of Paxlovid priscription, vaccine status, reinfection, and presence, type, and number of underlying diseases.
Results In terms of vaccination status, the aRR in the group with < 90 days after the 3 doses was 0.20 (CI:0.09-0.45) and ≥ 90 days was 0.14 (CI:0.06-0.32), that in the group with < 90 days after 4 doses was 0.18 (CI:0.06-0.43), compared with the non-vaccinated group. The fatality rate in the group prescribed Paxlovid was higher than that in the non-prescribed group. However, the difference was not statistically signi cant. The aRR of hypothyroidism was 5.75 (CI:1.10-30.13) and that of COPD and asthma were 2.84 (CI:1.15-6.99), compared with the group that did not have each underlying disease.
Conclusion We con rmed the preventive effects of vaccination on death and the high risk of death from hypothyroidism, COPD, and asthma in COVID-19-con rmed patients in long term care hospitals.
Abbreviations
References
Alqahtani, Oyelade, Aldhahir, Alghamdi, Almehmadi et al., Severity and Mortality associated with COPD and Smoking in patients with COVID-19: A Rapid Systematic Review and Meta-Analysis, PLoS One
Bogos, Berta, Cselko, Tisza, Szilasi et al., None
Brix, Hegedus, Hallas, Lund, Risk and course of SARS-CoV-2 infection in patients treated for hypothyroidism and hyperthyroidism, Lancet Diabetes Endocrinol
Collie, Champion, Moultrie, Bekker, Gray, Effectiveness of BNT162b2 Vaccine against Omicron Variant in South Africa, N Engl J Med
Cummings, Baldwin, Abrams, Jacobson, Meyer et al., Epidemiology, clinical course, and outcomes of critically ill adults with COVID-19 in New York City: a prospective cohort study, Lancet
Dehu, Jianghua, Xianzhi, The Role of the Acetylcholine System in Common Respiratory Diseases and COVID-19, Molecules
Dessie, Zewotir, Mortality-related risk factors of COVID-19: a systematic review and metaanalysis of 42 studies and 423,117 patients, BMC Infect Dis
Diniz, Senger, Carneiro-Ramos, Santos, Barreto-Chaves, Cardiac ACE2/angiotensin 1-7/Mas receptor axis is activated in thyroid hormone-induced cardiac hypertrophy, Ther Adv Cardiovasc Dis
Javanmardi, Keshavarzi, Akbari, Emami, Pirbonyeh, Prevalence of underlying diseases in died cases of COVID-19: A systematic review and meta-analysis, PLoS One
Ji, Ma, Peppelenbosch, Pan, Potential association between COVID-19 mortality and healthcare resource availability, Lancet Glob Health
Kompaniyets, Pennington, Goodman, Rosenblum, Belay et al., Underlying Medical Conditions and Severe Illness Among 540,667 Adults Hospitalized With COVID-19, Prev Chronic Dis
Konstantinoudis, Cameletti, Gomez-Rubio, Gomez, Pirani et al., Regional excess mortality during the 2020 COVID-19 pandemic in ve European countries, Nat Commun
Lacedonia, Scioscia, Santomasi, Fuso, Carpagnano et al., Impact of smoking, COPD and comorbidities on the mortality of COVID-19 patients, Sci Rep
Lee, Ionescu, Starkey, Little, Tilby et al., COVID-19: Third dose booster vaccine effectiveness against breakthrough coronavirus infection, hospitalisations and death in patients with cancer: A population-based study, Eur J Cancer
Leung, Yang, Tam, Shaipanich, Hackett et al., ACE-2 expression in the small airway epithelia of smokers and COPD patients: implications for COVID-19, Eur Respir J
Lillevang-Johansen, Abrahamsen, Jorgensen, Brix, Hegedus, Duration of over-and under-treatment of hypothyroidism is associated with increased cardiovascular risk, Eur J Endocrinol
Lj, Chemaitelly, Bertollini, Severity of SARS-CoV-2 Reinfections as Compared with Primary Infections, N Engl J Med
Mohammed, Pham-Tran, Yeoh, Wang, Mcmillan et al., A Systematic Review and Meta-Analysis on the Real-World Effectiveness of COVID-19 Vaccines against Infection, Symptomatic and Severe COVID-19 Disease Caused by the Omicron Variant (B.1.1.529), Vaccines (Basel)
Mohapatra, Kandi, Sarangi, Verma, Tuli et al., The recently emerged BA.4 and BA.5 lineages of Omicron and their global health concerns amid the ongoing wave of COVID-19 pandemic -Correspondence, Int J Surg
Nguyen, Houhamdi, Hoang, Delerce, Delorme et al., SARS-CoV-2 reinfection and COVID-19 severity, Emerg Microbes Infect
Park, Park, Lee, Lee, Ahn H. mRNA vaccine effectiveness against SARS-CoV-2 B.1.617.2 (Delta) and B.1.1.529 (Omicron) variant transmission from home care cases to household contacts in South Korea, Osong Public Health Res Perspect
Park, Park, Lee, Yu, Song et al., The effectiveness of Paxlovid treatment in longterm care facilities in South Korea during the outbreak of the Omicron variant of SARS-CoV-2, Osong Public Health Res Perspect
Polverino, Cigarette smoking and COVID-19: A complex interaction, American Journal of Respiratory and Critical Care Medicine
Shams, Basati, Kalvandi, Abdoli, Tavan, Frequency of underlying diseases, symptoms and mortality rate of COVID-19: a systematic review and meta-analysis, Reviews in Medical Microbiology
Thakur, Dubey, Benitez, Torres, Reddy et al., A systematic review and metaanalysis of geographic differences in comorbidities and associated severity and mortality among individuals with COVID-19, Sci Rep
Tulimilli, Dallavalasa, Basavaraju, Rao, Chikkahonnaiah et al., Variants of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) and Vaccine Effectiveness, Vaccines (Basel)
Weng, Xie, Han, Yuan, Li et al., Safety and E cacy of Paxlovid Against Omicron Variants of Coronavirus Disease 2019 in Elderly Patients, Infect Dis Ther
DOI record:
{
"DOI": "10.21203/rs.3.rs-3003449/v1",
"URL": "http://dx.doi.org/10.21203/rs.3.rs-3003449/v1",
"abstract": "<jats:title>Abstract</jats:title>\n <jats:p>Background\n This study aimed to estimate the effects of vaccine on reducing the mortality rate and the relationship between underlying diseases and death among long term care hospital residents during the Omicron epidemic.\nMethods\n This study included 2,507 inpatients at 18 long term care hospitals that experienced COVID-19 outbreaks more than twice in Daegu Metropolitan City and Gyeongsangbuk-do in Korea, from January 2022 to August 2022. Descriptive statistics were used to analyze participants’ demographic characteristics and mortality, which were expressed as percentages (%). Logistic regression analysis was performed to compare mortality, and the crude risk ratio (cRR) and adjusted risk risk (aRR) were estimated. The analysis model was adjusted for sex, age, region, history of Paxlovid priscription, vaccine status, reinfection, and presence, type, and number of underlying diseases.\nResults\n In terms of vaccination status, the aRR in the group with < 90 days after the 3 doses was 0.20 (CI:0.09–0.45) and ≥ 90 days was 0.14 (CI:0.06–0.32), that in the group with < 90 days after 4 doses was 0.18 (CI:0.06–0.43), compared with the non-vaccinated group. The fatality rate in the group prescribed Paxlovid was higher than that in the non-prescribed group. However, the difference was not statistically significant. The aRR of hypothyroidism was 5.75 (CI:1.10–30.13) and that of COPD and asthma were 2.84 (CI:1.15–6.99), compared with the group that did not have each underlying disease.\nConclusion\n We confirmed the preventive effects of vaccination on death and the high risk of death from hypothyroidism, COPD, and asthma in COVID-19-confirmed patients in long term care hospitals.</jats:p>",
"accepted": {
"date-parts": [
[
2023,
5,
31
]
]
},
"author": [
{
"affiliation": [
{
"name": "Division of Infectious Disease Response, Gyeongbuk Regional Center for Disease Control and Prevention, Korea Disease Control and Prevention Agency (KDCA), Daegu"
}
],
"family": "Park",
"given": "Hanul",
"sequence": "first"
},
{
"affiliation": [
{
"name": "Division of Infectious Disease Response, Gyeongbuk Regional Center for Disease Control and Prevention, Korea Disease Control and Prevention Agency (KDCA), Daegu"
}
],
"family": "Park",
"given": "Chungmin",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Division of Infectious Disease Response, Gyeongbuk Regional Center for Disease Control and Prevention, Korea Disease Control and Prevention Agency (KDCA), Daegu"
}
],
"family": "Choi",
"given": "Seong-Ju",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Division of Infectious Disease Response, Gyeongbuk Regional Center for Disease Control and Prevention, Korea Disease Control and Prevention Agency (KDCA), Daegu"
}
],
"family": "Jung",
"given": "Yeon Haw",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Division of Infectious Disease Response, Gyeongbuk Regional Center for Disease Control and Prevention, Korea Disease Control and Prevention Agency (KDCA), Daegu"
}
],
"family": "Hwang",
"given": "Myung-Jae",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Division of Infectious Disease Response, Gyeongbuk Regional Center for Disease Control and Prevention, Korea Disease Control and Prevention Agency (KDCA), Daegu"
}
],
"family": "Son",
"given": "Junseock",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Division of Infectious Disease Response, Gyeongbuk Regional Center for Disease Control and Prevention, Korea Disease Control and Prevention Agency (KDCA), Daegu"
}
],
"family": "Seo",
"given": "Inyeong",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Division of Infectious Disease Response, Gyeongbuk Regional Center for Disease Control and Prevention, Korea Disease Control and Prevention Agency (KDCA), Daegu"
}
],
"family": "Park",
"given": "Taeyeon",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Gyungsangbuk-do Welfare and health Bureau infectious Disease control Division, Gyungsangbuk-do"
}
],
"family": "Kim",
"given": "You Kyung",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Division of Infectious Disease Control, Daegu Metropolitan City Hall, Daegu"
}
],
"family": "Seong",
"given": "Ji-Seon",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Division of Infectious Disease Response, Gyeongbuk Regional Center for Disease Control and Prevention, Korea Disease Control and Prevention Agency (KDCA), Daegu"
}
],
"family": "Son",
"given": "Taejong",
"sequence": "additional"
}
],
"container-title": [],
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2023,
6,
16
]
],
"date-time": "2023-06-16T15:28:14Z",
"timestamp": 1686929294000
},
"deposited": {
"date-parts": [
[
2023,
10,
18
]
],
"date-time": "2023-10-18T04:59:48Z",
"timestamp": 1697605188000
},
"group-title": "In Review",
"indexed": {
"date-parts": [
[
2023,
10,
19
]
],
"date-time": "2023-10-19T05:06:52Z",
"timestamp": 1697692012148
},
"institution": [
{
"name": "Research Square"
}
],
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2023,
6,
16
]
]
},
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "unspecified",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
6,
16
]
],
"date-time": "2023-06-16T00:00:00Z",
"timestamp": 1686873600000
}
}
],
"link": [
{
"URL": "https://www.researchsquare.com/article/rs-3003449/v1",
"content-type": "text/html",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://www.researchsquare.com/article/rs-3003449/v1.html",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "8761",
"original-title": [],
"posted": {
"date-parts": [
[
2023,
6,
16
]
]
},
"prefix": "10.21203",
"published": {
"date-parts": [
[
2023,
6,
16
]
]
},
"publisher": "Research Square Platform LLC",
"reference-count": 0,
"references-count": 0,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.researchsquare.com/article/rs-3003449/v1"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subtitle": [],
"subtype": "preprint",
"title": "The association of mortality with vaccination and underlying disease among COVID-19 patients in long term care hospitals at Daegu and Gyeonsangbuk-do in Korea",
"type": "posted-content"
}