Sunlight exposure might account for the relatively low COVID-19 morbidity and mortality in tropical countries
et al., Tropical Biomedicine, doi:10.47665/tb.41.1.010, Mar 2024
Sunlight for COVID-19
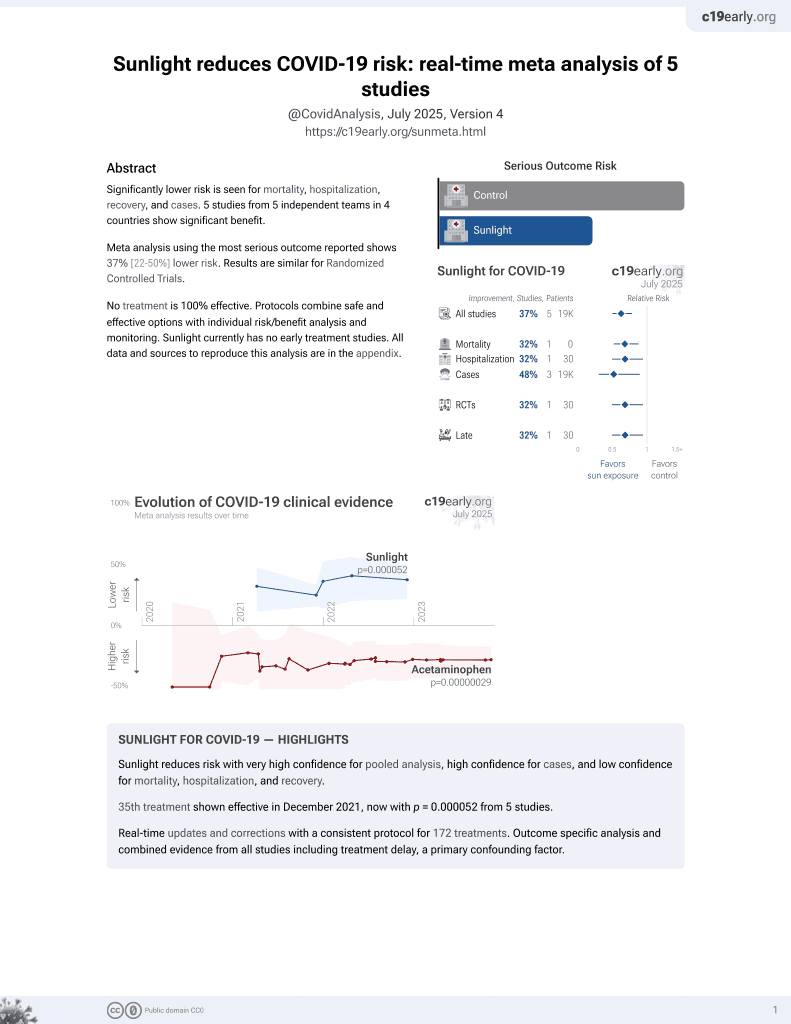
36th treatment shown to reduce risk in
December 2021, now with p = 0.000052 from 5 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective analysis of tropical and non-tropical countries showing significantly lower COVID-19 cases and mortality in tropical countries. The study found that specific photovoltaic power output, global horizontal irradiation, diffuse horizontal irradiation, and global tilted irradiation were inversely correlated with COVID-19 cases and mortality, suggesting that stronger sunlight exposure may lead to lower COVID-19 cases and deaths.
Muhammad et al., 25 Mar 2024, retrospective, peer-reviewed, 7 authors.
Sunlight exposure might account for the relatively low COVID-19 morbidity and mortality in tropical countries
Tropical Biomedicine, doi:10.47665/tb.41.1.010
The present study aimed at exploring whether sunlight exposure might account for the relative difference in COVID-19-related morbidity and mortality between tropical and non-tropical countries. A retrospective observational study was designed and data from the World Health Organization weekly COVID-19 epidemiological update was compiled. We examined the total number of confirmed COVID-19 cases per 100 000 population, as well as the total number of COVID-19-related mortalities per 100 000 population. Solar variables data were obtained from the Global Solar Atlas website (https://globalsolaratlas.info/). These data were analyzed to determine the association of sunlight exposure to COVID-19-related morbidity and mortality in tropical and non-tropical countries. Results revealed a statistically significant decrease in the number of confirmed COVID-19 cases per 100 000 population (P<0.001), as well as the number of COVID-19-related mortalities per 100 000 population (P<0.001) between tropical and non-tropical countries. Analyses of sunlight exposure data found that specific photovoltaic power output, global horizontal irradiation, diffuse horizontal irradiation and global tilted irradiation at optimum angle were significantly inversely correlated to COVID-19-related morbidity and mortality. This suggests that stronger sunlight exposure potentially leads to lower COVID-19-related morbidity and mortality. Findings from this study suggest that the relatively low COVID-19-related morbidity and mortality in tropical countries were possibly due to better sunlight exposure that translates into adequate vitamin D status.
Conflict of interest statement The authors declare that there are no conflicts of interest.
References
Aabed, Lashin, An analytical study of the factors that influence COVID-19 spread, Saudi Journal of Biological Sciences, doi:10.1016/j.sjbs.2020.11.067
Amariles, Granados, Ceballos, Montoya, COVID-19 in Colombia endpoints. Are we different, like Europe?, Research in Social and Administrative Pharmacy, doi:10.1016/j.sapharm.2020.03.013
Asyary, Veruswati, Sunlight exposure increased COVID-19 recovery rates: a study in the central pandemic area of Indonesia, Science of The Total Environment, doi:10.1016/j.scitotenv.2020.139016
Baktash, Hosack, Zahari, Shah, Kandiah et al., Vitamin D status and outcomes for hospitalised older patients with COVID-19, Postgraduate Medical Journal, doi:10.1136/postgradmedj-2020-138712
Barin, HIV / AIDs as a model for emerging infectious disease: origin, dating and circumstances of an emblematic epidemiological success, La Presse Mיdicale, doi:10.1016/j.lpm.2022.104128
Benskin, A basic review of the preliminary evidence that COVID-19 risk and severity is increased in Vitamin D deficiency, Frontiers in Public Health, doi:10.3389/fpubh.2020.00513
Bergman, The link between Vitamin D and COVID 19: distinguishing facts from fiction, Journal of Internal Medicine, doi:10.1111/joim.13158
Bilezikian, Bikle, Hewison, Lazaretti-Castro, Formenti et al., Mechanisms in endocrinology: vitamin D and COVID-19, European Journal of Endocrinology, doi:10.1530/EJE-20-0665
Brenner, Schöttker, Vitamin D insufficiency may account for almost nine of ten COVID-19 deaths: time to act. Comment on: "Vitamin D deficiency and outcome of COVID-19 patients, Nutrients, doi:10.3390/nu12123642
Calder, Carr, Gombart, Eggersdorfer, Optimal nutritional status for a well-functioning immune system ss an important factor to protect against viral infections, Nutrients, doi:10.3390/nu12041181
Carleton, Cornetet, Huybers, Meng, Proctor, Global evidence for ultraviolet radiation decreasing COVID-19 growth rates, Proceedings of the National Academy of Sciences, doi:10.1073/pnas.2012370118
Carta, Scano, Lindert, Bonanno, Rinaldi et al., Association between the spread of COVID-19 and weatherclimatic parameters, European Review for Medical and Pharmacological Sciences, doi:10.26355/eurrev_202008_22512
Cutolo, Paolino, Smith, Evidences for a protective role of vitamin D in COVID-19, RMD Open, doi:10.1136/rmdopen-2020-001454
D'avolio, Avataneo, Manca, Cusato, De Nicolò et al., 25-Hydroxyvitamin D concentrations are lower in patients with positive PCR for SARS-CoV-2, Nutrients, doi:10.3390/nu12051359
Ebadi, Montano-Loza, Perspective: improving vitamin D status in the management of COVID-19, European Journal of Clinical Nutrition, doi:10.1038/s41430-020-0661-0
Ghosh, Bernstein, Mersha, COVID-19 pandemic: the African paradox, Journal of Global Health, doi:10.7189/jogh.10.020348
Gibbons, Norton, Mccullough, Meltzer, Lavigne et al., Association between vitamin D supplementation and COVID-19 infection and mortality, Scientific Reports, doi:10.1038/s41598-022-24053-4
Gyselinck, Liesenborghs, Landeloos, Belmans, Verbeke et al., Direct antivirals working against the novel coronavirus: azithromycin (Dawn-Azithro), a randomized, multicenter, open-label, adaptive, proof-of-concept clinical trial of new antivirals working against SARS-CoV-2-zzithromycin trial, Trials, doi:10.1186/s13063-021-05033-x
Kontis, Bennett, Rashid, Parks, Pearson-Stuttard et al., Magnitude, demographics and dynamics of the effect of the first wave of the COVID-19 pandemic on all-cause mortality in 21 industrialized countries, Nature Medicine, doi:10.1038/s41591-020-1112-0
Laird, Rhodes, Kenny, Vitamin D and inflammation: potential implications for severity of COVID-19, Irish Medical Journal
Lansiaux, Pébaÿ, Picard, Forget, COVID-19 and vit-D: disease mortality negatively correlates with sunlight exposure, Spatial and Spatio-temporal Epidemiology, doi:10.1016/j.sste.2020.100362
Lone, Ahmad, COVID-19 pandemic -an African perspective, Emerging Microbes and Infection, doi:10.1080/22221751.2020.1775132
Mann, Whitney, On a test of whether one of two random variables is stochastically larger than the other, The Annals of Mathematical Statistics, doi:10.1214/aoms/1177730491
Martineau, Forouhi, Vitamin D for COVID-19: a case to answer?, Lancet Diabetes and Endocrinology, doi:10.1016/S2213-8587(20)30268-0
Mccartney, Byrne, Optimisation of Vitamin D status for enhanced immuno-protection against COVID-19, Irish Medical Journal
Meltzer, Best, Zhang, Vokes, Arora et al., Association of vitamin D status and other clinical characteristics with COVID-19 test results, JAMA Network Open, doi:10.1001/jamanetworkopen.2020.19722
Mercola, Grant, Wagner, Evidence regarding vitamin D and risk of COVID-19 and its severity, Nutrients, doi:10.3390/nu12113361
Mohan, Cherian, Sharma, Exploring links between vitamin D deficiency and COVID-19, PLoS Pathogens, doi:10.1371/journal.ppat.1008874
Muhammad, Hassan, Baba, Radda, Mutawakkil et al., Exploring NFkB pathway as a potent strategy to mitigate COVID-19 severe morbidity and mortality, Journal of Public Health in Africa, doi:10.4081/jphia.2022.1679
Naudet, Locher, Braillon, Gillibert, Letter to the editor: COVID-19 and Vit-D: disease mortality negatively correlates with sunlight exposure, Spatial and Spatio-temporal Epidemiology, doi:10.1016/j.sste.2020.100373
Njenga, Dawa, Nanyingi, Gachohi, Ngere et al., Why ss there low morbidity and mortality of COVID-19 in Africa?, American Journal of Tropical Medicine and Hygiene, doi:10.4269/ajtmh.20-0474
Okonji, Okonji, Mukumbang, Van Wyk, Understanding varying COVID-19 mortality rates reported in Africa compared to Europe, Americas and Asia, Tropical Medicine and International Health, doi:10.1111/tmi.13575
Panarese, Shahini, COVID-19, and vitamin D, Alimentary Pharmacology & Therapeutics, doi:10.1111/apt.15752
Pinzon, Pradana, Vitamin D deficiency among patients with COVID-19: case series and recent literature review, Tropical Medicine and Health, doi:10.1186/s41182-020-00277-w
Radujkovic, Hippchen, Tiwari-Heckler, Dreher, Boxberger et al., Vitamin D deficiency and outcome of COVID-19 patients, Nutrients, doi:10.3390/nu12092757
Rhodes, Subramanian, Laird, Kenny, Editorial: low population mortality from COVID-19 in countries south of latitude 35 degrees North supports vitamin D as a factor determining severity, Alimentary Pharmacology and Therapeutics, doi:10.1111/apt.15777
Ribeiro, De Santana, Oliver, Rond, Mendes et al., Does vitamin D play a role in the management of COVID-19 in Brazil?, Revista de Saude Publica, doi:10.11606/s1518-8787.2020054002545
Rosario, Mutz, Bernardes, Conte-Junior, Relationship between COVID-19 and weather: case study in a tropical country, International Journal of Hygiene and Environmental Health, doi:10.1016/j.ijheh.2020.113587
Ruiz-Beltrán, Herrero-Herrero, Martín-Sánchez, Martín-Gonzalez, Prevalence of antibodies to Rickettsia conorii, Coxiella burnetii and Rickettsia typhi in Salamanca province (Spain). Serosurvey in the human population, European Journal of Epidemiology, doi:10.1007/BF00150435
Santaolalla, Beckmann, Kibaru, Josephs, Van Hemelrijck et al., Association between vitamin D and novel SARS-CoV-2 respiratory dysfunction -a scoping review of current evidence and its implication for COVID-19 pandemic, Frontiers Physiology, doi:10.3389/fphys.2020.564387
Shao, Xie, Zhu, Mediation by human mobility of the association between temperature and COVID-19 transmission rate, Environmental Research, doi:10.1016/j.envres.2020.110608
Shaphiro, Wilk, An analysis of variance test for normality, Biometrika, doi:10.2307/2333709
Siddiqui, Manansala, Abdulrahman, Nasrallah, Smatti et al., Immune modulatory effects of vitamin D on viral infections, Nutrients, doi:10.3390/nu12092879
Suhaimi, Jalaludin, Latif, Demystifying a possible relationship between COVID-19, air quality and meteorological factors: evidence from Kuala Lumpur, Malaysia, Aerosol and Air Quality Research, doi:10.4209/aaqr.2020.05.0218
Sulli, Gotelli, Casabella, Paolino, Pizzorni et al., Vitamin D and lung outcomes in elderly COVID-19 patients, Nutrients, doi:10.3390/nu13030717
Tosepu, Gunawan, Effendy, Ahmad, Lestari et al., Correlation between weather and COVID-19 pandemic in Jakarta, Indonesia, Science of The Total Environment, doi:10.1016/j.scitotenv.2020.138436
Villani, Mckee, Cascini, Ricciardi, Boccia, Comparison of deaths rates for COVID-19 across Europe during the first wave of the COVID-19 pandemic, Frontiers in Public Health, doi:10.3389/fpubh.2020.620416
Waskom, Seaborn: statistical data visualization, The Journal of Open Source Software, doi:10.21105/joss.03021
Weir, Thenappan, Bhargava, Chen, Does vitamin D deficiency increase the severity of COVID-19?, Clinical Medicine, doi:10.7861/clinmed.2020-0301
Worobey, Gemmel, Teuwen, Haselkorn, Kunstman et al., Direct evidence of extensive diversity of HIV-1 in Kinshasa by 1960, Nature, doi:10.1038/nature07390
Xiao, Li, Su, Mu, Qu, Could SARS-CoV-2-induced lung injury be attenuated by vitamin D?, International Journal of Infectious Diseases, doi:10.1016/j.ijid.2020.10.059
Yamamoto, Bauer, Apparent difference in fatalities between Central Europe and East Asia due to SARS-CoV-2 and COVID-19: four hypotheses for possible explanation, Medical Hypotheses, doi:10.1016/j.mehy.2020.110160
Yousefifard, Zali, Ali, Neishaboori, Zarghi et al., Antiviral therapy in management of COVID-19: a systematic review on current evidence, Archives of Academic Emergency Medicine
Yudistira, Sumitro, Nahas, Riama, UV light influences COVID-19 activity through big data: trade offs between northern subtropical, tropical, and southern subtropical countries, MedRxiv, doi:10.1101/2020.04.30.20086983
Zemb, Bergman, Camargo, Cavalier, Cormier et al., Vitamin D deficiency and the COVID-19 pandemic, Journal of Global Antimicrobial Resistance, doi:10.1016/j.jgar.2020.05.006