Effects of vitamin D on COVID-19 risk and hospitalisation in the UK biobank
et al., PLoS One, doi:10.1371/journal.pone.0328232, Jul 2025
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 136 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Case-control analysis of 151,543 UK Biobank participants showing higher odds of COVID-19 hospitalisation for those with low baseline serum vitamin D, and slightly lower risk of cases. Vitamin D measurements were taken a decade before the pandemic.
This is the 222nd of 228 COVID-19 sufficiency studies for vitamin D, which collectively show higher levels reduce risk with p<0.0000000001.
Standard of Care (SOC) for COVID-19 in the study country,
the United Kingdom, is very poor with very low average efficacy for approved treatments1.
The United Kingdom focused on expensive high-profit treatments, approving only one low-cost early treatment, which required a prescription and had limited adoption. The high-cost prescription treatment strategy reduces the probability of early treatment due to access and cost barriers, and eliminates complementary and synergistic benefits seen with many low-cost treatments.
|
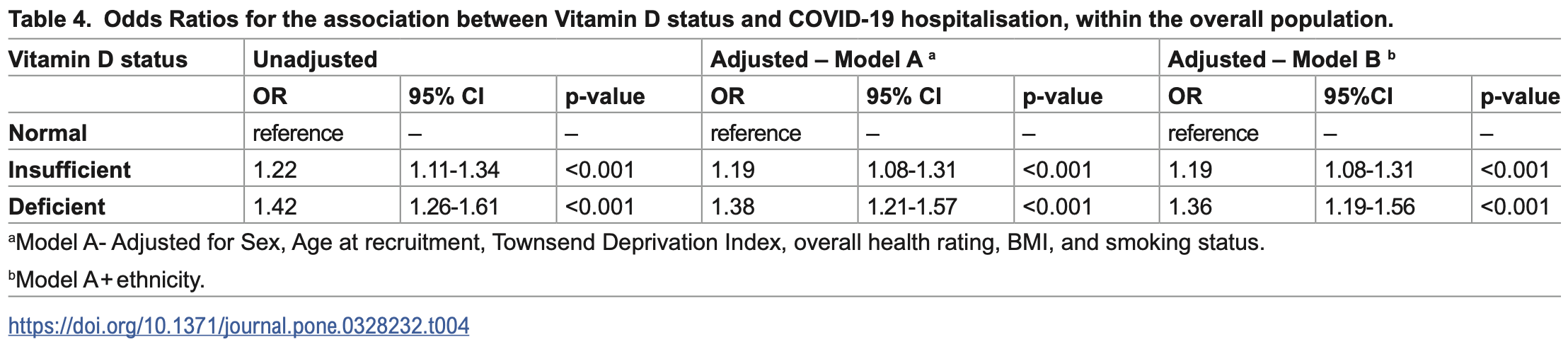
risk of hospitalization, 26.5% lower, OR 0.74, p < 0.001, high D levels (≥50nmol/L) 69,746, low D levels (<25nmol/L) 19,358, adjusted per study, inverted to make OR<1 favor high D levels (≥50nmol/L), deficiency, model B, multivariable, RR approximated with OR.
|
|
risk of hospitalization, 16.0% lower, OR 0.84, p < 0.001, high D levels (≥50nmol/L) 69,746, low D levels (<50nmol/L) 81,797, adjusted per study, inverted to make OR<1 favor high D levels (≥50nmol/L), deficiency, model B, multivariable, RR approximated with OR.
|
|
risk of case, 5.3% higher, OR 1.05, p = 0.03, high D levels (≥50nmol/L) 69,746, low D levels (<25nmol/L) 19,358, adjusted per study, inverted to make OR<1 favor high D levels (≥50nmol/L), deficiency, model B, multivariable, RR approximated with OR.
|
|
risk of case, 3.1% higher, OR 1.03, p = 0.05, high D levels (≥50nmol/L) 69,746, low D levels (<50nmol/L) 81,797, adjusted per study, inverted to make OR<1 favor high D levels (≥50nmol/L), deficiency, model B, multivariable, RR approximated with OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Monroy-Iglesias et al., 18 Jul 2025, retrospective, United Kingdom, peer-reviewed, mean age 56.0, 8 authors, study period March 2020 - October 2020.
Contact: maria.j.monroy_iglesias@kcl.ac.uk.
Effects of vitamin D on COVID-19 risk and hospitalisation in the UK biobank
doi:10.1371/journal.pone.0328232
Background Vitamin D (VitD) plays an important role in immune modulation. VitD deficiency is associated with increased susceptibility to acute respiratory syndrome as observed in COVID-19. We evaluated potential associations between serum VitD levels and risk of COVID-19 infection and hospitalisation, within the overall and cancer populations.
Methods We performed a nested case-control study within the UK biobank cohort, among all individuals with at least one serum VitD level measurement at baseline (2006)(2007)(2008)(2009)(2010) and a COVID-19 polymerase chain reaction (PCR) results recorded, and individuals with previous cancer diagnosis. Binary multivariable logistic regression was performed to assess associations between VitD levels and risk of COVID-19 infection (positive PCR), and hospitalisation (COVID-19-positive PCR in hospital), and stratified by ethnicity.
Results Of 151,543 participants, 21,396 tested positive for COVID-19. Of 24,400 individuals with cancer, 2,608 tested positive. In the total cohort, VitD insufficiency (Adjusted Odds Ratio (aOR) 0.97, 95% Confidence Interval (CI) 0.94-1.00) and deficiency (aOR 0.95, 95%CI 0.90-0.99) were associated with slightly lower odds of COVID-19 infection. In contrast, both VitD insufficiency (aOR 1.19, 95%CI 1.08-1.31) and deficiency (aOR 1.36, 95%CI 1.19-1.56) were associated with higher odds of COVID-19 hospitalisation. Among Asian (aOR 1.50; 95%CI 1.08-2.07) and Black (aOR 1.57; 95%CI 1.14-2.16) participants, VitD deficiency was associated with higher odds of COVID-19 infection. Among White participants, VitD insufficiency was associated with slightly lower odds of COVID-19 infection (aOR 0.97; 95%CI 0.86-0.95), while both VitD insufficiency (aOR 1.19; 95%CI 1.08-1.32) and deficiency (aOR 1.44; 95%CI 1.25-1.66) were associated with increased odds of hospitalisation. In the cancer population, vitamin D deficiency was associated with higher odds of infection only among Black participants (aOR 3.50; 95%CI 1.22-10.01); no other associations were observed.
Conclusions Low VitD levels were associated with an increased risk of COVID-19 hospitalisation but showed only a weak association with infection risk. Black and Asian populations had higher infection risk associated with VitD deficiency, but this did not translate to increased hospitalisation. In contrast, White populations with low VitD levels exhibited a higher risk of hospitalisation. There was no evidence of an interaction between VitD levels and ethnicity affecting infection or hospitalisation risk. In the cancer cohort, no significant associations were observed for COVID-19 infection or hospitalisation. provided the original author and source are credited.
Supporting information S1
References
Aoun, Maalouf, Fahed, Jabbour, When and How to Diagnose and Treat Vitamin D Deficiency in Adults: A Practical and Clinical Update, J Diet Suppl, doi:10.1080/19390211.2019.1577935
Bergman, The link between vitamin D and COVID-19: distinguishing facts from fiction, J Intern Med, doi:10.1111/joim.13158
Cheruiyot, Kipkorir, Ngure, Misiani, Munguti, Cancer is associated with coronavirus disease (COVID-19) severity and mortality: A pooled analysis, Am J Emerg Med, doi:10.1016/j.ajem.2020.08.025
Chung, Silwal, Kim, Modlin, Jo, Vitamin D-Cathelicidin Axis: at the Crossroads between Protective Immunity and Pathological Inflammation during Infection, Immune Netw, doi:10.4110/in.2020.20.e12
Contreras-Bolívar, García-Fontana, García-Fontana, Torres, Vitamin D and COVID-19: where are we now?, Postgrad Med, doi:10.1080/00325481.2021.2017647
Dananché, Elias, Hénaff, Amour, Kuczewski et al., Baseline clinical features of COVID-19 patients, delay of hospital admission and clinical outcome: A complex relationship, PLoS One, doi:10.1371/journal.pone.0261428
Dancer, Parekh, Lax, Souza, Zheng et al., Vitamin D deficiency contributes directly to the acute respiratory distress syndrome (ARDS), Thorax, doi:10.1136/thoraxjnl-2014-206680
Dinicolantonio, Keefe, Magnesium and vitamin D deficiency as a potential cause of immune dysfunction, cytokine storm and disseminated intravascular coagulation in COVID-19 patients, Mo Med
Fakih, Trump, Johnson, Tian, Muindi et al., Chemotherapy is linked to severe vitamin D deficiency in patients with colorectal cancer, Int J Colorectal Dis, doi:10.1007/s00384-008-0593-y
Fox, Monroy-Iglesias, Aggarwal, Haire, Purushotham et al., Association between COVID-19 burden and delays to diagnosis and treatment of cancer patients in England, J Cancer Policy, doi:10.1016/j.jcpo.2021.100316
Gao, Ding, Dong, Zhang, Azkur et al., Risk factors for severe and critically ill COVID-19 patients: A review, Allergy, doi:10.1111/all.14657
Hafez, Commentary: Vitamin D status in relation to the clinical outcome of hospitalized COVID-19 patients, Front Med, doi:10.3389/fmed.2022.977540
Hastie, Mackay, Ho, Celis-Morales, Katikireddi et al., Vitamin D concentrations and COVID-19 infection in UK Biobank, Diabetes Metab Syndr, doi:10.1016/j.dsx.2020.04.050
Hastie, Pell, Sattar, Vitamin D and COVID-19 infection and mortality in UK Biobank, Eur J Nutr, doi:10.1007/s00394-020-02372-4
Health, Beattie, Health and Deprivation Published by Croom Helm 212pp £19, Nurs Stand, doi:10.7748/ns.2.17.34.s66
Henn, Martin-Gorgojo, Moreno, Vitamin D in Cancer Prevention: Gaps in Current Knowledge and Room for Hope, Nutrients, doi:10.3390/nu14214512
Hosseini, El Abd, Ducharme, Effects of Vitamin D Supplementation on COVID-19 Related Outcomes: A Systematic Review and Meta-Analysis, Nutrients, doi:10.3390/nu14102134
Ismailova, White, Vitamin D, infections and immunity, Rev Endocr Metab Disord, doi:10.1007/s11154-021-09679-5
Johannesen, Smeland, Aaserud, Buanes, Skog et al., COVID-19 in Cancer Patients, Risk Factors for Disease and Adverse Outcome, a Population-Based Study From Norway, Front Oncol, doi:10.3389/fonc.2021.652535
Jolliffe, Camargo, Jr, Sluyter, Aglipay et al., Vitamin D supplementation to prevent acute respiratory infections: a systematic review and meta-analysis of aggregate data from randomised controlled trials, Lancet Diabetes Endocrinol, doi:10.1016/S2213-8587(21)00051-6
Jude, Ling, Allcock, Yeap, Pappachan, Vitamin D Deficiency Is Associated With Higher Hospitalization Risk From COVID-19: A Retrospective Case-control Study, J Clin Endocrinol Metab, doi:10.1210/clinem/dgab439
Li, Huang, Zou, Yang, Hui et al., Epidemiology of COVID-19: A systematic review and meta-analysis of clinical characteristics, risk factors, and outcomes, J Med Virol, doi:10.1002/jmv.26424
Li, Van Geffen, Van Weele, Zhang, He et al., An observational and Mendelian randomisation study on vitamin D and COVID-19 risk in UK Biobank, Sci Rep, doi:10.1038/s41598-021-97679-5
Libon, Cavalier, Nikkels, Skin color is relevant to vitamin D synthesis, Dermatology, doi:10.1159/000354750
Lin, Mulick, Mathur, Smeeth, Warren-Gash et al., The association between vitamin D status and COVID-19 in England: A cohort study using UK Biobank, PLoS One, doi:10.1371/journal.pone.0269064
Ma, Zhou, Heianza, Qi, Habitual use of vitamin D supplements and risk of coronavirus disease 2019 (COVID-19) infection: a prospective study in UK Biobank, Am J Clin Nutr, doi:10.1093/ajcn/nqaa381
Magesh, John, Li, Li, Mattingly-App et al., Disparities in COVID-19 Outcomes by Race, Ethnicity, and Socioeconomic Status: A Systematic-Review and Meta-analysis, JAMA Netw Open, doi:10.1001/jamanetworkopen.2021.34147
Maigoro, Lee, Exploring the Link Between Vitamin D Deficiency and Cytokine Storms in COVID-19 Patients: An In Silico Analysis, J Med Food, doi:10.1089/jmf.2021.K.0085
Manson, Cook, Lee, Bassuk, Mora, Vitamin D Supplements and Prevention of Cancer and Cardiovascular Disease, N Engl J Med, doi:10.1056/NEJMoa1809944
Mathur, Rentsch, Morton, Hulme, Schultze et al., Ethnic differences in SARS-CoV-2 infection and COVID-19-related hospitalisation, intensive care unit admission, and death in 17 million adults in England: an observational cohort study using the OpenSAFELY platform, Lancet, doi:10.1016/S0140-6736(21)00634-6
Meltzer, Best, Zhang, Vokes, Arora et al., Association of Vitamin D Levels, Race/Ethnicity, and Clinical Characteristics With COVID-19 Test Results, JAMA Netw Open, doi:10.1001/jamanetworkopen.2021.4117
Mercola, Grant, Wagner, Evidence Regarding Vitamin D and Risk of COVID-19 and Its Severity, Nutrients, doi:10.3390/nu12113361
Monroy-Iglesias, Russell, Crawley, Allen, Travis et al., Metabolic syndrome biomarkers and prostate cancer risk in the UK Biobank, Int J Cancer, doi:10.1002/ijc.33255
Muñoz, Grant, Vitamin D and Cancer: An Historical Overview of the Epidemiology and Mechanisms, Nutrients, doi:10.3390/nu14071448
Nielsen, Junker, Boelt, Cohen, Munger et al., Vitamin D status and severity of COVID-19, Sci Rep, doi:10.1038/s41598-022-21513-9
Ogunniyi, Commodore-Mensah, Kc, Race, Ethnicity, Hypertension, and Heart Disease: JACC Focus Seminar 1/9, J Am Coll Cardiol, doi:10.1016/j.jacc.2021.06.017
Pal, Banerjee, Bhadada, Shetty, Singh et al., Vitamin D supplementation and clinical outcomes in COVID-19: a systematic review and meta-analysis, J Endocrinol Invest, doi:10.1007/s40618-021-01614-4
Pereira, Damascena, Azevedo, De Almeida Oliveira, Da et al., Vitamin D deficiency aggravates COVID-19: systematic review and meta-analysis, Crit Rev Food Sci Nutr, doi:10.1080/10408398.2020.1841090
Raisi-Estabragh, Mccracken, Bethell, Cooper, Cooper et al., Greater risk of severe COVID-19 in Black, Asian and Minority Ethnic populations is not explained by cardiometabolic, socioeconomic or behavioural factors, or by 25(OH)-vitamin D status: study of 1326 cases from the UK Biobank, J Public Health (Oxf), doi:10.1093/pubmed/fdaa095
Roel, Pistillo, Recalde, Fernández-Bertolín, Aragón et al., Cancer and the risk of coronavirus disease 2019 diagnosis, hospitalisation and death: A population-based multistate cohort study including 4 618 377 adults in Catalonia, Spain, Int J Cancer, doi:10.1002/ijc.33846
Santaolalla, Beckmann, Kibaru, Josephs, Van Hemelrijck et al., Association Between Vitamin D and Novel SARS-CoV-2 Respiratory Dysfunction -A Scoping Review of Current Evidence and Its Implication for COVID-19 Pandemic, Front Physiol, doi:10.3389/fphys.2020.564387
Shah, Saxena, Mavalankar, Vitamin D supplementation, COVID-19 and disease severity: a meta-analysis, QJM, doi:10.1093/qjmed/hcab009
Shortreed, Gray, Akosile, Walker, Fuller et al., Increased COVID-19 Infection Risk Drives Racial and Ethnic Disparities in Severe COVID-19 Outcomes, J Racial Ethn Health Disparities, doi:10.1007/s40615-021-01205-2
Smolders, Van Den Ouweland, Geven, Pickkers, Kox, Letter to the Editor: Vitamin D deficiency in COVID-19: Mixing up cause and consequence, Metabolism, doi:10.1016/j.metabol.2020.154434
Stockman, Wood, Anderson, Racial and Ethnic Differences in COVID-19 Outcomes, Stressors, Fear, and Prevention Behaviors Among US Women: Web-Based Cross-sectional Study, J Med Internet Res, doi:10.2196/26296
Subramanian, Griffin, Hewison, Hopkin, Kenny et al., Vitamin D and COVID-19-Revisited, J Intern Med, doi:10.1111/joim.13536
Sudlow, Gallacher, Allen, Beral, Burton et al., UK biobank: an open access resource for identifying the causes of a wide range of complex diseases of middle and old age, PLoS Med, doi:10.1371/journal.pmed.1001779
Teshome, Adane, Girma, Mekonnen, The Impact of Vitamin D Level on COVID-19 Infection: Systematic Review and Meta-Analysis, Front Public Health, doi:10.3389/fpubh.2021.624559
Vieth, Critique of Public Health Guidance for Vitamin D and Sun Exposure in the Context of Cancer and COVID-19, Anticancer Res, doi:10.21873/anticanres.16011
Webb, Kazantzidis, Kift, Farrar, Wilkinson et al., Colour Counts: Sunlight and Skin Type as Drivers of Vitamin D Deficiency at UK Latitudes, Nutrients, doi:10.3390/nu10040457
Yisak, Ewunetei, Kefale, Mamuye, Teshome et al., Effects of Vitamin D on COVID-19 Infection and Prognosis: A Systematic Review, Risk Manag Healthc Policy, doi:10.2147/RMHP.S291584
