Evaluation of vitamin D in COVID-19 patients
et al., 1st Samarra International Conference for Pure and Applied Sciences (SICPS2021), doi:10.1063/5.0122108, Nov 2022
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 136 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Case control study with 52 COVID-19 patients and 30 matched controls, showing significantly lower vitamin D levels in COVID-19 patients.
This is the 148th of 228 COVID-19 sufficiency studies for vitamin D, which collectively show higher levels reduce risk with p<0.0000000001.
|
risk of case, 41.6% lower, OR 0.58, p = 0.27, high D levels (≥10ng/ml) 30 of 52 (57.7%) cases,
21 of 30 (70.0%) controls, NNT 8.2, case control OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Khalil et al., 8 Nov 2022, retrospective, Iraq, peer-reviewed, 3 authors.
Evaluation of Vitamin D in COVID-19 Patients
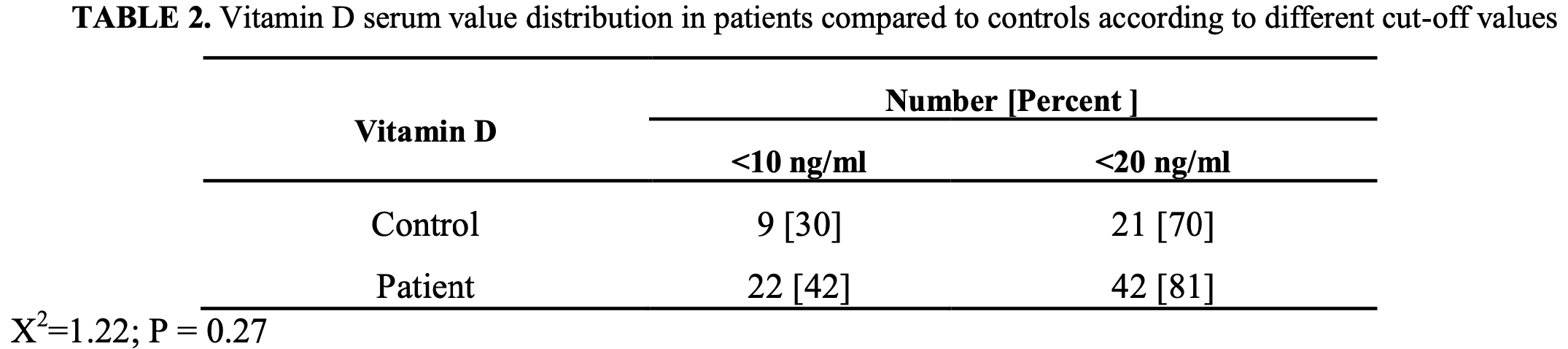
In a case-control study, fifty two subjects with COVID-19 were included in the study and 30 gender and age matched apparently healthy individuals were included as control. Vitamin D serum level determined by Mini Vidus, WBC, Lymphocytes and PCV by Swelab. CRP determined manually. SPSS package used for statistical analysis. Vitamin D mean serum level in COVID-19 subjects was significantly lower [P=0.007] than that in control group. Vitamin D mean serum value was lower than normal recommended value in patients with COVID-19. Additionally, the frequency of < 10 ng/ml was 30% in controls, while it was 42% in patients group. When the results stratified on < 20 ng/ml strata, controls show 70%, while patients corresponding value was 81%. The mean serum levels of vitamin D were higher in male compared to female, in smoker as compared to non-smoker and in patients with age of ≥ 50 years. However, the differences not reach significant values. There was inverse correlation between Vitamin D low serum levels and CRP levels indicating a significant association between disease severity and vitamin D serum levels. Serum vitamin D was higher in patients with chronic diseases than that in patients without chronic diseases history, however, the difference not reach significant level.
References
Abdollahi, Sarvestani, Rafat, Ghaderkhani, Mahmoudi-Aliabadi et al., None, Iran. J Med Virol, doi:10.1002/jmv.26726
Ahmed, Siman-Tov, Hall, Bhalla, Narayanan, None, Viruses, doi:10.3390/v11080704
Ali, None, Journal of Infection and Public Health, doi:10.1016/j.jiph.2020.06.021
Alipio, Vitamin D supplementation could possibly improve clinical outcomes of patients infected with coronavirus, SSRN Electron J
Almeida, Tyrrell, None, J Gen Virol, doi:10.1099/0022-1317-1-2-175
Alsamarai, Alobaidi, Alsamarai, None, AAJMS
Alsamarai, Alobaidi, Alsamarai, None, AAJMS
Alsamarai, None, AAJMS
Annweiler, Beaudenon, Gautier, Simon, Dubée et al., and on behalf of the COVIT-TRIAL study group, Trials, doi:10.1186/s13063-020-04928-5
Annweiler, Cao, Sabatier, None, Maturitas
Azhar, Madani, Ntoumi, Kock, Dar et al., None, Int. Journal Infect. Dis
Barlow, Svoboda, Mackellar, Nash, York et al., None, PLOS ONE, doi:10.1371/journal.pone.0025333
Baylink, Chen, Reeves, Xiao, Lacy et al., None, J Transl Med
Bilezikian, Bikle, Hewison, Lazaretti-Castro, Formenti et al., None, Eur J Endocrinol, doi:10.1530/EJE-20-0665
Bilezikian, Bikle, Hewison, Lazaretti-Castro, Formenti et al., None, European Eur J Endocrinol, doi:10.1530/EJE-20-0665
Bloom, Modlin, Myeloid Cells in Health and Disease
Boulkrane, Ilina, Melchakov, Fedotova, Drago et al., None, Front. Pharmacol, doi:10.3389/fphar.2020.604579
Brenner, Holleczek, Schöttker, None, Nutrients, doi:10.3390/nu12082488
Burt, Billington, Rose, Raymond, Hanley et al., None, JAMA
Ce Hastie, Mackay, Ho, Ca Celis-Morales, Katikireddi et al., None, Diabetes Metab. Syndr
Ce Hastie, Mackay, Ho, Ca Celis-Morales, Katikireddi et al., None, Diabetes Metab. Syndr, doi:10.1016/j.dsx.2020.04.050
Cereda, Bogliolo, Klersy, Lobascio, Masi et al., None, Clin Nutr, doi:10.1016/j.clnu.2020.10.055
Chan, Chan, None, J Thorac Dis, doi:10.1016/j.ijid.2020.01.009
Chan, None, J Thorac Dis
Chen, Wu, Guo, Cao, Huang et al., None, J Clin Invest, doi:10.1172/JCI137244
Chen, Xie, Yuan, Ma, Yu et al., None, MedRxiv
Christakos, Raval-Pandya, Wernyj, Yang, None, Biochem J, doi:10.1042/bj3160361
Correale, Ysrraelit, Gaitán, None, J.I
Cui, Xu, Li, Qiao, Han et al., None, Redox Biol, doi:10.1016/j.redox.2019.101295
Entrenas, Entrenas, Vaquero, Alcalá, López et al., None, J. Steroid Biochem. Mol. Biol
Faniyi, Lugg, Faustini, Webster, Duffy et al., None, Eur Respir J, doi:10.1183/13993003.04234-2020
Ferder, Martín Giménez, Inserra, Tajer, Antonietti et al., None, Am J Physiol Lung Cell Mol Physiol, doi:10.1152/ajplung.00186.2020
Fisher, Rahimzadeh, Brierley, Gration, Doree et al., None, PLOS ONE, doi:10.1371/journal.pone.0222313
Flanagan, Chiewchengchol, Wright, Edwards, Alswied et al., None, Inflamm. Bowel Dis, doi:10.1097/MIB.0000000000000387
Ganmaa, Uyanga, Zhou, Gantsetseg, Delgerekh et al., None, N Engl J Med
Grant, Lahore, Mcdonnell, Baggerly, French et al., None, Nutrients, doi:10.3390/nu12040988
Grant, Wagner, None, Nutrients
Griffin, Hewison, Hopkin, Kenny, Quinton et al., None, R. Soc. Open Sci, doi:10.1098/rsos.201912
Haider, Rothman-Ostrow, Osman, Arruda, Macfarlane-Berry et al., None, Front. Public Health, doi:10.3389/fpubh.2020.596944
Hastie, Pell, Sattar, None, Eur J Nutr
Hernández, Nan, Fernandez-Ayala, García-Unzueta, Hernández-Hernández et al., None, J Clin Endocrinol Metab
Hui, Azhar, Madani, Ntoumi, Kock et al., None, Int. J Infect Dis
Ilie, Stefanescu, Smith, None, Aging Clin Exp Res, doi:10.1007/s40520-020-01570-8
Jain, Chaurasia, Sengar, Singh, Mahor et al., None, Scientific Reports, doi:10.1038/s41598-020-77093-z
Kara, Ekiz, Ricci, Kara, Chang et al., None, Br J Nutr, doi:10.1017/S0007114520001749
Kaufman, Niles, Kroll, Bi, Holick, None, PLoS ONE
Liu, Sun, Wang, Zhang, Zhao et al., None, Int. J Infect Dis
Mackenzie, Smith, Mackenzie, Smith, None, Microbiol. Aust, doi:10.1071/MA20013
Maghbooli, Sahraian, Ebrahimi, Pazoki, Kafan et al., None, PLOS ONE, doi:10.1371/journal.pone.0239799
Mariani, Giménez, Bergam, Tajer, Antonietti et al., None, Health Security
Mariani, Giménez, Bergam, Tajer, Antonietti et al., None, Health Security
Martineau, Jolliffe, Greenberg, Aloia, Bergman et al., None, Health Technology Assessment, doi:10.3310/hta23020
Meltzer, Best, Zhang, Vokes, Arora et al., None, JAMA Netw Open
Mercola, Grant, Wagner, None, Nutrients
Merzon, Tworowski, Gorohovski, Vinker, Cohen et al., None, The FEBS Journal
Michos, Cainzos-Achirica, None, JAMA Network Open, doi:10.1001/jamanetworkopen.2021.0431
Nwosu, Kum-Nji, None, PLOS ONE, doi:10.1371/journal.pone.0205342
O'shea, Griffin, Brennan, Mulkerrin, None, J Nutr Sci, doi:10.1017/jns.2020.36
Panagiotou, Tee, Ihsan, Athar, Marchitelli et al., None, Clinical Endocrinology, doi:10.1111/cen.14276
Panfili, Roversi, D'argenio, Rossi, Cappa et al., None, J Endocrinol Invest, doi:10.1007/s40618-020-01327-0
Parekh, Patel, Scott, Lax, Dancer et al., None, Crit Care Med, doi:10.1097/CCM.0000000000002095
Pinzon, Angela, Pradana, None, Trop Med Health, doi:10.1186/s41182-020-00277-w
Radujkovic, Hippchen, Tiwari-Heckler, Dreher, Boxberger et al., None, Nutrients, doi:10.3390/nu12092757
Raharusun, Priambada, Budiarti, Agung, Budi, None, SSRN Journal
Rahimzadeh, Brierley, Gration, Doree, Kimber et al., None, plos one
Raisi-Estabragh, Mccracken, Bethell, Cooper, Cooper et al., None, J Public Health (Oxf), doi:10.1093/pubmed/fdaa095
Rodríguez, Montelongo, Martínez-Cuazitl, Puente, Reyes, None, Rev Sanid Milit Mex
Rodríguez, Montelongo, Martínez-Cuazitl, Puente, Reyes, None, Review Milit Mex
Santos, Maeda, Jardim, Lazaretti-Castro, Santos et al., None, Arch Endocrinol Metab
Schögler, Muster, Kieninger, Casaulta, Tapparel et al., None, European Respiratory Journal, doi:10.1183/13993003.00665-2015
Siuka, Pfeifer, Pinter, None, Mayo Clin Proc
Spiro, Buttriss, None, Nutr. Bull
Telcian, Zdrenghea, Edwards, Laza-Stanca, Mallia et al., None, Antiviral Res, doi:10.1016/j.antiviral.2016.11.004
Tsujino, Ushikoshi-Nakayama, Yamazaki, Matsumoto, Saito, None, J. Clin. Biochem. Nutr, doi:10.3164/jcbn.19-48
Vo, Koppel, Espinola, Mansbach, Celedón et al., None, J. Pediatr, doi:10.1016/j.jpeds.2018.07.097
Weir, Thenappan, Bhargava, Chen, None, Clin Med, doi:10.7861/clinmed.2020-0301
Who, WHO Coronavirus Disease (COVID-19) Dashboard
Who, WHO statement regarding cluster of pneumonia cases in Wuhan, China
Xu, Baylink, Chen, Reeves, Xiao et al., None, J Transl Med, doi:10.1186/s12967-020-02488-5
Ye, Tang, Liao, Shaw, Deng et al., None, J Am Coll Nutr
Yisak, Ewunetei, Kefale, Mamuye, Teshome et al., None, Risk Manag Healthc Policy, doi:10.2147/RMHP.S291584
Zdrenghea, Makrinioti, Bagacean, Bush, Johnston et al., None, Reviews in Medical Virology, doi:10.1002/rmv.1909
Zhang, Leung, Richers, Liu, Remigio et al., None, J. Immunol, doi:10.4049/jimmunol.1102412
DOI record:
{
"DOI": "10.1063/5.0122108",
"ISSN": [
"0094-243X"
],
"URL": "http://dx.doi.org/10.1063/5.0122108",
"author": [
{
"affiliation": [],
"family": "Khalil",
"given": "Mohammed Ahmed",
"sequence": "first"
},
{
"affiliation": [],
"family": "Alobaidi",
"given": "Amina Hamed",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Al-Samarrai",
"given": "Abdulmonaim Hamad",
"sequence": "additional"
}
],
"container-title": "1ST SAMARRA INTERNATIONAL CONFERENCE FOR PURE AND APPLIED SCIENCES (SICPS2021): SICPS2021",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2022,
11,
9
]
],
"date-time": "2022-11-09T01:30:26Z",
"timestamp": 1667957426000
},
"deposited": {
"date-parts": [
[
2022,
11,
9
]
],
"date-time": "2022-11-09T01:40:23Z",
"timestamp": 1667958023000
},
"event": "1ST SAMARRA INTERNATIONAL CONFERENCE FOR PURE AND APPLIED SCIENCES (SICPS2021): SICPS2021",
"indexed": {
"date-parts": [
[
2022,
11,
9
]
],
"date-time": "2022-11-09T05:50:29Z",
"timestamp": 1667973029572
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2022
]
]
},
"link": [
{
"URL": "http://aip.scitation.org/doi/pdf/10.1063/5.0122108",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "317",
"original-title": [],
"prefix": "10.1063",
"published": {
"date-parts": [
[
2022
]
]
},
"published-print": {
"date-parts": [
[
2022
]
]
},
"publisher": "AIP Publishing",
"reference": [
{
"DOI": "10.32441/aajms.3.2.12",
"doi-asserted-by": "crossref",
"key": "10.1063/5.0122108_c1",
"unstructured": "A.G.M Alsamarai, AAJMS 3, 1 (2020)."
},
{
"DOI": "10.32441/aajms.3.2.13",
"doi-asserted-by": "crossref",
"key": "10.1063/5.0122108_c2",
"unstructured": "A.G.M. Alsamarai, A.H.A. Alobaidi, M.M. Alsamarai, AAJMS 3, 151 (2020)."
},
{
"DOI": "10.3389/fpubh.2020.596944",
"doi-asserted-by": "publisher",
"key": "10.1063/5.0122108_c3"
},
{
"DOI": "10.1071/MA20013",
"doi-asserted-by": "publisher",
"key": "10.1063/5.0122108_c4"
},
{
"DOI": "10.1099/0022-1317-1-2-175",
"doi-asserted-by": "publisher",
"key": "10.1063/5.0122108_c5"
},
{
"key": "10.1063/5.0122108_c6",
"unstructured": "P.K.S. Chan and M.C.W. Chan, J Thorac Dis 5, S118 (2013)."
},
{
"DOI": "10.1016/j.ijid.2020.01.009",
"doi-asserted-by": "publisher",
"key": "10.1063/5.0122108_c7"
},
{
"key": "10.1063/5.0122108_c8",
"unstructured": "WHO. WHO statement regarding cluster of pneumonia cases in Wuhan, China (World Health Organization, January 9, 2020); Emergencies: Novel coronavirus 2019 (World Health Organization))"
},
{
"key": "10.1063/5.0122108_c9",
"unstructured": "WHO. WHO Coronavirus Disease (COVID-19) Dashboard. https://covid19.who.int/."
},
{
"DOI": "10.32441/aajms.3.2.12",
"doi-asserted-by": "crossref",
"key": "10.1063/5.0122108_c10",
"unstructured": "A.G.M. Alsamarai, A.H.A. Alobaidi, M.M. Alsamarai, AAJMS 3,159 (2020)."
},
{
"key": "10.1063/5.0122108_c11",
"unstructured": "NIH. COVOD-19 treatment guidelines. Therapeutic Management of Adults With COVID-19. https://www.covid19treatmentguidelines.nih.gov/therapeutic-management/. ]"
},
{
"DOI": "10.1001/jamanetworkopen.2021.0431",
"doi-asserted-by": "publisher",
"key": "10.1063/5.0122108_c12"
},
{
"DOI": "10.1186/s13063-020-04928-5",
"doi-asserted-by": "publisher",
"key": "10.1063/5.0122108_c13"
},
{
"key": "10.1063/5.0122108_c14",
"unstructured": "R.N. dos Santos, S.S. Maeda, J.R. Jardim, M. Lazaretti-Castro, R.N. dos Santos, S.S. Maeda, J.R. Jardim, and M. Lazaretti-Castro, Arch Endocrinol Metab 64, 498 (2020)."
},
{
"DOI": "10.1016/j.ijid.2020.01.009",
"doi-asserted-by": "crossref",
"key": "10.1063/5.0122108_c15",
"unstructured": "E.I. Azhar, T.A. Madani, F. Ntoumi, R. Kock, O. Dar, G. Ippolito, T.D. Mchugh, Z.A. Memish, C. Drosten, A. Zumla, and E. Petersen, Int. Journal Infect. Dis 91, 264 (2021)."
},
{
"DOI": "10.3310/hta23020",
"doi-asserted-by": "publisher",
"key": "10.1063/5.0122108_c16"
},
{
"DOI": "10.1016/j.jpeds.2018.07.097",
"doi-asserted-by": "publisher",
"key": "10.1063/5.0122108_c17"
},
{
"DOI": "10.3390/nu12082488",
"doi-asserted-by": "publisher",
"key": "10.1063/5.0122108_c18"
},
{
"DOI": "10.1530/EJE-20-0665",
"doi-asserted-by": "publisher",
"key": "10.1063/5.0122108_c19"
},
{
"DOI": "10.1128/9781555819194.ch41",
"doi-asserted-by": "crossref",
"key": "10.1063/5.0122108_c20",
"unstructured": "R. Bloom and R.L. Modlin, in Myeloid Cells in Health and Disease (John Wiley & Sons, Ltd, 2017), pp. 727–738."
},
{
"DOI": "10.1097/MIB.0000000000000387",
"doi-asserted-by": "publisher",
"key": "10.1063/5.0122108_c21"
},
{
"key": "10.1063/5.0122108_c22",
"unstructured": "D.J. Baylink, C.-S. Chen, M.E. Reeves, J. Xiao, C. Lacy and H. Cao, J Transl Med 18,322 (2021)."
},
{
"DOI": "10.3390/v11080704",
"doi-asserted-by": "publisher",
"key": "10.1063/5.0122108_c23"
},
{
"DOI": "10.1016/j.antiviral.2016.11.004",
"doi-asserted-by": "publisher",
"key": "10.1063/5.0122108_c24"
},
{
"DOI": "10.1183/13993003.00665-2015",
"doi-asserted-by": "publisher",
"key": "10.1063/5.0122108_c25"
},
{
"DOI": "10.1371/journal.pone.0025333",
"doi-asserted-by": "publisher",
"key": "10.1063/5.0122108_c26"
},
{
"DOI": "10.1007/s40618-020-01327-0",
"doi-asserted-by": "publisher",
"key": "10.1063/5.0122108_c27"
},
{
"DOI": "10.1002/rmv.1909",
"doi-asserted-by": "publisher",
"key": "10.1063/5.0122108_c28"
},
{
"DOI": "10.4049/jimmunol.1102412",
"doi-asserted-by": "publisher",
"key": "10.1063/5.0122108_c29"
},
{
"DOI": "10.3164/jcbn.19-48",
"doi-asserted-by": "publisher",
"key": "10.1063/5.0122108_c30"
},
{
"DOI": "10.1097/CCM.0000000000002095",
"doi-asserted-by": "publisher",
"key": "10.1063/5.0122108_c31"
},
{
"key": "10.1063/5.0122108_c32",
"unstructured": "Rodríguez, M.E. Montelongo , A. Martínez-Cuazitl, N.A.V. Puente, P.R. Reyes, Review Milit Mex.74, 1(2021)."
},
{
"DOI": "10.4049/jimmunol.1000588",
"doi-asserted-by": "crossref",
"key": "10.1063/5.0122108_c33",
"unstructured": "J. Correale, M.C. Ysrraelit, and M.I. Gaitán, J.I. 185, 4948 (2010)."
},
{
"DOI": "10.1098/rsos.201912",
"doi-asserted-by": "publisher",
"key": "10.1063/5.0122108_c34"
},
{
"DOI": "10.1042/bj3160361",
"doi-asserted-by": "publisher",
"key": "10.1063/5.0122108_c35"
},
{
"DOI": "10.1152/ajplung.00186.2020",
"doi-asserted-by": "publisher",
"key": "10.1063/5.0122108_c36"
},
{
"key": "10.1063/5.0122108_c37",
"unstructured": "M.C.W. Chan, J Thorac Dis 5, S118 (2014)."
},
{
"DOI": "10.7861/clinmed.2020-0301",
"doi-asserted-by": "publisher",
"key": "10.1063/5.0122108_c38"
},
{
"DOI": "10.1172/JCI137244",
"doi-asserted-by": "publisher",
"key": "10.1063/5.0122108_c39"
},
{
"DOI": "10.1371/journal.pone.0222313",
"doi-asserted-by": "publisher",
"key": "10.1063/5.0122108_c40"
},
{
"DOI": "10.1016/j.redox.2019.101295",
"doi-asserted-by": "publisher",
"key": "10.1063/5.0122108_c41"
},
{
"DOI": "10.1186/s12967-020-02488-5",
"doi-asserted-by": "publisher",
"key": "10.1063/5.0122108_c42"
},
{
"key": "10.1063/5.0122108_c43",
"unstructured": "M. Rahimzadeh, C. Brierley, B. Gration, C. Doree, C.E. Kimber, A.P. Cajide, A.A. Lamikanra, and D.J. Roberts, plos one . (2019)."
},
{
"DOI": "10.1017/jns.2020.36",
"doi-asserted-by": "publisher",
"key": "10.1063/5.0122108_c44"
},
{
"DOI": "10.1016/j.jiph.2020.06.021",
"doi-asserted-by": "publisher",
"key": "10.1063/5.0122108_c45"
},
{
"DOI": "10.1530/EJE-20-0665",
"doi-asserted-by": "publisher",
"key": "10.1063/5.0122108_c46"
},
{
"key": "10.1063/5.0122108_c47",
"unstructured": "J. Mariani, V.M.M. Giménez, I. Bergam, C. Tajer, L. Antonietti, F. Inserra, L. Ferder, and W. Manucha, Health Security (2020)."
},
{
"DOI": "10.1016/j.clnu.2020.10.055",
"doi-asserted-by": "publisher",
"key": "10.1063/5.0122108_c48"
},
{
"key": "10.1063/5.0122108_c49",
"unstructured": "T.A. Rodríguez , M.E. Montelongo , A. Martínez-Cuazitl, N.A.V. Puente, P.R. Reyes, Rev Sanid Milit Mex.74, 1(2020)."
},
{
"DOI": "10.1183/13993003.04234-2020",
"doi-asserted-by": "publisher",
"key": "10.1063/5.0122108_c50"
},
{
"DOI": "10.1002/jmv.26726",
"doi-asserted-by": "publisher",
"key": "10.1063/5.0122108_c51"
},
{
"DOI": "10.1371/journal.pone.0239799",
"doi-asserted-by": "publisher",
"key": "10.1063/5.0122108_c52"
},
{
"DOI": "10.1186/s41182-020-00277-w",
"doi-asserted-by": "publisher",
"key": "10.1063/5.0122108_c53"
},
{
"DOI": "10.1017/S0007114520001749",
"doi-asserted-by": "publisher",
"key": "10.1063/5.0122108_c54"
},
{
"DOI": "10.3390/nu12040988",
"doi-asserted-by": "publisher",
"key": "10.1063/5.0122108_c55"
},
{
"key": "10.1063/5.0122108_c56",
"unstructured": "K. Ye, F. Tang, X. Liao, B.A. Shaw, M. Deng, G. Huang, Z. Qin, X. Peng, H. Xiao, C. Chen, X. Liu, L. Ning, B. Wang, N. Tang, M. Li, F. Xu, S. Lin, and J. Yang, J Am Coll Nutr 0, 1 (2020)."
},
{
"DOI": "10.1016/j.dsx.2020.04.050",
"doi-asserted-by": "publisher",
"key": "10.1063/5.0122108_c57"
},
{
"key": "10.1063/5.0122108_c58",
"unstructured": "J.L. Hernández, D. Nan, M. Fernandez-Ayala, M. García-Unzueta, M.A. Hernández-Hernández, M. López- Hoyos, P. Muñoz-Cacho, J.M. Olmos, M. Gutiérrez-Cuadra, J.J. Ruiz-Cubillán, J. Crespo, and V.M. Martínez-Taboada, J Clin Endocrinol Metab (2020)."
},
{
"DOI": "10.1038/s41598-020-77093-z",
"doi-asserted-by": "publisher",
"key": "10.1063/5.0122108_c59"
},
{
"key": "10.1063/5.0122108_c60",
"unstructured": "P. Raharusun, S. Priambada, C. Budiarti, E. Agung, and C. Budi, SSRN Journal (2020)."
},
{
"DOI": "10.1371/journal.pone.0205342",
"doi-asserted-by": "publisher",
"key": "10.1063/5.0122108_c61"
},
{
"key": "10.1063/5.0122108_c62",
"unstructured": "W.B. Grant, C.L. Wagner, Nutrients. (2021)."
},
{
"DOI": "10.1111/cen.14276",
"doi-asserted-by": "publisher",
"key": "10.1063/5.0122108_c63"
},
{
"DOI": "10.3390/nu12092757",
"doi-asserted-by": "publisher",
"key": "10.1063/5.0122108_c64"
},
{
"key": "10.1063/5.0122108_c65",
"unstructured": "J. Mariani, V.M.M. Giménez, I. Bergam, C. Tajer, L. Antonietti, F. Inserra, L. Ferder, and W. Manucha, Health Security (2020)."
},
{
"DOI": "10.1016/j.maturitas.2020.06.003",
"doi-asserted-by": "crossref",
"key": "10.1063/5.0122108_c66",
"unstructured": "C. Annweiler, Z. Cao, and J.-M. Sabatier, jMaturitas 140, 24 (2020)."
},
{
"DOI": "10.1007/s40520-020-01570-8",
"doi-asserted-by": "publisher",
"key": "10.1063/5.0122108_c67"
},
{
"DOI": "10.3389/fphar.2020.604579",
"doi-asserted-by": "publisher",
"key": "10.1063/5.0122108_c68"
},
{
"DOI": "10.2147/RMHP.S291584",
"doi-asserted-by": "publisher",
"key": "10.1063/5.0122108_c69"
},
{
"DOI": "10.1093/pubmed/fdaa095",
"doi-asserted-by": "publisher",
"key": "10.1063/5.0122108_c70"
},
{
"DOI": "10.1016/j.dsx.2020.04.050",
"doi-asserted-by": "crossref",
"key": "10.1063/5.0122108_c71",
"unstructured": "CE Hastie, DF Mackay, F Ho, CA Celis-Morales, SV Katikireddi, CL Niedzwiedz, B.D. Jani, P. Welsh, F.S. Mair, S.R. Gray, and C.A.O'Donnell, Diabetes Metab. Syndr 14, 561 (2020)."
},
{
"DOI": "10.1016/j.ijid.2020.12.077",
"doi-asserted-by": "crossref",
"key": "10.1063/5.0122108_c72",
"unstructured": "N. Liu, J. Sun, X. Wang, T. Zhang, M. Zhao, and H. Li, Int. J Infect Dis.104:58-64(2021)."
},
{
"key": "10.1063/5.0122108_c73",
"unstructured": "J. Chen, L. Xie, P. Yuan, J. Ma, P. Yu, C. Zheng, and X. Liu, MedRxiv 2020.10.24.20218974 (2020)."
},
{
"DOI": "10.2139/ssrn.3571484",
"doi-asserted-by": "crossref",
"key": "10.1063/5.0122108_c74",
"unstructured": "M. Alipio, Vitamin D supplementation could possibly improve clinical outcomes of patients infected with coronavirus-2019 (COVID-2019). SSRN Electron J. (2020)."
},
{
"DOI": "10.3390/nu12113361",
"doi-asserted-by": "crossref",
"key": "10.1063/5.0122108_c75",
"unstructured": "J. Mercola, W.B. Grant, C.L. Wagner, Nutrients.12, 3361(2020)."
},
{
"DOI": "10.1016/j.mayocp.2020.05.036",
"doi-asserted-by": "crossref",
"key": "10.1063/5.0122108_c76",
"unstructured": "D. Siuka, M. Pfeifer, B. Pinter, Mayo Clin Proc, 95, 1804 (2020)."
},
{
"DOI": "10.1111/nbu.12108",
"doi-asserted-by": "crossref",
"key": "10.1063/5.0122108_c77",
"unstructured": "A. Spiro, JL. Buttriss, Nutr. Bull. 39, 322 (2014)."
},
{
"DOI": "10.1007/s00394-020-02372-4",
"doi-asserted-by": "crossref",
"key": "10.1063/5.0122108_c78",
"unstructured": "C.E. Hastie, J.P. Pell, and N. Sattar, Eur J Nutr 60, 545 (2021).."
},
{
"DOI": "10.1111/febs.15495",
"doi-asserted-by": "crossref",
"key": "10.1063/5.0122108_c79",
"unstructured": "E. Merzon, D. Tworowski, A. Gorohovski, S. Vinker, A.G. Cohen, I. Green, and M. Frenkel-Morgenstern, The FEBS Journal 287, 3693 (2020).."
},
{
"DOI": "10.1001/jamanetworkopen.2020.19722",
"doi-asserted-by": "crossref",
"key": "10.1063/5.0122108_c80",
"unstructured": "D.O. Meltzer, T.J. Best, H. Zhang, T. Vokes, V. Arora, and J. Solway, JAMA Netw Open 3, e2019722 (2020)."
},
{
"DOI": "10.1371/journal.pone.0239252",
"doi-asserted-by": "crossref",
"key": "10.1063/5.0122108_c81",
"unstructured": "H.W. Kaufman, J.K. Niles, M.H. Kroll, C. Bi, and M.F. Holick, PLoS ONE 15, e0239252 (2020)."
},
{
"DOI": "10.1016/j.jsbmb.2020.105751",
"doi-asserted-by": "crossref",
"key": "10.1063/5.0122108_c82",
"unstructured": "C.M. Entrenas, C.L.M. Entrenas, B.J.M. Vaquero, D.J.F. Alcalá, M.J. López, R. Bouillon, and J.M.Q. Gomez, J. Steroid Biochem. Mol. Biol 203, 105751 (2020)."
},
{
"key": "10.1063/5.0122108_c83",
"unstructured": "European Centre for Disease Prevention and Control. 2020 Considerations relating to social distancing measures in response to COVID-19 –second update. Stockholm, Sweden: ECDC. Seehttps://www.ecdc. europa. eu/ sites/default/files/documents/covid-19-social-distancing-measuresgguide-second-update.pdf. Accessed 5 March (2021)."
},
{
"DOI": "10.1056/NEJMoa1915176",
"doi-asserted-by": "crossref",
"key": "10.1063/5.0122108_c84",
"unstructured": "D. Ganmaa, B. Uyanga, X. Zhou, G. Gantsetseg, B. Delgerekh, D. Enkhmaa, D. Khulan, S. Ariunzaya, E. Sumiya, B. Bolortuya, J. Yanjmaa, T. Enkhtsetseg, A. Munkhzaya, M. Tunsag, P. Khudyakov, J.A. Seddon, B.J. Marais, O. Batbayar, G. Erdenetuya, B. Amarsaikhan, D. Spiegelman, J. Tsolmon, and A.R. Martineau, N Engl J Med 383, 359 (2020)."
},
{
"DOI": "10.1001/jama.2019.11889",
"doi-asserted-by": "crossref",
"key": "10.1063/5.0122108_c85",
"unstructured": "L.A. Burt, E.O. Billington, M.S. Rose, D.A. Raymond, D.A. Hanley, and S.K. Boyd, JAMA 322, 736 (2019)."
},
{
"key": "10.1063/5.0122108_c86",
"unstructured": "Scientific advisory committee on nutrition (SACN). Vitamin D and Health. 2016. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/537616/SACN_Vitamin_D_and_Health_report.pdf (accessed 5 March 2021)."
}
],
"reference-count": 86,
"references-count": 86,
"relation": {},
"resource": {
"primary": {
"URL": "http://aip.scitation.org/doi/abs/10.1063/5.0122108"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subtitle": [],
"title": "Evaluation of vitamin D in COVID-19 patients",
"type": "proceedings-article"
}
