Polypharmacy and Proton Pump Inhibitor Use Independently Predict One-Year Mortality in Critical COVID-19: An Explainable AI–Based Survival Analysis
et al., medRxiv, doi:10.1101/2025.10.27.25338863, Oct 2025
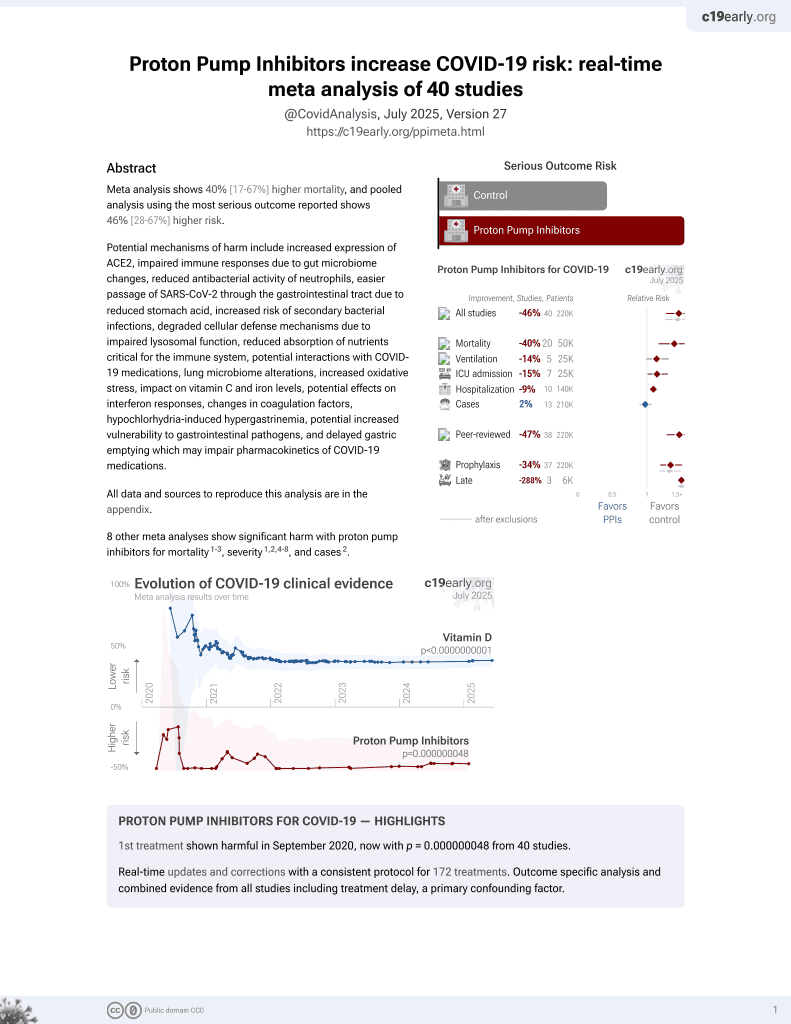
PPIs for COVID-19
1st treatment shown to increase risk in
September 2020, now with p = 0.000000048 from 40 studies.
6,400+ studies for
210+ treatments. c19early.org
|
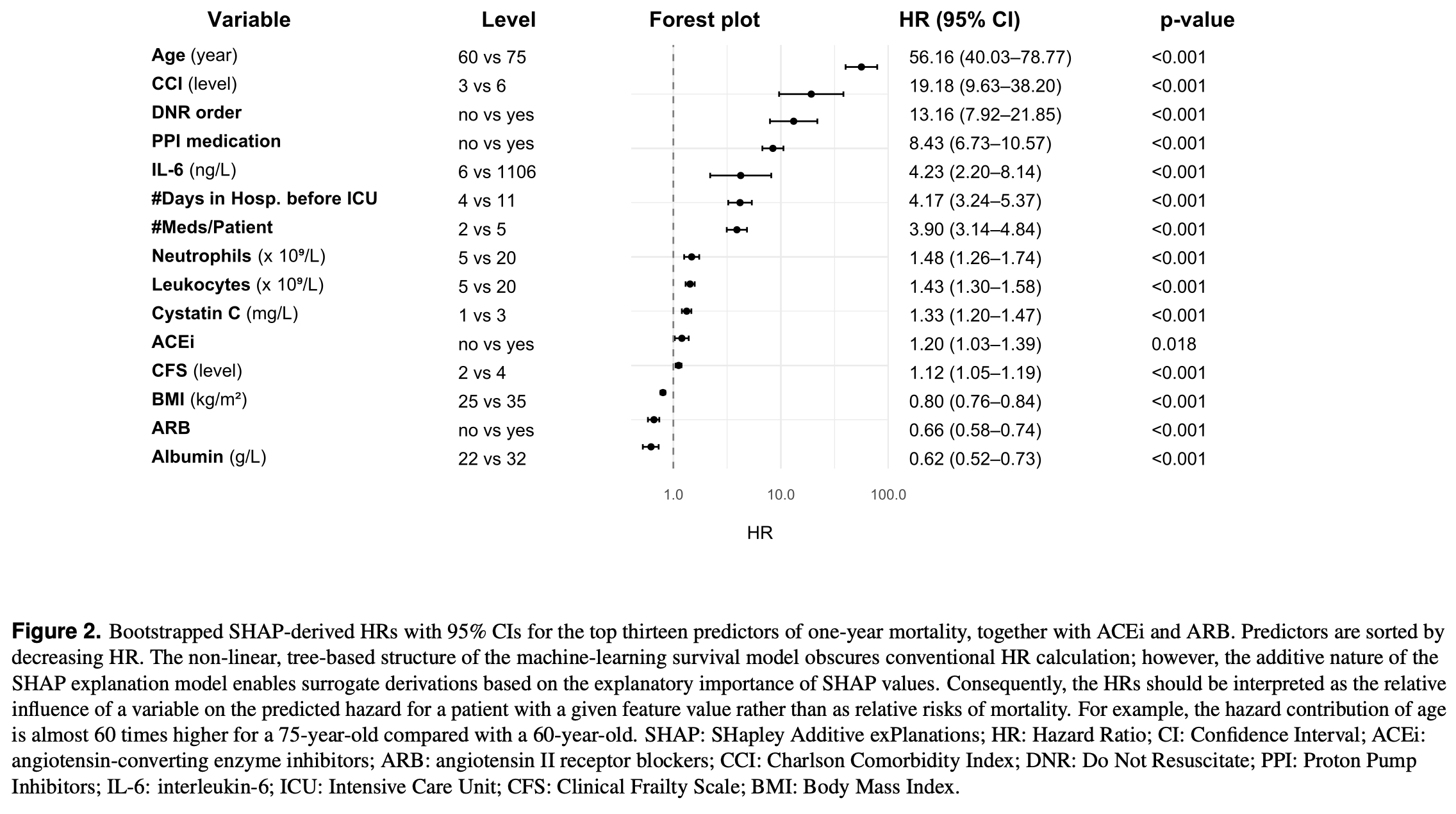
Retrospective 497 critically ill COVID-19 patients in Swedish ICUs showing proton pump inhibitor use associated with higher one-year mortality. The machine-learning survival model obscures conventional HR calculation; however, the additive nature of the
SHAP explanation model enables surrogate derivations based on the explanatory importance of SHAP values. The HR should be interpreted as the relative influence on the predicted hazard rather than the relative risk for mortality.
SHAP explanation model enables surrogate derivations based on the explanatory importance of SHAP values. The HR should be interpreted as the relative influence on the predicted hazard rather than the relative risk for mortality.
|
risk of death, 743.0% higher, HR 8.43, p < 0.001, treatment 104, control 393, SHAP-derived HR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Hjärtström et al., 28 Oct 2025, retrospective, Sweden, preprint, median age 66.0, 6 authors, study period May 2020 - May 2021.
Contact: malin.hjartstrom@med.lu.se.
Polypharmacy and Proton Pump Inhibitor Use Independently Predict One-Year Mortality in Critical COVID-19: An Explainable AI–Based Survival Analysis
doi:10.1101/2025.10.27.25338863
Mortality among patients admitted to intensive care with coronavirus disease 2019 (COVID-19) remains substantial despite advances in management. The contribution of pre-admission medication profiles to long-term survival is poorly defined. We analysed 497 adults with confirmed COVID-19 admitted to six intensive care units in southern Sweden between May 2020 and May 2021. Clinical and laboratory data were combined with prescription information from the national drug registry; drugs dispensed at least twice within eight months before admission were classified by Anatomical Therapeutic Chemical code. Polypharmacy was defined as the use of five or more medications. An XGBoost survival model with a Cox partial-likelihood objective was trained to predict one-year mortality and interpreted using SHapley Additive exPlanations (SHAP). The model achieved a concordance index of 0.74. Age was the strongest predictor of mortality, followed by the number of medications per patient, which ranked above the Charlson Comorbidity Index and Clinical Frailty Scale. Proton pump inhibitors were the only individual drug class among the top predictors, showing a modest positive association with mortality, whereas angiotensin-converting enzyme inhibitors and angiotensin II receptor blockers had negligible contributions. These findings identify cumulative medication burden as an independent and clinically relevant marker of vulnerability in critical COVID-19.
Author contributions statement
Additional information The authors declare no competing interests.
References
Akiba, Sano, Yanase, Ohta, Koyama et al., A next-generation hyperparameter optimization framework
Almario, Chey, Spiegel, Increased risk of COVID-19 among users of proton pump inhibitors, The Am. J. Gastroenterol, doi:10.14309/ajg.0000000000000798
Chen, Guestrin, XGBoost: A scalable tree boosting system, doi:10.1145/2939672.2939785
Clemente-Moragón, Metoprolol in critically ill patients with COVID-19, J. Am. Coll. Cardiol
Didriksson, Intensive care unit burden is associated with increased mortality in critically ill COVID-19 patients, Acta Anaesthesiol. Scand, doi:10.1111/aas.14184
Halpin, Singh, Hadfield, Inhaled corticosteroids and COVID-19: a systematic review and clinical perspective, Eur. Respir. J, doi:10.1183/13993003.01009-2020
Imhann, Proton pump inhibitors affect the gut microbiome, Gut, doi:10.1136/gutjnl-2015-310376
Kow, Ramachandram, Hasan, Clinical outcomes of hypertensive patients with COVID-19 receiving calcium channel blockers: a systematic review and meta-analysis, Hypertens. Res
Lee, Severe clinical outcomes of COVID-19 associated with proton pump inhibitors: a nationwide cohort study with propensity score matching, Gut
Lundberg, Lee, A unified approach to interpreting model predictions
Mancia, Rea, Ludergnani, Apolone, Corrao, Renin-angiotensin-aldosterone system blockers and the risk of Covid-19, New Engl. J. Medicine, doi:10.1056/NEJMoa2006923
Maret-Ouda, Panula, Santoni, Xie, Lagergren, Proton pump inhibitor use and risk of pneumonia: a self-controlled case series study, J. Gastroenterol
Masnoon, Shakib, Kalisch-Ellett, Caughey, What is polypharmacy? A systematic review of definitions, BMC Geriatr
Palmowski, Persistent mortality in critical COVID-19 ICU cases from wild-type to delta variant: A descriptive cohort study, Sci. Reports, doi:10.1038/s41598-025-94483-3
Park, Kwak, Park, Heo, Lee, Association of dipeptidyl peptidase-4 inhibitor use with COVID-19 mortality in diabetic patients: A nationwide cohort study in korea, J. Clin. Medicine
Reynolds, Adhikari, Pulgarin, Renin-angiotensin-aldosterone system inhibitors and risk of Covid-19, New Engl. J. Medicine, doi:10.1056/NEJMoa2008975
Schultze, Walker, Mackenna, Risk of COVID-19-related death among patients with chronic respiratory diseases prescribed inhaled corticosteroids: an observational cohort study using opensafely, The Lancet Respir. Medicine, doi:10.1016/S2213-2600(20)30415-X
Seo, Impact of prior vaccination on clinical outcomes of patients with COVID-19, Emerg. microbes & infections, doi:10.1080/22221751.2022.2069516
Singh, Mortality and severity in COVID-19 patients on ACEIs and ARBs-a systematic review, meta-analysis, and meta-regression analysis, Front. Medicine, doi:10.3389/fmed.2021.703661
Solerte, D'addio, Trevisan, Sitagliptin treatment at the time of hospitalization was associated with reduced mortality in patients with type 2 diabetes and COVID-19: A multicenter, case-control, retrospective, observational study, Diabetes Care, doi:10.2337/dc20-1521
Sundrani, Lu, Computing the hazard ratios associated with explanatory variables using machine learning models of survival data, JCO Clin. Cancer Informatics, doi:10.1200/CCI.20.00172
Vaduganathan, Renin-angiotensin-aldosterone system inhibitors in patients with Covid-19, New Engl. J. Medicine, doi:10.1056/NEJMsr2005760
Van Buuren, Multiple imputation of discrete and continuous data by fully conditional specification, Stat. Methods Med. Res
Van Diepen, Association between vaccination status and outcomes in patients admitted to the ICU with COVID-19, Critical care medicine, doi:10.1097/CCM.0000000000005928
DOI record:
{
"DOI": "10.1101/2025.10.27.25338863",
"URL": "http://dx.doi.org/10.1101/2025.10.27.25338863",
"abstract": "<jats:p>Mortality among patients admitted to intensive care with coronavirus disease 2019 (COVID-19) remains substantial despite advances in management. The contribution of pre-admission medication profiles to long-term survival is poorly defined. We analysed 497 adults with confirmed COVID-19 admitted to six intensive care units in southern Sweden between May 2020 and May 2021. Clinical and laboratory data were combined with prescription information from the national drug registry; drugs dispensed at least twice within eight months before admission were classified by Anatomical Therapeutic Chemical code. Polypharmacy was defined as the use of five or more medications. An XGBoost survival model with a Cox partial-likelihood objective was trained to predict one-year mortality and interpreted using SHapley Additive exPlanations (SHAP). The model achieved a concordance index of 0.74. Age was the strongest predictor of mortality, followed by the number of medications per patient, which ranked above the Charlson Comorbidity Index and Clinical Frailty Scale. Proton pump inhibitors were the only individual drug class among the top predictors, showing a modest positive association with mortality, whereas angiotensin-converting enzyme inhibitors and angiotensin II receptor blockers had negligible contributions. These findings identify cumulative medication burden as an independent and clinically relevant marker of vulnerability in critical COVID-19.</jats:p>",
"accepted": {
"date-parts": [
[
2025,
10,
28
]
]
},
"author": [
{
"ORCID": "https://orcid.org/0000-0002-5294-8472",
"affiliation": [],
"authenticated-orcid": false,
"family": "Hjärtström",
"given": "Malin",
"sequence": "first"
},
{
"ORCID": "https://orcid.org/0000-0003-1334-7583",
"affiliation": [],
"authenticated-orcid": false,
"family": "Didriksson",
"given": "Ingrid",
"sequence": "additional"
},
{
"ORCID": "https://orcid.org/0000-0001-8754-899X",
"affiliation": [],
"authenticated-orcid": false,
"family": "Spångfors",
"given": "Martin",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Friberg",
"given": "Hans",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Jakobsson",
"given": "Andreas",
"sequence": "additional"
},
{
"ORCID": "https://orcid.org/0000-0002-0155-4828",
"affiliation": [],
"authenticated-orcid": false,
"family": "Frigyesi",
"given": "Attila",
"sequence": "additional"
}
],
"container-title": [],
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2025,
10,
29
]
],
"date-time": "2025-10-29T01:05:10Z",
"timestamp": 1761699910000
},
"deposited": {
"date-parts": [
[
2025,
10,
29
]
],
"date-time": "2025-10-29T01:05:11Z",
"timestamp": 1761699911000
},
"group-title": "Intensive Care and Critical Care Medicine",
"indexed": {
"date-parts": [
[
2025,
10,
29
]
],
"date-time": "2025-10-29T08:11:49Z",
"timestamp": 1761725509161,
"version": "build-2065373602"
},
"institution": [
{
"name": "medRxiv"
}
],
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2025,
10,
28
]
]
},
"license": [
{
"URL": "http://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2025,
10,
28
]
],
"date-time": "2025-10-28T00:00:00Z",
"timestamp": 1761609600000
}
}
],
"link": [
{
"URL": "https://syndication.highwire.org/content/doi/10.1101/2025.10.27.25338863",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "246",
"original-title": [],
"posted": {
"date-parts": [
[
2025,
10,
28
]
]
},
"prefix": "10.1101",
"published": {
"date-parts": [
[
2025,
10,
28
]
]
},
"publisher": "Cold Spring Harbor Laboratory",
"reference-count": 0,
"references-count": 0,
"relation": {},
"resource": {
"primary": {
"URL": "http://medrxiv.org/lookup/doi/10.1101/2025.10.27.25338863"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"subtype": "preprint",
"title": "Polypharmacy and Proton Pump Inhibitor Use Independently Predict One-Year Mortality in Critical COVID-19: An Explainable AI–Based Survival Analysis",
"type": "posted-content"
}