Trump’s 63 Million Doses of Hydroxychloroquine Could Have Been Great for America
et al., Brownstone Journal, Sep 2024
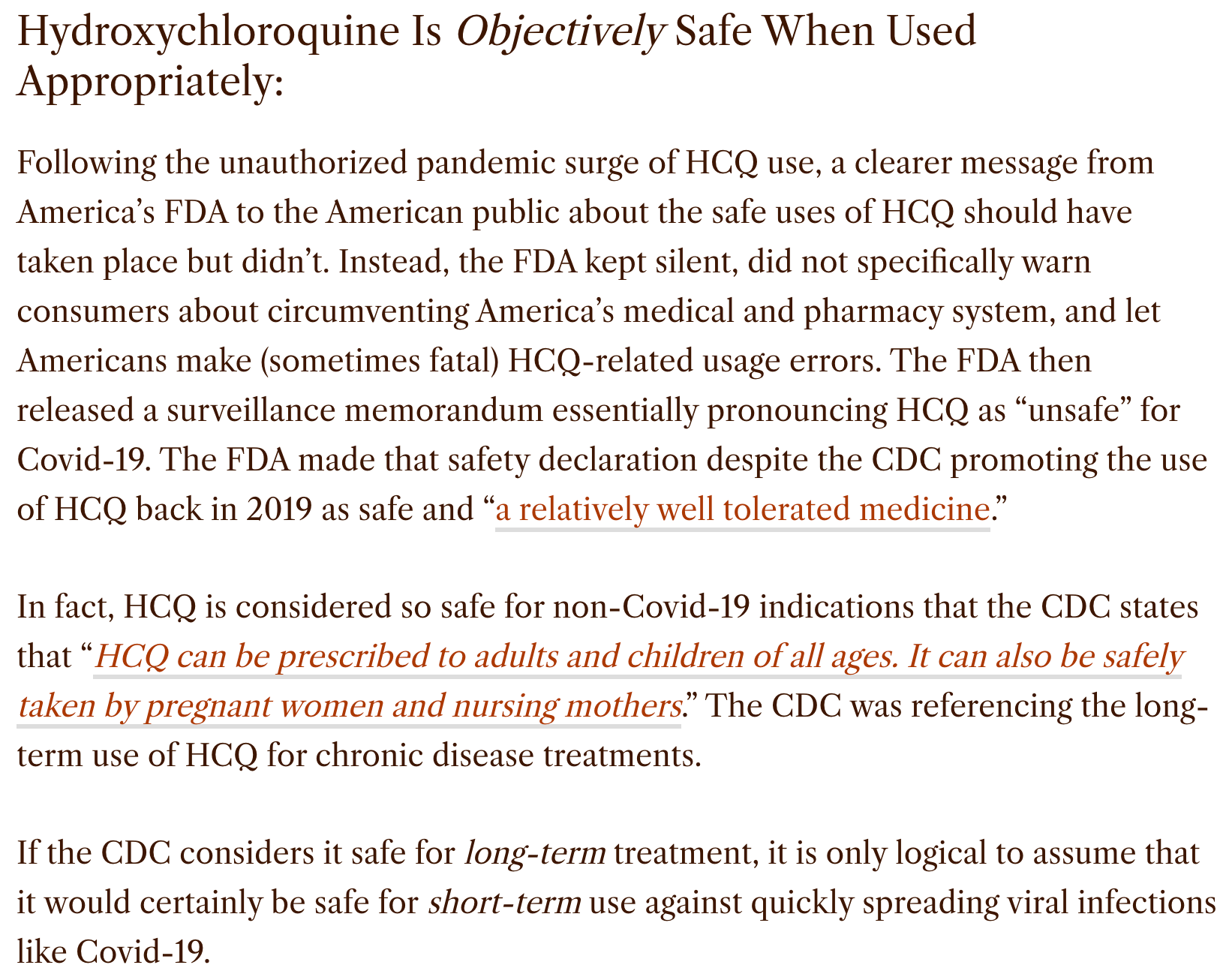
HCQ for COVID-19
1st treatment shown to reduce risk in
March 2020, now with p < 0.00000000001 from 424 studies, used in 59 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Review of the safety and efficacy of HCQ for the treatment and prevention of COVID-19, with a focus on the political and media landscape surrounding its use. Author reports that the FDA's decision to revoke HCQ's emergency use authorization was based on flawed data and methodology, with the inclusion of overdose cases and inappropriate dosing, and that the FDA further actively discouraged use and portrayed HCQ as unsafe, in contradiction to pre-COVID-19 guidelines and safety data. The author also discusses the biased and inaccurate portrayal of HCQ's safety and efficacy by the media and medical experts, often driven by political opposition. Meta analysis of over 400 studies demonstrates HCQ's effectiveness in early treatment and prophylaxis. Author highlights the significant financial implications of prioritizing expensive, novel treatments over repurposed drugs like HCQ, and concludes that the suppression of HCQ represents a major scandal in American medicine and calls for a full investigation into the matter.
1.
Mothae et al., SARS-CoV-2 host-pathogen interactome: insights into more players during pathogenesis, Virology, doi:10.1016/j.virol.2025.110607.
2.
Monsalve et al., NETosis: A key player in autoimmunity, COVID-19, and long COVID, Journal of Translational Autoimmunity, doi:10.1016/j.jtauto.2025.100280.
3.
Xie et al., The role of reactive oxygen species in severe acute respiratory syndrome coronavirus 2 (SARS-COV-2) infection-induced cell death, Cellular & Molecular Biology Letters, doi:10.1186/s11658-024-00659-6.
4.
Gkioulekas et al., Use of hydroxychloroquine in multidrug protocols for SARS-CoV-2, Tasman Medical Journal, 6:4, tasmanmedicaljournal.com/2024/10/use-of-hydroxychloroquine-in-multidrug-protocols-for-sars-cov-2a/.
5.
Gortler et al., Those Published “17,000 Hydroxychloroquine Deaths” Never Happened, Brownstone Journal, brownstone.org/articles/those-published-17000-hydroxychloroquine-deaths-never-happened/.
6.
Boretti et al., Correct Use of HCQ Did Not Cause Extra Fatalities in COVID-19 Infection, Coronaviruses, doi:10.2174/0126667975327612240902104505.
7.
Gortler (B) et al., Trump’s 63 Million Doses of Hydroxychloroquine Could Have Been Great for America, Brownstone Journal, brownstone.org/articles/trumps-63-million-doses-of-hydroxychloroquine-could-have-been-great-for-america/.
8.
Enyeji et al., Effective Treatment of COVID-19 Infection with Repurposed Drugs: Case Reports, Viral Immunology, doi:10.1089/vim.2024.0034.
9.
Asaba et al., Interplay of TLR4 and SARS-CoV-2: Unveiling the Complex Mechanisms of Inflammation and Severity in COVID-19 Infections, Journal of Inflammation Research, doi:10.2147/jir.s474707.
10.
Scheim et al., Back to the Basics of SARS-CoV-2 Biochemistry: Microvascular Occlusive Glycan Bindings Govern Its Morbidities and Inform Therapeutic Responses, Viruses, doi:10.3390/v16040647.
11.
Ali et al., SARS-CoV-2 Syncytium under the Radar: Molecular Insights of the Spike-Induced Syncytia and Potential Strategies to Limit SARS-CoV-2 Replication, Journal of Clinical Medicine, doi:10.3390/jcm12186079.
12.
Brouqui et al., There is no such thing as a Ministry of Truth and why it is important to challenge conventional “wisdom” - A personal view, New Microbes and New Infections, doi:10.1016/j.nmni.2023.101155.
13.
Loo et al., Recent Advances in Inhaled Nanoformulations of Vaccines and Therapeutics Targeting Respiratory Viral Infections, Pharmaceutical Research, doi:10.1007/s11095-023-03520-1.
14.
Boretti (B), A., Pharmacotherapy for Covid-19 infection in the countries of the Cooperation Council for the Arab States, Journal of Taibah University Medical Sciences, doi:10.1016/j.jtumed.2021.08.005.
15.
Vigbedor et al., Review of four major biomolecular target sites for COVID-19 and possible inhibitors as treatment interventions, Journal of Applied Pharmaceutical Science, doi:10.7324/JAPS.2021.110825.
16.
Kaur et al., Folic acid as placebo in controlled clinical trials of hydroxychloroquine prophylaxis in COVID-19: Is it scientifically justifiable?, Medical Hypotheses, doi:10.1016/j.mehy.2021.110539.
17.
Raoult, D., Rational for meta-analysis and randomized treatment: the COVID-19 example, Clinical Microbiology and Infection, doi:10.1016/j.cmi.2020.10.012.
18.
Matada et al., A comprehensive review on the biological interest of quinoline and its derivatives, Bioorganic & Medicinal Chemistry, doi:10.1016/j.bmc.2020.115973.
19.
IHU, Natural history and therapeutic options for COVID-19, Expert Review of Clinical Immunology, www.mediterranee-infection.com/wp-content/uploads/2020/09/ERM-2020-0073.R1_Proof_hi.pdf.
20.
Hecel et al., Zinc(II)—The Overlooked Éminence Grise of Chloroquine’s Fight against COVID-19?, Pharmaceuticals, 13:9, 228, doi:10.3390/ph13090228.
21.
Li et al., Is hydroxychloroquine beneficial for COVID-19 patients?, Cell Death & Disease volume 11, doi:10.1038/s41419-020-2721-8.
22.
Goldstein, L., Hydroxychloroquine-based COVID-19 Treatment, A Systematic Review of Clinical Evidence and Expert Opinion from Physicians’ Surveys, Preprint, July 7, 2020, wattsupwiththat.com/2020/07/07/hydroxychloroquine-based-covid-19-treatment-a-systematic-review-of-clinical-evidence-and-expert-opinion-from-physicians-surveys/.
23.
Roussel et al., Influence of conflicts of interest on public positions in the COVID-19 era, the case of Gilead Sciences, New Microbes and New Infections, Volume 38
, doi:10.1016/j.nmni.2020.100710.
24.
Mo et al., Chloroquine phosphate: therapeutic drug for COVID-19, Journal of Southern Medical University, doi:10.12122/j.issn.1673-4254.2020.04.22.
25.
Gao et al., Update on Use of Chloroquine/Hydroxychloroquine to Treat Coronavirus Disease 2019 (COVID-19), Biosci Trends, May 21, 2020, 14:2, 156-158, doi:10.5582/bst.2020.03072.
26.
Derwand et al., Does zinc supplementation enhance the clinical efficacy of chloroquine/hydroxychloroquine to win today's battle against COVID-19?, Medical Hypotheses, doi:10.1016/j.mehy.2020.109815.
27.
Sahraei et al., Aminoquinolines against coronavirus disease 2019 (COVID-19): chloroquine or hydroxychloroquine, International Journal of Antimicrobial Agents, April 2020, 55:4, doi:10.1016/j.ijantimicag.2020.105945.
28.
Todaro et al., An Effective Treatment for Coronavirus (COVID-19), 3/13, github.com/covidtrial/info/raw/master/An%20Effective%20Treatment%20for%20Coronavirus%20(COVID-19).pdf.
Gortler et al., 9 Sep 2024, preprint, 1 author.
Trump's 63 Million Doses of Hydroxychloroquine Could Have Been Great for America brownstone.org/articles/trumps-63-million-doses-of-hydroxychloroquine-could-have-been-great-for-america/ Early in the pandemic, President Donald Trump and White House senior official Peter Navarro arranged the donation of 63 million doses of hydroxychloroquine (HCQ) to America's strategic drug stockpile to combat Covid-19. The government began securing HCQ in March 2020, after Trump, on the advice of his medical and scientific advisors, lauded HCQ as "very encouraging," "very powerful," and a "game-changer." While HCQ (and its structurally similar analogue chloroquine) was not FDA-indicated for Covid-19, it was well-known to have specific off-label pharmacological functionality for preventing viral particle entry into cells, chemical derivatives of which have been utilized for antiviral use as far back as 1934. Following Trump's proposal, HCQ suddenly came under an unwarranted full-scale attack from federal officials, the press, so-called "fact-checkers," and university professors. Many of the attacks contained outright falsehoods about HCQ's pharmacology and safety or Trump's endeavor to make HCQ available to eligible patients. The FDA initially issued an emergency use authorization (EUA) for HCQ in March 2020, but withdrew authorization on June 15th 2020, stating the drug is "unlikely to be effective in treating COVID-19 for the [EUA] authorized uses." Around the same time, the FDA also wrote a methodologically questionable report criticizing HCQ's safety. The FDA's narrative was based on preliminary and time-compartmentalized findings, and not a reflection of historical safety or based on the appropriate clinical use of HCQ dosing, prescribing, timing, and duration. The FDA then seemed to label its findings as conclusive, figuratively slamming the door shut on the consideration of new findings.
FDA Hydroxychloroquine Safety Assessment Based on: Known Overdoses, and Clinically Unsupervised Uses According to its uncharacteristically brief 15-page safety review memorandum of HCQ published on May 19, 2020, the FDA considered data from the National Poison Data System (NPDS) which means it seems to have included the use of non-pharmaceuticalgrade and/or self-administered HCQ and/or overdose data in its clinical evaluation. Obviously, overdose or any non-medically supervised, self-diagnosis, and/or self-dosing of any prescription drug has a higher potential to result in adverse events, especially because the antiviral dose/duration of HCQ and/or chloroquine were not immediately obvious to the lay public. Of note, "if it bleeds it leads"-type sensationalized news reporting caused anxious and desperate Americans with incomplete or incorrect transmission and mortality information to go so far as to self-administer "fish tank" chloroquine-containing cleaning products of containing other chemicals to..
Simone, P. Chiara, R. Francesca, S. Maria, S. Massimiliano, and S. Stefano, Role of low-molecular weight heparin in hospitalized patients with SARS-CoV-2 pneumonia: a prospective observational study Nov 2020, Open Forum Infectious Diseases, Volume 7, Issue 12 LATE TREATMENT 315 patient HCQ late treatment PSM study: 65% lower mortality (p=0.2). Prospective observational study of 315 hospitalized patients in Italy showing 65% lower mortality with HCQ. The median treatment delay was 6 days for survivors and 6. Retrospective 258 hospitalized patients in Italy showing lower mortality with HCQ treatment, unadjusted relative risk RR 0.455, p<0.001. Data is in the supplementary appendix. https://c19p.org/boari 144. D. Águila-Gordo, J. Martínez-del Río, V. Mazoteras-Muñoz, M. Negreira-Caamaño, P. Nieto-Sandoval Martín de la Sierra, and J. Piqueras-Flores, Mortality and associated prognostic factors in elderly and very elderly hospitalized patients with respiratory disease COVID-19 Nov 2020, Revista Española de Geriatría y Gerontología, Volume 56, Issue 5, Page 259-267 LATE TREATMENT 416 patient HCQ late treatment study: 67% lower mortality (p=0.1). 67% lower mortality with HCQ. Retrospective 416 elderly patients in Spain showing adjusted HCQ mortality hazard ratio HR 0.33, p = 0.1. https://c19p.org/aguilagordo 145. E. Coll, M. Fernández-Ruiz, J. Sánchez-Álvarez, J. Martínez-Fernández, M. Crespo, J. Gayoso, T. Bada-Bosch, F. Oppenheimer, F. Moreso, M. López-Oliva, E. Melilli, M...
References
Alqassieh, Bsisu, Al-Sabbagh, El-Hammuri, Yousef et al., Clinical characteristics and predictors of the duration of hospital stay in COVID-19 patients in Jordan Dec 2020, F1000Research
Babalola, Ndanusa, Ajayi, Ogedengbe, Thairu et al., A Randomized Controlled Trial of Ivermectin Monotherapy Versus Hydroxychloroquine, Ivermectin, and Azithromycin Combination Therapy in Covid-19 Patients in Nigeria Sep 2021
Babayigit, Kokturk, Kul, Cetinkaya, Nayci et al., The association of antiviral drugs with COVID-19 morbidity: The retrospective analysis of a nationwide COVID-19 cohort Aug 2022, doi:10.3389/fmed.2022.894126/full
Barratt-Due, Olsen, Nezvalova-Henriksen, Kåsine, Lund-Johansen et al., Evaluation of the Effects of Remdesivir and Hydroxychloroquine on Viral Clearance in COVID-19 Jul 2021, doi:10.7326/M21-0653
Beaumont, Vignes, Sterpu, Bussone, Kansau et al., Early versus late acute kidney injury among patients with COVID-19-a multicenter study from Wuhan, China Dec 2020, Nephrology Dialysis Transplantation
Bhattacharya, Chowdhury, Mukherjee, Kulshrestha, Ghosh et al., Pre exposure Hydroxychloroquine use is associated with reduced COVID19 risk in healthcare workers Jun 2020, medRxix 106 patient HCQ prophylaxis study: 81% fewer cases (p=0.001), HCQ reduced cases from, doi:10.1101/2020.06.09.20116806v1
Bielza, Sanz, Zambrana, Arias, Malmierca et al., Clinical characteristics, frailty and mortality of residents with COVID-19 in nursing homes of a region of Madrid Dec 2020, J. the American Medical Directors Association
Bozdağ, Seval, Hindilerden, Hindilerden, Andıç et al., Clinical Characteristics and Outcome of COVID-19 in Turkish 388
Burdick, Lam, Mataraso, Siefkas, Braden et al., Is Machine Learning a Better Way to IdentifyCOVID-19 Patients Who Might Benefit fromHydroxychloroquineTreatment?-The IDENTIFY Trial Nov 2020, J. Clinical Medicine
Calderón, Padmanabhan, Salazar, Hernández, Martínez et al., Treatment with hydroxychloroquine vs nitazoxanide in patients with COVID-19: brief report Nov 2021, PAMJ -Clinical Medicine LATE TREATMENT 44 patient HCQ late
Chari, Samur, Martinez-Lopez, Cook, Biran et al., Clinical features associated with COVID-19 outcome in multiple myeloma: first results from the International Myeloma Society data set Dec 2020, Blood
Chen, Liu, Liu, Liu, Xu et al., A pilot study of hydroxychloroquine in treatment of patients with common coronavirus disease-19 (COVID-19) Mar 2020
Cárdenas-Jaén, Sánchez-Luna, Vaillo-Rocamora, Castro-Zocchi, Guberna-Blanco et al., Gastrointestinal symptoms and complications in patients hospitalized due to COVID-19, an international multicentre prospective cohort study (TIVURON project) Jun 2023
De Gonzalo-Calvo, Molinero, Benítez, Perez-Pons, García-Mateo et al., A blood microRNA classifier for the prediction of ICU mortality in COVID-19 patients: a multicenter validation study Jun 2023, Respiratory Research, doi:10.1186/s12931-023-02462-x
De La Iglesia, Fernández, Flores, Gómez, González De Haro et al., Analysis of autoimmune disease patients on HCQ, compared to a control group from the general population (matched on age and sex, but not adjusted for autoimmune disease), showing non-significant differences between groups. Other research shows that the risk of COVID-19 for systemic autoimmune disease patients is much higher overall, doi:10.1101/2020.08.31.20185314v1
Desbois, Marques, Lefèvre, Barmo, Lorenzo et al., Prevalence and clinical features of COVID-19 in a large cohort of 199 patients with sarcoidosis Jul 2020, Research Square 199 patient HCQ prophylaxis study: 17% fewer cases (p=1). Retrospective 199 sarcoidosis patients showing non-statistically significant HCQ RR 0
Ebongue, Lemogoum, Endale-Mangamba, Barche, Eyoum et al., Factors predicting in-hospital all-cause mortality in COVID 19 patients at the Laquintinie Hospital Douala, Cameroon Mar 2022
Euras, Late, TREATMENT 147 patient HCQ ICU study: 3% lower mortality (p=0.85). Retrospective 147 ICU patients in Turkey, showing
Fernández-Cruz, Puyuelo, Núñez Martín-Buitrago, Sánchez-Chica, Díaz-Pedroche et al., Higher mortality of hospitalized haematologic patients with COVID-19 compared to non-haematologic is driven by thrombotic complications and development of ARDS: An age-matched cohorts study Jan 2022
Ferreira, Beranger, Sampaio, Filho, Lima, Outcomes associated with Hydroxychloroquine and Ivermectin in hospitalized patients with COVID-19: a single-center experience Nov 2021
Florescu, Stanciu, Zaharia, Kosa, Codreanu et al., Longterm (180-Day) Outcomes in Critically Ill Patients With COVID-19 in the REMAP-CAP Randomized Clinical Trial Dec 2022
Geleris, Sun, Platt, Zucker, Baldwin et al., Observational Study of Hydroxychloroquine in Hospitalized Patients with Covid-19 May 2020, doi:10.1056/NEJMoa2012410
Gendebien, Von Frenckell, Ribbens, André, Thys et al., patient HCQ prophylaxis study: 4% fewer cases (p=0.93). Small study of SLE patients taking HCQ with a phone survey for COVID-19 suggestive symptoms. There was 2 hospitalizations (group not identified) and no ICU or death cases. A similar percentage of suspected infections were reported for HCQ users and non-HCQ users, Annals of the Rheumatic Diseases
Gianfrancesco, Hyrich, Al-Adely, Carmona, Danila et al., patient HCQ prophylaxis study: 3% lower hospitalization (p=0.82). Analysis of rheumatic disease patients showing no significant association between antimalarial therapy and hospitalization, Annals of the Rheumatic Diseases
Goenka, Afzalpurkar, Goenka, Das, Mukherjee et al., Seroprevalence of COVID-19 Amongst Health Care Workers in a Tertiary Care Hospital of a Metropolitan City from India Oct 2020, SSRN 962 patient HCQ prophylaxis study: 87% lower IgG positivity (p=0.03). Study of SARS-CoV-2-IgG antibodies in 1122 health care workers in India finding 87% lower positives for adequate HCQ prophylaxis, 1.3% HCQ versus 12.3% for no HCQ prophylaxis. Adequate prophylaxis is defined as 400mg 1/wk for >6 weeks
Goldman, Lye, Hui, Marks, Bruno et al., TREATMENT 397 patient HCQ late treatment study: 22% lower mortality (p=0.46). Study focused on remdesivir but with results for HCQ in the supplementary appendix, showing 9% death with HCQ versus, NEJM, doi:10.1056/NEJMoa2015301
González, Gonzalo, Lopez, Fernández, Pérez et al., The Prognostic Value of Eosinophil Recovery in COVID-19: A Multicentre, Retrospective Cohort Study on Patients Hospitalised in Spanish Hospitals Aug 2020, medRxiv LATE TREATMENT 9,644 patient HCQ late treatment study: 27% lower mortality (p=0.06). Retrospective study focused on eosinophil recovery with 9,644 hospitalized patients in Spain, showing lower mortality for HCQ, AZ, doi:10.1101/2020.08.18.20172874v1
Gupta, Hayek, Wang, Chan, Mathews et al., Factors Associated With Death in Critically Ill Patients With Coronavirus Disease 2019 in the US Jul 2020, JAMA Intern. Med
Hafez, Saleh, Al Baha, Tariq, Hamdan et al., Antiviral Used among Non-Severe COVID-19 Cases in Relation to Time till Viral Clearance: A Retrospective Cohort Study Apr 2022
Hcq Vs ; Sapan, Desai, set of HCQ vs. nitazoxanide patients (which were protocol deviations in the planned RCT), showing reduced hospitalization time and ICU admission with nitazoxanide
Ho, Wei, Tan, Woh, Gill et al., Retrospective 325 hospitalized COVID-19 patients in Malaysia, showing higher progression with HCQ, however the groups are not comparable. 17 HCQ
Ip, Berry, Hansen, Goy, Pecora et al., Retrospective study of late stage use on 2,512 hospitalized patients showing no significant differences in associated mortality for patients receiving, HCQ alone (HR, doi:https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0237693
Isnardi, Roberts, Saurit, Petkovic, Báez et al., Sociodemographic and clinical factors associated with poor COVID-19 outcomes in patients with rheumatic diseases: data from the SAR-COVID Registry Oct 2022, doi:10.1007/s10067-022-06393-8
Jacobs, Stammers, St, Louis, Hayanga et al., The Effect of Pre-admission Hydroxychloroquine Treatment on COVID-19-Related Intensive Care Follow-up in Geriatric Patients Apr 2021
Kalligeros, Shehadeh, Atalla, Mylona, Aung et al., Hydroxychloroquine use in hospitalised patients with COVID-19: An observational matched cohort study Aug 2020
Karruli, Boccia, Gagliardi, Patauner, Ursi et al., Multidrug-Resistant Infections and Outcome of Critically Ill Patients with Coronavirus Disease 2019: A Single Center Experience Aug 2021, doi:10.1089/mdr.2020.0489
Klebanov, Pahalyants, Said, Murphy, Theodosakis et al., antimalarial prophylaxis for PCR+ cases (99% HCQ). Authors provide only PCR+ and mortality outcomes, and do not provide intermediate clinical outcomes that may show a statistically significant benefit. Authors do not adjust for the very different baseline risk for systemic autoimmune disease patients. Other research shows that the risk of COVID-19 for systemic autoimmune disease patients is, J. Drugs in Dermatology
Konig, Kim, Scheetz, Graef, Liew et al., Baseline use of hydroxychloroquine in systemic lupus erythematosus does not preclude SARS-CoV-2 336
Krishnan, Patel, Desai, Sule, Paik et al., Retrospective 152 mechanically ventilated patients in the USA showing unadjusted lower mortality with vitamin C, vitamin D, HCQ, and zinc treatment, statistically significant only for vitamin C, Blood Cancer J
Lavilla Olleros, García, Bendala, Estrada, Muñoz et al., Use of glucocorticoids megadoses in SARS-CoV-2 infection in a spanish registry: SEMI-COVID-19 Jan 2022, PLOS ONE, doi:https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0261711
Llanos-Cuentas, Schwalb, Quintana, Delfin, Alvarez et al., Hydroxychloroquine to prevent SARS-CoV-2 infection among healthcare workers: early termination of a phase 3, randomised, open-label, controlled clinical trial Feb 2023, BMC Research Notes, doi:10.1186/s13104-023-06281-7
Luo, Rizvi, Preeshagul, Egger, Hoyos et al., COVID-19 infection in a northern-Italian cohort of systemic lupus erythematosus assessed by telemedicine May 2020
Lyngbakken, Berdal, Eskesen, Kvale, Olsen et al., HCQ late treatment RCT: 4% lower mortality (p=1) and 71% improved viral reduction rate (p=0.51). Small RCT of nasopharyngeal viral load not showing significant differences. The rate of reduction for HCQ, Nature Communications
Mahto, Banerjee, Biswas, Kumar, Agarwal et al., Seroprevalence of IgG against SARS-CoV-2 and its determinants among healthcare workers of a COVID-19 dedicated hospital of India Feb 2021
Mallat, Hamed, Balkis, Mohamed, Mooty et al., ). Very small retrospective analysis of 34 patients finding slower binary PCR viral clearance with HCQ. No information on severity for treatment versus control is provided. No deaths, ICU admission, or mechanical ventilation. Binary PCR does not distinguish replication-competence. HCQ treatment started very late for many patients with >= 9 days for 25%, Medicine
Martin-Vicente, Almansa, Martínez, Tedim, Bustamante et al., Absent or insufficient anti-SARS-CoV-2 S antibodies at ICU admission are associated to higher viral loads in plasma, antigenemia and mortality in COVID-19 patients Mar, doi:10.1101/2021.03.08.21253121v1
Mckinnon, Wang, Zervos, Saval, Marshall-Nightengale et al., prophylaxis RCT: 2% fewer symptomatic cases (p=1) and 51% fewer cases (p=0.6). HCQ prophylaxis RCT with 201 weekly HCQ patients, 197 daily HCQ patients, and 200 control patients, concluding the prophylaxis is safe. There were no grade 3 or 4 AEs, SAEs, ER visits, or hospitalizations. There were only 4 confirmed cases, 2 in the placebo arm and one in each HCQ arm. 60% of patients had exposure at baseline. HCQ 400mg weekly or HCQ 200mg daily after, Int. J. Infectious Diseases
Menardi, Infante, Del, Bono, Fenoglio et al., A retrospective analysis on pharmacological approaches to COVID-19 patients in an Italian hub hospital during the early phase of the pandemic Sep 2021, PharmAdvances
Pablos, Galindo, Carmona, Lledó, Retuerto et al., Retrospective 228 rheumatic disease and 228 non-rheumatic disease hospitalized COVID-19 patients in Spain, showing higher risk of severe COVID-19 with HCQ treatment, doi:10.1136/annrheumdis-2020-218296
Paccoud, Tubach, Baptiste, Bleibtreu, Hajage et al., Compassionate use of hydroxychloroquine in clinical practice for patients with mild to severe Covid-19 in a French university hospital Jun 2020, doi:10.1093/cid/ciaa791/5859555
Panda, Singh, Moirangthem, Bahurupi, Saha et al., Antiviral Combination Clinically Better Than Standard Therapy in Severe but Not in Non-Severe COVID-19 Sep 2021, Clinical Pharmacology: Advances and Applications
Pasquini, Montalti, Temperoni, Canovari, Mancini et al., Effectiveness of remdesivir in patients with COVID-19 under mechanical ventilation in an Italian ICU Aug 2020
Purandare, Rajhans, Jog, Dalvi, Prayag et al., A Retrospective Observational Study of Hypoxic COVID-19 Patients Treated with Immunomodulatory Drugs in a Tertiary Care Hospital Dec 2020, Indian J. Critical Care Medicine, doi:10.5005/jp-journals-10071-23599
Qin, Dong, Zhang, Hu, Chen et al., LATE TREATMENT 749 patient HCQ late treatment study: 34% lower mortality (p=0.61). Low molecular weight heparin study also showing results for HCQ treatment, unadjusted HCQ mortality relative risk RR 0, Thrombosis Research
Rivera-Izquierdo, Valero-Ubierna, R-Delamo, Fernández-García, Martínez-Diz et al., LATE TREATMENT 238 patient HCQ late treatment study: 19% lower mortality (p=0.75). Retrospective 238 hospitalized patients in Spain showing lower mortality with HCQ, adjusted, Medicina Clínica
Rodrigues, Freitas-Santos, Levi, Senerchia, Lopes et al., Hydroxychloroquine plus azithromycin early treatment of mild COVID-19 in outpatient setting: a randomized, double-blinded, placebo-controlled clinical trial evaluating viral clearance Aug 2021, Int. J. Antimicrobial Agents
Rodríguez, Moreno, Gómez, Carbonell, Picó-Plana et al., Severe infection due to the SARS-CoV-2 coronavirus: Experience of a tertiary hospital with COVID-19 patients during the 2020 pandemic Nov 2020, Medicina Intensiva
Roger, Collange, Mezzarobba, Abou-Arab, Teule et al., French Multicentre Observational Study on SARS-CoV-2 infections Intensive care initial management: the FRENCH CORONA Study Jul 2021, Anaesthesia Critical Care & Pain Medicine
Roomi, Ullah, Ahmed, Farooq, Sadiq et al., Efficacy of hydroxychloroquine and tocilizumab in patients with COVID-19: A single-center retrospective chart review Aug 2020, J. Medical Internet Research
Réa-Neto, Bernardelli, Câmara, Reese, Queiroga et al., An open-label randomized controlled trial evaluating the efficacy of chloroquine/hydroxychloroquine in severe COVID-19 patients Apr 2021, Scientific Reports
Salvador, Oliveira, Costa, Fidalgo, Neto et al., Prevalence of COVID-19 in patients with rheumatoid arthritis (RA) already treated with hydroxychloroquine (HCQ) compared with HCQ-naive patients with RA: a multicentre cross-sectional study Jan 2021, Postgraduate Medical J
Salvarani, Mancuso, Gradellini, Viani, Pandolfi et al., Comparison of CQ/HCQ users with the general population in a region of Italy, showing no significant difference in the probability of COVID-19. CQ/HCQ users were mostly systemic autoimmune disease patients and authors do not adjust for the very different baseline risk for these patients. Other research shows that the risk of COVID-19 for systemic autoimmune disease patients is much higher overall, Arthritis & Rheumatology, doi:10.1002/art.41475
Santos, Morales, Álvarez, Castro, Robles et al., Determinants of COVID-19 disease severity in patients with underlying rheumatic disease Jul 2020, Clinical Rheumatology, doi:10.1007/s10067-020-05301-2
Sarhan, Harb, Abou Warda, Salem-Bekhit, Shakeel et al., Efficacy of the early treatment with tocilizumabhydroxychloroquine and tocilizumab-remdesivir in severe COVID-19 Patients Nov 2021, J. Infection and Public Health
Schmidt, Tucker, Bakouny, Labaki, Hsu et al., Association Between Androgen Deprivation Therapy and Mortality Among Patients With Prostate Cancer and COVID-19 Nov 2021, JAMA Network Open
Self, Semler, Leither, Casey, Angus et al., ). Early terminated very late stage (65% on supplemental oxygen) RCT with 242 HCQ and 237 control patients showing no significant difference in outcomes, JAMA
Shabani, Totonchi, Rezaeimirghaed, Gachkar, Hajiesmaeili et al., HCQ prophylaxis study: 19% fewer symptomatic cases (p=1) and 6% more cases (p=1). Small PEP trial with 51 HCQ patients, not showing a significant difference in cases, Pulmonary Pharmacology & Therapeutics
Shabrawishi, Naser, Alwafi, Aldobyany, Touman, Negative nasopharyngeal SARS-CoV-2 PCR conversion in response to different therapeutic interventions May 2020, doi:10.1101/2020.05.08.20095679v1
Shahrin, Mahfuz, Rahman, Hossain, Khandaker et al., Hospital-Based Quasi-Experimental Study on Hydroxychloroquine Pre-Exposure Prophylaxis for COVID-19 in Healthcare Providers with Its Potential Side-Effects Dec 2022, Life
Singer, Kaelber, Antonelli, Hydroxychloroquine ineffective for COVID-19 prophylaxis in lupus and rheumatoid arthritis Aug 2020
Sivapalan, Ulrik, Lapperre, Bojesen, Eklöf et al., double-blinded placebo-controlled trial Jun
Sobngwi, Zemsi, Guewo, Katte, Kouanfack et al., Doxycycline vs Hydroxychloroquine + Azithromycin in the Management of COVID-19 Patients: An Open-Label Randomized Clinical Trial in Sub-Saharan Africa (DOXYCOV) Jul 2021
Sosa-García, Gutiérrez-Villaseñor, García-Briones, Romero-González, Juárez-Hernández et al., Experience in the management of severe COVID-19 patients in an intensive care unit Jun 2020, Cir Cir
Spila Alegiani, Crisafulli, Rossi, Mancuso, Salvarani et al., HCQ prophylaxis study: 8% higher mortality (p=0.64) and 18% lower hospitalization (p=0.03). Retrospective database analysis case control study of rheumatic patients. When compared with other cDMARDs, HCQ users had significantly lower hospitalization, however there was no significant difference in mortality. Results differ significantly from previous studies, Rheumatology, doi:10.1093/rheumatology/keab348/6226505?searchresult=1
Syed, Hassan, Arif, Batool, Niazi et al., Pre-exposure Prophylaxis With Various Doses of Hydroxychloroquine Among Healthcare Personnel With High-Risk Exposure to COVID-19: A Randomized Controlled Trial May
Tehrani, Killander, Åstrand, Jakobsson, Gille-Johnson, LATE TREATMENT 255 patient HCQ late treatment study: 13% lower mortality (p=0.63). Retrospective 255 hospitalized patients, 65 treated with HCQ, Int. J. Infectious Diseases
Tirupakuzhi Vijayaraghavan, Jha, Rajbhandari, Myatra, Ghosh et al., Hydroxychloroquine plus personal protective equipment versus personal protective equipment alone for the prevention of laboratory-confirmed COVID-19 infections among healthcare workers: a multicentre, parallel-group randomised controlled trial from India May 2022, BMJ Open, doi:10.1136/bmjopen-2021-059540
Trullàs, Ruiz, Weisweiler, Badosa, Serra et al., High in-hospital mortality due to COVID-19 in a community hospital in Spain: a prospective observational study Jul 2020, Research Square LATE TREATMENT 100 patient HCQ late treatment study: 36% lower mortality (p=0.12). Retrospective 100 hospitalized patients in Spain showing lower mortality with HCQ+AZ
Ulrich, Troxel, Carmody, Eapen, Bäcker et al., Treating Covid-19 With Hydroxychloroquine (TEACH): A Multicenter, Double-Blind, Randomized Controlled Trial in Hospitalized Patients Sep 2020, doi:10.1093/ofid/ofaa446/5910201
Uyaroğlu, Sönmezer, Telli Dizman, Çalık Başaran, Karahan et al., Comparison of Favipiravir to Hydroxychloroquine Plus Azithromycin in the Treatment of Patients with Non-critical COVID-19: A Single-center, Retrospective, Propensity Score-matched Study Mar 2022, Acta Medica
Zhong Nanshan, 钟南⼭), Efficacy and safety of chloroquine for treatment of COVID-19. An open-label, multi-center, non-randomized trial Mar 2020, Zhong Nanshan LATE TREATMENT 197 patient HCQ late treatment study: 80% improved viral clearance (p=0.0001). 197 patients. CQ effective
