Safety of High-Dose Vitamin C in Non-Intensive Care Hospitalized Patients with COVID-19: An Open-Label Clinical Study
et al., Journal of Clinical Medicine, doi:10.3390/jcm13133987, NCT04323514, Jul 2024
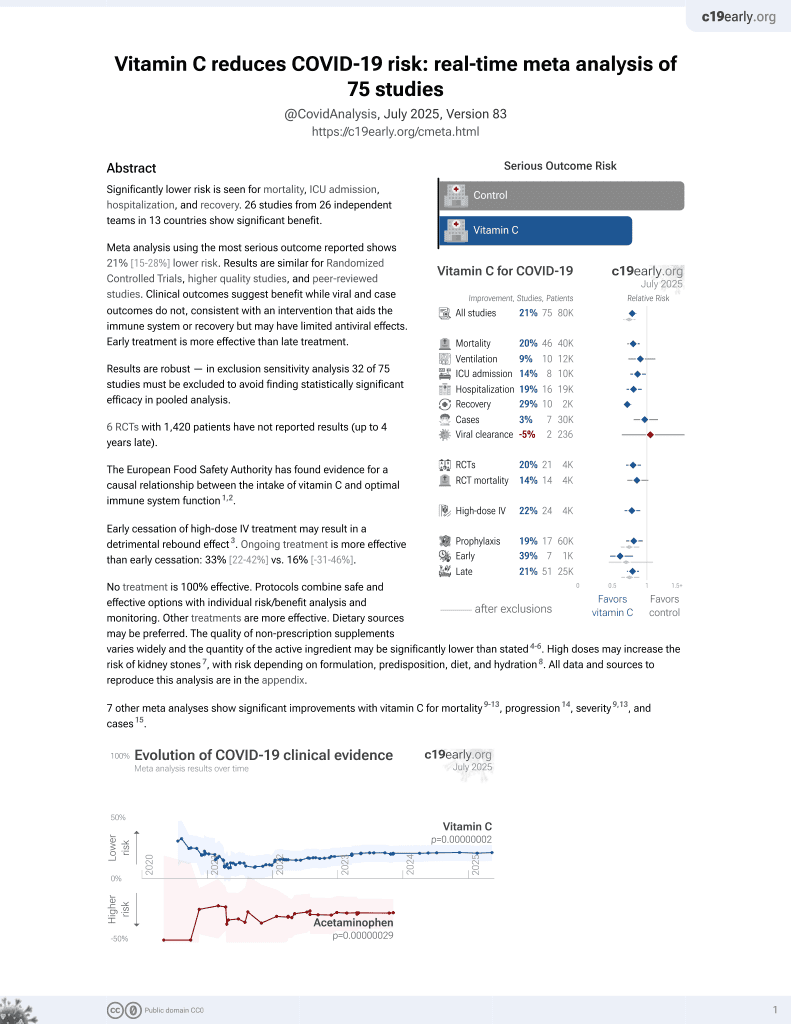
Vitamin C for COVID-19
6th treatment shown to reduce risk in
September 2020, now with p = 0.000000068 from 74 studies, recognized in 22 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
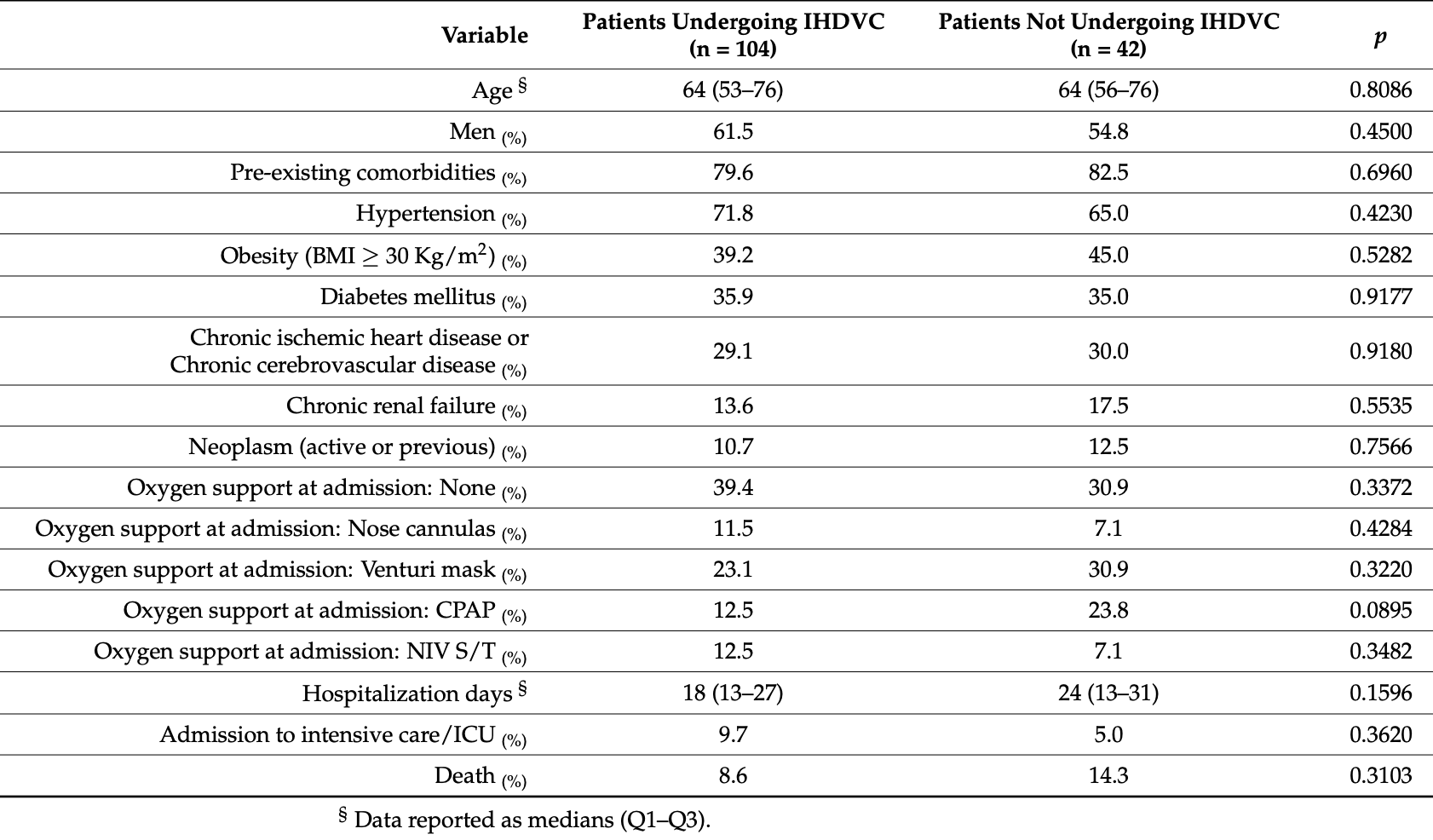
Prospective study of 146 hospitalized COVID-19 patients showing shorter hospitalization with high-dose intravenous vitamin C. 104 patients received 10g of vitamin C intravenously daily for 3 days and 42 patients received only standard care. Mortality was lower with treatment (8.7% vs 14.3%) without statistical significance. Treatment was associated with significantly shorter hospitalization in multivariable analysis (-4.95, p=0.041). No adverse events were reported in the vitamin C group.
This is the 71st of 74 COVID-19 controlled studies for vitamin C, which collectively show efficacy with p=0.000000068.
21 studies are RCTs, which show efficacy with p=0.0012.
|
risk of death, 39.4% lower, RR 0.61, p = 0.37, treatment 9 of 104 (8.7%), control 6 of 42 (14.3%), NNT 18.
|
|
risk of death/ICU, 19.0% lower, OR 0.81, p = 0.24, treatment 104, control 42, adjusted per study, multivariable, RR approximated with OR.
|
|
risk of ICU admission, 101.9% higher, RR 2.02, p = 0.51, treatment 10 of 104 (9.6%), control 2 of 42 (4.8%).
|
|
hospitalization time, 25.0% lower, relative time 0.75, p = 0.16, treatment 104, control 42.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Corrao et al., 8 Jul 2024, prospective, Italy, peer-reviewed, 7 authors, trial NCT04323514 (history).
Safety of High-Dose Vitamin C in Non-Intensive Care Hospitalized Patients with COVID-19: An Open-Label Clinical Study
doi:10.3390/jcm13133987
Background: Vitamin C has been used as an antioxidant and has been proven effective in boosting immunity in different diseases, including coronavirus disease ). An increasing awareness was directed to the role of intravenous vitamin C in COVID-19. Methods: In this study, we aimed to assess the safety of high-dose intravenous vitamin C added to the conventional regimens for patients with different stages of COVID-19. An open-label clinical trial was conducted on patients with COVID-19. One hundred four patients underwent high-dose intravenous administration of vitamin C (in addition to conventional therapy), precisely 10 g in 250 cc of saline solution in slow infusion (60 drops/min) for three consecutive days. At the same time, 42 patients took the standardof-care therapy. Results: This study showed the safety of high-dose intravenous administration of vitamin C. No adverse reactions were found. When we evaluated the renal function indices and estimated the glomerular filtration rate (eGRF, calculated with the CKD-EPI Creatinine Equation) as the main side effect and contraindication related to chronic renal failure, no statistically significant differences between the two groups were found. High-dose vitamin C treatment was not associated with a statistically significant reduction in mortality and admission to the intensive care unit, even if the result was bound to the statistical significance. On the contrary, age was independently associated with admission to the intensive care unit and in-hospital mortality as well as noninvasive ventilation (N.I.V.) and continuous positive airway pressure (CPAP) (OR 2.17, 95% CI 1. OR 7.50, OR 8.84, respectively). When considering the length of hospital stay, treatment with high-dose vitamin C predicts shorter hospitalization (OR -4.95 CI -0.21--9.69). Conclusions: Our findings showed that an intravenous high dose of vitamin C is configured as a safe and promising therapy for patients with moderate to severe COVID-19.
Institutional Review Board Statement: The Ethics Committee has approved the conduct of the study at our institution. The approval number assigned to this study is 3143-2020. Informed Consent Statement: Informed consent was obtained from all subjects involved in the study.
Conflicts of Interest: The authors declare no conflicts of interest.
References
Argano, Mallaci Bocchio, Lo Monaco, Scibetta, Natoli et al., An Overview of Systematic Reviews of the Role of Vitamin D on Inflammation in Patients with Diabetes and the Potentiality of Its Application on Diabetic Patients with COVID-19, Int. J. Mol. Sci, doi:10.3390/ijms23052873
Argano, Mallaci Bocchio, Natoli, Scibetta, Lo Monaco et al., Protective Effect of Vitamin D Supplementation on COVID-19-Related Intensive Care Hospitalization and Mortality: Definitive Evidence from Meta-Analysis and Trial Sequential Analysis, Pharmaceuticals, doi:10.3390/ph16010130
Argano, Natoli, Mularo, Nobili, Monaco et al., Impact of Diabetes Mellitus and Its Comorbidities on Elderly Patients Hospitalized in Internal Medicine Wards: Data from the RePoSi Registry, Healthcare, doi:10.3390/healthcare10010086
Argano, Scichilone, Natoli, Nobili, Corazza et al., Pattern of Comorbidities and 1-Year Mortality in Elderly Patients with COPD Hospitalized in Internal Medicine Wards: Data from the RePoSI Registry, Intern. Emerg. Med, doi:10.1007/s11739-020-02412-1
Azkur, Akdis, Azkur, Sokolowska, Van De Veen et al., Immune Response to SARS-CoV-2 and Mechanisms of Immunopathological Changes in COVID-19, Allergy, doi:10.1111/all.14364
Bae, Kim, Mini-Review on the Roles of Vitamin C, Vitamin D, and Selenium in the Immune System against COVID-19, Molecules, doi:10.3390/molecules25225346
Barker, Taxman, Ting, Cross-Regulation between the IL-1β/IL-18 Processing Inflammasome and Other Inflammatory Cytokines, Curr. Opin. Immunol, doi:10.1016/j.coi.2011.07.005
Bergsbaken, Fink, Cookson, Pyroptosis: Host Cell Death and Inflammation, Nat. Rev. Microbiol, doi:10.1038/nrmicro2070
Berti, Kale-Pradhan, Giuliano, Aprilliano, Miller et al., Clinical Outcomes of Zinc Supplementation Among COVID-19 Patients, Curr. Drug Saf, doi:10.2174/1574886317666220317115023
Betakova, Kostrabova, Lachova, Turianova, Cytokines Induced During Influenza Virus Infection, Curr. Pharm. Des, doi:10.2174/1381612823666170316123736
Biancatelli, Berrill, Catravas, Marik, Quercetin et al., An Experimental, Synergistic Therapy for the Prevention and Treatment of SARS-CoV-2 Related Disease (COVID-19), Front. Immunol, doi:10.3389/fimmu.2020.01451
Braciale, Sun, Kim, Regulating the Adaptive Immune Response to Respiratory Virus Infection, Nat. Rev. Immunol, doi:10.1038/nri3166
Brant, Angus, Is High-Dose Vitamin C Beneficial for Patients with Sepsis?, JAMA, doi:10.1001/jama.2019.11643
Briguglio, Pregliasco, Lombardi, Perazzo, Banfi, The Malnutritional Status of the Host as a Virulence Factor for New Coronavirus SARS-CoV-2, Front. Med, doi:10.3389/fmed.2020.00146
Carr, Maggini, Vitamin C and Immune Function, Nutrients, doi:10.3390/nu9111211
Cerullo, Negro, Parimbelli, Pecoraro, Perna et al., The Long History of Vitamin C: From Prevention of the Common Cold to Potential Aid in the Treatment of COVID-19, Front. Immunol, doi:10.3389/fimmu.2020.574029
Chaplin, Overview of the Immune Response, J. Allergy Clin. Immunol, doi:10.1016/j.jaci.2009.12.980
Chen, Zhou, Dong, Qu, Gong et al., Epidemiological and Clinical Characteristics of 99 Cases of 2019 Novel Coronavirus Pneumonia in Wuhan, China: A Descriptive Study, Lancet, doi:10.1016/S0140-6736(20)30211-7
Corrao, Gervasi, Di Bernardo, Argano, Immune Response Failure in Paucisymptomatic Long-Standing SARS-CoV-2 Spreaders, Clin. Pract, doi:10.3390/clinpract11010021
Corrao, Gervasi, Di Bernardo, Natoli, Raspanti et al., Immunological Characteristics of Non-Intensive Care Hospitalized COVID-19 Patients: A Preliminary Report, J. Clin. Med, doi:10.3390/jcm10040849
Corrao, Mallaci Bocchio, Lo Monaco, Natoli, Cavezzi et al., Does Evidence Exist to Blunt Inflammatory Response by Nutraceutical Supplementation during COVID-19 Pandemic? An Overview of Systematic Reviews of Vitamin D, Vitamin C, Melatonin, and Zinc, Nutrients, doi:10.3390/nu13041261
Corrao, Natoli, Nobili, Mannucci, Pietrangelo et al., Comorbidity Does Not Mean Clinical Complexity: Evidence from the RePoSI Register, Intern. Emerg. Med, doi:10.1007/s11739-019-02211-3
Corrao, Use of Ascorbic Acid in Patients with COVID 19
D'errico, Zanon, Montanaro, Radaelli, Sessa et al., More than Pneumonia: Distinctive Features of SARS-CoV-2 Infection. From Autopsy Findings to Clinical Implications: A Systematic Review, Microorganisms, doi:10.3390/microorganisms8111642
Engelmann, Massberg, Thrombosis as an Intravascular Effector of Innate Immunity, Nat. Rev. Immunol, doi:10.1038/nri3345
Fajgenbaum, June, Storm, None, N. Engl. J. Med, doi:10.1056/NEJMra2026131
Filip, Gheorghita Puscaselu, Anchidin-Norocel, Dimian, Savage, Global Challenges to Public Health Care Systems during the COVID-19 Pandemic: A Review of Pandemic Measures and Problems, J. Pers. Med, doi:10.3390/jpm12081295
Fowler, Syed, Knowlson, Sculthorpe, Farthing et al., Phase I Safety Trial of Intravenous Ascorbic Acid in Patients with Severe Sepsis, J. Transl. Med, doi:10.1186/1479-5876-12-32
Fowler, Truwit, Hite, Morris, Dewilde et al., Effect of Vitamin C Infusion on Organ Failure and Biomarkers of Inflammation and Vascular Injury in Patients With Sepsis and Severe Acute Respiratory Failure: The CITRIS-ALI Randomized Clinical Trial, JAMA, doi:10.1001/jama.2019.11825
Gao, Xu, Wang, Lv, Ma et al., The Efficiency and Safety of High-Dose Vitamin C in Patients with COVID-19: A Retrospective Cohort Study, Aging, doi:10.18632/aging.202557
Gavriatopoulou, Ntanasis-Stathopoulos, Korompoki, Fotiou, Migkou et al., Emerging Treatment Strategies for COVID-19 Infection, Clin. Exp. Med, doi:10.1007/s10238-020-00671-y
Harker, Lewis, Mack, Zuniga, Late Interleukin-6 Escalates T Follicular Helper Cell Responses and Controls a Chronic Viral Infection, Science, doi:10.1126/science.1208421
Hemilä, Chalker, Vitamin C May Reduce the Duration of Mechanical Ventilation in Critically Ill Patients: A Meta-Regression Analysis, J. Intensive Care, doi:10.1186/s40560-020-0432-y
Hemilä, Louhiala, Vitamin C May Affect Lung Infections, J. R. Soc. Med, doi:10.1177/014107680710001109
Hemilä, Louhiala, Vitamin C for Preventing and Treating Pneumonia, Cochrane Database Syst. Rev, doi:10.1002/14651858.CD005532.pub3
Hewitt, Carter, Vilches-Moraga, Quinn, Braude et al., The Effect of Frailty on Survival in Patients with COVID-19 (COPE): A Multicentre, European, Observational Cohort Study, Lancet Public Health, doi:10.1016/S2468-2667(20)30146-8
Hosmer, Jr, Lemeshow, Applied Logistic Regression
Hu, Huang, Yin, The Cytokine Storm and COVID-19, J. Med. Virol, doi:10.1002/jmv.26232
Iwasaki, Medzhitov, Regulation of Adaptive Immunity by the Innate Immune System, Science, doi:10.1126/science.1183021
Jamalimoghadamsiahkali, Zarezade, Koolaji, Seyedalinaghi, Zendehdel et al., Safety and Effectiveness of High-Dose Vitamin C in Patients with COVID-19: A Randomized Open-Label Clinical Trial, Eur. J. Med. Res, doi:10.1186/s40001-021-00490-1
Karki, Kanneganti, The, Cytokine Storm": Molecular Mechanisms and Therapeutic Prospects, Trends Immunol, doi:10.1016/j.it.2021.06.001
Kawai, Akira, Innate Immune Recognition of Viral Infection, Nat. Immunol, doi:10.1038/ni1303
Kim, Jo, Eom, Mok, Kim et al., Hydrocortisone, and Thiamine Therapy for Patients with Severe Pneumonia Who Were Admitted to the Intensive Care Unit: Propensity Score-Based Analysis of a before-after Cohort Study, J. Crit. Care, doi:10.1016/j.jcrc.2018.07.004
Kim, Kim, Bae, Choi, Lim et al., Vitamin C Is an Essential Factor on the Anti-Viral Immune Responses through the Production of Interferon-α/β at the Initial Stage of Influenza A Virus (H3N2) Infection, Immune Netw, doi:10.4110/in.2013.13.2.70
Klinkhammer, Schnepf, Ye, Schwaderlapp, Gad et al., IFN-λ Prevents Influenza Virus Spread from the Upper Airways to the Lungs and Limits Virus Transmission, eLife, doi:10.7554/eLife.33354
Kumari, Dembra, Dembra, Bhawna, Gul et al., The Role of Vitamin C as Adjuvant Therapy in COVID-19, Cureus, doi:10.7759/cureus.11779
Langlois, Manzanares, Adhikari, Lamontagne, Stoppe et al., Vitamin C Administration to the Critically Ill: A Systematic Review and Meta-Analysis, J. Parenter. Enter. Nutr, doi:10.1002/jpen.1471
Lee, Gardner, Porter, Louis, Ahmed et al., Current Concepts in the Diagnosis and Management of Cytokine Release Syndrome, Blood, doi:10.1182/blood-2014-05-552729
Lee, Ortiz-Reyes, Lew, Hasan, Ke et al., Intravenous Vitamin C Monotherapy in Critically Ill Patients: A Systematic Review and Meta-Analysis of Randomized Controlled Trials with Trial Sequential Analysis, Ann. Intensive Care, doi:10.1186/s13613-023-01116-x
Li, Ching, Hipple, Lopez, Sahibzada et al., Use of Intravenous Vitamin C in Critically Ill Patients With COVID-19 Infection, J. Pharm. Pract, doi:10.1177/08971900211015052
Li, Geng, Peng, Meng, Lu, Molecular Immune Pathogenesis and Diagnosis of COVID-19, J. Pharm. Anal, doi:10.1016/j.jpha.2020.03.001
Lin, Xu, Lv, Han, Xiang et al., An NLRP3 Inflammasome-Triggered Cytokine Storm Contributes to Streptococcal Toxic Shock-like Syndrome (STSLS), PLoS Pathog, doi:10.1371/journal.ppat.1007795
Linster, Van Schaftingen, Vitamin, Biosynthesis, Recycling and Degradation in Mammals, FEBS J, doi:10.1111/j.1742-4658.2006.05607.x
Litwak, Cho, Nguyen, Moussavi, Bushell et al., Hydrocortisone, and Thiamine for the Treatment of Severe Sepsis and Septic Shock: A Retrospective Analysis of Real-World Application, J. Clin. Med, doi:10.3390/jcm8040478
Liu, Liu, Xiang, Pu, Xiong et al., Neutrophil-to-Lymphocyte Ratio Predicts Critical Illness Patients with 2019 Coronavirus Disease in the Early Stage, J. Transl. Med, doi:10.1186/s12967-020-02374-0
Liugan, Carr, Vitamin C and Neutrophil Function: Findings from Randomized Controlled Trials, Nutrients, doi:10.3390/nu11092102
Lui, Guaraldi, Drug Treatment of COVID-19 Infection, Curr. Opin. Pulm. Med, doi:10.1097/MCP.0000000000000953
Mangalmurti, Hunter, Cytokine Storms: Understanding COVID-19, Immunity, doi:10.1016/j.immuni.2020.06.017
Manning, Mitchell, Appadurai, Shakya, Pierce et al., Vitamin C Promotes Maturation of T-Cells, Antioxid. Redox Signal, doi:10.1089/ars.2012.4988
Marik, Khangoora, Rivera, Hooper, Catravas, Hydrocortisone, Vitamin C, and Thiamine for the Treatment of Severe Sepsis and Septic Shock: A Retrospective Before-After Study, Chest, doi:10.1016/j.chest.2016.11.036
May, Harrison, Role of Vitamin C in the Function of the Vascular Endothelium, Antioxid. Redox Signal, doi:10.1089/ars.2013.5205
Medzhitov, Recognition of Microorganisms and Activation of the Immune Response, Nature, doi:10.1038/nature06246
Milani, Macchi, Guz-Mark, Vitamin C in the Treatment of COVID-19, Nutrients, doi:10.3390/nu13041172
Myint, Wilson, Clark, Luben, Wareham et al., Plasma Vitamin C Concentrations and Risk of Incident Respiratory Diseases and Mortality in the European Prospective Investigation into Cancer-Norfolk Population-Based Cohort Study, Eur. J. Clin. Nutr, doi:10.1038/s41430-019-0393-1
Newton, Cardani, Braciale, The Host Immune Response in Respiratory Virus Infection: Balancing Virus Clearance and Immunopathology, Semin. Immunopathol, doi:10.3390/antiox11071247
Noris, Benigni, Remuzzi, The Case of Complement Activation in COVID-19 Multiorgan Impact, Kidney Int, doi:10.1016/j.kint.2020.05.013
Olczak-Pruc, Swieczkowski, Ladny, Pruc, Juarez-Vela et al., Vitamin C Supplementation for the Treatment of COVID-19: A Systematic Review and Meta-Analysis, Nutrients, doi:10.3390/nu14194217
Osuchowski, Winkler, Skirecki, Cajander, Shankar-Hari et al., The COVID-19 Puzzle: Deciphering Pathophysiology and Phenotypes of a New Disease Entity, Lancet Respir. Med, doi:10.1016/S2213-2600(21)00218-6
Padayatty, Katz, Wang, Eck, Kwon et al., Vitamin C as an Antioxidant: Evaluation of Its Role in Disease Prevention, J. Am. Coll. Nutr, doi:10.1080/07315724.2003.10719272
Padayatty, Sun, Wang, Riordan, Hewitt et al., Vitamin C Pharmacokinetics: Implications for Oral and Intravenous Use, Ann. Intern. Med, doi:10.7326/0003-4819-140-7-200404060-00010
Parasher, COVID-19: Current Understanding of Its Pathophysiology, Clinical Presentation and Treatment, Postgrad. Med. J, doi:10.1136/postgradmedj-2020-138577
Ramasamy, Subbian, Critical Determinants of Cytokine Storm and Type I Interferon Response in COVID-19 Pathogenesis, Clin. Microbiol. Rev, doi:10.1128/CMR.00299-20
Rawat, Roy, Maitra, Shankar, Khanna et al., Vitamin D Supplementation and COVID-19 Treatment: A Systematic Review and Meta-Analysis, Diabetes Metab. Syndr, doi:10.1016/j.dsx.2021.102189
Rodrigues, De Sá, Ishimoto, Becerra, Oliveira et al., Inflammasomes Are Activated in Response to SARS-CoV-2 Infection and Are Associated with COVID-19 Severity in Patients, J. Exp. Med, doi:10.1084/jem.20201707
Rydyznski Moderbacher, Ramirez, Dan, Grifoni, Hastie et al., Antigen-Specific Adaptive Immunity to SARS-CoV-2 in Acute COVID-19 and Associations with Age and Disease Severity, Cell, doi:10.1016/j.cell.2020.09.038
Sharma, Sumanadasa, Shahi, Woodman, Mangoni et al., Efficacy and Safety of Vitamin C Supplementation in the Treatment of Community-Acquired Pneumonia: A Systematic Review and Meta-Analysis with Trial Sequential Analysis, Sci. Rep, doi:10.1038/s41598-024-62571-5
Shilotri, Bhat, Effect of Mega Doses of Vitamin C on Bactericidal Ativity of Leukocytes, Am. J. Clin. Nutr, doi:10.1093/ajcn/30.7.1077
Shimabukuro-Vornhagen, Gödel, Subklewe, Stemmler, Schlößer et al., Cytokine Release Syndrome, J. Immunother. Cancer, doi:10.1186/s40425-018-0343-9
Szarpak, Pruc, Gasecka, Jaguszewski, Michalski et al., Should We Supplement Zinc in COVID-19 Patients? Evidence from a Meta-Analysis, Pol. Arch. Intern. Med, doi:10.20452/pamw.16048
Takahashi, Ellingson, Wong, Israelow, Lucas et al., Sex Differences in Immune Responses That Underlie COVID-19 Disease Outcomes, Nature, doi:10.1038/s41586-020-2700-3
Teafatiller, Agrawal, De Robles, Rahmatpanah, Subramanian et al., Vitamin C Enhances Anti-viral Functions of Lung Epithelial Cells, Biomolecules, doi:10.3390/biom11081148
Tian, Zhang, Jin, Feng, Wang et al., Immune Suppression in the Early Stage of COVID-19 Disease, Nat. Commun, doi:10.1038/s41467-020-19706-9
Van De Veerdonk, Netea, Van Deuren, Van Der Meer, De Mast et al., Kallikrein-Kinin Blockade in Patients with COVID-19 to Prevent Acute Respiratory Distress Syndrome, eLife, doi:10.7554/eLife.57555
Van Eijk, Binkhorst, Bourgonje, Offringa, Mulder et al., COVID-19: Immunopathology, Pathophysiological Mechanisms, and Treatment Options, J. Pathol, doi:10.1002/path.5642
Vissers, Wilkie, Ascorbate Deficiency Results in Impaired Neutrophil Apoptosis and Clearance and Is Associated with Up-Regulation of Hypoxia-Inducible Factor 1α, J. Leukoc. Biol, doi:10.1189/jlb.0806541
Vollbracht, Kraft, Feasibility of Vitamin C in the Treatment of Post Viral Fatigue with Focus on Long COVID, Based on a Systematic Review of IV Vitamin C on Fatigue, Nutrients, doi:10.3390/nu13041154
Wang, Hu, Hu, Zhu, Liu et al., Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China, JAMA, doi:10.1001/jama.2020.1585
Wang, Nie, Wang, Zhao, Xiong et al., Characteristics of Peripheral Lymphocyte Subset Alteration in COVID-19 Pneumonia, J. Infect. Dis, doi:10.1093/infdis/jiaa150
Waterer, Understanding COVID-19 Pathophysiology: What Defines Progress?, Am. J. Respir. Cell Mol. Biol, doi:10.1165/rcmb.2021-0452ED
Wei, Wang, Liao, Guo, Wen et al., Efficacy of Vitamin C in Patients with Sepsis: An Updated Meta-Analysis, Eur. J. Pharmacol, doi:10.1016/j.ejphar.2019.172889
Williamson, Walker, Bhaskaran, Bacon, Bates et al., Factors Associated with COVID-19-Related Death Using OpenSAFELY, Nature, doi:10.1038/s41586-020-2521-4
Xia, Cao, Xie, Zhang, Chen et al., Evasion of Type I Interferon by SARS-CoV-2, Cell Rep, doi:10.1016/j.celrep.2020.108234
Xu, Shi, Wang, Zhang, Huang et al., Pathological Findings of COVID-19 Associated with Acute Respiratory Distress Syndrome, Lancet Respir. Med, doi:10.1016/S2213-2600(20)30076-X
Zaim, Chong, Sankaranarayanan, Harky, COVID-19 and Multiorgan Response, Curr. Probl. Cardiol, doi:10.1016/j.cpcardiol.2020.100618
Zhang, Jativa, Vitamin C Supplementation in the Critically Ill: A Systematic Review and Meta-Analysis, SAGE Open Med, doi:10.1177/2050312118807615
Zhang, Rao, Li, Zhu, Liu et al., Pilot Trial of High-Dose Vitamin C in Critically Ill COVID-19 Patients, Ann. Intensive Care, doi:10.1186/s13613-020-00792-3
Zhang, Tan, Ling, Lu, Liu et al., Viral and Host Factors Related to the Clinical Outcome of COVID-19, Nature, doi:10.1038/s41586-020-2355-0
Zhao, Di, Xu, The NLRP3 Inflammasome and COVID-19: Activation, Pathogenesis and Therapeutic Strategies, Cytokine Growth Factor. Rev, doi:10.1016/j.cytogfr.2021.06.002
Zhou, Fu, Zheng, Wang, Zhao et al., Pathogenic T-Cells and Inflammatory Monocytes Incite Inflammatory Storms in Severe COVID-19 Patients, Natl. Sci. Rev, doi:10.1093/nsr/nwaa041
Zhu, Zhang, Wang, Li, Yang et al., A Novel Coronavirus from Patients with Pneumonia in China, N Engl. J. Med, doi:10.1056/NEJMoa2001017
Zuo, Yalavarthi, Shi, Gockman, Zuo et al., Neutrophil Extracellular Traps in COVID-19, J.C.I. Insight, doi:10.1172/jci.insight.138999