Clinical Prognosis and Risk Factors of Death for Covid-19 Patients Complicated with Coronary Heart Disease/Diabetes/Hypertension-A Retrospective, Real-World Study
et al., Elsevier BV, doi:10.2139/ssrn.4488145, Jun 2023
Retrospective 1,281 COVID-19 patients with comorbidities in China, showing 2% lower mortality with paxlovid.
Resistance. Variants may be resistant to paxlovid1-8. Use may promote the emergence of variants that weaken host immunity and potentially contribute to long COVID9. Confounding by contraindication. Hoertel et al. find that over 50% of patients that died had a contraindication for the use of Paxlovid10. Retrospective studies that do not exclude contraindicated patients may significantly overestimate efficacy. Black box warning. The FDA notes that severe, life-threatening, and/or fatal adverse reactions due to drug interactions have been reported in patients treated with paxlovid11. Kidney and liver injury. Studies show significantly increased risk of acute kidney injury12 and liver injury13,14. Viral rebound. Studies show significantly increased risk of replication-competent viral rebound15-17.
Standard of Care (SOC) for COVID-19 in the study country,
China, is average with moderate efficacy for approved treatments18.
|
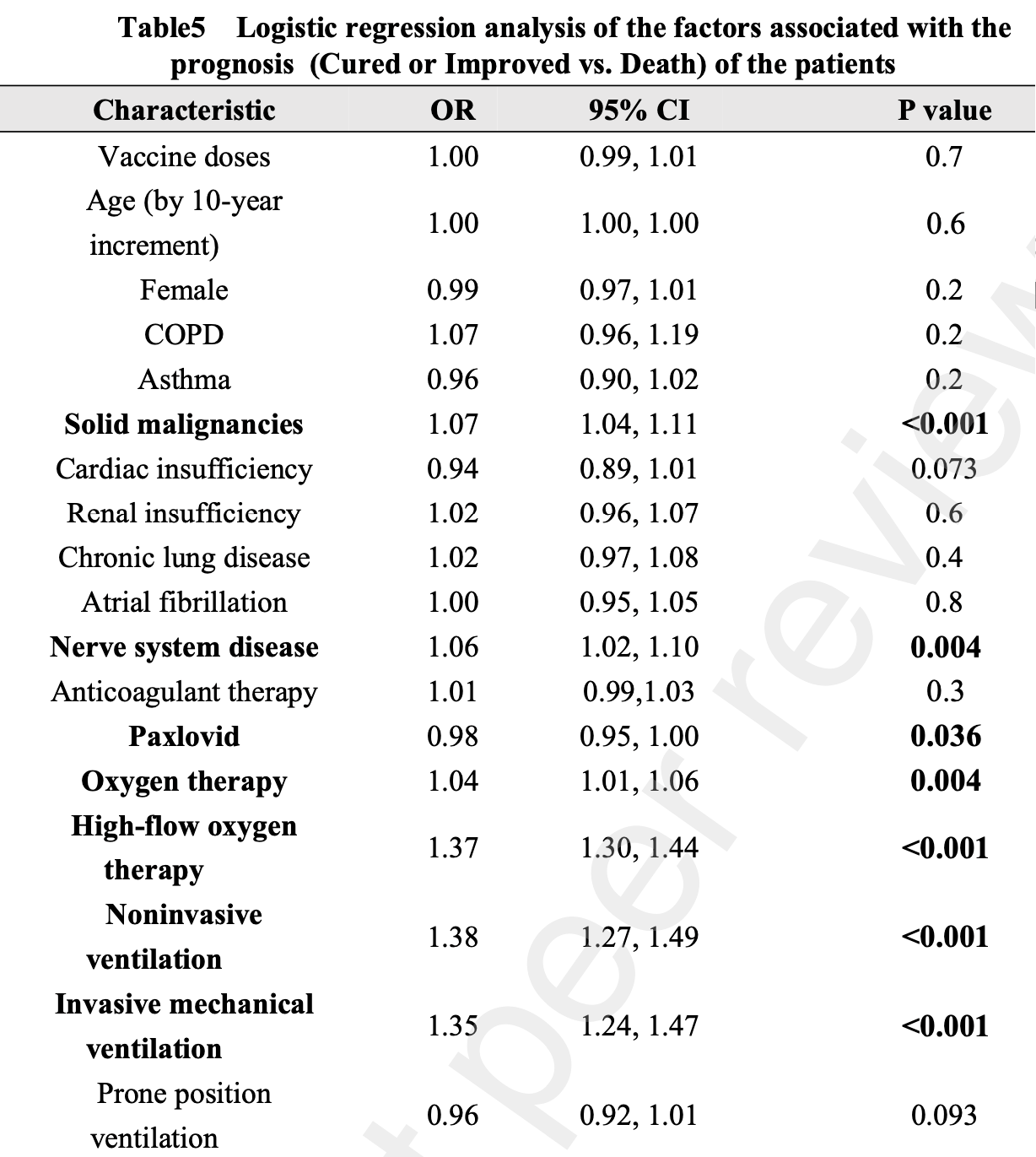
risk of death, 2.0% lower, OR 0.98, p = 0.04, treatment 220, control 1,061, adjusted per study, multivariable, RR approximated with OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
1.
Zhou et al., Nirmatrelvir-resistant SARS-CoV-2 variants with high fitness in an infectious cell culture system, Science Advances, doi:10.1126/sciadv.add7197.
2.
Moghadasi et al., Rapid resistance profiling of SARS-CoV-2 protease inhibitors, npj Antimicrobials and Resistance, doi:10.1038/s44259-023-00009-0.
3.
Jochmans et al., The Substitutions L50F, E166A, and L167F in SARS-CoV-2 3CLpro Are Selected by a Protease Inhibitor In Vitro and Confer Resistance To Nirmatrelvir, mBio, doi:10.1128/mbio.02815-22.
4.
Lopez et al., SARS-CoV-2 Resistance to Small Molecule Inhibitors, Current Clinical Microbiology Reports, doi:10.1007/s40588-024-00229-6.
5.
Zvornicanin et al., Molecular Mechanisms of Drug Resistance and Compensation in SARS-CoV-2 Main Protease: The Interplay Between E166 and L50, bioRxiv, doi:10.1101/2025.01.24.634813.
6.
Vukovikj et al., Impact of SARS-CoV-2 variant mutations on susceptibility to monoclonal antibodies and antiviral drugs: a non-systematic review, April 2022 to October 2024, Eurosurveillance, doi:10.2807/1560-7917.ES.2025.30.10.2400252.
7.
Deschenes et al., Functional and structural characterization of treatment-emergent nirmatrelvir resistance mutations at low frequencies in the main protease (Mpro) reveals a unique evolutionary route for SARS-CoV-2 to gain resistance, The Journal of Infectious Diseases, doi:10.1093/infdis/jiaf294.
8.
Zhou (B) et al., SARS-CoV-2 Mpro inhibitor ensitrelvir: asymmetrical cross-resistance with nirmatrelvir and emerging resistance hotspots, Emerging Microbes & Infections, doi:10.1080/22221751.2025.2552716.
9.
Thomas et al., Nirmatrelvir-Resistant Mutations in SARS-CoV-2 Mpro Enhance Host Immune Evasion via Cleavage of NF-κB Essential Modulator, bioRxiv, doi:10.1101/2024.10.18.619137.
10.
Hoertel et al., Prevalence of Contraindications to Nirmatrelvir-Ritonavir Among Hospitalized Patients With COVID-19 at Risk for Progression to Severe Disease, JAMA Network Open, doi:10.1001/jamanetworkopen.2022.42140.
11.
FDA, Fact sheet for healthcare providers: emergency use authorization for paxlovid, www.fda.gov/media/155050/download.
12.
Kamo et al., Association of Antiviral Drugs for the Treatment of COVID-19 With Acute Renal Failure, In Vivo, doi:10.21873/invivo.13637.
13.
Wang et al., Development and validation of a nomogram to assess the occurrence of liver dysfunction in patients with COVID-19 pneumonia in the ICU, BMC Infectious Diseases, doi:10.1186/s12879-025-10684-1.
14.
Siby et al., Temporal Trends in Serious Adverse Events Associated with Oral Antivirals During the COVID-19 Pandemic: Insights from the FAERS Database (2020–2023), Open Forum Infectious Diseases, doi:10.1093/ofid/ofaf695.1825.
15.
Edelstein et al., SARS-CoV-2 virologic rebound with nirmatrelvir-ritonavir therapy, medRxiv, doi:10.1101/2023.06.23.23288598.
16.
Shah et al., SARS-CoV-2 infectious shedding and rebound among adults with and without oral antiviral use: two case-ascertained prospective household studies, The Lancet Microbe, doi:10.1016/j.lanmic.2025.101227.
Yang et al., 22 Jun 2023, retrospective, China, preprint, mean age 70.5, 22 authors, study period 1 March, 2022 - 30 June, 2022.
Contact: jwx02467@gmail.com, ff4719@yahoo.com, bai.chunxue@zs-hospital.sh.cn, ylsong70@163.com, yang.dawei@zs-hospital.sh.cn, whf6296@163.com, lijing@centennialsci.com, 854719218@qq.com, ju.minjie@zs-hospital.sh.cn, wang.hao@zs-hospital.sh.cn, jia.yicheng@zs-hospital.sh.cn, wang.xiaodan@zs-hospital.sh.cn, fan.jia@zs-hospital.sh.cn, yan.zuoqin@zs-hospital.sh.cn, zhou.jian@fudan.edu.cn, chencuicui001@126.com, yinzhoufeng@163.com, 624630944@qq.com, houdn2014@126.com, luxingwei@centennialsci.com, johnny.yang@suvalue.com, grace.wu@suvalue.com.
Clinical prognosis and risk factors of death for COVID-19 patients complicated with coronary heart disease/diabetes/hypertension-a retrospective, real-world study
Objectives : To explore the clinical prognosis and the risk factors of death of COVID-19 patients complicated with one of the three major comorbidities (coronary heart disease, diabetes, or hypertension) based on real-world data. Methods: This single-center retrospective real-world study investigated all in-hospital patients who were transferred to the Coronavirus Special Ward of the Elderly Center of Zhongshan Hospital from March to June 2022 with a positive COVID-19 virus nucleic acid test and with at least one of the three comorbidities (coronary heart disease, diabetes or hypertension). Clinical data and laboratory test results of eligible patients were collected.A multivariate logistic regression analysis was performed to explore the risk associated with the prognosis. Results:For the 1,281 PCR positive patients at the admission included in the analysis, the mean age was 70.5±13.7 years and 658 (51.4%) were males. There were 1,092 (85.2%) patients with hypertension, 477(37.2%) patients with diabetes, and 124 (9.7%) patients with coronary heart disease. The length of hospital stay (LOS) was 9.2±5.1 days. Among all admitted patients,1112 (91.5%) were fully recovered, 77 (6.9%) were improved, and 29 (2.6%) died. Over the hospitalization, 172 (13.4%) PCR positive patients experienced rebound COVID following initial recovery with negative PCR test. A multivariate logistic regression analysis showed that vaccination had no protective effects in this study population; Paxlovid was associated with a lower risk of death(OR =0 .98, 95% CI: 0.95-1.00). Whereas, presence of solid malignancies and nerve system disease were significantly associated with increased risk of death (OR=1.04, 95%
Conflict of Interest Huifen Weng, Lijing, Xingwei Lu were employed by Shanghai Centennial Scientific Co., Ltd. Shanghai, China.Wei Yang were employed by Shanghai Suvalue Healthcare Scientific Co., Ltd. Shanghai, China. The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest. This preprint research paper has not been peer reviewed. Electronic copy available at: https://ssrn.com/abstract=4488145 P r e p r i n t n o t p e e r r e v i e w e d
Appendix Table 1A COVID-19 Diagnosis and Treatment Protocol (Trial Version 9)
Clinical type Clinical symptoms
Mild The clinical symptoms were mild, and no pneumonia was observed on imaging.
Moderate With the above clinical manifestations, imaging findings of pneumonia. This preprint research paper has not been peer reviewed. Electronic copy available at: https://ssrn.com/abstract=4488145 P r e p r i n t n o t p e e r r e v i e w e d
12/13 Severe Adults meet any of the following criteria :1. Shortness of breath, RR ≥ 30 times/min; 2. In the resting state, oxygen saturation ≤ 93% when inhaling air; Arterial partial pressure of oxygen (PaO2) / oxygen concentration (FiO2) ≤ 300mmHg (1mmHg = 0.133kPa); The PaO2/FiO2 should be calibrated according to the following formula for high altitudes (above 1000m): PaO2/FiO2×[760/ atmospheric pressure (mmHg)]. 4. The clinical symptoms were progressively aggravated, and the..
References
Ahmad M, Shinde, The Impact of COVID-19 On Comorbidities: A Review Of Recent Updates For Combating It[J], Saudi J Biol Sci
Al K N, Zhang, Xia, Effect of 2 Inactivated SARS-CoV-2 Vaccines on Symptomatic COVID-19 Infection in Adults: A Randomized Clinical Trial, JAMA
Cheng S, Wang P H, The Benefits of Molnupiravir Treatment in Healthcare Facilities Patients with COVID-19[J], Drug Des Devel Ther
Coupland C A, Mehta N, Risk prediction of covid-19 related death and hospital admission in adults after covid-19 vaccination: national prospective cohort study, BMJ
Fu, Yuan, Clinical characteristics of coronavirus disease 2019 (COVID-19) in China: A systematic review and meta-analysis[J], J Infect
Guan W, Liang W H, Zhao, Comorbidity and its impact on 1590 patients with COVID-19 in China: a nationwide analysis[J], Eur Respir J
Lopez B, Andrews, Gower, Effectiveness of the Pfizer-BioNTech and Oxford-AstraZeneca vaccines on covid-19 related symptoms, hospital admissions, and mortality in older adults in England: test negative case-control study, BMJ
Mcmenamin M E, Vaccine effectiveness of one, two, and three doses of BNT162b2 and CoronaVac against COVID-19 in Hong Kong: a population-based observational study, Lancet Infect Dis
Saglik, Ener, Akalin, Association of SARS-CoV-2 cycle threshold (Ct) values with clinical course and serum biomarkers in COVID-19 patients[J], J Infect Dev Ctries
Tang, Efficacy and safety of three new oral antiviral treatment (molnupiravir, fluvoxamine and Paxlovid) for COVID-19:a meta-analysis[J], Ann Med
Xie, You, Wu, Impact of Cardiovascular Disease on Clinical Characteristics and Outcomes of Coronavirus Disease 2019 (COVID-19)[J], Circ J
Yang, Weng, Wang R, Evaluation of COVID-19 vaccines in primary prevention against infections and reduction in severity of illness following the outbreak of SARS-CoV-2 omicron variant in Shanghai[J], Front Med (Lausanne)
DOI record:
{
"DOI": "10.2139/ssrn.4488145",
"URL": "http://dx.doi.org/10.2139/ssrn.4488145",
"author": [
{
"affiliation": [],
"family": "Yang",
"given": "Dawei",
"sequence": "first"
},
{
"affiliation": [],
"family": "Weng",
"given": "Huifeng",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Li",
"given": "Jing",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ju",
"given": "MinJie",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Wang",
"given": "Hao",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Jia",
"given": "Yi-Chen",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Wang",
"given": "Xiao-Dan",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Fan",
"given": "Jia",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Yan",
"given": "Zuoqin",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Zhou",
"given": "Jian",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Chen",
"given": "Cuicui",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Feng",
"given": "Yin-zhou",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Chen",
"given": "Xiao-yan",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Hou",
"given": "Dong-ni",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Lu",
"given": "Xing-wei",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Yang",
"given": "Wei",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Wu",
"given": "Yin",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Chen",
"given": "Zheng-Guo",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Hu",
"given": "Xiao-han",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Xuan",
"given": "Jian-Wei",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Bai",
"given": "Chunxue",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Song",
"given": "Yuanlin",
"sequence": "additional"
}
],
"container-title": [],
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2023,
6,
24
]
],
"date-time": "2023-06-24T11:34:40Z",
"timestamp": 1687606480000
},
"deposited": {
"date-parts": [
[
2023,
6,
24
]
],
"date-time": "2023-06-24T11:34:41Z",
"timestamp": 1687606481000
},
"group-title": "SSRN",
"indexed": {
"date-parts": [
[
2023,
6,
25
]
],
"date-time": "2023-06-25T04:36:54Z",
"timestamp": 1687667814567
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2023
]
]
},
"member": "78",
"original-title": [],
"posted": {
"date-parts": [
[
2023
]
]
},
"prefix": "10.2139",
"published": {
"date-parts": [
[
2023
]
]
},
"publisher": "Elsevier BV",
"reference-count": 0,
"references-count": 0,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.ssrn.com/abstract=4488145"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subtitle": [],
"subtype": "preprint",
"title": "Clinical Prognosis and Risk Factors of Death for Covid-19 Patients Complicated with Coronary Heart Disease/Diabetes/Hypertension-A Retrospective, Real-World Study",
"type": "posted-content"
}