Repurposing Niclosamide as a Novel Anti-SARS-CoV-2 Drug by Restricting Entry Protein CD147
et al., Biomedicines, doi:10.3390/biomedicines11072019, Jul 2023
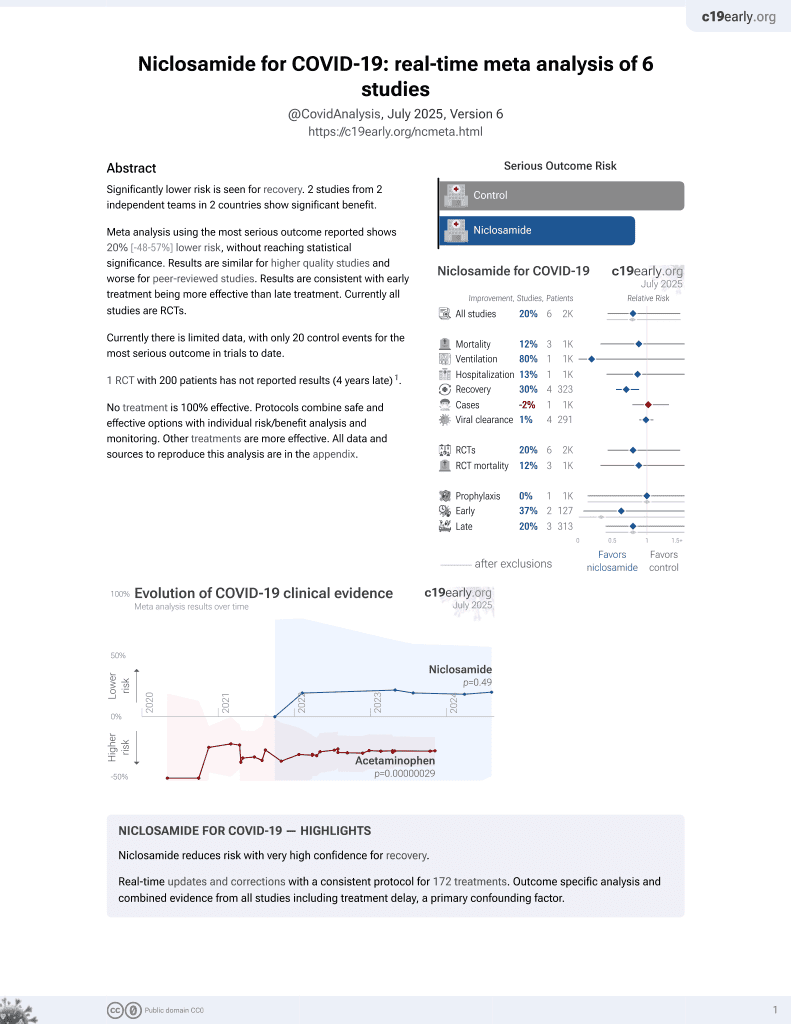
56th treatment shown to reduce risk in
August 2025, now with p = 0.0069 from 7 studies.
Lower risk for recovery.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
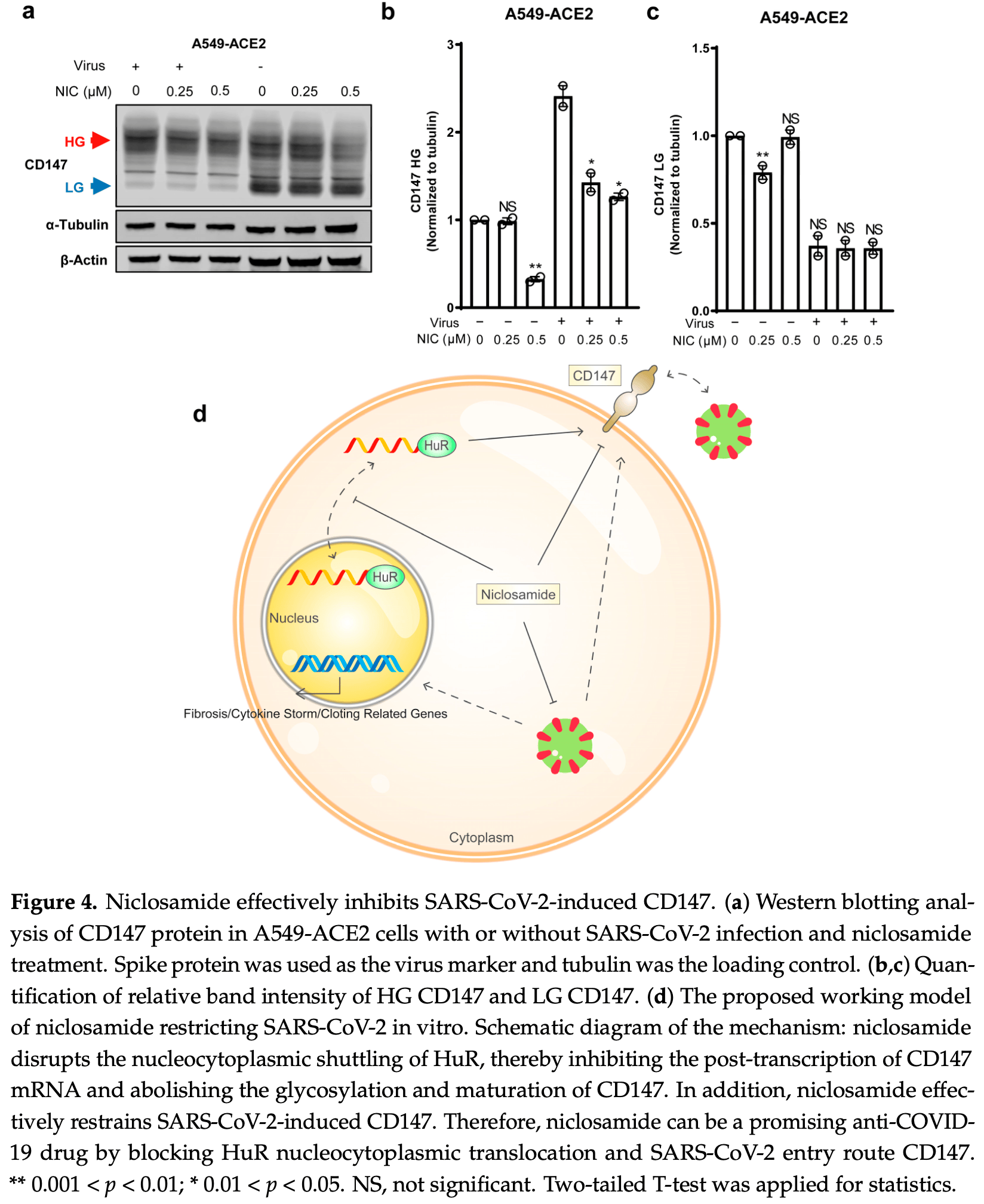
In vitro study showing that niclosamide reduces CD147 protein levels and inhibits SARS-CoV-2-induced upregulation of CD147 in A549-ACE2 cells. Authors find that the RNA-binding protein HuR binds to the 3'-UTR of BSG mRNA and upregulates CD147 expression. Niclosamide inhibits the nucleocytoplasmic translocation of HuR and reduces CD147 levels in various cell lines, including respiratory cell lines WI-38, NL20, and H460. Niclosamide also effectively suppressed the SARS-CoV-2-induced increase in the highly glycosylated form of CD147, which has been implicated in COVID-19 disease progression and post-COVID-19 cardiac complications.
9 preclinical studies support the efficacy of niclosamide for COVID-19:
In silico studies predict inhibition of SARS-CoV-2 with niclosamide or metabolites via binding to the spikeA,1, MproB,1, RNA-dependent RNA polymeraseC,1, PLproD,1, nucleocapsidE,1, and helicaseF,1 proteins.
Niclosamide inhibits endolysosomal acidification and suppresses
TLR3-mediated pro-inflammatory signaling in human small airway
epithelial cells stimulated with TLR3 agonists mimicking viral RNA2, modulates host lipid metabolism and reduces
infectious SARS-CoV-2 virion production in Vero E6 cells4, reduces CD147 protein levels and inhibits
SARS-CoV-2-induced upregulation of CD147 in A549-ACE2 cells, including
the highly glycosylated form of CD147 which has been implicated in
COVID-19 disease progression and post-COVID-19 cardiac complications5, blocked the formation of syncytia mediated by
SARS-CoV-2 spike protein pseudovirus-producing cells6, may reduce inflammation, NLRP3 formation, and
caspase-1 activity9, may inhibit viral uncoating, replication, and
assembly via disruption of pH gradients and reduced ATP production in
host cells8, may counter immune evasion by reversing E-, ORF7a-, and ORF8-mediated down-regulation of MHC-I, preserving CD8⁺ T-cell recognition10, and shows strong synergy when combined with
ivermectin7.
1.
Haque et al., Exploring potential therapeutic candidates against COVID-19: a molecular docking study, Discover Molecules, doi:10.1007/s44345-024-00005-5.
2.
Pejler et al., Blockade of endolysosomal acidification suppresses TLR3-mediated pro-inflammatory signaling in airway epithelial cells, Journal of Allergy and Clinical Immunology, doi:10.1016/j.jaci.2024.05.031.
3.
Walia et al., SARS-CoV-2 virulence factor ORF3a blocks lysosome function by modulating TBC1D5-dependent Rab7 GTPase cycle, Nature Communications, doi:10.1038/s41467-024-46417-2.
4.
Garrett et al., Niclosamide as a chemical probe for analyzing SARS-CoV-2 modulation of host cell lipid metabolism, Frontiers in Microbiology, doi:10.3389/fmicb.2023.1251065.
5.
Yang et al., Repurposing Niclosamide as a Novel Anti-SARS-CoV-2 Drug by Restricting Entry Protein CD147, Biomedicines, doi:10.3390/biomedicines11072019.
6.
Sheng et al., A pseudovirus-based method to dynamically mimic SARS-CoV-2-associated cell-to-cell fusion and transmission, Acta Biochimica et Biophysica Sinica, doi:10.3724/abbs.2023129.
7.
Jitobaom et al., Synergistic anti-SARS-CoV-2 activity of repurposed anti-parasitic drug combinations, BMC Pharmacology and Toxicology, doi:10.1186/s40360-022-00580-8.
8.
Needham, D., The pH Dependence of Niclosamide Solubility, Dissolution, and Morphology: Motivation for Potentially Universal Mucin-Penetrating Nasal and Throat Sprays for COVID19, its Variants and other Viral Infections, Pharmaceutical Research, doi:10.1007/s11095-021-03112-x.
a.
The trimeric spike (S) protein is a glycoprotein that mediates viral entry by binding to the host ACE2 receptor, is critical for SARS-CoV-2's ability to infect host cells, and is a target of neutralizing antibodies. Inhibition of the spike protein prevents viral attachment, halting infection at the earliest stage.
b.
The main protease or Mpro, also known as 3CLpro or nsp5, is a cysteine protease that cleaves viral polyproteins into functional units needed for replication. Inhibiting Mpro disrupts the SARS-CoV-2 lifecycle within the host cell, preventing the creation of new copies.
c.
RNA-dependent RNA polymerase (RdRp), also called nsp12, is the core enzyme of the viral replicase-transcriptase complex that copies the positive-sense viral RNA genome into negative-sense templates for progeny RNA synthesis. Inhibiting RdRp blocks viral genome replication and transcription.
d.
The papain-like protease (PLpro) has multiple functions including cleaving viral polyproteins and suppressing the host immune response by deubiquitination and deISGylation of host proteins. Inhibiting PLpro may block viral replication and help restore normal immune responses.
e.
The nucleocapsid (N) protein binds and encapsulates the viral genome by coating the viral RNA. N enables formation and release of infectious virions and plays additional roles in viral replication and pathogenesis. N is also an immunodominant antigen used in diagnostic assays.
f.
The helicase, or nsp13, protein unwinds the double-stranded viral RNA, a crucial step in replication and transcription. Inhibition may prevent viral genome replication and the creation of new virus components.
Yang et al., 18 Jul 2023, peer-reviewed, 9 authors.
Contact: xul@ku.edu (corresponding author), ejones11@kumc.edu.
In vitro studies are an important part of preclinical research, however results may be very different in vivo.
Repurposing Niclosamide as a Novel Anti-SARS-CoV-2 Drug by Restricting Entry Protein CD147
Biomedicines, doi:10.3390/biomedicines11072019
The outbreak of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has led to the global coronavirus disease 2019 (COVID-19) pandemic, and the search for effective treatments has been limited. Furthermore, the rapid mutations of SARS-CoV-2 have posed challenges to existing vaccines and neutralizing antibodies, as they struggle to keep up with the increased viral transmissibility and immune evasion. However, there is hope in targeting the CD147-spike protein, which serves as an alternative point for the entry of SARS-CoV-2 into host cells. This protein has emerged as a promising therapeutic target for the development of drugs against COVID-19. Here, we demonstrate that the RNA-binding protein Human-antigen R (HuR) plays a crucial role in the post-transcriptional regulation of CD147 by directly binding to its 3 -untranslated region (UTR). We observed a decrease in CD147 levels across multiple cell lines upon HuR depletion. Furthermore, we identified that niclosamide can reduce CD147 by lowering the cytoplasmic translocation of HuR and reducing CD147 glycosylation. Moreover, our investigation revealed that SARS-CoV-2 infection induces an upregulation of CD147 in ACE2-expressing A549 cells, which can be effectively neutralized by niclosamide in a dose-dependent manner. Overall, our study unveils a novel regulatory mechanism of regulating CD147 through HuR and suggests niclosamide as a promising therapeutic option against COVID-19.
Author Contributions: Z.Y. contributed to experimental design, execution, and data analysis as well as the writing of this manuscript; Q.Z. contributed to experimental execution, data analysis, and manuscript revision; S.H. contributed to the SARS-CoV-2 infection assay; X.H. contributed to experimental design and execution. E.J. contributed to the immunohistochemical staining assay; Y.Z., X.W., and J.Q. provided material support, assisted with experimental design, and revised the manuscript; L.X. oversaw all experimental design, execution, analysis, interpretation, and communication of results as well as manuscript revision. All authors have read and agreed to the published version of the manuscript.
Abbreviations
References
Adamsick, Gandhi, Bidell, Elshaboury, Bhattacharyya et al., Remdesivir in Patients with Acute or Chronic Kidney Disease and COVID-19, J. Am. Soc. Nephrol, doi:10.1681/ASN.2020050589
Adhikary, Kandel, Mamani, Mustafa, Hao et al., Discovery of Small Anti-ACE2 Peptides to Inhibit SARS-CoV-2 Infectivity, Adv. Ther, doi:10.1002/adtp.202100087
Avolio, Carrabba, Milligan, Williamson, Beltrami et al., The SARS-CoV-2 Spike protein disrupts human cardiac pericytes function through CD147 receptor-mediated signalling: A potential non-infective mechanism of COVID-19 microvascular disease, Clin. Sci, doi:10.1042/CS20210735
Badeti, Jiang, Naghizadeh, Tseng, -C.; Bushkin et al., Development of a novel human CD147 knock-in NSG mouse model to test SARS-CoV-2 viral infection, Cell Biosci, doi:10.1186/s13578-022-00822-6
Barrett, Bilaloglu, Cornwell, Burgess, Virginio et al., Platelets contribute to disease severity in COVID-19, J. Thromb. Haemost, doi:10.1111/jth.15534
Beigel, Tomashek, Dodd, Mehta, Zingman et al., Remdesivir for the Treatment of COVID-19-Final Report, N. Engl. J. Med, doi:10.1056/NEJMoa2007764
Bian, Zheng, Wei, Wen, Zhang et al., Safety and efficacy of meplazumab in healthy volunteers and COVID-19 patients: A randomized phase 1 and an exploratory phase 2 trial, Signal Transduct. Target. Ther, doi:10.1038/s41392-021-00603-6
Boyapally, Pulivendala, Bale, Godugu, Niclosamide alleviates pulmonary fibrosis in vitro and in vivo by attenuation of epithelial-to-mesenchymal transition, matrix proteins & Wnt/β-catenin signaling: A drug repurposing study, Life Sci, doi:10.1016/j.lfs.2018.12.061
Braga, Ali, Secco, Chiavacci, Neves et al., Drugs that inhibit TMEM16 proteins block SARS-CoV-2 spike-induced syncytia, Nature, doi:10.1038/s41586-021-03491-6
Chang, Zhen, Liu, Ren, Hu et al., The antihelmenthic phosphate niclosamide impedes renal fibrosis by inhibiting homeodomain-interacting protein kinase 2 expression, Kidney Int, doi:10.1016/j.kint.2017.01.018
De Almeida, Da Silva, Rodrigues, Oliveira, Ishimoto et al., Identification of immunomodulatory drugs that inhibit multiple inflammasomes and impair SARS-CoV-2 infection, Sci. Adv, doi:10.1126/sciadv.abo5400
Figarola, Singhal, Singhal, Kusari, Riggs, Bioenergetic modulation with the mitochondria uncouplers SR4 and niclosamide prevents proliferation and growth of treatment-naïve and vemurafenib-resistant melanomas, Oncotarget
Gassen, Niemeyer, Muth, Corman, Martinelli et al., SKP2 attenuates autophagy through Beclin1-ubiquitination and its inhibition reduces MERS-Coronavirus infection, Nat. Commun, doi:10.1038/s41467-019-13659-4
Geng, Chen, Yuan, Wang, Wang et al., CD147 antibody specifically and effectively inhibits infection and cytokine storm of SARS-CoV-2 and its variants delta, alpha, beta, and gamma, Signal Transduct. Target. Ther, doi:10.1038/s41392-021-00760-8
Geng, Zhang, Chen, Miao, Yao et al., Enhancement of CD147 on M1 macrophages induces differentiation of Th17 cells in the lung interstitial fibrosis, Biochim. Biophys. Acta-Mol. Basis Dis, doi:10.1016/j.bbadis.2014.06.008
George, Wells, Jenkins, Pulmonary fibrosis and COVID-19: The potential role for antifibrotic therapy, Lancet Respir. Med, doi:10.1016/S2213-2600(20)30225-3
Gevers, Welink, Van Nieuwkoop, Remdesivir in COVID-19 Patients with Impaired Renal Function, J. Am. Soc. Nephrol, doi:10.1681/ASN.2020101535
Grubaugh, Cobey, Of variants and vaccines, Cell, doi:10.1016/j.cell.2021.11.013
Gyamfi, Lee, Min, Choi, Niclosamide reverses adipocyte induced epithelial-mesenchymal transition in breast cancer cells via suppression of the interleukin-6/STAT3 signalling axis, Sci. Rep, doi:10.1038/s41598-019-47707-2
Hao, Ning, Kuz, Vorhies, Yan et al., Long-Term Modeling of SARS-CoV-2 Infection of In Vitro Cultured Polarized Human Airway Epithelium, mBio, doi:10.1128/mBio.02852-20
Hinman, Lou, Diverse molecular functions of Hu proteins, Cell. Mol. Life Sci, doi:10.1007/s00018-008-8252-6
Hoffmann, Kleine-Weber, Schroeder, Krüger, Herrler et al., SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor, Cell, doi:10.1016/j.cell.2020.02.052
Hu, Fu, Li, Yang, Cao et al., Chemical mitochondrial uncouplers share common inhibitory effect on NLRP3 inflammasome activation through inhibiting NFκB nuclear translocation, Toxicol. Appl. Pharmacol, doi:10.1016/j.taap.2021.115426
Jeon, Ko, Lee, Choi, Byun et al., Identification of Antiviral Drug Candidates against SARS-CoV-2 from FDA-Approved Drugs, Antimicrob. Agents Chemother, doi:10.1128/AAC.00819-20
Kabinger, Stiller, Schmitzová, Dienemann, Kokic et al., Mechanism of molnupiravir-induced SARS-CoV-2 mutagenesis, Nat. Struct. Mol. Biol, doi:10.1038/s41594-021-00651-0
Kalejaiye, Bhattacharya, Burt, Travieso, Okafor et al., SARS-CoV-2 Employ BSG/CD147 and ACE2 Receptors to Directly Infect Human Induced Pluripotent Stem Cell-Derived Kidney Podocytes, Front. Cell Dev. Biol, doi:10.3389/fcell.2022.855340
Katsanou, Papadaki, Milatos, Blackshear, Anderson et al., HuR as a negative posttranscriptional modulator in inflammation, Mol. Cell, doi:10.1016/j.molcel.2005.08.007
Kong, Liao, Zhang, Xu, Li et al., A Regulatory Loop Involving miR-22, Sp1, and c-Myc Modulates CD147 Expression in Breast Cancer Invasion and Metastasis, Cancer Res, doi:10.1158/0008-5472.CAN-13-3555
Kumar, Rodrigues, Buko, Denissen, Cytochrome P450-mediated metabolism of the HIV-1 protease inhibitor ritonavir (ABT-538) in human liver microsomes, J. Pharmacol. Exp. Ther
Kunzelmann, Ousingsawat, Cabrita, Doušová, Bähr et al., TMEM16A in Cystic Fibrosis: Activating or Inhibiting? Front, Pharmacol, doi:10.3389/fphar.2019.00003
Li, Liu, Zhou, Qu, Yang et al., 2.0: Decoding miRNA-ceRNA, miRNA-ncRNA and protein-RNA interaction networks from large-scale CLIP-Seq data, Nucleic Acids Res, doi:10.1093/nar/gkt1248
Li, Tang, Wu, Karnak, Meng et al., HAb18G/CD147 Promotes pSTAT3-Mediated Pancreatic Cancer Development via CD44s, Clin. Cancer Res, doi:10.1158/1078-0432.CCR-13-0621
Lu, Wu, Hao, Shang, Xu et al., Basolateral CD147 induces hepatocyte polarity loss by E-cadherin ubiquitination and degradation in hepatocellular carcinoma progress, Hepatology, doi:10.1002/hep.29798
Marzi, Vakil, Bahmanyar, Zarenezhad, Paxlovid, Mechanism of Action, Synthesis, and In Silico Study, BioMed Res. Int, doi:10.1155/2022/7341493
Maugeri, De Lorenzo, Clementi, Antonia Diotti, Criscuolo et al., Unconventional CD147-dependent platelet activation elicited by SARS-CoV-2 in COVID-19, J. Thromb. Haemost, doi:10.1111/jth.15575
Mcclain, Constantine, Henao, Liu, Tsalik et al., Dysregulated transcriptional responses to SARS-CoV-2 in the periphery, Nat. Commun, doi:10.1038/s41467-021-21289-y
Miner, Labitzke, Liu, Wang, Henckels et al., Drug Repurposing: The Anthelmintics Niclosamide and Nitazoxanide Are Potent TMEM16A Antagonists That Fully Bronchodilate Airways, Front. Pharmacol, doi:10.3389/fphar.2019.00051
Pushkarsky, Zybarth, Dubrovsky, Yurchenko, Tang et al., CD147 facilitates HIV-1 infection by interacting with virus-associated cyclophilin A, Proc. Natl. Acad. Sci, doi:10.1073/pnas.111583198
Sanda, Morrison, Goldman, N-and O-Glycosylation of the SARS-CoV-2 Spike Protein, Anal. Chem, doi:10.1021/acs.analchem.0c03173
Santi Laurini, Montanaro, Motola, Safety Profile of Molnupiravir in the Treatment of COVID-19: A Descriptive Study Based on FAERS Data, J. Clin. Med, doi:10.3390/jcm12010034
Shajahan, Supekar, Gleinich, Azadi, Deducing the N-and O-glycosylation profile of the spike protein of novel coronavirus SARS-CoV-2, Glycobiology, doi:10.1093/glycob/cwaa042
Shang, Zhao, Emerging role of HuR in inflammatory response in kidney diseases, Acta Biochim. Et Biophys. Sin, doi:10.1093/abbs/gmx071
Shi, Ju, Li, Yuan, Cui et al., CD147 Promotes CXCL1 Expression and Modulates Liver Fibrogenesis, Int. J. Mol. Sci, doi:10.3390/ijms19041145
Shilts, Crozier, Greenwood, Lehner, Wright, No evidence for basigin/CD147 as a direct SARS-CoV-2 spike binding receptor, Sci. Rep, doi:10.1038/s41598-020-80464-1
Shukri, Wang, Chia, Nawi, The SARS-CoV-2 Variants and their Impacts, J. Pure Appl. Microbiol, doi:10.22207/JPAM.16.3.45
Spagnolo, Balestro, Aliberti, Cocconcelli, Biondini et al., Pulmonary fibrosis secondary to COVID-19: A call to arms?, Lancet Respir. Med, doi:10.1016/S2213-2600(20)30222-8
Stewart, Carpenter, West, Knifley, Liu et al., S100A4 drives non-small cell lung cancer invasion, associates with poor prognosis, and is effectively targeted by the FDA-approved anti-helminthic agent niclosamide, Oncotarget, doi:10.18632/oncotarget.8969
Tang, Chang, Hemler, Links between CD147 Function, Glycosylation, and Caveolin-1, Mol. Biol. Cell, doi:10.1091/mbc.e04-05-0402
Thorne, Bouhaddou, Reuschl, Zuliani-Alvarez, Polacco et al., Evolution of enhanced innate immune evasion by SARS-CoV-2, Nature, doi:10.1038/s41586-021-04352-y
Trivlidis, Aloufi, Al-Habeeb, Nair, Azuelos et al., HuR drives lung fibroblast differentiation but not metabolic reprogramming in response to TGF-beta and hypoxia, Respir. Res, doi:10.1186/s12931-021-01916-4
Trugilho, Azevedo-Quintanilha, Gesto, Moraes, Mandacaru et al., Platelet proteome reveals features of cell death, antiviral response and viral replication in COVID-19, Cell Death Discov, doi:10.1038/s41420-022-01122-1
Ulrich, Pillat, CD147 as a Target for COVID-19 Treatment: Suggested Effects of Azithromycin and Stem Cell Engagement, Stem Cell Rev. Rep, doi:10.1007/s12015-020-09976-7
Volle, Murer, Petkidis, Andriasyan, Savi et al., Methylene blue, Mycophenolic acid, Posaconazole, and Niclosamide inhibit SARS-CoV-2 Omicron variant BA.1 infection of human airway epithelial organoids, Curr. Res. Microb. Sci, doi:10.1016/j.crmicr.2022.100158
Wang, Chen, Zhang, Deng, Lian et al., CD147-spike protein is a novel route for SARS-CoV-2 infection to host cells, Signal Transduct. Target. Ther, doi:10.1038/s41392-020-00426-x
Weiss, Touret, Baronti, Gilles, Hoen et al., Niclosamide shows strong antiviral activity in a human airway model of SARS-CoV-2 infection and a conserved potency against the Alpha (B.1.1.7), Beta (B.1.351) and Delta variant (B.1.617, PLoS ONE, doi:10.1371/journal.pone.0260958
Who, WHO COVID-19 Dashboard
Woodhoo, Iruarrizaga-Lejarreta, Beraza, Garcia-Rodriguez, Embade et al., Human antigen R contributes to hepatic stellate cell activation and liver fibrosis, Hepatology, doi:10.1002/hep.25828
Wu, Chen, Qin, Huo, Liang et al., CD147 contributes to SARS-CoV-2induced pulmonary fibrosis, Signal Transduct. Target. Ther, doi:10.1038/s41392-022-01230-5
Wu, Gardashova, Lan, Han, Zhong et al., Targeting the interaction between RNA-binding protein HuR and FOXQ1 suppresses breast cancer invasion and metastasis, Commun. Biol, doi:10.1038/s42003-020-0933-1
Wu, Jan, Chen, Hsieh, Hwang et al., Inhibition of Severe Acute Respiratory Syndrome Coronavirus Replication by Niclosamide, Antimicrob. Agents Chemother, doi:10.1128/AAC.48.7.2693-2696.2004
Xie, Xu, Bowe, Al-Aly, Long-term cardiovascular outcomes of COVID-19, Nat. Med
Xu, Shi, Wang, Zhang, Huang et al., Pathological findings of COVID-19 associated with acute respiratory distress syndrome, Lancet Respir. Med, doi:10.1016/S2213-2600(20)30076-X
Yan, Qu, Zhang, Huang, Qu et al., CD147 promotes liver fibrosis progression via VEGF-A/VEGFR2 signalling-mediated cross-talk between hepatocytes and sinusoidal endothelial cells, Clin. Sci, doi:10.1042/CS20140823
Zhong, Zhao, Zhao, Gu, Lu et al., The Role of CD147 in Pathological Cardiac Hypertrophy Is Regulated by Glycosylation, Oxid. Med. Cell. Longev, doi:10.1155/2022/6603296
Zhou, Wang, Wang, Cui, Zhao et al., SARS-CoV-2 pseudovirus enters the host cells through spike protein-CD147 in an Arf6-dependent manner, Emerg. Microbes Infect, doi:10.1080/22221751.2022.2059403
Zou, Xiong, Hao, Zhang, Baumlin et al., The SARS-CoV-2 Transcriptome and the Dynamics of the S Gene Furin Cleavage Site in Primary Human Airway Epithelia, mBio, doi:10.1128/mBio.01006-21
DOI record:
{
"DOI": "10.3390/biomedicines11072019",
"ISSN": [
"2227-9059"
],
"URL": "http://dx.doi.org/10.3390/biomedicines11072019",
"abstract": "<jats:p>The outbreak of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has led to the global coronavirus disease 2019 (COVID-19) pandemic, and the search for effective treatments has been limited. Furthermore, the rapid mutations of SARS-CoV-2 have posed challenges to existing vaccines and neutralizing antibodies, as they struggle to keep up with the increased viral transmissibility and immune evasion. However, there is hope in targeting the CD147-spike protein, which serves as an alternative point for the entry of SARS-CoV-2 into host cells. This protein has emerged as a promising therapeutic target for the development of drugs against COVID-19. Here, we demonstrate that the RNA-binding protein Human-antigen R (HuR) plays a crucial role in the post-transcriptional regulation of CD147 by directly binding to its 3′-untranslated region (UTR). We observed a decrease in CD147 levels across multiple cell lines upon HuR depletion. Furthermore, we identified that niclosamide can reduce CD147 by lowering the cytoplasmic translocation of HuR and reducing CD147 glycosylation. Moreover, our investigation revealed that SARS-CoV-2 infection induces an upregulation of CD147 in ACE2-expressing A549 cells, which can be effectively neutralized by niclosamide in a dose-dependent manner. Overall, our study unveils a novel regulatory mechanism of regulating CD147 through HuR and suggests niclosamide as a promising therapeutic option against COVID-19.</jats:p>",
"alternative-id": [
"biomedicines11072019"
],
"author": [
{
"ORCID": "http://orcid.org/0000-0003-3232-0626",
"affiliation": [
{
"name": "Department of Molecular Biosciences, The University of Kansas, Lawrence, KS 66045, USA"
}
],
"authenticated-orcid": false,
"family": "Yang",
"given": "Zhe",
"sequence": "first"
},
{
"affiliation": [
{
"name": "Higuchi Biosciences Center, The University of Kansas, Lawrence, KS 66045, USA"
}
],
"family": "Zhang",
"given": "Qi",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Higuchi Biosciences Center, The University of Kansas, Lawrence, KS 66045, USA"
},
{
"name": "The University of Kansas Cancer Center, The University of Kansas Medical Center, Kansas City, KS 66160, USA"
}
],
"family": "Wu",
"given": "Xiaoqing",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Microbiology, Molecular Genetics and Immunology, The University of Kansas Medical Center, Kansas City, KS 66160, USA"
}
],
"family": "Hao",
"given": "Siyuan",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Molecular Biosciences, The University of Kansas, Lawrence, KS 66045, USA"
}
],
"family": "Hao",
"given": "Xinbao",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Pharmacology, Toxicology & Therapeutics, The University of Kansas Medical Center, Kansas City, KS 66160, USA"
}
],
"family": "Jones",
"given": "Elizabeth",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-9951-3583",
"affiliation": [
{
"name": "Department of Pharmacology, Toxicology & Therapeutics, The University of Kansas Medical Center, Kansas City, KS 66160, USA"
}
],
"authenticated-orcid": false,
"family": "Zhang",
"given": "Yuxia",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-9850-1695",
"affiliation": [
{
"name": "Department of Microbiology, Molecular Genetics and Immunology, The University of Kansas Medical Center, Kansas City, KS 66160, USA"
}
],
"authenticated-orcid": false,
"family": "Qiu",
"given": "Jianming",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-9196-4232",
"affiliation": [
{
"name": "Department of Molecular Biosciences, The University of Kansas, Lawrence, KS 66045, USA"
},
{
"name": "The University of Kansas Cancer Center, The University of Kansas Medical Center, Kansas City, KS 66160, USA"
},
{
"name": "Department of Radiation Oncology, The University of Kansas Medical Center, Kansas City, KS 66160, USA"
}
],
"authenticated-orcid": false,
"family": "Xu",
"given": "Liang",
"sequence": "additional"
}
],
"container-title": "Biomedicines",
"container-title-short": "Biomedicines",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2023,
7,
19
]
],
"date-time": "2023-07-19T04:54:01Z",
"timestamp": 1689742441000
},
"deposited": {
"date-parts": [
[
2023,
7,
19
]
],
"date-time": "2023-07-19T07:28:31Z",
"timestamp": 1689751711000
},
"funder": [
{
"DOI": "10.13039/100000002",
"award": [
"R01CA243445",
"R33CA252158"
],
"doi-asserted-by": "publisher",
"id": [
{
"asserted-by": "publisher",
"id": "10.13039/100000002",
"id-type": "DOI"
}
],
"name": "National Institutes of Health"
},
{
"award": [
"W81XWH2110573"
],
"name": "Midwest Biomedical Accelerator Consortium"
},
{
"award": [
"USAWA1/2020",
"NR-52281"
],
"name": "Centers for Disease Control and Prevention"
}
],
"indexed": {
"date-parts": [
[
2023,
11,
19
]
],
"date-time": "2023-11-19T12:19:24Z",
"timestamp": 1700396364115
},
"is-referenced-by-count": 1,
"issue": "7",
"issued": {
"date-parts": [
[
2023,
7,
18
]
]
},
"journal-issue": {
"issue": "7",
"published-online": {
"date-parts": [
[
2023,
7
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
7,
18
]
],
"date-time": "2023-07-18T00:00:00Z",
"timestamp": 1689638400000
}
}
],
"link": [
{
"URL": "https://www.mdpi.com/2227-9059/11/7/2019/pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1968",
"original-title": [],
"page": "2019",
"prefix": "10.3390",
"published": {
"date-parts": [
[
2023,
7,
18
]
]
},
"published-online": {
"date-parts": [
[
2023,
7,
18
]
]
},
"publisher": "MDPI AG",
"reference": [
{
"key": "ref_1",
"unstructured": "WHO (2020). WHO COVID-19 Dashboard, World Health Organization. Available online: https://covid19.who.int/."
},
{
"DOI": "10.1016/j.cell.2021.11.013",
"article-title": "Of variants and vaccines",
"author": "Grubaugh",
"doi-asserted-by": "crossref",
"first-page": "6222",
"journal-title": "Cell",
"key": "ref_2",
"volume": "184",
"year": "2021"
},
{
"DOI": "10.22207/JPAM.16.3.45",
"article-title": "The SARS-CoV-2 Variants and their Impacts",
"author": "Shukri",
"doi-asserted-by": "crossref",
"first-page": "1409",
"journal-title": "J. Pure Appl. Microbiol.",
"key": "ref_3",
"volume": "16",
"year": "2022"
},
{
"DOI": "10.1155/2022/7341493",
"article-title": "Paxlovid: Mechanism of Action, Synthesis, and In Silico Study",
"author": "Marzi",
"doi-asserted-by": "crossref",
"first-page": "7341493",
"journal-title": "BioMed Res. Int.",
"key": "ref_4",
"volume": "2022",
"year": "2022"
},
{
"article-title": "Cytochrome P450-mediated metabolism of the HIV-1 protease inhibitor ritonavir (ABT-538) in human liver microsomes",
"author": "Kumar",
"first-page": "423",
"journal-title": "J. Pharmacol. Exp. Ther.",
"key": "ref_5",
"volume": "277",
"year": "1996"
},
{
"DOI": "10.1056/NEJMoa2007764",
"article-title": "Remdesivir for the Treatment of COVID-19-Final Report",
"author": "Beigel",
"doi-asserted-by": "crossref",
"first-page": "1813",
"journal-title": "N. Engl. J. Med.",
"key": "ref_6",
"volume": "383",
"year": "2020"
},
{
"DOI": "10.1038/s41594-021-00651-0",
"article-title": "Mechanism of molnupiravir-induced SARS-CoV-2 mutagenesis",
"author": "Kabinger",
"doi-asserted-by": "crossref",
"first-page": "740",
"journal-title": "Nat. Struct. Mol. Biol.",
"key": "ref_7",
"volume": "28",
"year": "2021"
},
{
"DOI": "10.1681/ASN.2020050589",
"article-title": "Remdesivir in Patients with Acute or Chronic Kidney Disease and COVID-19",
"author": "Adamsick",
"doi-asserted-by": "crossref",
"first-page": "1384",
"journal-title": "J. Am. Soc. Nephrol.",
"key": "ref_8",
"volume": "31",
"year": "2020"
},
{
"DOI": "10.1681/ASN.2020101535",
"article-title": "Remdesivir in COVID-19 Patients with Impaired Renal Function",
"author": "Gevers",
"doi-asserted-by": "crossref",
"first-page": "518",
"journal-title": "J. Am. Soc. Nephrol.",
"key": "ref_9",
"volume": "32",
"year": "2021"
},
{
"DOI": "10.3390/jcm12010034",
"doi-asserted-by": "crossref",
"key": "ref_10",
"unstructured": "Santi Laurini, G., Montanaro, N., and Motola, D. (2023). Safety Profile of Molnupiravir in the Treatment of COVID-19: A Descriptive Study Based on FAERS Data. J. Clin. Med., 12."
},
{
"key": "ref_11",
"unstructured": "Centers for Disease Control and Prevention (CDC) (2023, June 11). Updated Healthcare Infection Prevention and Control Recommendations in Response to COVID-19 Vaccination, Available online: https://www.cdc.gov/."
},
{
"DOI": "10.1038/s41392-020-00426-x",
"article-title": "CD147-spike protein is a novel route for SARS-CoV-2 infection to host cells",
"author": "Wang",
"doi-asserted-by": "crossref",
"first-page": "283",
"journal-title": "Signal Transduct. Target. Ther.",
"key": "ref_12",
"volume": "5",
"year": "2020"
},
{
"DOI": "10.1016/j.cell.2020.02.052",
"article-title": "SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor",
"author": "Hoffmann",
"doi-asserted-by": "crossref",
"first-page": "271",
"journal-title": "Cell",
"key": "ref_13",
"volume": "181",
"year": "2020"
},
{
"DOI": "10.1080/22221751.2022.2059403",
"article-title": "SARS-CoV-2 pseudovirus enters the host cells through spike protein-CD147 in an Arf6-dependent manner",
"author": "Zhou",
"doi-asserted-by": "crossref",
"first-page": "1135",
"journal-title": "Emerg. Microbes Infect.",
"key": "ref_14",
"volume": "11",
"year": "2022"
},
{
"DOI": "10.1158/0008-5472.CAN-13-3555",
"article-title": "A Regulatory Loop Involving miR-22, Sp1, and c-Myc Modulates CD147 Expression in Breast Cancer Invasion and Metastasis",
"author": "Kong",
"doi-asserted-by": "crossref",
"first-page": "3764",
"journal-title": "Cancer Res.",
"key": "ref_15",
"volume": "74",
"year": "2014"
},
{
"DOI": "10.1002/hep.29798",
"article-title": "Basolateral CD147 induces hepatocyte polarity loss by E-cadherin ubiquitination and degradation in hepatocellular carcinoma progress",
"author": "Lu",
"doi-asserted-by": "crossref",
"first-page": "317",
"journal-title": "Hepatology",
"key": "ref_16",
"volume": "68",
"year": "2018"
},
{
"DOI": "10.1158/1078-0432.CCR-13-0621",
"article-title": "HAb18G/CD147 Promotes pSTAT3-Mediated Pancreatic Cancer Development via CD44s",
"author": "Li",
"doi-asserted-by": "crossref",
"first-page": "6703",
"journal-title": "Clin. Cancer Res.",
"key": "ref_17",
"volume": "19",
"year": "2013"
},
{
"DOI": "10.1073/pnas.111583198",
"article-title": "CD147 facilitates HIV-1 infection by interacting with virus-associated cyclophilin A",
"author": "Pushkarsky",
"doi-asserted-by": "crossref",
"first-page": "6360",
"journal-title": "Proc. Natl. Acad. Sci. USA",
"key": "ref_18",
"volume": "98",
"year": "2001"
},
{
"DOI": "10.1186/s13578-022-00822-6",
"article-title": "Development of a novel human CD147 knock-in NSG mouse model to test SARS-CoV-2 viral infection",
"author": "Badeti",
"doi-asserted-by": "crossref",
"first-page": "88",
"journal-title": "Cell Biosci.",
"key": "ref_19",
"volume": "12",
"year": "2022"
},
{
"DOI": "10.3389/fcell.2022.855340",
"article-title": "SARS-CoV-2 Employ BSG/CD147 and ACE2 Receptors to Directly Infect Human Induced Pluripotent Stem Cell-Derived Kidney Podocytes",
"author": "Kalejaiye",
"doi-asserted-by": "crossref",
"first-page": "855340",
"journal-title": "Front. Cell Dev. Biol.",
"key": "ref_20",
"volume": "10",
"year": "2022"
},
{
"DOI": "10.1038/s41420-022-01122-1",
"article-title": "Platelet proteome reveals features of cell death, antiviral response and viral replication in COVID-19",
"author": "Trugilho",
"doi-asserted-by": "crossref",
"first-page": "324",
"journal-title": "Cell Death Discov.",
"key": "ref_21",
"volume": "8",
"year": "2022"
},
{
"DOI": "10.1111/jth.15534",
"article-title": "Platelets contribute to disease severity in COVID-19",
"author": "Barrett",
"doi-asserted-by": "crossref",
"first-page": "3139",
"journal-title": "J. Thromb. Haemost.",
"key": "ref_22",
"volume": "19",
"year": "2021"
},
{
"DOI": "10.1111/jth.15575",
"article-title": "Unconventional CD147-dependent platelet activation elicited by SARS-CoV-2 in COVID-19",
"author": "Maugeri",
"doi-asserted-by": "crossref",
"first-page": "434",
"journal-title": "J. Thromb. Haemost.",
"key": "ref_23",
"volume": "20",
"year": "2021"
},
{
"DOI": "10.1042/CS20210735",
"article-title": "The SARS-CoV-2 Spike protein disrupts human cardiac pericytes function through CD147 receptor-mediated signalling: A potential non-infective mechanism of COVID-19 microvascular disease",
"author": "Avolio",
"doi-asserted-by": "crossref",
"first-page": "2667",
"journal-title": "Clin. Sci.",
"key": "ref_24",
"volume": "135",
"year": "2021"
},
{
"DOI": "10.1038/s41392-022-01230-5",
"article-title": "CD147 contributes to SARS-CoV-2-induced pulmonary fibrosis",
"author": "Wu",
"doi-asserted-by": "crossref",
"first-page": "382",
"journal-title": "Signal Transduct. Target. Ther.",
"key": "ref_25",
"volume": "7",
"year": "2022"
},
{
"DOI": "10.1038/s41392-021-00603-6",
"article-title": "Safety and efficacy of meplazumab in healthy volunteers and COVID-19 patients: A randomized phase 1 and an exploratory phase 2 trial",
"author": "Bian",
"doi-asserted-by": "crossref",
"first-page": "194",
"journal-title": "Signal Transduct. Target. Ther.",
"key": "ref_26",
"volume": "6",
"year": "2021"
},
{
"DOI": "10.1038/s41392-021-00760-8",
"article-title": "CD147 antibody specifically and effectively inhibits infection and cytokine storm of SARS-CoV-2 and its variants delta, alpha, beta, and gamma",
"author": "Geng",
"doi-asserted-by": "crossref",
"first-page": "347",
"journal-title": "Signal Transduct. Target. Ther.",
"key": "ref_27",
"volume": "6",
"year": "2021"
},
{
"DOI": "10.1128/AAC.48.7.2693-2696.2004",
"article-title": "Inhibition of Severe Acute Respiratory Syndrome Coronavirus Replication by Niclosamide",
"author": "Wu",
"doi-asserted-by": "crossref",
"first-page": "2693",
"journal-title": "Antimicrob. Agents Chemother.",
"key": "ref_28",
"volume": "48",
"year": "2004"
},
{
"DOI": "10.1038/s41467-019-13659-4",
"article-title": "SKP2 attenuates autophagy through Beclin1-ubiquitination and its inhibition reduces MERS-Coronavirus infection",
"author": "Gassen",
"doi-asserted-by": "crossref",
"first-page": "5770",
"journal-title": "Nat. Commun.",
"key": "ref_29",
"volume": "10",
"year": "2019"
},
{
"DOI": "10.1128/AAC.00819-20",
"article-title": "Identification of Antiviral Drug Candidates against SARS-CoV-2 from FDA-Approved Drugs",
"author": "Jeon",
"doi-asserted-by": "crossref",
"first-page": "e00819-20",
"journal-title": "Antimicrob. Agents Chemother.",
"key": "ref_30",
"volume": "64",
"year": "2020"
},
{
"article-title": "Methylene blue, Mycophenolic acid, Posaconazole, and Niclosamide inhibit SARS-CoV-2 Omicron variant BA.1 infection of human airway epithelial organoids",
"author": "Volle",
"first-page": "100158",
"journal-title": "Curr. Res. Microb. Sci.",
"key": "ref_31",
"volume": "3",
"year": "2022"
},
{
"DOI": "10.1371/journal.pone.0260958",
"doi-asserted-by": "crossref",
"key": "ref_32",
"unstructured": "Weiss, A., Touret, F., Baronti, C., Gilles, M., Hoen, B., Nougairède, A., de Lamballerie, X., and Sommer, M.O.A. (2021). Niclosamide shows strong antiviral activity in a human airway model of SARS-CoV-2 infection and a conserved potency against the Alpha (B.1.1.7), Beta (B.1.351) and Delta variant (B.1.617.2). PLoS ONE, 16."
},
{
"DOI": "10.1038/s41598-019-47707-2",
"article-title": "Niclosamide reverses adipocyte induced epithelial-mesenchymal transition in breast cancer cells via suppression of the interleukin-6/STAT3 signalling axis",
"author": "Gyamfi",
"doi-asserted-by": "crossref",
"first-page": "11336",
"journal-title": "Sci. Rep.",
"key": "ref_33",
"volume": "9",
"year": "2019"
},
{
"DOI": "10.18632/oncotarget.8969",
"article-title": "S100A4 drives non-small cell lung cancer invasion, associates with poor prognosis, and is effectively targeted by the FDA-approved anti-helminthic agent niclosamide",
"author": "Stewart",
"doi-asserted-by": "crossref",
"first-page": "34630",
"journal-title": "Oncotarget",
"key": "ref_34",
"volume": "7",
"year": "2016"
},
{
"DOI": "10.1038/s41586-021-03491-6",
"article-title": "Drugs that inhibit TMEM16 proteins block SARS-CoV-2 spike-induced syncytia",
"author": "Braga",
"doi-asserted-by": "crossref",
"first-page": "88",
"journal-title": "Nature",
"key": "ref_35",
"volume": "594",
"year": "2021"
},
{
"DOI": "10.3389/fphar.2019.00051",
"article-title": "Drug Repurposing: The Anthelmintics Niclosamide and Nitazoxanide Are Potent TMEM16A Antagonists That Fully Bronchodilate Airways",
"author": "Miner",
"doi-asserted-by": "crossref",
"first-page": "51",
"journal-title": "Front. Pharmacol.",
"key": "ref_36",
"volume": "10",
"year": "2019"
},
{
"DOI": "10.18632/oncotarget.26421",
"article-title": "Bioenergetic modulation with the mitochondria uncouplers SR4 and niclosamide prevents proliferation and growth of treatment-naïve and vemurafenib-resistant melanomas",
"author": "Figarola",
"doi-asserted-by": "crossref",
"first-page": "36945",
"journal-title": "Oncotarget",
"key": "ref_37",
"volume": "9",
"year": "2018"
},
{
"DOI": "10.1126/sciadv.abo5400",
"article-title": "Identification of immunomodulatory drugs that inhibit multiple inflammasomes and impair SARS-CoV-2 infection",
"author": "Rodrigues",
"doi-asserted-by": "crossref",
"first-page": "eabo5400",
"journal-title": "Sci. Adv.",
"key": "ref_38",
"volume": "8",
"year": "2022"
},
{
"DOI": "10.1016/j.kint.2017.01.018",
"article-title": "The antihelmenthic phosphate niclosamide impedes renal fibrosis by inhibiting homeodomain-interacting protein kinase 2 expression",
"author": "Chang",
"doi-asserted-by": "crossref",
"first-page": "612",
"journal-title": "Kidney Int.",
"key": "ref_39",
"volume": "92",
"year": "2017"
},
{
"DOI": "10.1016/j.lfs.2018.12.061",
"article-title": "Niclosamide alleviates pulmonary fibrosis in vitro and in vivo by attenuation of epithelial-to-mesenchymal transition, matrix proteins & Wnt/β-catenin signaling: A drug repurposing study",
"author": "Boyapally",
"doi-asserted-by": "crossref",
"first-page": "8",
"journal-title": "Life Sci.",
"key": "ref_40",
"volume": "220",
"year": "2019"
},
{
"DOI": "10.3389/fphar.2019.00003",
"article-title": "TMEM16A in Cystic Fibrosis: Activating or Inhibiting?",
"author": "Kunzelmann",
"doi-asserted-by": "crossref",
"first-page": "3",
"journal-title": "Front. Pharmacol.",
"key": "ref_41",
"volume": "10",
"year": "2019"
},
{
"DOI": "10.1016/S2213-2600(20)30222-8",
"article-title": "Pulmonary fibrosis secondary to COVID-19: A call to arms?",
"author": "Spagnolo",
"doi-asserted-by": "crossref",
"first-page": "750",
"journal-title": "Lancet Respir. Med.",
"key": "ref_42",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1016/S2213-2600(20)30076-X",
"article-title": "Pathological findings of COVID-19 associated with acute respiratory distress syndrome",
"author": "Xu",
"doi-asserted-by": "crossref",
"first-page": "420",
"journal-title": "Lancet Respir. Med.",
"key": "ref_43",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1016/S2213-2600(20)30225-3",
"article-title": "Pulmonary fibrosis and COVID-19: The potential role for antifibrotic therapy",
"author": "George",
"doi-asserted-by": "crossref",
"first-page": "807",
"journal-title": "Lancet Respir. Med.",
"key": "ref_44",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1007/s12015-020-09976-7",
"article-title": "CD147 as a Target for COVID-19 Treatment: Suggested Effects of Azithromycin and Stem Cell Engagement",
"author": "Ulrich",
"doi-asserted-by": "crossref",
"first-page": "434",
"journal-title": "Stem Cell Rev. Rep.",
"key": "ref_45",
"volume": "16",
"year": "2020"
},
{
"DOI": "10.1002/adtp.202100087",
"article-title": "Discovery of Small Anti-ACE2 Peptides to Inhibit SARS-CoV-2 Infectivity",
"author": "Adhikary",
"doi-asserted-by": "crossref",
"first-page": "2100087",
"journal-title": "Adv. Ther.",
"key": "ref_46",
"volume": "4",
"year": "2021"
},
{
"DOI": "10.1128/mBio.02852-20",
"article-title": "Long-Term Modeling of SARS-CoV-2 Infection of In Vitro Cultured Polarized Human Airway Epithelium",
"author": "Hao",
"doi-asserted-by": "crossref",
"first-page": "6",
"journal-title": "mBio",
"key": "ref_47",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.1128/mBio.01006-21",
"article-title": "The SARS-CoV-2 Transcriptome and the Dynamics of the S Gene Furin Cleavage Site in Primary Human Airway Epithelia",
"author": "Zou",
"doi-asserted-by": "crossref",
"first-page": "3",
"journal-title": "mBio",
"key": "ref_48",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.1038/s41467-021-21289-y",
"article-title": "Dysregulated transcriptional responses to SARS-CoV-2 in the periphery",
"author": "McClain",
"doi-asserted-by": "crossref",
"first-page": "1079",
"journal-title": "Nat. Commun.",
"key": "ref_49",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.1093/nar/gkt1248",
"article-title": "StarBase v2.0: Decoding miRNA-ceRNA, miRNA-ncRNA and protein–RNA interaction networks from large-scale CLIP-Seq data",
"author": "Li",
"doi-asserted-by": "crossref",
"first-page": "D92",
"journal-title": "Nucleic Acids Res.",
"key": "ref_50",
"volume": "42",
"year": "2013"
},
{
"DOI": "10.1016/j.molcel.2005.08.007",
"article-title": "HuR as a negative posttranscriptional modulator in inflammation",
"author": "Katsanou",
"doi-asserted-by": "crossref",
"first-page": "777",
"journal-title": "Mol. Cell",
"key": "ref_51",
"volume": "19",
"year": "2005"
},
{
"DOI": "10.1186/s12931-021-01916-4",
"article-title": "HuR drives lung fibroblast differentiation but not metabolic reprogramming in response to TGF-beta and hypoxia",
"author": "Trivlidis",
"doi-asserted-by": "crossref",
"first-page": "323",
"journal-title": "Respir. Res.",
"key": "ref_52",
"volume": "22",
"year": "2021"
},
{
"DOI": "10.1002/hep.25828",
"article-title": "Human antigen R contributes to hepatic stellate cell activation and liver fibrosis",
"author": "Woodhoo",
"doi-asserted-by": "crossref",
"first-page": "1870",
"journal-title": "Hepatology",
"key": "ref_53",
"volume": "56",
"year": "2012"
},
{
"DOI": "10.1093/abbs/gmx071",
"article-title": "Emerging role of HuR in inflammatory response in kidney diseases",
"author": "Shang",
"doi-asserted-by": "crossref",
"first-page": "753",
"journal-title": "Acta Biochim. Et Biophys. Sin.",
"key": "ref_54",
"volume": "49",
"year": "2017"
},
{
"DOI": "10.1038/s42003-020-0933-1",
"article-title": "Targeting the interaction between RNA-binding protein HuR and FOXQ1 suppresses breast cancer invasion and metastasis",
"author": "Wu",
"doi-asserted-by": "crossref",
"first-page": "193",
"journal-title": "Commun. Biol.",
"key": "ref_55",
"volume": "3",
"year": "2020"
},
{
"DOI": "10.1007/s00018-008-8252-6",
"article-title": "Diverse molecular functions of Hu proteins",
"author": "Hinman",
"doi-asserted-by": "crossref",
"first-page": "3168",
"journal-title": "Cell. Mol. Life Sci.",
"key": "ref_56",
"volume": "65",
"year": "2008"
},
{
"DOI": "10.1016/j.taap.2021.115426",
"article-title": "Chemical mitochondrial uncouplers share common inhibitory effect on NLRP3 inflammasome activation through inhibiting NFκB nuclear translocation",
"author": "Hu",
"doi-asserted-by": "crossref",
"first-page": "115426",
"journal-title": "Toxicol. Appl. Pharmacol.",
"key": "ref_57",
"volume": "414",
"year": "2021"
},
{
"DOI": "10.1091/mbc.e04-05-0402",
"article-title": "Links between CD147 Function, Glycosylation, and Caveolin-1",
"author": "Tang",
"doi-asserted-by": "crossref",
"first-page": "4043",
"journal-title": "Mol. Biol. Cell",
"key": "ref_58",
"volume": "15",
"year": "2004"
},
{
"DOI": "10.1155/2022/6603296",
"article-title": "The Role of CD147 in Pathological Cardiac Hypertrophy Is Regulated by Glycosylation",
"author": "Zhong",
"doi-asserted-by": "crossref",
"first-page": "6603296",
"journal-title": "Oxid. Med. Cell. Longev.",
"key": "ref_59",
"volume": "2022",
"year": "2022"
},
{
"DOI": "10.1038/s41598-020-80464-1",
"article-title": "No evidence for basigin/CD147 as a direct SARS-CoV-2 spike binding receptor",
"author": "Shilts",
"doi-asserted-by": "crossref",
"first-page": "413",
"journal-title": "Sci. Rep.",
"key": "ref_60",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.1016/j.bbadis.2014.06.008",
"article-title": "Enhancement of CD147 on M1 macrophages induces differentiation of Th17 cells in the lung interstitial fibrosis",
"author": "Geng",
"doi-asserted-by": "crossref",
"first-page": "1770",
"journal-title": "Biochim. Biophys. Acta-Mol. Basis Dis.",
"key": "ref_61",
"volume": "1842",
"year": "2014"
},
{
"DOI": "10.3390/ijms19041145",
"doi-asserted-by": "crossref",
"key": "ref_62",
"unstructured": "Shi, W.P., Ju, D., Li, H., Yuan, L., Cui, J., Luo, D., Chen, Z.N., and Bian, H.J. (2018). CD147 Promotes CXCL1 Expression and Modulates Liver Fibrogenesis. Int. J. Mol. Sci., 19."
},
{
"DOI": "10.1042/CS20140823",
"article-title": "CD147 promotes liver fibrosis progression via VEGF-A/VEGFR2 signalling-mediated cross-talk between hepatocytes and sinusoidal endothelial cells",
"author": "Yan",
"doi-asserted-by": "crossref",
"first-page": "699",
"journal-title": "Clin. Sci.",
"key": "ref_63",
"volume": "129",
"year": "2015"
},
{
"DOI": "10.1021/acs.analchem.0c03173",
"article-title": "N- and O-Glycosylation of the SARS-CoV-2 Spike Protein",
"author": "Sanda",
"doi-asserted-by": "crossref",
"first-page": "2003",
"journal-title": "Anal. Chem.",
"key": "ref_64",
"volume": "93",
"year": "2021"
},
{
"DOI": "10.1093/glycob/cwaa042",
"article-title": "Deducing the N- and O-glycosylation profile of the spike protein of novel coronavirus SARS-CoV-2",
"author": "Shajahan",
"doi-asserted-by": "crossref",
"first-page": "981",
"journal-title": "Glycobiology",
"key": "ref_65",
"volume": "30",
"year": "2020"
},
{
"DOI": "10.1038/s41586-021-04352-y",
"article-title": "Evolution of enhanced innate immune evasion by SARS-CoV-2",
"author": "Thorne",
"doi-asserted-by": "crossref",
"first-page": "487",
"journal-title": "Nature",
"key": "ref_66",
"volume": "602",
"year": "2022"
},
{
"DOI": "10.1038/s41591-022-01689-3",
"article-title": "Long-term cardiovascular outcomes of COVID-19",
"author": "Xie",
"doi-asserted-by": "crossref",
"first-page": "583",
"journal-title": "Nat. Med.",
"key": "ref_67",
"volume": "28",
"year": "2022"
}
],
"reference-count": 67,
"references-count": 67,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.mdpi.com/2227-9059/11/7/2019"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"title": "Repurposing Niclosamide as a Novel Anti-SARS-CoV-2 Drug by Restricting Entry Protein CD147",
"type": "journal-article",
"volume": "11"
}