The safety and efficacy of melatonin in the treatment of COVID-19: A systematic review and meta-analysis
et al., Medicine, doi:10.1097/MD.0000000000030874, Sep 2022
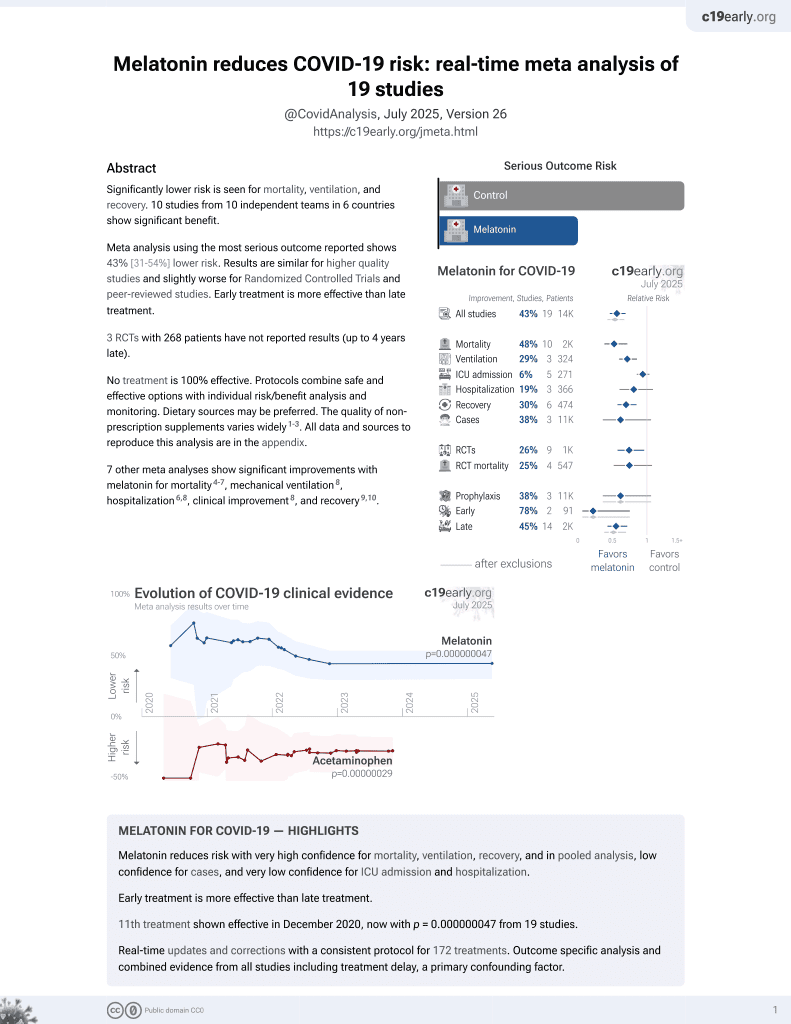
Melatonin for COVID-19
12th treatment shown to reduce risk in
December 2020, now with p = 0.0000000099 from 19 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
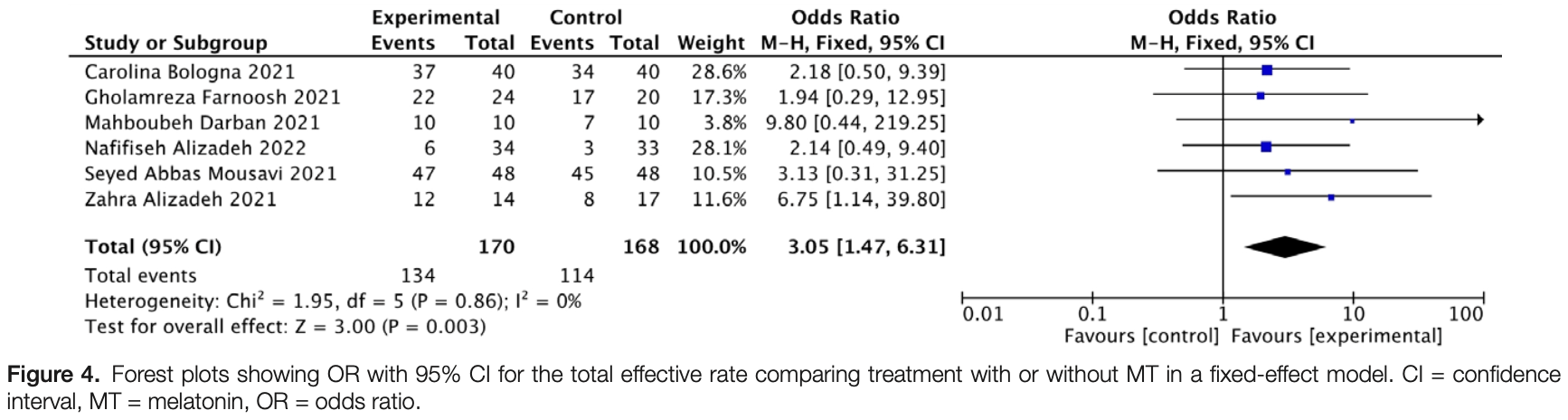
Systematic review and meta analysis of 6 melatonin studies showing significant improvement in recovery.
7 meta-analyses show significant improvements with melatonin for mortality1-4,
mechanical ventilation5,
hospitalization3,5,
improvement5, and
recovery6,7.
Currently there are 19 melatonin for COVID-19 studies, showing 33% lower mortality [19‑44%], 32% lower ventilation [19‑43%], 14% lower ICU admission [-1‑28%], 18% lower hospitalization [3‑30%], and 38% fewer cases [-6‑64%].
|
risk of no recovery, 67.2% lower, RR 0.33, p = 0.003, inverted to make RR<1 favor treatment.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
1.
Pilia et al., Does melatonin reduce mortality in COVID-19?, Annals of Medicine and Surgery, doi:10.1016/j.amsu.2022.103817.
2.
Tóth et al., Melatonin as adjuvant treatment in COVID-19 patients. A meta-analysis of randomized and propensity matched studies, Signa Vitae, doi:10.22514/sv.2023.076.
3.
Amin et al., Role of Melatonin in Management of COVID-19: A Systematic Review, Microbes, Infection and Chemotherapy, doi:10.54034/mic.e1982.
4.
Qin et al., Benefits of melatonin on mortality in severe-to-critical COVID-19 patients: A systematic review and meta-analysis of randomized controlled trials, Clinics, doi:10.1016/j.clinsp.2025.100638.
5.
Taha et al., Safety and efficacy of melatonin as an adjuvant therapy in COVID-19 patients: Systematic review and meta-analysis, Advances in Medical Sciences, doi:10.1016/j.advms.2023.09.007.
Wang et al., 30 Sep 2022, peer-reviewed, 4 authors.
Contact: caiyefeng@126.com.
The safety and efficacy of melatonin in the treatment of COVID-19: A systematic review and meta-analysis
Medicine, doi:10.1097/md.0000000000030874
Background: As an infectious disease caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the common signs of coronavirus disease 2019 (COVID-19) are respiratory symptoms, fever, cough, shortness of breath, and dyspnea, with multiple organ injuries in severe cases. Therefore, finding drugs to prevent and treat COVID-19 is urgently needed and expected by the public. Several studies suggested beneficial effects of melatonin for the relevant prevention and treatment. To explore the effect and safety of melatonin in the treatment and provide theoretical support and reference for seeking the most suitable drug for COVID-19, the meta-analysis was carried out accordingly. Methods: It included randomized clinical trials of patients with COVID-19 treated with melatonin. Total effective rate was the primary outcome, while C-reactive protein (CRP), arterial oxygen saturation (SaO 2 ), white blood cell count (WBC) were the secondary measures. Random-effect and fixed-effect models were used to evaluate the effect size of some indicators in this meta-analysis. Results: Six eligible studies with 338 participants were included. One hundred seventy subjects were treated with melatonin adjuvant therapy and 168 subjects were assigned to the control group, with total excellent effective rate in subjects treated with melatonin [odds ratio = 3.05, 95 % confidence interval (CI) = 1.47, 6.31, P = .003]. Homogeneity was analyzed by fixed effect model (I 2 = 0%). There was no significant difference in CRP between the melatonin group and the control group (weighted mean difference [WMD] = -0.36, 95% CI = -3.65, 2.92, P = .83). Significant difference was not existed in SaO 2 between the melatonin treatment group and the control group (WMD = 1, 95% CI = -1.21, 3.22, P = .37). In terms of WBC, there was no significant difference between the 2 groups (WMD = -1.07, 95% CI = -2.44, 0.30, P = .13). Conclusions: The meta-analysis showed that melatonin had the beneficial effects for COVID-19 prevention and treatment as an adjunctive agent in combination with basic treatment for the treatment. Abbreviations: CI = confidence interval, COVID-19 = coronavirus pandemic disease 2019, CRP = C-reactive protein, PRM = prolonged-release melatonin, RCT = randomized clinical trials, SaO 2 = arterial oxygen saturation, SARS-CoV-2 = severe acute respiratory syndrome coronavirus 2, WBC = white blood cells, WMD = weighted mean difference.
Author contributions X.W. finished the data analysis. X.W., G.W., and S.Z. wrote and revised the manuscript. S.Z. conceived and designed the study. Y.C. and S.Z. acquired funding supports and approved the final manuscript as submitted. Formal analysis: Xin-Chen Wang, Shi-Jie Zhang. Investigation: Xin-Chen Wang, Guang-Liang Wu, Shi-Jie Zhang. Project administration: Xin-Chen Wang, Ye-Feng Cai. Resources: Xin-Chen Wang, Guang-Liang Wu, Shi-Jie Zhang. Software: Xin-Chen Wang, Guang-Liang Wu. Supervision: Ye-Feng Cai, Shi-Jie Zhang. Visualization: Ye-Feng Cai. Writing -review & editing: Xin-Chen Wang.
References
Alizadeh, Dianatkhah, Alimohamadi, High dose melatonin as an adjuvant therapy in intubated patients with COVID-19: a randomized clinical trial, J Taibah Univ Med Sci
Alizadeh, Keyhanian, Ghaderkhani, A pilot study on controlling coronavirus disease 2019 (COVID-19) inflammation using melatonin supplement, Iran J Allergy Asthma Immunol
Auld, Maschauer, Morrison, Evidence for the efficacy of melatonin in the treatment of primary adult sleep disorders, Sleep Med Rev
Bologna, Madonna, Pone, Efficacy of prolonged-release melatonin 2 mg (PRM 2 mg) prescribed for insomnia in hospitalized patients for COVID-19: a retrospective observational study, J Clin Med
Camp, Bai, Gonullu, Melatonin interferes with COVID-19 at several distinct ROS-related steps, J Inorg Biochem
Chitimus, Popescu, Voiculescu, Melatonin's impact on antioxidative and anti-inflammatory reprogramming in homeostasis and disease, Biomolecules
Comai, Ochoa-Sanchez, Gobbi, Sleep-wake characterization of double MT/MT receptor knockout mice and comparison with MT and MT receptor knockout mice, Behav Brain Res
Darban, Malek, Memarian, Efficacy of high dose Vitamin C, melatonin and zinc in Iranian patients with acute respiratory syndrome due to coronavirus infection: a pilot randomized trial, Cytokines Cell Mol Ther
Dersimonian, Laird, Meta-analysis in clinical trials, Control Clin Trials
Farnoosh, Akbariqomi, Badri, Efficacy of a low dose of melatonin as an adjunctive therapy in hospitalized patients with COVID-19: a randomized, double-blind clinical trial, Arch Med Res
Galley, Lowes, Allen, Melatonin as a potential therapy for sepsis: a phase I dose escalation study and an ex vivo whole blood model under conditions of sepsis, J Pineal Res
Gray, Ryce, Melatonin for the Treatment of Insomnia: A Review of Clinical Effectiveness, Cost-Effectiveness, and Guidelines
Gunata, Parlakpinar, Acet, Melatonin: a review of its potential functions and effects on neurological diseases, Rev Neurol
Hardeland, Targeting host defense system and rescuing compromised mitochondria to increase tolerance against pathogens by melatonin may impact outcome of deadly virus infection pertinent to COVID-19, Molecules
Higgins, Altman, Gotzsche, The Cochrane Collaboration's tool for assessing risk of bias in randomised trials, BMJ
Higgins, Thompson, Deeks, Measuring inconsistency in meta-analyses, BMJ
Hosseini, Kashani, Nikzad, The novel coronavirus Disease-2019 (COVID-19): mechanism of action, detection and recent therapeutic strategies, Virology
Lu, Xiang, Du, SARS-CoV-2 infection in children -understanding the immune responses and controlling the pandemic, Pediatr Allergy Immunol
Majumder, Minko, Recent developments on therapeutic and diagnostic approaches for COVID-19, AAPS J
Mousavi, Heydari, Mehravaran, Melatonin effects on sleep quality and outcomes of COVID-19 patients: an open-label, randomized, controlled trial, J Med Virol
Oliveira, Coroa, Madeira, Treatment options for insomnia in schizophrenia: a systematic review, Pharmacopsychiatry
Otmani, Demazièresa, Staner, Effects of prolonged-release melatonin, zolpidem, and their combination on psychomotor functions, memory recall, and driving skills in healthy middle aged and elderly volunteers, Human Psychopharmacol Clin Exp
Page, Mckenzie, Bossuyt, Updating guidance for reporting systematic reviews: development of the PRISMA 2020 statement, J Clin Epidemiol
Pan, Mu, Yang, Clinical characteristics of COVID-19 patients with digestive symptoms in Hubei, China: a descriptive, cross-sectional, multicenter study, Am J Gastroenterol
Papillon, Mallet, Should melatonin be used as a sleeping aid for elderly people? Can, J Hosp Pharm
Rai, Kumar, Deekshit, Detection technologies and recent developments in the diagnosis of COVID-19 infection, Appl Microbiol Biotechnol
Samudrala, Kumar, Choudhary, Virology, pathogenesis, diagnosis and in-line treatment of COVID-19, Eur J Pharmacol
Schrire, Phillips, Chapman, Safety of higher doses of melatonin in adults: a systematic review and meta-analysis, J Pineal Res
Singal, Jaiswal, Seth, SARS-CoV-2, more than a respiratory virus: its potential role in neuropathogenesis, ACS Chem Neurosci
Solun, Shoenfeld, Inhibition of metalloproteinases in therapy for severe lung injury due to COVID-19, Med Drug Dis
Su, Wong, Shi, Epidemiology, genetic recombination, and pathogenesis of coronaviruses, Trends Microbiol
Ueland, Holter, Holten, Distinct and early increase in circulating MMP-9 in COVID-19 patients with respiratory failure, J Infect
Williamson, Walker, Bhaskaran, OpenSAFELY: factors associated with COVID-19 death in 17 million patients, Nature
Wu, Ji, Wang, Melatonin alleviates radiation-induced lung injury via regulation of miR-30e/NLRP3 Axis, Oxid Med Cell Longev
Wu, Yau, Yu, The diagnostic methods in the COVID-19 pandemic, today and in the future, Expert Rev Mol Diagn
Xie, Chen, Li, a review of sleep disorders and melatonin a review of sleep disorders and melatonin, Neurol Res
Yip, Chang, Wallace, Melatonin treatment improves adipose-derived mesenchymal stem cell therapy for acute lung ischemia-reperfusion injury, J Pineal Res
Zabetakis, Lordan, Norton, COVID-19: the inflammation link and the role of nutrition in potential mitigation, Nutrients
DOI record:
{
"DOI": "10.1097/md.0000000000030874",
"ISSN": [
"1536-5964"
],
"URL": "http://dx.doi.org/10.1097/MD.0000000000030874",
"author": [
{
"affiliation": [],
"family": "Wang",
"given": "Xin-Chen",
"sequence": "first"
},
{
"affiliation": [],
"family": "Wu",
"given": "Guang-Liang",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Cai",
"given": "Ye-Feng",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Zhang",
"given": "Shi-Jie",
"sequence": "additional"
}
],
"container-title": "Medicine",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2022,
9,
30
]
],
"date-time": "2022-09-30T13:07:49Z",
"timestamp": 1664543269000
},
"deposited": {
"date-parts": [
[
2022,
9,
30
]
],
"date-time": "2022-09-30T19:09:07Z",
"timestamp": 1664564947000
},
"indexed": {
"date-parts": [
[
2022,
10,
1
]
],
"date-time": "2022-10-01T05:17:52Z",
"timestamp": 1664601472635
},
"is-referenced-by-count": 0,
"issue": "39",
"issued": {
"date-parts": [
[
2022,
9,
30
]
]
},
"journal-issue": {
"issue": "39",
"published-print": {
"date-parts": [
[
2022
]
]
}
},
"language": "en",
"link": [
{
"URL": "https://journals.lww.com/10.1097/MD.0000000000030874",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "276",
"original-title": [],
"page": "e30874",
"prefix": "10.1097",
"published": {
"date-parts": [
[
2022,
9,
30
]
]
},
"published-print": {
"date-parts": [
[
2022,
9,
30
]
]
},
"publisher": "Ovid Technologies (Wolters Kluwer Health)",
"reference": [
{
"DOI": "10.1080/14737159.2020.1816171",
"article-title": "The diagnostic methods in the COVID-19 pandemic, today and in the future.",
"author": "Wu",
"doi-asserted-by": "crossref",
"first-page": "985",
"journal-title": "Expert Rev Mol Diagn",
"key": "R1-20220930",
"volume": "20",
"year": "2020"
},
{
"DOI": "10.1016/j.tim.2016.03.003",
"article-title": "Epidemiology, genetic recombination, and pathogenesis of coronaviruses.",
"author": "Su",
"doi-asserted-by": "crossref",
"first-page": "490",
"journal-title": "Trends Microbiol",
"key": "R2-20220930",
"volume": "24",
"year": "2016"
},
{
"DOI": "10.1021/acschemneuro.0c00251",
"article-title": "SARS-CoV-2, more than a respiratory virus: its potential role in neuropathogenesis.",
"author": "Singal",
"doi-asserted-by": "crossref",
"first-page": "1887",
"journal-title": "ACS Chem Neurosci",
"key": "R3-20220930",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.14309/ajg.0000000000000620",
"article-title": "Clinical characteristics of COVID-19 patients with digestive symptoms in Hubei, China: a descriptive, cross-sectional, multicenter study.",
"author": "Pan",
"doi-asserted-by": "crossref",
"first-page": "766",
"journal-title": "Am J Gastroenterol",
"key": "R4-20220930",
"volume": "115",
"year": "2020"
},
{
"DOI": "10.1111/pai.13267",
"article-title": "SARS-CoV-2 infection in children – understanding the immune responses and controlling the pandemic.",
"author": "Lu",
"doi-asserted-by": "crossref",
"first-page": "449",
"journal-title": "Pediatr Allergy Immunol",
"key": "R5-20220930",
"volume": "31",
"year": "2020"
},
{
"DOI": "10.1208/s12248-020-00532-2",
"article-title": "Recent developments on therapeutic and diagnostic approaches for COVID-19.",
"author": "Majumder",
"doi-asserted-by": "crossref",
"first-page": "14",
"journal-title": "AAPS J",
"key": "R6-20220930",
"volume": "23",
"year": "2021"
},
{
"DOI": "10.1016/j.ejphar.2020.173375",
"article-title": "Virology, pathogenesis, diagnosis and in-line treatment of COVID-19.",
"author": "Samudrala",
"doi-asserted-by": "crossref",
"first-page": "173375",
"journal-title": "Eur J Pharmacol",
"key": "R7-20220930",
"volume": "883",
"year": "2020"
},
{
"DOI": "10.1007/s00253-020-11061-5",
"article-title": "Detection technologies and recent developments in the diagnosis of COVID-19 infection.",
"author": "Rai",
"doi-asserted-by": "crossref",
"first-page": "441",
"journal-title": "Appl Microbiol Biotechnol",
"key": "R8-20220930",
"volume": "105",
"year": "2021"
},
{
"DOI": "10.1016/j.virol.2020.08.011",
"article-title": "The novel coronavirus Disease-2019 (COVID-19): mechanism of action, detection and recent therapeutic strategies.",
"author": "Seyed Hosseini",
"doi-asserted-by": "crossref",
"first-page": "1",
"journal-title": "Virology",
"key": "R9-20220930",
"volume": "551",
"year": "2020"
},
{
"DOI": "10.1016/j.neurol.2019.07.025",
"article-title": "Melatonin: a review of its potential functions and effects on neurological diseases.",
"author": "Gunata",
"doi-asserted-by": "crossref",
"first-page": "148",
"journal-title": "Rev Neurol (Paris)",
"key": "R10-20220930",
"volume": "176",
"year": "2020"
},
{
"DOI": "10.1111/jpi.12020",
"article-title": "Melatonin treatment improves adipose-derived mesenchymal stem cell therapy for acute lung ischemia-reperfusion injury.",
"author": "Yip",
"doi-asserted-by": "crossref",
"first-page": "207",
"journal-title": "J Pineal Res",
"key": "R11-20220930",
"volume": "54",
"year": "2013"
},
{
"article-title": "Melatonin alleviates radiation-induced lung injury via regulation of miR-30e/NLRP3 Axis.",
"author": "Wu",
"first-page": "4087298",
"journal-title": "Oxid Med Cell Longev",
"key": "R12-20220930",
"volume": "2019",
"year": "2019"
},
{
"DOI": "10.3390/molecules25194410",
"article-title": "Targeting host defense system and rescuing compromised mitochondria to increase tolerance against pathogens by melatonin may impact outcome of deadly virus infection pertinent to COVID-19.",
"author": "Hardeland",
"doi-asserted-by": "crossref",
"first-page": "4410",
"journal-title": "Molecules (Basel, Switzerland)",
"key": "R13-20220930",
"volume": "25",
"year": "2020"
},
{
"DOI": "10.3390/biom10091211",
"article-title": "Melatonin’s impact on antioxidative and anti-inflammatory reprogramming in homeostasis and disease.",
"author": "Chitimus",
"doi-asserted-by": "crossref",
"first-page": "1211",
"journal-title": "Biomolecules",
"key": "R14-20220930",
"volume": "10",
"year": "2020"
},
{
"DOI": "10.1016/j.jclinepi.2021.02.003",
"article-title": "Updating guidance for reporting systematic reviews: development of the PRISMA 2020 statement.",
"author": "Page",
"doi-asserted-by": "crossref",
"first-page": "103",
"journal-title": "J Clin Epidemiol",
"key": "R15-20220930",
"volume": "134",
"year": "2021"
},
{
"DOI": "10.1136/bmj.d5928",
"article-title": "The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials.",
"author": "Higgins",
"doi-asserted-by": "crossref",
"first-page": "1",
"journal-title": "BMJ",
"key": "R16-20220930",
"volume": "343",
"year": "2011"
},
{
"DOI": "10.1016/0197-2456(86)90046-2",
"article-title": "Meta-analysis in clinical trials.",
"author": "DerSimonian",
"doi-asserted-by": "crossref",
"first-page": "177",
"journal-title": "Control Clin Trials",
"key": "R17-20220930",
"volume": "7",
"year": "1986"
},
{
"DOI": "10.1136/bmj.327.7414.557",
"article-title": "Measuring inconsistency in meta-analyses.",
"author": "Higgins",
"doi-asserted-by": "crossref",
"first-page": "557",
"journal-title": "BMJ",
"key": "R18-20220930",
"volume": "327",
"year": "2003"
},
{
"article-title": "A pilot study on controlling coronavirus disease 2019 (COVID-19) inflammation using melatonin supplement.",
"author": "Alizadeh",
"first-page": "494",
"journal-title": "Iran J Allergy Asthma Immunol",
"key": "R19-20220930",
"volume": "20",
"year": "2021"
},
{
"article-title": "Efficacy of high dose Vitamin C, melatonin and zinc in Iranian patients with acute respiratory syndrome due to coronavirus infection: a pilot randomized trial.",
"author": "Darban",
"first-page": "164",
"journal-title": "Cytokines Cell Mol Ther",
"key": "R20-20220930",
"volume": "6",
"year": "2021"
},
{
"DOI": "10.1016/j.arcmed.2021.06.006",
"article-title": "Efficacy of a low dose of melatonin as an adjunctive therapy in hospitalized patients with COVID-19: a randomized, double-blind clinical trial.",
"author": "Farnoosh",
"doi-asserted-by": "crossref",
"first-page": "79",
"journal-title": "Arch Med Res",
"key": "R21-20220930",
"volume": "53",
"year": "2020"
},
{
"DOI": "10.3390/jcm10245857",
"article-title": "Efficacy of prolonged-release melatonin 2 mg (PRM 2 mg) prescribed for insomnia in hospitalized patients for COVID-19: a retrospective observational study.",
"author": "Bologna",
"doi-asserted-by": "crossref",
"first-page": "5857",
"journal-title": "J Clin Med",
"key": "R22-20220930",
"volume": "10",
"year": "2021"
},
{
"DOI": "10.1002/jmv.27312",
"article-title": "Melatonin effects on sleep quality and outcomes of COVID-19 patients: an open-label, randomized, controlled trial.",
"author": "Mousavi",
"doi-asserted-by": "crossref",
"first-page": "263271",
"journal-title": "J Med Virol",
"key": "R23-20220930",
"volume": "94",
"year": "2022"
},
{
"article-title": "High dose melatonin as an adjuvant therapy in intubated patients with COVID-19: a randomized clinical trial.",
"author": "Alizadeh",
"first-page": "454",
"journal-title": "J Taibah Univ Med Sci",
"key": "R24-20220930",
"volume": "17",
"year": "2022"
},
{
"DOI": "10.1016/j.smrv.2016.06.005",
"article-title": "Evidence for the efficacy of melatonin in the treatment of primary adult sleep disorders.",
"author": "Auld",
"doi-asserted-by": "crossref",
"first-page": "10",
"journal-title": "Sleep Med Rev",
"key": "R25-20220930",
"volume": "34",
"year": "2017"
},
{
"DOI": "10.1055/a-0658-1645",
"article-title": "Treatment options for insomnia in schizophrenia: a systematic review.",
"author": "Oliveira",
"doi-asserted-by": "crossref",
"first-page": "165",
"journal-title": "Pharmacopsychiatry",
"key": "R26-20220930",
"volume": "52",
"year": "2019"
},
{
"DOI": "10.1111/jpi.12134",
"article-title": "Melatonin as a potential therapy for sepsis: a phase I dose escalation study and an ex vivo whole blood model under conditions of sepsis.",
"author": "Galley",
"doi-asserted-by": "crossref",
"first-page": "427",
"journal-title": "J Pineal Res",
"key": "R28-20220930",
"volume": "56",
"year": "2014"
},
{
"article-title": "Safety of higher doses of melatonin in adults: a systematic review and meta-analysis.",
"author": "Schrire",
"first-page": "e12782",
"journal-title": "J Pineal Res",
"key": "R29-20220930",
"volume": "72",
"year": "2022"
},
{
"DOI": "10.3390/nu12051466",
"article-title": "COVID-19: the inflammation link and the role of nutrition in potential mitigation.",
"author": "Zabetakis",
"doi-asserted-by": "crossref",
"first-page": "1466",
"journal-title": "Nutrients",
"key": "R30-20220930",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1016/j.bbr.2013.01.008",
"article-title": "Sleep-wake characterization of double MT/MT receptor knockout mice and comparison with MT and MT receptor knockout mice.",
"author": "Comai",
"doi-asserted-by": "crossref",
"first-page": "231",
"journal-title": "Behav Brain Res",
"key": "R31-20220930",
"volume": "243",
"year": "2013"
},
{
"DOI": "10.1080/01616412.2017.1315864",
"article-title": "a review of sleep disorders and melatonin a review of sleep disorders and melatonin.",
"author": "Xie",
"doi-asserted-by": "crossref",
"first-page": "559",
"journal-title": "Neurol Res",
"key": "R32-20220930",
"volume": "39",
"year": "2019"
},
{
"DOI": "10.1002/hup.980",
"article-title": "Effects of prolonged-release melatonin, zolpidem, and their combination on psychomotor functions, memory recall, and driving skills in healthy middle aged and elderly volunteers.",
"author": "Otmani",
"doi-asserted-by": "crossref",
"first-page": "693",
"journal-title": "Human Psychopharmacol Clin Exp",
"key": "R33-20220930",
"volume": "23",
"year": "2010"
},
{
"article-title": "Should melatonin be used as a sleeping aid for elderly people?",
"author": "Papillon",
"first-page": "327",
"journal-title": "Can J Hosp Pharm",
"key": "R34-20220930",
"volume": "72",
"year": "2019"
},
{
"DOI": "10.1016/j.jinorgbio.2021.111546",
"article-title": "Melatonin interferes with COVID-19 at several distinct ROS-related steps.",
"author": "Camp",
"doi-asserted-by": "crossref",
"first-page": "111546",
"journal-title": "J Inorg Biochem",
"key": "R35-20220930",
"volume": "223",
"year": "2021"
},
{
"DOI": "10.1038/s41586-020-2521-4",
"article-title": "OpenSAFELY: factors associated with COVID-19 death in 17 million patients.",
"author": "Williamson",
"doi-asserted-by": "crossref",
"first-page": "430",
"journal-title": "Nature",
"key": "R36-20220930",
"volume": "584",
"year": "2020"
},
{
"DOI": "10.1016/j.jinf.2020.06.061",
"article-title": "Distinct and early increase in circulating MMP-9 in COVID-19 patients with respiratory failure.",
"author": "Ueland",
"doi-asserted-by": "crossref",
"first-page": "e41",
"journal-title": "J Infect",
"key": "R37-20220930",
"volume": "81",
"year": "2020"
},
{
"DOI": "10.1016/j.medidd.2020.100052",
"article-title": "Inhibition of metalloproteinases in therapy for severe lung injury due to COVID-19.",
"author": "Solun",
"doi-asserted-by": "crossref",
"first-page": "100052",
"journal-title": "Med Drug Dis",
"key": "R38-20220930",
"volume": "7",
"year": "2020"
}
],
"reference-count": 37,
"references-count": 37,
"relation": {},
"resource": {
"primary": {
"URL": "https://journals.lww.com/10.1097/MD.0000000000030874"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"General Medicine"
],
"subtitle": [],
"title": "The safety and efficacy of melatonin in the treatment of COVID-19: A systematic review and meta-analysis",
"type": "journal-article",
"volume": "101"
}