Role of Melatonin in Management of COVID-19: A Systematic Review
et al., Microbes, Infection and Chemotherapy, doi:10.54034/mic.e1982, Jun 2024
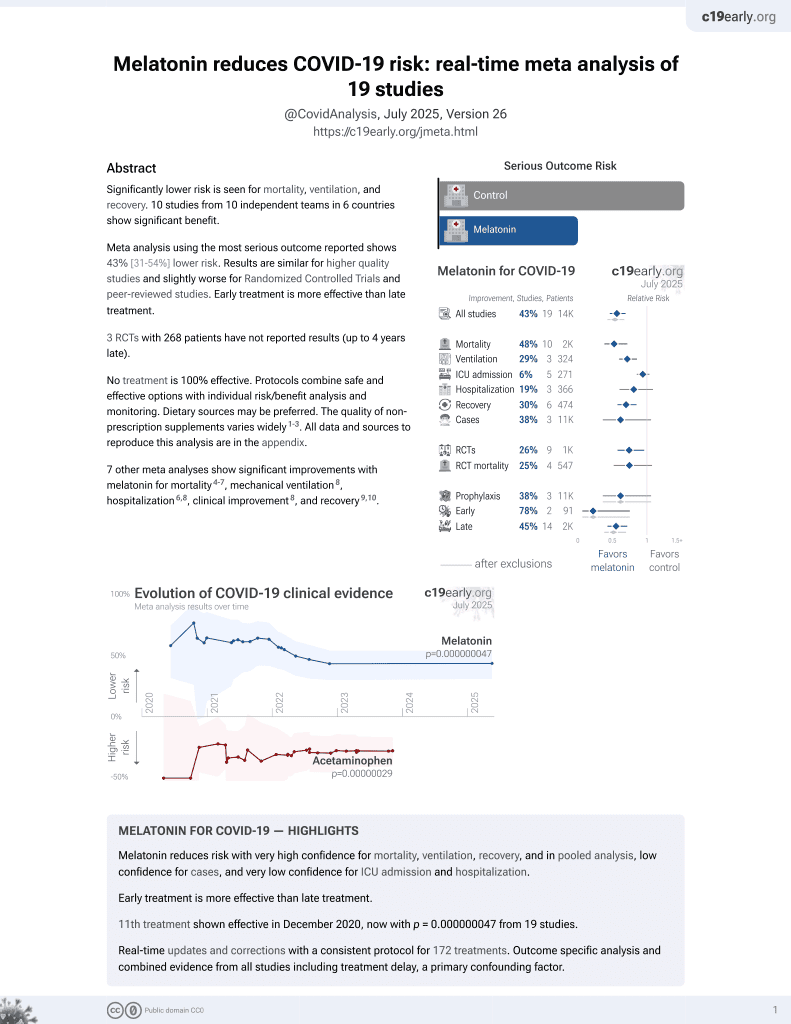
Melatonin for COVID-19
12th treatment shown to reduce risk in
December 2020, now with p = 0.000000015 from 18 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Meta analysis of 7 RCTs showing lower mortality and hospitalization time with melatonin treatment for COVID-19.
7 meta-analyses show significant improvements with melatonin for mortality1-4,
mechanical ventilation5,
hospitalization3,5,
improvement5, and
recovery6,7.
Currently there are 18 melatonin for COVID-19 studies, showing 33% lower mortality [19‑44%], 32% lower ventilation [19‑43%], 22% lower ICU admission [-4‑41%], 18% lower hospitalization [3‑30%], and 38% fewer cases [-6‑64%].
|
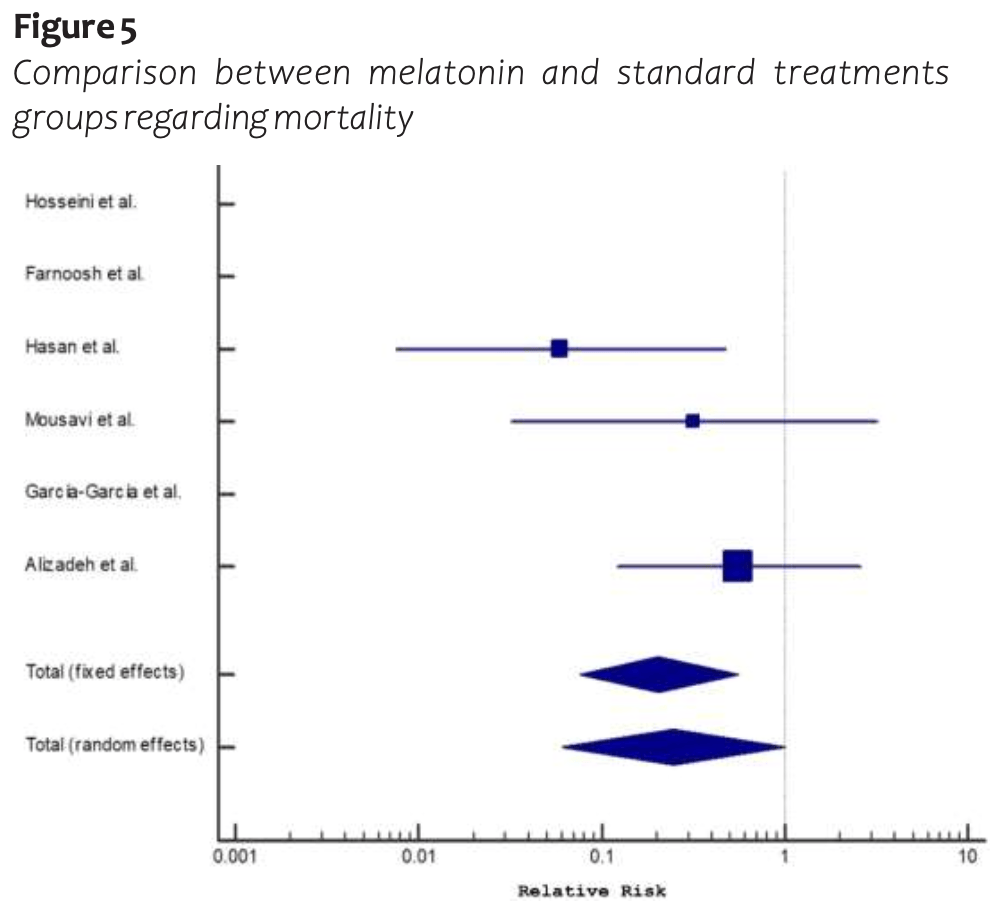
risk of death, 79.0% lower, RR 0.21, p = 0.002.
|
|
risk of ICU admission, 55.0% lower, RR 0.45, p = 0.13.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
1.
Pilia et al., Does melatonin reduce mortality in COVID-19?, Annals of Medicine and Surgery, doi:10.1016/j.amsu.2022.103817.
2.
Tóth et al., Melatonin as adjuvant treatment in COVID-19 patients. A meta-analysis of randomized and propensity matched studies, Signa Vitae, doi:10.22514/sv.2023.076.
3.
Amin et al., Role of Melatonin in Management of COVID-19: A Systematic Review, Microbes, Infection and Chemotherapy, doi:10.54034/mic.e1982.
4.
Qin et al., Benefits of melatonin on mortality in severe-to-critical COVID-19 patients: A systematic review and meta-analysis of randomized controlled trials, Clinics, doi:10.1016/j.clinsp.2025.100638.
5.
Taha et al., Safety and efficacy of melatonin as an adjuvant therapy in COVID-19 patients: Systematic review and meta-analysis, Advances in Medical Sciences, doi:10.1016/j.advms.2023.09.007.
Amin et al., 8 Jun 2024, peer-reviewed, 4 authors.
Contact: farouk.allam@med.asu.edu.eg.
Role of Melatonin in Management of COVID-19: A Systematic Review
Microbes, Infection and Chemotherapy, doi:10.54034/mic.e1982
Background: the COVID-19 pandemic has significantly impacted global healthcare and economic systems. The clinical manifestation of the disease varies from flu-like symptoms to severe pneumonia and, in some cases, death. Melatonin and its metabolites play a crucial role in immunomodulation and possess anti-oxidative properties, capable of directly and indirectly scavenging reactive oxygen species. Objective: the aim of the present systematic review was to assess the effectiveness of melatonin in the management of COVID-19 patients and its role in expediting the return of patients to their baseline health. Methodology: the literature review was conducted up to August 2022, resulting in the identification of 533 articles after sorting them by authors and year of publication. Following the removal of 223 duplicate articles, 310 abstracts were screened, leading to the exclusion of 281. Subsequently, 29 full-text studies were evaluated for eligibility, with 22 being excluded. Finally, seven studies met the inclusion criteria and were included for further qualitative and quantitative analyses. Results: the findings revealed a noteworthy reduction in hospital stay among patients who received melatonin compared to those who received a placebo (standardized mean difference: -0.50, Standard error: 0.15, 95% CI: -0.80, -0.20, P value: 0.001). Melatonin was associated with a significant decrease in mortality in COVID-19 patients when compared to the placebo (Pooled RR: 0.21, 95% CI: 0.08, 0.56, P value: 0.002). However, there were no significant differences between melatonin and placebo regarding the need for hospitalization, ICU admission, artificial ventilation, and the requirement for oxygen therapy. Conclusion: melatonin may decrease the mortality rate among patients with COVID-19. Melatonin may reduce the duration of hospital stay in patients with COVID-19. Melatonin had no effect on the following outcomes in COVID-19 patients: the need for hospitalization, ICU admission, artificial ventilation and the need for oxygen therapy.
Author contributions Field work supervision: Ghada Essam El-Din Amin, Salwa Mostafa Mohammad Abdel Rahman, Rehab Mohamed Ali Mohamed and Mohamed Farouk Allam. Analysis strategy and design: Ghada Essam El-Din Amin, Salwa Mostafa Mohammad Abdel Rahman, Rehab Mohamed Ali Mohamed and Mohamed Farouk Allam. Data management: Ghada Essam El-Din Amin, Salwa Mostafa Mohammad Abdel Rahman, Rehab Mohamed Ali Mohamed and Mohamed Farouk Allam. Data analysis and interpretation of results: Ghada Essam El-Din Amin, Salwa Mostafa Mohammad Abdel Rahman, Rehab Mohamed Ali Mohamed and Mohamed Farouk Allam. Decision making on content and paper write-up and revision of final draft: Ghada Essam El-Din Amin, Salwa Mostafa Mohammad Abdel Rahman, Rehab Mohamed Ali Mohamed and Mohamed Farouk Allam.
Ethics approval and consent to participate Not applicable .
Availability of data and materials Our study is a Systematic Review/Meta-analysis. The datasets analyzed during the current study are available in the published pooled study. Also, the datasets used and analyzed during the current study available from the corresponding author on reasonable request.
Competing interests No competing interests.
References
Alizadeh, Dianatkhah, Alimohamadi, Moradi, Akbarpour et al., High dose melatonin as an adjuvant therapy in intubated patients with COVID-19: A randomized clinical trial, J Taibah Univ Med Sci
Arendt, Aulinas, Physiology of the Pineal Gland and Melatonin
Davoodian, Sharifimood, Salarbashi, Elyasi, Baniasad et al., The effect of melatonin as an adjuvant therapy on COVID-19: A randomized clinical trial, SSRN Electron J
Dhama, Khan, Tiwari, Sircar, Bhat et al., Coronavirus Disease 2019-COVID-19, Clin Microbiol Rev, doi:10.1128/CMR.00028-20
Farnoosh, Akbariqomi, Badri, Bagheri, Izadi et al., Efficacy of a low dose of melatonin as an adjunctive therapy in hospitalized patients with COVID-19: A randomized, double-blind clinical trial, Arch Med Res
García-García, Seco-Meseguer, Ruiz-Seco, Navarro-Jimenez, Martínez-Porqueras et al., Melatonin in the prophylaxis of SARS-CoV-2 infection in healthcare workers (MeCOVID): A randomised clinical trial, J Clin Med
Gholizadeh, Abaj, Hasani, Mirzababaei, Mirzaei, Does the melatonin supplementation decrease the severity of the outcomes in COVID-19 patients? A mini review of observational data in the in vivo and in vitro studies, Melatonin Research
Gur, Taka, Yilmaz, Kilinc, Aktas et al., Conformational transition of SARS-CoV -2 spike glycoprotein between its closed and open states, J Chem Phys
Hacışevki, Baba, An Overview of Melatonin as an Antioxidant Molecule: A Biochemical Approach, Melatonin -Molecular Biology, Clinical and Pharmaceutical A, doi:10.5772/intechopen.79421
Hardeland, Melatonin and the pathologies of weakened or dysregulated circadian oscillators, J Pineal Res
Hasan, Atrakji, Mehuaiden, The effect of melatonin on thrombosis, sepsis and mortality rate in COVID-19 patients, Int J Infect Dis
Hosseini, Gouvarchin Ghaleh, Aghamollaei, Ramandi, Alishiri et al., Evaluation of Th1 and Th2 mediated cellular and humoral immunity in patients with COVID-19 following the use of melatonin as an adjunctive treatment, Eur J Pharmacol
Jackson, Farzan, Chen, Choe, Mechanisms of SARS-CoV-2 entry into cells, Nat Rev Mol Cell Biol
Kvetnoy, Ivanov, Mironova, Evsyukova, Nasyrov et al., Melatonin as the cornerstone of neuroimmunoendocrinology, Int J Mol Sci
Lan, Lee, Chao, Chang, Lu et al., Efficacy of melatonin in the treatment of patients with COVID-19: A systematic review and meta-analysis of randomized controlled trials, J Med Virol
Lankarani, Akbari, Homayounfar, Tabrizi, Vali et al., Therapeutic Efficacy of Melatonin in Patients with Coronavirus 2019: A Systematic Review and Meta-Analysis of Randomized Controlled Trials, Galen Medical Journal
Leroy, Han, Woottum, Bracq, Bouchet et al., Virus-mediated cell-cell fusion, Int J Mol Sci
Mao, Wang, Hu, Chen, He, Neurologic manifestations of hospitalized patients with Coronavirus disease 2019 in Wuhan, China, JAMA Neurol
Mousavi, Heydari, Mehravaran, Saeedi, Alizadeh-Navaei et al., Melatonin effects on sleep quality and outcomes of COVID-19 patients: An open-label, randomized, controlled trial, J Med Virol
Mubashshir, Ahmad, Negi, Rawal, Singhvi et al., Therapeutic Benefits of Melatonin against COVID-19, Neuroimmunomodulation, doi:10.1159/000531550
Pinato, Ramos, Hataka, Rossignoli, Granado et al., Day/night expression of MT1 and MT2 receptors in hypothalamic nuclei of the primate Sapajus apella, J Chem Neuroanat
Reiter, Sharma, Ma, Dominquez-Rodriguez, Marik et al., Melatonin inhibits COVID-19induced cytokine storm by reversing aerobic glycolysis in immune cells: A mechanistic analysis, Med Drug Discov
Reiter, Sharma, Ma, Rosales-Corral, Acuna-Castroviejo et al., Inhibition of mitochondrial pyruvate dehydrogenase kinase: a proposed mechanism by which melatonin causes cancer cells to overcome cytosolic glycolysis, reduce tumor biomass and reverse insensitivity to chemotherapy, Melatonin Res
Schoeman, Fielding, Coronavirus envelope protein: current knowledge, Virol J
Suofu, Li, Fg, Jia, Khattar et al., Dual role of mitochondria in producing melatonin and driving GPCR signaling to block cytochrome c release, Proc Natl Acad Sci U S A
Tesarik, After corona: there is life after the pandemic, Reprod Biomed Online
Tian, Li, Huang, Xia, Lu et al., Potent binding of 2019 novel coronavirus spike protein by a SARS coronavirus-specific human monoclonal antibody, Emerg Microbes Infect
Wang, Wu, Cai, Zhang, The safety and efficacy of melatonin in the treatment of COVID-19: A systematic review and meta-analysis, Medicine
Zambrelli, Canevini, Gambini, Agostino, Delirium and sleep disturbances in COVID-19: a possible role for melatonin in hospitalized patients?, Sleep Med
Zhang, Gao, Zhang, Sun, Li, Prophylactic use of exogenous melatonin and melatonin receptor agonists to improve sleep and delirium in the intensive care units: a systematic review and meta-analysis of randomized controlled trials, Sleep Breath
Zhang, Wang, Ni, Di, Ma et al., COVID-19: Melatonin as a potential adjuvant treatment, Life Sci
DOI record:
{
"DOI": "10.54034/mic.e1982",
"ISSN": [
"2789-4274"
],
"URL": "http://dx.doi.org/10.54034/mic.e1982",
"abstract": "<jats:p>Background: the COVID-19 pandemic has significantly impacted global healthcare and economic systems. The clinical manifestation of the disease varies from flu-like symptoms to severe pneumonia and, in some cases, death. Melatonin and its metabolites play a crucial role in immunomodulation and possess anti-oxidative properties, capable of directly and indirectly scavenging reactive oxygen species. Objective: the aim of the present systematic review was to assess the effectiveness of melatonin in the management of COVID-19 patients and its role in expediting the return of patients to their baseline health. Methodology: the literature review was conducted up to August 2022, resulting in the identification of 533 articles after sorting them by authors and year of publication. Following the removal of 223 duplicate articles, 310 abstracts were screened, leading to the exclusion of 281. Subsequently, 29 full-text studies were evaluated for eligibility, with 22 being excluded. Finally, seven studies met the inclusion criteria and were included for further qualitative and quantitative analyses. Results: the findings revealed a noteworthy reduction in hospital stay among patients who received melatonin compared to those who received a placebo (standardized mean difference: -0.50, Standard error: 0.15, 95% CI: -0.80, -0.20, P value: 0.001). Melatonin was associated with a significant decrease in mortality in COVID-19 patients when compared to the placebo (Pooled RR: 0.21, 95% CI: 0.08, 0.56, P value: 0.002). However, there were no significant differences between melatonin and placebo regarding the need for hospitalization, ICU admission, artificial ventilation, and the requirement for oxygen therapy. Conclusion: melatonin may decrease the mortality rate among patients with COVID-19. Melatonin may reduce the duration of hospital stay in patients with COVID-19. Melatonin had no effect on the following outcomes in COVID-19 patients: the need for hospitalization, ICU admission, artificial ventilation and the need for oxygen therapy.</jats:p>",
"author": [
{
"affiliation": [],
"family": "Amin",
"given": "Ghada Essam El-din",
"sequence": "first"
},
{
"affiliation": [],
"family": "Abdel Rahman",
"given": "Salwa Mostafa Mohammad",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Mohamed",
"given": "Rehab Mohamed Ali",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-5954-8909",
"affiliation": [],
"authenticated-orcid": false,
"family": "Allam",
"given": "Mohamed Farouk",
"sequence": "additional"
}
],
"container-title": "Microbes, Infection and Chemotherapy",
"container-title-short": "Microbes Infect. Chemother.",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2024,
6,
14
]
],
"date-time": "2024-06-14T14:14:58Z",
"timestamp": 1718374498000
},
"deposited": {
"date-parts": [
[
2024,
6,
14
]
],
"date-time": "2024-06-14T14:14:58Z",
"timestamp": 1718374498000
},
"indexed": {
"date-parts": [
[
2024,
6,
15
]
],
"date-time": "2024-06-15T00:27:29Z",
"timestamp": 1718411249719
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2024,
6,
8
]
]
},
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0",
"content-version": "unspecified",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2024,
6,
8
]
],
"date-time": "2024-06-08T00:00:00Z",
"timestamp": 1717804800000
}
}
],
"link": [
{
"URL": "https://revistas.unheval.edu.pe/index.php/mic/article/download/1982/1916",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://revistas.unheval.edu.pe/index.php/mic/article/download/1982/1916",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "19082",
"original-title": [],
"page": "e1982",
"prefix": "10.54034",
"published": {
"date-parts": [
[
2024,
6,
8
]
]
},
"published-online": {
"date-parts": [
[
2024,
6,
8
]
]
},
"publisher": "Universidad Nacional Hermilio Valdizan",
"reference-count": 0,
"references-count": 0,
"relation": {},
"resource": {
"primary": {
"URL": "https://revistas.unheval.edu.pe/index.php/mic/article/view/1982"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"title": "Role of Melatonin in Management of COVID-19: A Systematic Review",
"type": "journal-article",
"volume": "4"
}