Association of Vitamin D levels on the Clinical Outcomes of Patients Hospitalized for COVID-19 in a Tertiary Hospital
et al., Journal of the ASEAN Federation of Endocrine Societies, doi:10.15605/jafes.038.01.07, Feb 2023
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 135 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 135 hospitalized COVID-19 patients in the Philippines, showing higher risk of a poor outcome with vitamin D deficiency.
This is the 158th of 228 COVID-19 sufficiency studies for vitamin D, which collectively show higher levels reduce risk with p<0.0000000001.
|
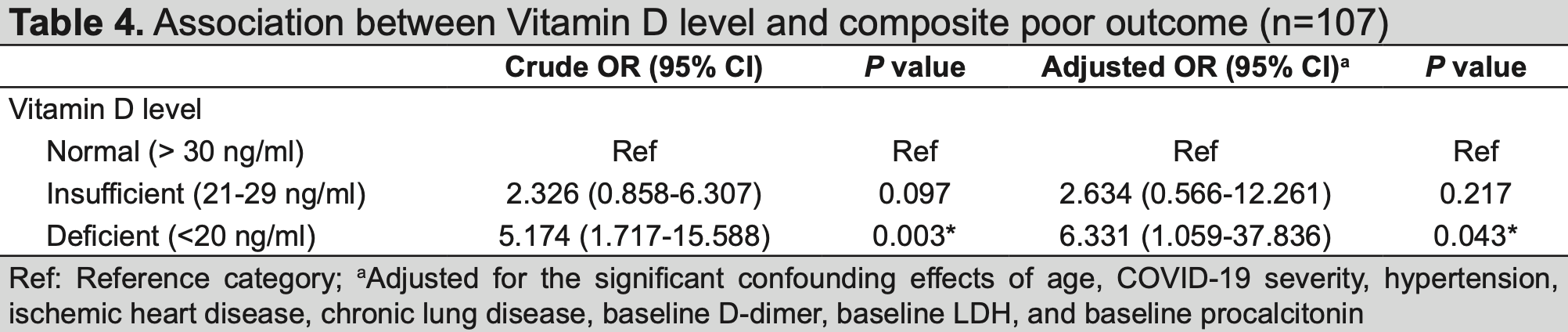
risk of progression, 71.5% lower, RR 0.29, p = 0.04, high D levels (≥30ng/mL) 7 of 38 (18.4%), low D levels (<20ng/mL) 18 of 34 (52.9%), NNT 2.9, adjusted per study, inverted to make RR<1 favor high D levels (≥30ng/mL), odds ratio converted to relative risk, combined mortality and morbidity, multivariable.
|
|
risk of death, 91.1% lower, RR 0.09, p = 0.002, high D levels (≥30ng/mL) 1 of 38 (2.6%), low D levels (<20ng/mL) 10 of 34 (29.4%), NNT 3.7, unadjusted.
|
|
risk of ICU admission, 82.1% lower, RR 0.18, p = 0.010, high D levels (≥30ng/mL) 2 of 38 (5.3%), low D levels (<20ng/mL) 10 of 34 (29.4%), NNT 4.1, unadjusted.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Tan et al., 27 Feb 2023, retrospective, Philippines, peer-reviewed, 3 authors.
Association of Vitamin D levels on the Clinical Outcomes of Patients Hospitalized for COVID-19 in a Tertiary Hospital
Journal of the ASEAN Federation of Endocrine Societies, doi:10.15605/jafes.038.01.07
Objectives. This study aimed to compare the severity of COVID-19, inflammatory parameters and clinical outcomes among patients with normal and subnormal levels of Vitamin D. Methodology. This is a retrospective cohort study of 135 patients admitted in a tertiary hospital for COVID-19. Patients were grouped according to their Vitamin D level. Primary outcome measure was the composite of all-cause mortality and morbidity. Other outcome measures determined were the comparison among the groups on the severity of COVID-19 infection, changes in inflammatory parameters, length of hospital stay and duration of respiratory support. Results. There was a significant trend of higher ICU admission (p-value=0.024), mortality (p-value=0.006) and poor clinical outcome (p-value=0.009) among the Vitamin D deficient group. No significant difference was found for most of the inflammatory parameters, duration of hospital stay and respiratory support. Overall, patients with deficient, but not insufficient Vitamin D level had 6 times higher odds of composite poor outcome than those with normal Vitamin D (crude OR=5.18, p-value=0.003; adjusted OR =6.3, p-value=0.043).
Conclusion. The inverse relationship between Vitamin D level and poor composite outcome observed in our study suggests that low Vitamin D may be a risk factor for poor prognosis among patients admitted for COVID-19.
CONCLUSION The high occurrence of hypovitaminosis D in severe and critical COVID-19 patients implies a potential relation to poor prognosis. Overall, patients with deficient, but not insufficient Vitamin D level had 6 times higher odds of composite poor outcome than those with normal Vitamin D after adjusting for potential confounders (Crude OR = 5.18; adjusted OR = 6.3). The inverse association between serum 25(OH)D levels and composite poor outcome (ICU admission, in-hospital mortality and morbidity) observed in our retrospective study suggests that a lower Vitamin D status upon admission may be an independent risk factor for poor prognosis in COVID-19.
Statement of Authorship The authors certified fulfillment of ICMJE authorship criteria.
CRediT Author
Author Disclosure The authors declared no conflict of interest.
Funding Source None. Authors are required to accomplish, sign and submit scanned copies of the JAFES Author Form consisting of: (1) Authorship Certification, that authors contributed substantially to the work, that the manuscript has been read and approved by all authors, and that the requirements for authorship have been met by each author; (2) the Author Declaration, that the article represents original material that is not being considered for publication or has not been published or accepted for publication elsewhere, that the article does not infringe or violate any copyrights or intellectual property rights, and that no references have been made..
References
Agarwal, Phan, Willix R Jr, Barber, Schwarz, Is Vitamin D deficiency associated with heart failure? A review of current evidence, J Cardiovasc Pharmacol Ther, doi:10.1177/1074248410390214
Ali, Role of Vitamin D in preventing of COVID-19 infection, progression and severity, J Infect Public Health, doi:10.1016/j.jiph.2020.06.021
Aranow, Vitamin D and the immune system, J Investig Med, doi:10.2310/JIM.0b013e31821b8755
Campi, Gennari, Merlotti, Vitamin D and COVID-19 severity and related mortality: A prospective study in Italy, BMC Infect Dis, doi:10.1186/s12879-021-06281-7
Daneshkhah, Agrawal, Eshein, Subramanian, Roy et al., Evidence for possible association of Vitamin D status with cytokine storm and unregulated inflammation in COVID-19 patients, Aging Clin Exp Res, doi:10.1007/s40520-020-01677-y
Demir, Demir, Aygun, Vitamin D deficiency is associated with COVID-19 positivity and severity of the disease, J Med Virol, doi:10.1002/jmv.26832
Driggin, Madhavan, Gupta, The role of Vitamin D in cardiovascular disease and COVID-19, Rev Endocr Metab Disord, doi:10.1007/s11154-021-09674-w
Fatemi, Ardehali, Eslamian, Noormohammadi, Malek, Association of Vitamin D deficiency with COVID-19 severity and mortality in Iranian people: A prospective observational study, Acute Crit Care, doi:PMCID:PMC8907463.ttps://doi.org/10.4266/acc.2021.00605
Grant, Lahore, Mcdonnell, Evidence that Vitamin D supplementation could reduce risk of influenza and COVID-19 infections and deaths, Nutrients, doi:10.3390/nu12040988
Greenland, Pearce, Statistical foundations for model-based adjustments, Annu Rev Public Health, doi:10.1146/annurev-publhealth-031914-122559
Holick, Binkley, Bischoff-Ferrari, Evaluation, treatment, and prevention of Vitamin D deficiency: An Endocrine Society clinical practice guideline, J Clin Endocrinol Metab, doi:10.1210/jc.2011-0385
Holick, The Vitamin D deficiency pandemic: Approaches for diagnosis, treatment and prevention, Rev Endocr Metab Disord, doi:10.1007/s11154-017-9424-1
Ilie, Stefanescu, Smith, The role of Vitamin D in the prevention of coronavirus disease 2019 infection and mortality, Aging Clin Exp Res, doi:10.1007/s40520-020-01570-8
Infante, Buoso, Pieri, Low Vitamin D status at admission as a risk factor for poor survival in hospitalized patients with COVID-19: An Italian retrospective study, J Am Nutr Assoc, doi:10.1080/07315724.2021.1877580
Jain, Chaurasia, Sengar, Singh, Mahor et al., Analysis of Vitamin D level among asymptomatic and critically ill COVID-19 patients and its correlation with inflammatory markers, Sci Rep, doi:10.1038/s41598-020-77093-z
Jolliffe, Holt, Greenig, Effect of a test-and-treat approach to Vitamin D supplementation on risk of all cause acute respiratory tract infection and covid-19: phase 3 randomised controlled trial (CORONAVIT), BMJ, doi:10.1136/bmj-2022-071230
Li, Hu, Yu, Ma, Retrospective analysis of laboratory testing in 54 patients with severe-or critical-type 2019 novel coronavirus pneumonia, Lab Invest, doi:10.1038/s41374-020-0431-6
Orchard, Baldry, Nasim-Mohi, Vitamin-D levels and intensive care unit outcomes of a cohort of critically ill COVID-19 patients, Clin Chem Lab Med, doi:10.1515/cclm-2020-1567
Palomer, González-Clemente, Blanco-Vaca, Role of Vitamin D in the pathogenesis of type 2 diabetes mellitus, Diabetes Obes Metab, doi:10.1111/j.1463-1326.2007
Pecina, Merry, Park, Td, Vitamin D status and severe COVID-19 disease outcomes in hospitalized patients, J Prim Care Community Health, doi:10.1177/21501327211041206
Peng, Liu, Zheng, Immunological aspects of SARS-CoV-2 infection and the putative beneficial role of Vitamin-D, Int J Mol Sci, doi:10.3390/ijms22105251
Pereira, Damascena, Azevedo, De Almeida Oliveira, Da et al., Vitamin D deficiency aggravates COVID-19: Systematic review and meta-analysis, Crit Rev Food Sci Nutr, doi:10.1080/104
Perlas, Capanzana, Vitamin D status of Filipino adults: Evidence from the 8th National Nutrition Survey 2013, Malays J Nutr
Reis, Fernandes, Sales, Influence of Vitamin D status on hospital length of stay and prognosis in hospitalized patients with moderate to severe COVID-19: A multicenter prospective cohort study, Am J Clin Nutr, doi:10.1093/ajcn/nqab151.medicalcharts
Samprathi, Jayashree, Biomarkers in COVID-19: An Up-To-Date review, Front Pediatr, doi:10.3389/fped.2020.607647
Sengupta, Majumder, Majumder, Role of Vitamin D in treating COVID-19-associated coagulopathy: Problems and perspectives, Mol Cell Biochem, doi:10.1007/s11010-021-04093-6
Sung, Liao, Lu, Wu, Role of Vitamin D in insulin resistance, J Biomed Biotechnol, doi:10.1155/2012/634195
Syquio, Genuino, Tolosa, Should Vitamin D supplements be used as adjunct treatment for COVID-19? Philippine COVID-19 Living Clinical Practice Guidelines
Teama, Abdelhakam, Elmohamadi, Badr, Vitamin D deficiency as a predictor of severity in patients with COVID-19 infection, Sci Prog, doi:10.1177/00368504211036854
Vranić, Mikolašević, Milić, Vitamin D deficiency: Consequence or cause of obesity?, Medicina, doi:10.3390/medicina55090541
Yao, Cao, Wang, D-dimer as a biomarker for disease severity and mortality in COVID-19 patients: A case control study, J Intensive Care, doi:10.1186/s40560-020-00466-z
DOI record:
{
"DOI": "10.15605/jafes.038.01.07",
"ISSN": [
"0857-1074",
"2308-118X"
],
"URL": "http://dx.doi.org/10.15605/jafes.038.01.07",
"author": [
{
"affiliation": [],
"family": "Tan",
"given": "Margarita Katrina Amor",
"sequence": "first"
},
{
"affiliation": [],
"name": "Chinese General Hospital and Medical Center, Philippines",
"sequence": "first"
},
{
"affiliation": [],
"family": "Lim Alba",
"given": "Rebecca",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Li",
"given": "Kingbherly",
"sequence": "additional"
}
],
"container-title": "Journal of the ASEAN Federation of Endocrine Societies",
"container-title-short": "JAFES",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2023,
3,
1
]
],
"date-time": "2023-03-01T08:35:44Z",
"timestamp": 1677659744000
},
"deposited": {
"date-parts": [
[
2023,
5,
18
]
],
"date-time": "2023-05-18T05:52:33Z",
"timestamp": 1684389153000
},
"indexed": {
"date-parts": [
[
2024,
3,
2
]
],
"date-time": "2024-03-02T03:19:33Z",
"timestamp": 1709349573027
},
"is-referenced-by-count": 1,
"issue": "1",
"issued": {
"date-parts": [
[
2023,
5,
18
]
]
},
"journal-issue": {
"issue": "1",
"published-online": {
"date-parts": [
[
2023,
5,
18
]
]
},
"published-print": {
"date-parts": [
[
2023,
5,
18
]
]
}
},
"link": [
{
"URL": "https://asean-endocrinejournal.org/index.php/JAFES/article/view/2437",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "6244",
"original-title": [],
"page": "81-89",
"prefix": "10.15605",
"published": {
"date-parts": [
[
2023,
5,
18
]
]
},
"published-online": {
"date-parts": [
[
2023,
5,
18
]
]
},
"published-print": {
"date-parts": [
[
2023,
5,
18
]
]
},
"publisher": "Journal of the ASEAN Federation of Endocrine Societies (JAFES)",
"reference-count": 0,
"references-count": 0,
"relation": {},
"resource": {
"primary": {
"URL": "https://asean-endocrinejournal.org/index.php/JAFES/article/view/2437"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Endocrinology",
"Endocrinology, Diabetes and Metabolism"
],
"subtitle": [],
"title": "Association of Vitamin D levels on the Clinical Outcomes of Patients Hospitalized for COVID-19 in a Tertiary Hospital",
"type": "journal-article",
"volume": "38"
}
